Published online Oct 15, 1998. doi: 10.3748/wjg.v4.i5.443
Revised: July 16, 1998
Accepted: August 23, 1998
Published online: October 15, 1998
AIM: To evaluate the therapeutic mechanism of Yinchenhao Chengqi ( YCHCQ ) decoction (containing mainly Herba Artemisia capillaris) combined with endoscopic sphincterotomy (EST) for endotoxemia (ETM) in acute cholangitis.
METHODS: Twenty-one cases of acute cholangitis with ETM were divided randomly into two groups: group A, 10 patients treated with YCHCQ decoction combined with EST, group B, 11 patients treated with EST. The incidence rate of ETM, plasmic ET, serum superoxide dismutase (SOD) activity, malonyldialdehyde (MDA), complement C3 and C-reactive protein (CRP) were studied respectively.
RESULTS: The ET level of group A (35.92 ng/L ± 8.30 ng/L) was significantly reduced after 7 days of treatment (P < 0.05) in contrast to that of group B (47.8 ng/L ± 11.62 ng/L), so did the level of MDA and CRP. But the SOD activity and C3 level in group A increased significantly (P < 0.05).
CONCLUSION: YCHCQ decoction combined with EST had a beneficial effect for ETM in acute cholangitis.
- Citation: Shang D, Guan FL, Jin PY, Chen HL, Cui JH. Effect of combined therapy of Yinchenhao Chengqi decoction and endoscopic sphincterotomy for endotoxemia in acute cholangitis. World J Gastroenterol 1998; 4(5): 443-445
- URL: https://www.wjgnet.com/1007-9327/full/v4/i5/443.htm
- DOI: https://dx.doi.org/10.3748/wjg.v4.i5.443
Endotoxemia (ETM) is one of the most important physiopathologic causes of acute cholangitis and it is the trigger of cytokines and inflammatory factors. In recent studies it has been found that Yinchenhao Chengqi (YCHCQ) decoction has a beneficial effect on ETM in acute cholangitis. With the development of endoscopic surgery, endoscopic sphincterotomy (EST) has become an effective replacement for some operations in the treatment of acute cholangitis[1]. The effect of YCHCQ decoction combined with EST on ET, oxygen free radical and complement C3 was observed in order to find out its therapeutic mechanism.
Twenty-one cases of acute cholangitis with endotoxemia were divided randomly into two groups: group A, 10 patients (6 males and 4 females) treated with YCHCQ decoction and EST; and group B, 11 patients (6 males, 5 females) treated with EST (Table 1, Table 2).
| Group | No. of patients | Common bile duct stones (%) | Benign stenosis of Oddi’s sphincter (%) | Biliary ascariasis (%) |
| Group B | 11 | 6 (55) | 4 (36) | 1 (9) |
| Group A | 10 | 6 (60) | 3 (30) | 1 (10) |
| Group | No. of patients | WBC in peripheral blood (109/L) | Percent of neutrophil cell | Temperature ( °C ) | Age (years) |
| Group B | 11 | 15.47 ± 6.83 | 0.85 ± 0.08 | 38.92 ± 1.32 | 52.43 ± 13.61 |
| Group A | 10 | 15.36 ± 7.26 | 0.83 ± 0.09 | 38.87 ± 1.24 | 56.21 ± 14.17 |
| P | > 0.05 | > 0.05 | > 0.05 | > 0.05 |
EST treatment EST was performed on the patients with benign stenosis of Oddi’s sphincter. Besides EST, stone extraction using Dormia basket, retrieval balloon or mechanical lithotriptor was also followed in the patients with common bile duct stones, and ascaris lumbricoides extraction using forceps was conducted in those with biliary ascariasis.
Combined treatment of EST and YCHCQ decoction The patients in group A took one YCHCQ decoction a day, 100 mL in the morning and 100 mL at night. YCHCQ dection was composed of Herba Artemisiae capillaris 30 g, Fructus Gardeniae 15 g, Cortex Magnoliae Officinalis 15 g, Fructus Aurantii 15 g, Radix et rhizoma Rhei 15 g (added later) and Natrii Sulfas 10 g (taking with hot decoction).
Assay of ET, superoxide dismutase (SOD), malonyldialdehyde (MDA), complement C3 and C-reactive protein (CRP) in peripheral blood Plasmic ET was measured using limulus ozo-group development process, serum SOD was determined using xanthine oxidase process, and MDA by the thiobarbituric acid clorimetric method. CRP and C3 were detected with fully-automatic instruments for biochemical analysis.
Definition of ETM ET in peripheral blood of 50 normal volunteers was measured. The result was 32.53 ng/L ± 10.32 ng/L. Plasmic ET of 95% normal volunteers ranged from 0 ng/L to 53.84 ng/L. If it is above 54 ng/L, it is defined as ETM.
The results were expressed as -x±sx. Data were analyzed using Student’s t test. The incidence rate of ETM was analyzed using χ2 test. P value less than 0.05 was considered significant.
The average days of hospitalization in group A were 7 days, 9 recovered and 1 improved, and no complication occurred, while, the average days of hospitalization of group B were 12 days, 9 recovered and 3 improved, and complications occurred in 2 cases, including one case of acute peritonitis, and one case of common bile duct stones at the ampulla of Vater who underwent an operation to remove the stones.
In Table 3, plasmic ET level of the two groups was markedly higher than that of the normal volunteers, and ETM occurred. On the 3rd day after treatment, the incidence rate of ETM in group A was lowered significantly, as compared with that before treatment. The incidence rate of group B also decreased, but there was no significant difference as compared with before until the 5th day after treatment. The plasmic ET level of the two groups declined obviously on the 3rd day, but without significant difference between the two groups. On the 5th and 7th day, ET level was lower in group A than in group B.
Before treatment, the activity of serum SOD was lower in both groups than normal (104.2 kNU/L ± 18.8 kNU/L). There was nosignificant difference between the two groups, although on the 3rd and 7th day after treatment, the activity of serum SOD in the two groups obviously increased, that of group A being much higher than that of group B (P < 0.05). On the 7th day, serum SOD values of group A had already turned normal (Table 4).
| Group | No.of patients | Before treatment | After treatment | ||
| d3 | d5 | d7 | |||
| Plasmic ET (ng/L) | |||||
| Group B | 11 | 97.12 ± 15.20 | 72.84 ± 10.36a | 62.61 ± 10.08a | 47.80 ± 11.62a |
| Group A | 10 | 98.67 ± 15.54 | 67.07 ± 13.50a | 48.18 ± 11.46ac | 35.92 ± 8.30ac |
| Serum SOD (kNU/L) | |||||
| Group B | 11 | 62.52 ± 8.01 | 72.38 ± 10.52a | 86.89 ± 13.56a | |
| Group A | 10 | 63.68 ± 9.45 | 96.47 ± 15.35ac | 105.18 ± 13.21ac | |
| Serum MDA (μmol/L) | |||||
| Group B | 11 | 38.50 ± 2.29 | 24.40 ± 2.43a | 12.47 ± 1.70a | |
| Group A | 10 | 37.32 ± 3.80 | 6.40 ± 1.28ac | 4.33 ± 1.03ac | |
It is shown in Table 4 that the level of serum MDA lowered in various degrees in both groups after treatment. MDA level in group A became nearly normal on the 7th day.
There was no difference in the CRP level between the two groups, which was both obviously higher than the normal level before treatment. The CRP level obviously decreased after treatment on the 3rd and 7th day. However, the CRP value in group A declined much more significantly than that in group B (P < 0.05) (Figure 1).
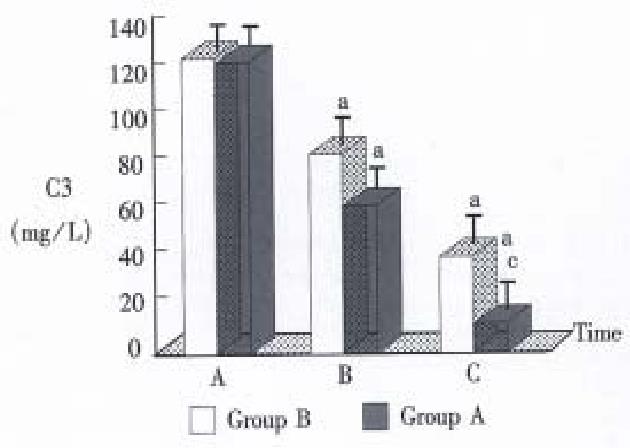
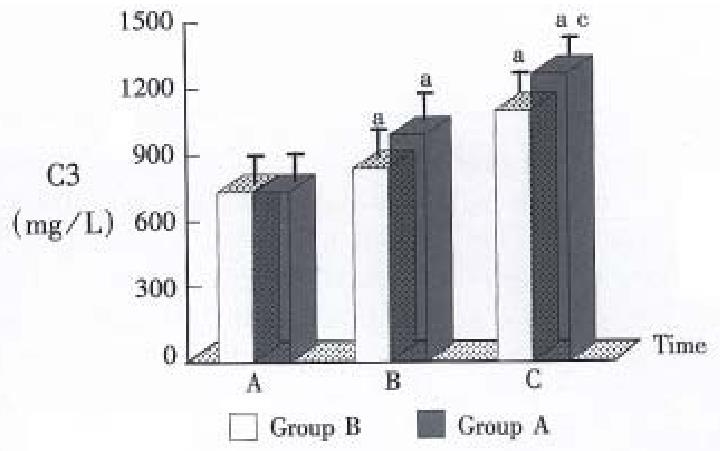
As shown in Figure 2, there was no significant difference in serum C3 of the two groups which was both lower than the normal before treatment. However, patients treated with combined YCHCQ decoction and EST had significantly higher serum SOD than group B.
As an antagonistic agent, YCHCQ decoction can reduce ET production and absorption. Redix et Rhizoma Rhei and Natrii Sulfas could get rid of abdominal mass, bacteria and ET with an effect of “Tongligongxia” in TCM to reduce the ET. Redix et Rhizoma Rhei, Fructus Gardeniae and Cortex Magnoliae Officinalis have a more powerful bacteriostatic effect to reduce the production of ET and the incidence of ETM derived from the gut[2]. Redix et Rhizoma Rhei, Herba Artemisiae Scopariae and Fructus Gardeniae are also cholagogues, antispasmodics and anti-inflammatory agents. They can lower the incidence rate of ETM which resulted from bile duct obstruction because the inflammatory bile in the bile duct flows into the intestinal tract. Some studies have confirmed that Redix et Rhizoma Rhe has a more powerful antagonistic effect on ET. The destroyed reticular structure of ET by Redix et Rhizoma Rhe was observed under electron microscope.
YCHCQ decoction could reduce the production of oxygen free radical. ET could activate the respiratory burst of leukocyte. A large amount of oxygen free radicals strongly damage the histocyte, particularly the gut barrier[3]. Peroxide, such as MDA etc, is produced because of lipid peroxidation by oxygen free radical which could attack multiple unsaturated fatty acid on the biological membrane[4]. YCHCQ decoction may reduce the production of peroxide MDA, increase the activity of SOD, decrease the permeability of capillary, and promote microcirculation. Therefore, it can reduce the production of oxygen free radical, keep the balance of oxidation and antioxidation, lessen the damage to the gut barrier, reduce the production and absorption of ET, inhibit the cascade effect of ET and oxygen free radical, stop pernicious circulation, keep the stabilization of the internal environment, raise the ability of antioxidation and alleviate the damage of peroxidation to organisms.
YCHCQ decoction could enhance immunologic function, and promote the recovery of the function of the complement system, the macrophage system and the inactivation of ET.
This study confirms that YCHCQ decoction combined with EST had a better therapentic effect on ETM in acute cholangitis. Its advantages are that: EST could incise part of the papilla so as to clear common bile duct stones with mechanical litheropsy instrument, and to eliminate the factors of mechanical obstruction and bile duct stenosis. On the basis of this action, the therapeutic effect of YCHCQ decoction could be fully exerted. Thus, the most important factors of acute cholangitis were eliminated because common bile duct stones were successfully removed with the combined treatment. In addition, endoscopic retrograde biliary drainage or endoscopic nasobiliary drainage were performed after EST, in order to reduce the pressure of the bile duct, drain the inflammatory bile, remove the “Damp-Heat” and the mass on the abdomen, normalize secretion and discharge the bile, reduce jaundice, and preserve the function of the liver and the kidney.
EST is an established non-²surgical method of management for patients with acute cholangitis from biliary obstruction or various causes. The results show that the patients undergoing EST do not require surgical operation and rarely suffer from complications. They need only a short time of hospitalization, experience little pain, and obtain a rapid recovery. Also, this treatment dose not have the limitations caused by repeated surgical operations or the conditions of patients[5]. YCHCQ decoction could reduce or eliminate the occurrence of ETM in acute cholangitis. With its therapeutic effect of “Tongligongxia” and clearing away “damp-heat” and “Fuzhengquxie” in TCM, YCHCQ decoction can reduce the production of oxygen free radical and lipid peroxidation, thus inhibiting the production and absorption of ET.
Project supported by the National Natural Science Foundation of China, No.38970871.
| 1. | Boender J, Nix GA, de Ridder MA, Dees J, Schütte HE, van Buuren HR, van Blankenstein M. Endoscopic sphincterotomy and biliary drainage in patients with cholangitis due to common bile duct stones. Am J Gastroenterol. 1995;90:233-238. [PubMed] |
| 2. | Chen HL, Zhou JY, Guan FL. [Effect of da cheng qi decoction co. on endotoxemia in obstructive jaundice]. Zhongxiyi Jiehe Zazhi. 1991;11:724-76, 709. [PubMed] |
| 3. | Chen HL, Wu XZ. Cytokines and Multiple system organ failure. Foreign Med Sci (Sec Physiol Pathol Clin). 1995;15:261-264. |
| 4. | Borregaard N, Miller LJ, Springer TA. Chemoattractant-regulated mobilization of a novel intracellular compartment in human neutrophils. Science. 1987;237:1204-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 166] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Prat F, Tennenbaum R, Ponsot P, Altman C, Pelletier G, Fritsch J, Choury AD, Bernades P, Etienne JP. Endoscopic sphincterotomy in patients with liver cirrhosis. Gastrointest Endosc. 1996;43:127-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |