Published online Sep 21, 2021. doi: 10.3748/wjg.v27.i35.5958
Peer-review started: May 10, 2021
First decision: June 27, 2021
Revised: July 8, 2021
Accepted: August 18, 2021
Article in press: August 18, 2021
Published online: September 21, 2021
Processing time: 128 Days and 2.3 Hours
Endoscopic resection of duodenal subepithelial lesions (SELs) is a difficult procedure with a high risk of perforation. At present, dealing with perforation after endoscopic resection of duodenal SELs is still considered a great challenge.
To evaluate the effectiveness and safety of an over-the-scope clip (OTSC) in the treatment of perforation post-endoscopic resection of duodenal SELs.
From May 2015 to November 2019, 18 patients with perforation following endoscopic resection of duodenal SELs were treated with OTSCs. Data comprising the rate of complete resection, closure of intraprocedural perforation, delayed bleeding, delayed perforation, and postoperative infection were extracted.
The rate of complete removal of duodenal SELs and successful closure of the perforation was 100%. The median perforation size was 1 cm in diameter. Seventeen patients had minor intraoperative bleeding, while the remaining 1 patient had considerable amount of bleeding during the procedure. Seven patients had postoperative abdominal infections, of which 1 patient developed an abscess in the right iliac fossa and another patient developed septic shock. All 18 patients recovered and were discharged. No delayed bleeding or perforation was reported. The mean time taken to resume normal diet after the procedure was 6.5 d. The mean postoperative hospital stay was 9.5 d. No residual or recurrent lesions were detected during the follow-up period (15-66 mo).
Closing a perforation after endoscopic resection of duodenal SELs with OTSCs seems to be an effective and reasonably safe therapeutic method.
Core Tip: This study presents the use of over-the-scope clip in closing duodenal perforation of 18 patients. We believe that our study makes a significant contribution to the literature because dealing with perforation after endoscopic resection of duodenal subepithelial lesions is challenging. This study aimed to evaluate the effectiveness and safety of over-the-scope clip in closing perforation after endoscopic resection of duodenal subepithelial lesions. The rate of successful closure was 100%. No delayed perforation occurred in any of the patients. Seven patients had postoperative infection, of which 1 patient developed septic shock and underwent surgery. All 18 patients recovered.
- Citation: Wang ZZ, Zhou XB, Wang Y, Mao XL, Ye LP, Yan LL, Chen YH, Song YQ, Cai Y, Xu SW, Li SW. Effectiveness and safety of over-the-scope clip in closing perforations after duodenal surgery. World J Gastroenterol 2021; 27(35): 5958-5966
- URL: https://www.wjgnet.com/1007-9327/full/v27/i35/5958.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i35.5958
Duodenal subepithelial lesions (SELs) include Brunner’s adenomas, lipomas, heterotopic pancreas, leiomyomas, neuroendocrine tumors, and gastrointestinal stromal tumors (GISTs). Most of these are benign, while some lesions, such as neuroendocrine tumors and GISTs, are potentially malignant[1-3]. Resection of these lesions may contribute to improvement in diagnosis and treatment outcomes.
Surgery, including pancreatoduodenectomy and limited resection, is the most basic treatment for duodenal lesions. However, due to the complexity of the operation, risk of trauma, high incidence of postoperative complications, poor quality of life of patients after surgery, and other difficulties, these surgeries are not easily consented by patients, which also puts the medical staff in a difficult position. With the recent development of minimally invasive endoscopic treatment technologies, such as endoscopic submucosal dissection (ESD), endoscopic muscularis excavation, and endoscopic full-thickness resection, endoscopic treatment has become increasingly popular, which brings hope for the use of minimally invasive treatment of duodenal SELs in the future.
However, endoscopic resection of duodenal SELs is still regarded as a challenging procedure due to a high risk of perforation. The incidence of perforations in duodenal ESD has been reported to range from 6.7%-36.6% during the procedure and 0%-14.3% during the postoperative period[1,4-7]. Management of perforations after endoscopic removal of duodenal SELs is particularly challenging. However, this may be achieved by using over-the-scope clips (OTSCs). An OTSC was developed as an endoscopic full-thickness gastrointestinal closure device and has become one of the treatment options for gastrointestinal perforation because it is less invasive compared to conventional surgical closure. At present, there are few reports on endoscopic resection of duodenal SELs and endoscopic methods for the management of perforations[1,2,8,9]. To explore further this area, this study aimed to assess the effectiveness and safety of OTSCs in the treatment of perforation after endoscopic resection of duodenal SELs.
This was a retrospective study and was approved by the ethics committee of Taizhou Hospital of Zhejiang Province (Linhai, China). The study included 18 consecutive patients who were treated with OTSCs to close perforations that resulted after endoscopic resection of duodenal SELs, from May 2015 to November 2019. Patients were recruited if they met all of the following criteria: (1) Patients with duodenal SELs diagnosed by computed tomography and endoscopic ultrasound (EUS) with a high-frequency miniprobe (UM-2R, 12 MHz; UM-3R, 20 MHz, Olympus Optical, Tokyo, Japan); (2) Patients who underwent endoscopic resection of duodenal SELs and had intraoperative or postoperative perforations; (3) The duodenal perforation was closed using an OTSC; and (4) Patients who were able to tolerate general anesthesia and had no blood coagulation disorders prior to the procedure.
Before the endoscopic procedure, informed consent was obtained from all 18 patients. Patients were also informed that an OTSC might be used, and surgical intervention might be required in case of unsuccessful resection of the lesion or the occurrence of severe complications that cannot be successfully managed by endoscopic methods and conservative treatment.
The main outcome measurements were as follows: (1) The rate of complete closure of intraprocedural perforation; (2) Delayed perforation rate; and (3) Postoperative infection rate. All endoscopic resection procedures were performed by an experienced endoscopist in a sterile operating room while the patients were under general anesthesia with tracheal intubation.
The main equipment and accessories used were as follows: A single-accessory channel endoscope (Q260J; Olympus) with a transparent cap (ND-201-11802; Olympus) attached to its tip, an argon plasma coagulation unit (APC 300; ERBE, Tübingen, Germany), a high-frequency electronic cutting device (ICC 200; ERBE), a hook knife (KD-620LR; Olympus), an insulated-tip knife (KD-611L, IT2; Olympus), hot biopsy forceps (FD-410LR; Olympus), foreign body forceps (FG-B-24, Kangjin, Changzhou, China), a snare (SD-230U-20; Olympus), a carbon dioxide insufflator (Olympus), twin graspers (Ovesco Endoscopy AG, Tuebingen, Germany), an OTSC (12/6 t-type, Ovesco Endoscopy AG,), a titanium clip (HX-600-135; Olympus and M00522600), and endoloop (Leo Medical Co., Ltd, Changzhou, China).
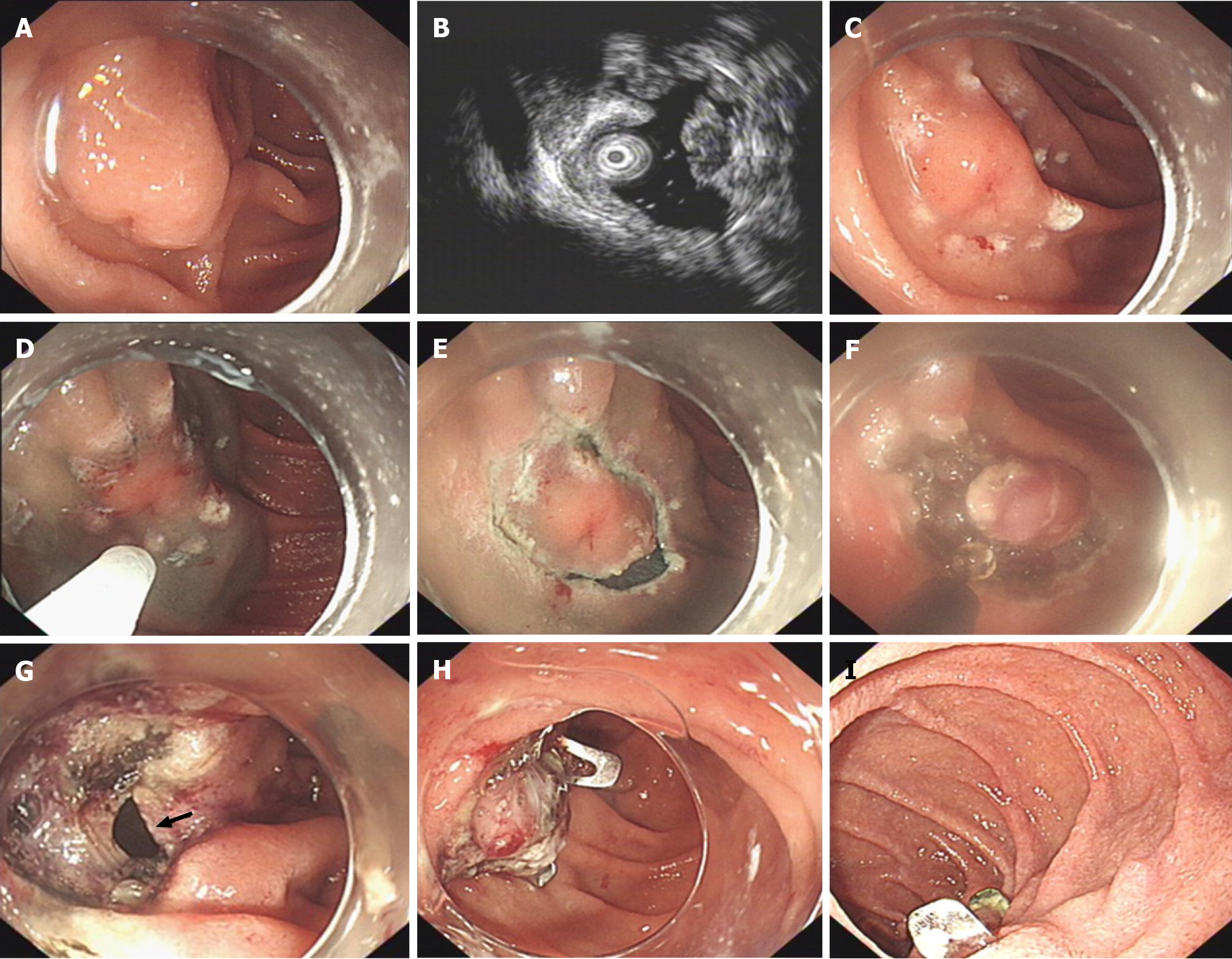
Endoscopic resection was performed as follows (Figure 1): (1) Several marking dots were initially made around the lesion using a needle-knife to define the border; (2) A submucosal elevation was made by injection of solution (100 mL saline plus 1 mL epinephrine and 2 mL indigo carmine); (3) Subsequently, the mucosa was incised with a hook knife outside the border to reveal the lesion; (4) A circumferential excavation was made as deep as the submucosa or muscularis propria layer around the lesion using an insulated tip knife; (5) After the lesion was completely resected, it was removed using a snare or foreign body forceps; and (6) Duodenal tissues adjacent to the perforation were clamped with twin graspers and then drawn into the transparent cap of the OTSC device until they were fully inhaled into the transparent cap following which the OTSC closure system was released to close the wound. If defect closure was not complete, several clip and/or endoloops were used to close the remaining portions. The mucosa defect was closed with several clips in a ‘side to center’ manner, and an endoloop was placed to trap all the clips. Finally, the endoloop was slowly tightened, and all the clips were tied together with the endoloop[8].
After the operation, all patients were treated with postoperative fasting, gastro
Every patient underwent follow-up endoscopies to monitor wound healing at 3 mo and 6 mo after endoscopic resection. EUS was performed to check for residual lesions after 3 mo. Patients with potentially malignant lesions, such as neuroendocrine tumors and GISTs, were monitored by endoscopy and/or EUS to detect recurrent lesions, and abdominal US and/or computed tomography to detect distant metastasis every 12 mo.
Data were analyzed using SPSS software (version 20.0; SPSS Inc., Armonk, NY, United States). Descriptive statistics were used for this study. The median was used for variables with a skewed distribution, while the mean was used in the case of a normal distribution of variables. Enumeration data are expressed as case numbers and percentages (%).
Patient information is summarized in Table 1 and therapeutic outcomes, are described in Table 2. The rate of successful en bloc resection was 100%. The vertical and horizontal margins of all specimens were tumor-free. Thus, the complete resection rate was 100%.
| Patients | |
| Median age, yr (range) | 53.5 (29-74) |
| Gender | |
| Male | 8 (44.4) |
| Female | 10 (55.6) |
| Symptom | |
| Upper abdominal pain | 3 (16.7) |
| Abdominal distention | 4 (22.2) |
| Melena | 5 (27.8) |
| Asymptomatic | 6 (33.3) |
| Lesions | |
| Median size, cm (range) | 2.0 (1.3-5.0) |
| Location of lesion | |
| Duodenal bulb | 11 (61.1) |
| Descending junction of duodenal bulb | 4 (22.2) |
| Descending duodenum | 3 (16.7) |
| Origination of lesion | |
| Submucosal layer | 9 (50.0) |
| Muscularis propria layer | 9 (50.0) |
| Therapeutic outcome and adverse events | |
| Complete resection | 18 (100) |
| Histology diagnosis | |
| Brunner’s adenoma | 1 (5.6) |
| Heterotopic pancreas | 7 (38.9) |
| GIST | 7 (38.9) |
| Very low risk | 1 (5.6) |
| Low risk | 6 (33.3) |
| Neuroendocrine tumors | 3 (16.6) |
| Complication | |
| Delayed perforation | 0 (0) |
| Delayed bleeding | 0 (0) |
| Postoperative infection | 7 (38.9) |
| Mean time of diet recovery after the procedure, d (range) | 6.5 (2-14) |
| Mean hospital stay after the procedure, d (range) | 9.5 (4-18) |
| Median follow-up period, mo (range) | 27 (15-66) |
All 18 patients had intraoperative perforations. The median perforation size was 1 cm in diameter (range, 0.5-3.0 cm). The wound was closed with an OTSC in 6 cases, an OTSC + a titanium clip in 1 case, and an OTSC + a titanium clip + an endoloop in 5 cases. The rate of successful intraprocedural perforation closure was 100%.
Seventeen patients had minor intraoperative bleeding. The remaining 1 patient, who had a tumor originating from the lamina propria, growing mainly out of the lumen, with rich blood supply, had considerable amount of bleeding during the procedure. All patients were treated with hot biopsy forceps to achieve hemostasis during the procedure.
None of the patients developed delayed bleeding or perforation. Seven patients had postoperative abdominal infections and were administered intensive antibiotic therapy. Among the 7 patients, 1 patient developed an abscess in the right iliac fossa that improved after puncture and drainage, while another patient developed septic shock and received peritoneal lavage and underwent distal subtotal gastrectomy with duodenal bulb resection. All 18 patients recovered and were discharged. The mean time taken to resume normal diet after the procedure was 6.5 d. The mean postoperative hospital stay was 9.5 d.
The median follow-up period after the procedure was 27 mo (range, 15-66 mo). No residual or recurrent lesions, duodenal stenosis, or adhesions were detected during the follow-up period in any of the patients.
Currently, endoscopic resection of duodenal SELs is a challenging procedure with a high risk of perforation. Published studies about endoscopic resection of duodenal SELs and endoscopic methods for management of perforations are limited[1,2,8,9]. In this study, we used OTSCs to close perforations in 18 patients. The rate of complete removal of duodenal SELs and successful perforation closure was 100%. No delayed bleeding or perforation occurred in any of the patients. This suggests that the use of OTSCs can effectively close perforations following endoscopic resection of duodenal SELs when performed by an experienced endoscopist.
The clinical manifestations of duodenal SELs are nonspecific and related to the location, size, growth pattern, presence of mucosal ulcers, and invasion or compression of adjacent organs. Most duodenal lesions have no symptoms and are usually found incidentally during endoscopic examinations. Clinical symptoms such as gastrointestinal bleeding, abdominal pain, and abdominal distention may occur when the lesion is very large or when an ulcer develops on the surface of the lesion.
Though most duodenal SELs, such as lipomas, Brunner’s adenomas, heterotopic pancreas, and cysts, are benign, some including neuroendocrine tumors and GISTs are potentially malignant[1-3]. Endoscopy and EUS are of great value in the diagnosis of duodenal SELs; however, they may be difficult to diagnose on some occasions. Patients with duodenal SELs can be monitored by endoscopy, especially for asymptomatic tumors that lack high-risk features as identified by EUS[10]. However, surveillance using only endoscopy may increase the risk of delayed diagnosis of a malignancy[11]. Furthermore, the difficulty of the operation and risk of combined evisceration will increase if the lesion is large. In such cases, removal of the lesion is inevitable.
Traditional surgical approaches for duodenal lesions, including pancreatoduodenectomy and limited resection, are traumatic and may result in serious complications, such as bleeding, perforation, and infection. Considering these potential risks associated with surgical therapy, endoscopic treatment is used as an alternative choice, which may be safer, more effective, and is minimally invasive. However, endoscopic resection of duodenal SELs is still considered to be a challenging procedure because the duodenal lumen is narrow and the initial part (ball to lower part) is an anti-c loop, which renders the endoscope unstable. Moreover, the abundant blood vessels and Brunner glands in the submucosa of the duodenum make it difficult to lift the mucosa after injection. In addition, compared to other parts of the gastrointestinal tract, the muscularis propria layer of the duodenum is soft and thin, and the posterior wall lacks the serosal layer; therefore, perforation can occur easily during or after the endoscopic resection of duodenal lesions, especially duodenal SELs[8]. The incidence of intraprocedural perforations in duodenal ESD has been reported to range from 6.7%-36.6%, and is 0%-14.3% in delayed perforations[1,4-7]. Moreover, emergency operations have been performed in 3.3%-25.0% of patients due to intraprocedural uncontrollable perforation or delayed perforation[1,4-7]. Our previous study reported that the perforation rate of endoscopic resection of duodenal SELs in our hospital was 7.4%[8].
Perioperative perforation associated with endoscopic therapy was previously considered a serious complication that usually requires surgery. With the development of endoscopic suture instruments and techniques, patients with iatrogenic gastrointestinal perforation can be successfully managed using endoscopic methods and conservative treatment without surgical intervention[12,13]. Thus, most perforations related to endoscopic treatment are no longer life-threatening complications. However, endoscopic closure of perforations after endoscopic resection of duodenal SELs remains a great challenge.
In the past, titanium clips were used for endoscopic closure of gastrointestinal perforations, especially for small acute perforations (< 5 mm). However, a titanium clip has a narrow wingspan and lacks the ability to approximate adequately the margins of the defect. Consequently, the rate of leakage after repairing a large perforation of more than 1 cm is high as the seal is confined to the surface rather than the full-thickness of the mucosa[14-16]. An OTSC has a greater holding strength[16,17]; it can clamp the entire wall of the lumen and grasp more tissue. The design can manage full-thickness perforations with diameters of up to 3 cm[14]. Moreover, the gap between the teeth of an OTSC allows blood to pass through to avoid tissue necrosis. The advantage of an OTSC lies in its ease of use, ability to close defects between 1 and 3 cm with a single clip, and safety, which allows endoscopists to deal effectively with acute perforations immediately after identification[18]. Thus, OTSCs are easy to operate and can effectively shorten operation times. Moreover, The European Society of Gastrointestinal Endoscopy recommends OTSCs for endoscopic closure of iatrogenic perforations[18]. According to a systematic review, the success rate of using OTSCs to manage perforations was 85.3%, while 9.4% of patients still required surgical intervention after an OTSC placement to achieve complete closure[19]. Voermans et al[14] reported 12 cases of duodenal perforation that were treated with OTSCs, nine of which were effectively closed, with an overall success rate of 75%. In our study, the rate of successful closure of intraprocedural perforations was 100%. However, we have also used a titanium clip in 1 case and a titanium clip along with an endoloop in 5 cases. It seems that if the perforation is larger than 1.5 cm, using an OTSC alone may fail to achieve complete closure. We speculate that the combination of OTSC, titanium clip, and endoloops may be more effective. Given that the duodenal lumen is narrow, caution should be exercised to avoid grasping too much tissue to avoid further narrowing of the lumen while deploying the OTSC in the duodenum. In our study, no duodenal stenosis was detected in any patient during the follow-up period.
The duodenum is exposed to pancreatic juices and bile, causing delayed perforations more likely to occur after endoscopic resection of duodenal lesions. Complete closure of the wound facilitates prevention of delayed perforation[6,7,17]. Due to its the strong tightening force and the gap between its teeth, an OTSC can manage to close full-thickness duodenal perforations and avoid tissue necrosis, which effectively reduces the occurrence of delayed perforations. A carbon dioxide pump is also recommended to use with endoscopic treatment, especially when a perforation occurs. The use of gastrointestinal decompression after endoscopic closure of perforation is helpful for the absorption of gas and liquid in the intestinal cavity. It also reduces tension in the wound, and promotes wound healing, which can reduce the incidence of delayed perforations. In this study, we placed a jejunal nutrition tube next to the wound and a gastrointestinal decompression tube to extract gas and digestive juice. Thereafter, none of the patients developed delayed perforations.
The duodenum is an interperitoneal organ, most of which is located in the retroperitoneum. After perforation or full-thickness resection, digestive fluid from the duodenum (mainly bile and pancreatic juice) flows into the peritoneal cavity or retroperitoneal cavity, which may cause serious abdominal or retroperitoneal infection. In our study, 7 patients (38.9%) had postoperative abdominal infection, including 1 who developed an abscess in the right iliac fossa and another who developed septic shock. Severe infection in the 2 cases were considered to be caused by long operation times and large amounts of digestive juice entering the abdominal cavity. Timely conversion of the endoscopic procedure to surgery or combining with laparoscopy when the resection is found to be difficult may help avoid such complications.
Due to their strong holding strength, OTSCs are more difficult to detach spontaneously from the mucosa than normal titanium clips. The OTSC is made of nitinol, which has favorable biocompatibility. Thus, this device is considered a permanent implanted material. However, OTSCs should be removed in the following circumstances: (1) Poor healing; (2) OTSC misplacement; (3) Repeat biopsy/therapy or further treatment; (4) Adverse events after OTSC implantation, such as ulcers and stenosis of the digestive tract; (5) Removal after recovery; and (6) Patient’s wishes[20]. In our study, there were no such indications for removal. During the follow-up period, OTSCs detached spontaneously in most cases.
This study has a few limitations. First, this was a single-center retrospective study and the sample size was relatively small; therefore, selection bias may have been present. Second, since this was a retrospective study, it lacked randomized and control samples. Third, our institution is a tertiary endoscopic center in Zhejiang Province where the procedures were performed by an experienced operator; thus, the results of this study may not be applicable to all other endoscopic centers.
Closing of perforations after endoscopic resection of duodenal SELs with OTSCs is an effective and reasonably safe therapeutic method. However, this procedure should be performed by an experienced endoscopic team. If the endoscopic procedure fails or the postoperative complications are difficult to manage, the patient should be planned to undergo surgery immediately.
Currently, endoscopic resection of duodenal subepithelial lesions (SELs) is a challenging procedure with a high risk of perforation.
It is importance to deal with perforation after endoscopic resection of duodenal SELs. However, so far, there were few reports on endoscopic methods for management of perforations.
We aim to evaluate the effectiveness and safety of over-the-scope clip (OTSC) in the closing the perforation after endoscopic resection of duodenal SELs.
This was a retrospective study. We collected data of 18 consecutive patients who were treated with OTSCs to close the perforation after endoscopic resection of duodenal SELs and analyzed the rate of complete resection, closure of intraprocedural perforation, delayed bleeding, delayed perforation, and postoperative infection.
All the perforations after endoscopic resection of duodenal SELs were successfully closed. No delayed bleeding or perforation occurred in any of the patients.
OTSC can effectively and safely close the perforations after endoscopic resection of duodenal SELs by an experienced endoscopist.
We need to expand the sample size to confirm further the effectiveness and safety of OTSC in closing the perforation after endoscopic resection of duodenal SELs. In addition, the long-term outcome of OTSC should be observed by extending the follow-up time.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Masaki S, Seicean A S-Editor: Gao CC L-Editor: Filipodia P-Editor: Liu JH
| 1. | Matsumoto S, Miyatani H, Yoshida Y. Endoscopic submucosal dissection for duodenal tumors: a single-center experience. Endoscopy. 2013;45:136-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Musumba C, Sonson R, Tutticci N, Nanda K, Bourke MJ. Endoscopic submucosal dissection of a duodenal neuroendocrine tumor. Gastrointest Endosc. 2014;79:716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Xu GQ, Wu YQ, Wang LJ, Chen HT. Values of endoscopic ultrasonography for diagnosis and treatment of duodenal protruding lesions. J Zhejiang Univ Sci B. 2008;9:329-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Hoteya S, Yahagi N, Iizuka T, Kikuchi D, Mitani T, Matsui A, Ogawa O, Yamashita S, Furuhata T, Yamada A, Kimura R, Nomura K, Kuribayashi Y, Kaise M. Endoscopic submucosal dissection for nonampullary large superficial adenocarcinoma/adenoma of the duodenum: feasibility and long-term outcomes. Endosc Int Open. 2013;1:2-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Jung JH, Choi KD, Ahn JY, Lee JH, Jung HY, Choi KS, Lee GH, Song HJ, Kim DH, Kim MY, Bae SE, Kim JH. Endoscopic submucosal dissection for sessile, nonampullary duodenal adenomas. Endoscopy. 2013;45:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 104] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 6. | Nonaka S, Oda I, Tada K, Mori G, Sato Y, Abe S, Suzuki H, Yoshinaga S, Nakajima T, Matsuda T, Taniguchi H, Saito Y, Maetani I. Clinical outcome of endoscopic resection for nonampullary duodenal tumors. Endoscopy. 2015;47:129-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Yamamoto Y, Yoshizawa N, Tomida H, Fujisaki J, Igarashi M. Therapeutic outcomes of endoscopic resection for superficial non-ampullary duodenal tumor. Dig Endosc. 2014;26 Suppl 2:50-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 89] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 8. | Ye LP, Mao XL, Zheng HH, Zhang Y, Shen LY, Zhou XB, Zhu LH. Safety of endoscopic resection for duodenal subepithelial lesions with wound closure using clips and an endoloop: an analysis of 68 cases. Surg Endosc. 2017;31:1070-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Schmidt A, Bauder M, Riecken B, von Renteln D, Muehleisen H, Caca K. Endoscopic full-thickness resection of gastric subepithelial tumors: a single-center series. Endoscopy. 2015;47:154-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, Pisters PW, Raut CP, Riedel RF, Schuetze S, Sundar HM, Trent JC, Wayne JD. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw. 2010;8 Suppl 2:S1-41; quiz S42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 826] [Cited by in RCA: 822] [Article Influence: 54.8] [Reference Citation Analysis (0)] |
| 11. | Białek A, Wiechowska-Kozłowska A, Pertkiewicz J, Polkowski M, Milkiewicz P, Karpińska K, Ławniczak M, Starzyńska T. Endoscopic submucosal dissection for treatment of gastric subepithelial tumors (with video). Gastrointest Endosc. 2012;75:276-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 131] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 12. | Yoshizumi F, Yasuda K, Kawaguchi K, Suzuki K, Shiraishi N, Kitano S. Submucosal tunneling using endoscopic submucosal dissection for peritoneal access and closure in natural orifice transluminal endoscopic surgery: a porcine survival study. Endoscopy. 2009;41:707-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Guo J, Liu Z, Sun S, Liu X, Wang S, Ge N, Wang G, Qi Y. Endoscopic full-thickness resection with defect closure using an over-the-scope clip for gastric subepithelial tumors originating from the muscularis propria. Surg Endosc. 2015;29:3356-3362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 71] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 14. | Voermans RP, Le Moine O, von Renteln D, Ponchon T, Giovannini M, Bruno M, Weusten B, Seewald S, Costamagna G, Deprez P, Fockens P; CLIPPER Study Group. Efficacy of endoscopic closure of acute perforations of the gastrointestinal tract. Clin Gastroenterol Hepatol. 2012;10:603-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 154] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 15. | Verlaan T, Voermans RP, van Berge Henegouwen MI, Bemelman WA, Fockens P. Endoscopic closure of acute perforations of the GI tract: a systematic review of the literature. Gastrointest Endosc. 2015;82:618-28.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 79] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 16. | Singhal S, Changela K, Papafragkakis H, Anand S, Krishnaiah M, Duddempudi S. Over the scope clip: technique and expanding clinical applications. J Clin Gastroenterol. 2013;47:749-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Mori H, Shintaro F, Kobara H, Nishiyama N, Rafiq K, Kobayashi M, Nakatsu T, Miichi N, Suzuki Y, Masaki T. Successful closing of duodenal ulcer after endoscopic submucosal dissection with over-the-scope clip to prevent delayed perforation. Dig Endosc. 2013;25:459-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Paspatis GA, Dumonceau JM, Barthet M, Meisner S, Repici A, Saunders BP, Vezakis A, Gonzalez JM, Turino SY, Tsiamoulos ZP, Fockens P, Hassan C. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2014;46:693-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 186] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 19. | Bartell N, Bittner K, Kaul V, Kothari TH, Kothari S. Clinical efficacy of the over-the-scope clip device: A systematic review. World J Gastroenterol. 2020;26:3495-3516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 67] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (6)] |
| 20. | Ou YH, Kong WF, Li LF, Chen PS, Deng SH, He FJ, Peng QQ, Yue H. Methods for Endoscopic Removal of Over-the-Scope Clip: A Systematic Review. Can J Gastroenterol Hepatol. 2020;2020:5716981. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |