Published online Mar 21, 2016. doi: 10.3748/wjg.v22.i11.3296
Peer-review started: November 4, 2015
First decision: November 27, 2015
Revised: December 28, 2015
Accepted: January 9, 2016
Article in press: January 11, 2016
Published online: March 21, 2016
Processing time: 131 Days and 17.9 Hours
Primary esophageal or gastric melanoma is a very rare disease with early metastasis. Due to its atypical symptom and less efficiency of chemotherapy and radiotherapy, the prognosis of esophageal or gastric melanoma is still very poor. Surgical resection remains the preferential treatment for esophageal or gastric melanoma. Here we present an extremely rare case of primary advanced esophago-gastric melanoma. Debulking surgery was performed without chemotherapy or radiotherapy. However, abdominal recurrence and hepatic metastases were found within one month by a postoperative follow-up computed tomography. Three and a half months after surgical resection, the patient died of extensive abdominal metastasis.
Core tip: Primary malignant digestive melanoma is a very rare disease with poor prognosis. Here we report an extremely rare and advanced case of primary esophago-gastric melanoma. Although the effect of combination strategy of surgical resection with chemotherapy or radiotherapy is still unclear, we strongly recommend a postoperative chemotherapy or radiotherapy due to the fast progression and extremely short survival of our case.
- Citation: Wang L, Zong L, Nakazato H, Wang WY, Li CF, Shi YF, Zhang GC, Tang T. Primary advanced esophago-gastric melanoma: A rare case. World J Gastroenterol 2016; 22(11): 3296-3301
- URL: https://www.wjgnet.com/1007-9327/full/v22/i11/3296.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i11.3296
Primary esophageal or gastric melanoma is an extremely rare disease in the digestive system. Baur firstly reported primary esophageal melanoma in 1906[1]. So far, a total of 369 cases of primary esophageal melanoma and 19 cases of primary gastric melanoma have been reported worldwide. The annual incidence of primary esophageal melanoma is around 0.02-0.036 per million populations[2,3], but there are no reported data regarding the incidence of primary gastric melanoma. Barely 15% of all melanomas are encountered in non-cutaneous sites and only 20% of these non-cutaneous melanomas originate from the mucosa[3] and with less than 0.5% of mucosal melanoma arising from the esophagus, ranging from 0.1% to 0.2% of all esophageal malignancies[4,5]. Herein, we report an extremely rare case of primary advanced esophago-gastric melanoma in an attempt to share our experience in treating this case and propose the possible useful treatment strategy.
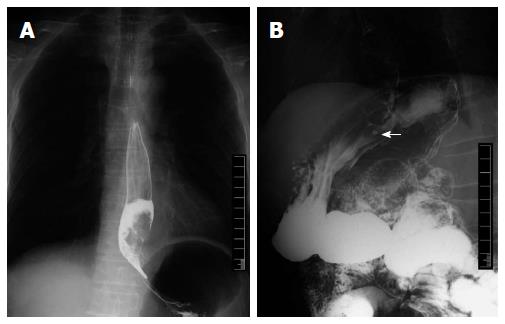
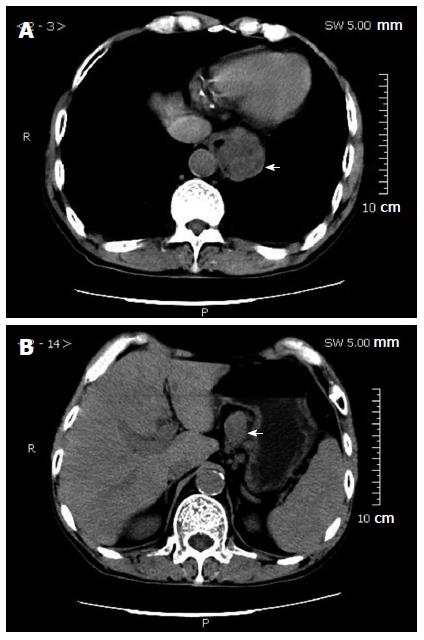
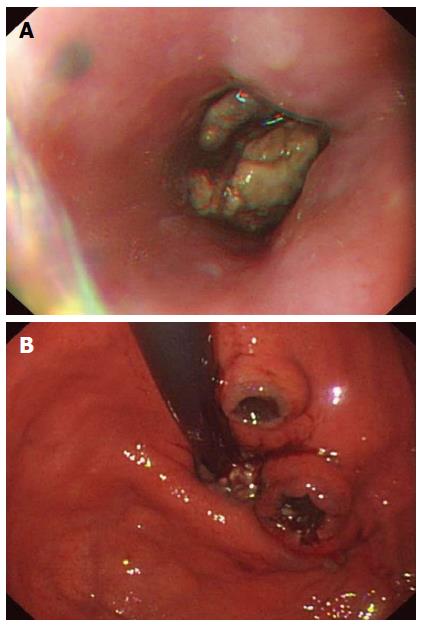
A 65-year-old man was admitted to the China-Japan Friendship hospital with a chief complaint of progressive dysphagia for 3 mo. He also complained of a drastic weight loss of 8 kg in the past 2 mo. He denied a history of smoking, alcohol intake and substance abuse, but had a chronic atrophic gastritis for nearly 10 years. Also, there was no family history of genetic defect or malignancy. Physical examination showed no palpable findings. Admission blood test showed a slight decrease in hemoglobin (106 g/L). Upper gastrointestinal (GI) examination using barium contrasts showed a large tumor blocking the esophago-gastric junction (Figure 1). Computed tomography (CT) scan revealed a soft mass in the esophago-gastric junction with lymph node metastasis in the lesser curvature of the stomach (Figure 2). Endoscopic examination showed a black spot in the lower esophagus and a bulky black mass blocking the esophago-gastric junction, as well as two black crater-like ulcers in the fundus of the stomach (Figure 3). Biopsy specimens taken from the tumor were identified as poorly differentiated adenocarcinoma. Preoperative nutrition status of this case was scored 2 based on the Nutrition Risk Screening 2002 (NRS 2002)[6].
Because of the obstructive symptom caused by the tumor, a debulking surgery of distal esophagectomy and proximal gastrectomy was performed. Esophagogastric anastomosis and reconstruction was then completed with stapling device. Intraoperatively, the tumor was found located at the esophago-gastric junction and the tumor infiltrated the whole layer with lymph node metastasis at station four. No ascites or dissemination of the tumor was observed in the peritoneal cavity.
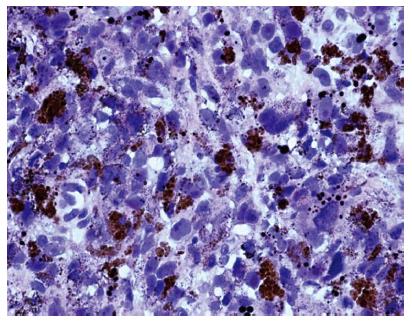
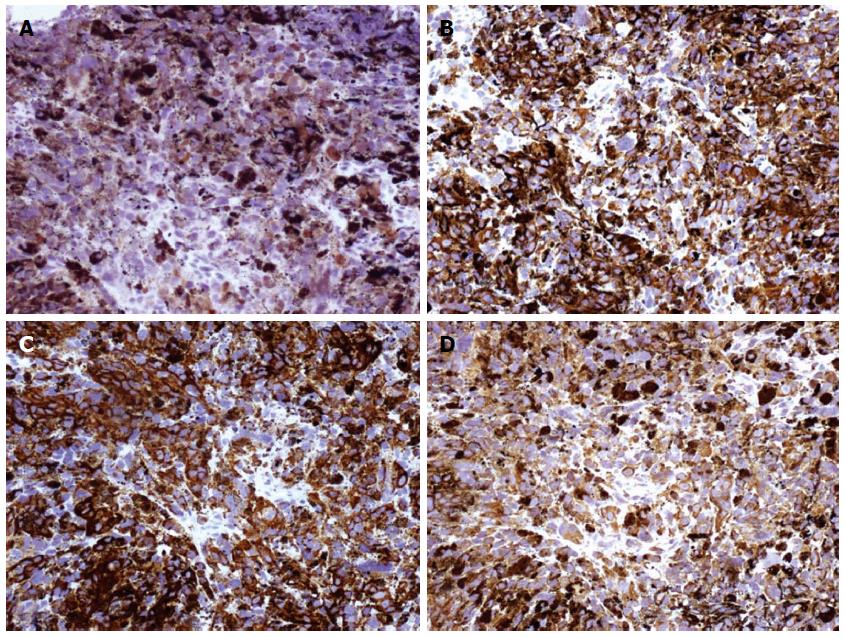
The tumor measured 3 cm × 6 cm in size with black pigmentation (Figure 4). There were several pigmented satellite nodules beside the main tumor lesion, the largest one being 1 cm × 1 cm in diameter. Moreover, two ulceration lesions were found at the fundus of the stomach. Microscopically, the excised tumor tissue was composed of non-organized and pleomorphic cells exhibiting atypical nuclei, and abundant melanin granules (Figure 5). Pathological examination identified this case at a stage of IVA (T4aN1M0). Immunohistochemical staining showed that the tumor was positive for S-100, HMB-45, mclean-A and Vimentin, but negative for cytokeratin 7 and cytokeratin 20 (Figure 6). Based on these results, a diagnosis of primary advanced esophago-gastric melanoma was established.
The postoperative course was smooth and without complications. The patient gradually recovered and was discharged 14 d after surgery. As the patient denied a postoperative adjuvant therapy, abdominal recurrence and hepatic metastases were found within one month by a postoperative follow-up CT. No other effective treatment was administered afterwards. The patient died of diffuse metastatic disease 2 mo later.
To date, little is known about the exact etiology of esophageal or gastric melanoma, and no definite risk factors have been identified[7]. At the time of initial diagnosis, detectable metastases are present in 30%-40% of patients[2]. The incidence of metastasis to regional lymph nodes is as high as 40%-80%, and the most common sites are periesophageal, mediastinal and celiac lymph nodes[8,9]. The hematogenous dissemination is most prone to the liver, lung and brain[10]. In 2009, AJCC introduced a new classification for melanoma of the upper aerodigestive tract[11]. In this classification, T1 and T2, Stage I and Stage II are omitted due to the aggressive nature of mucosal melanomas (Table 1 and Table 2). Based on this classification, our case was identified with a stage of IVA (T4aN1M0).
| T | Tx | Tumor cannot be evaluated |
| T0 | No signs of tumor | |
| T3 | Epithelium/submucosa (mucosal disease) | |
| T4a | Deep soft tissue, cartilage, bone or overlying skin | |
| T4b | Brain, dura, skull base, lower cranial nerves, masticator space, carotid artery, prevertebral space, mediastinal structures, cartilage, skeletal muscle or bone | |
| N | Nx | Regional lymph nodes cannot be evaluated |
| N0 | Tumor cells absent from regional lymph nodes | |
| N1 | Regional lymph node metastasis present | |
| M | M0 | No distant metastasis |
| M1 | Metastasis to distant organs |
| AJCC staging | |||
| Stage III | T3 | N0 | M0 |
| Stage IVA | T4a | N0 | M0 |
| T3,T4a | N1 | M0 | |
| Stage IVB | T4b | Any N | M0 |
| Stage IVC | Any T | Any N | M1 |
Due to the rarity of the disease, no standard treatment has been established so far. Surgical resection and a combination of different adjuvant therapies are reasonable options, and the choice of treatment should be individualized for each patient. Due to the tendency of the tumor to spread longitudinally along the submucosa, some authors stated that a greater capacious safety margin of resection was necessary[12]. The median overall survival associated with primary malignant melanoma of the GI tract is reportedly 17 mo, whereas that associated with primary gastric melanoma is only 5 mo[13], and the mean survival time is 9-14.2 mo after surgical resection of primary esophageal melanoma[14].
The curative effects of chemotherapy are not satisfactory for malignant melanoma, and the long-term survival is poor on the whole, so it does not seem to have a major role in the management of this disease[2]. Local application of INF-β alone or combined with systemic chemotherapy was tried and found to be effective[14]. The gene mutation of BARF, NRas and KIT in the MAPK pathway has been the focus of eager investigation as novel therapeutic targets with medications[15], such as sorefenib, farnesyltransferase inhibitor and imatinib. Moreover, various kinds of vaccines against cancer-testis (CT) antigens for treatment of melanoma, such as dendritic-cell vaccine, were explored[16]. Survivin is strongly expressed in melanoma and appears to be involved in melanocyte resistance to some agents, so the survivin inhibitor of YM-155 may be considered as a potential option[17].
Radiotherapy has been tried to treat this disease for many years, however, most researchers believed that melanoma was non-sensitive to radiation or with little benefits[18,19], so radiotherapy merely plays a palliative role, such as palliating the symptom of dysphagia with large tumors or reducing the probability of relapse after operation. Furthermore, heavy-ion radiation[20], radiotherapy combined with hyperthermia[21] and intraluminal brachytherapy are also administered in sporadic cases and demonstrate good initial responses.
In short, the aggressive biological behavior, the advanced stage and lack of effective therapy contribute to the poor prognosis of melanomas of the upper digestive system. Here we reported our experience in treating this rare case of primary advanced malignant melanoma in esophago-gastric junction. Debulking surgery was performed alone without chemotherapy or radiotherapy. However, abdominal recurrence and hepatic metastases were found within one month by a postoperative follow-up CT. Finally the patient died of diffuse metastatic disease two months later. Although the effect of combination therapy of surgical resection with chemotherapy or radiotherapy is still unclear, we strongly recommend a postoperative chemotherapy or radiotherapy due to the fast progression and extremely short survival of our case.
We thank Dr. Masanobu Abe (Division for Health Service Promotion, University of Tokyo Hospital, Tokyo, Japan) for discussing about the combination therapy of malignant melanoma.
A 65-year-old man with a chief complaint of progressive dysphagia for 3 mo.
Physical examination showed no palpable findings.
Melanocytosis, distal esophageal cancer, cardiac cancer and proximal stomach cancer.
Hemoglobin 106 g/L.
Upper gastrointestinal (GI) barium examination, computed tomography and endoscopy showed a soft mass involving the esophago-gastric junction, with swelling lymph nodes in the lesser curvature of the stomach.
Preoperative biopsy suggested the presence of poorly differentiated adenocarcinoma, and postoperative immunohistochemical staining showed that the tumor was positive for S-100, HMB-45, mclean-A and Vimentin, and negative for cytokeratin 7 and cytokeratin20.
A debulking surgery of distal esophagectomy and proximal gastrectomy was performed, and esophagogastric anastomosis and reconstruction was performed using stapling device, with no postoperative adjuvant therapy.
There are few reports of primary esophageal or gastric melanoma treated with multidisciplinary strategies including surgery and a combination of different adjuvant therapies, such as chemotherapy, radiotherapy and immunotherapy. Thus, the data were insufficient to help achieve a long-term survival in a highly advanced malignant melanoma of the upper digestive tract.
To control the highly aggressive biologic behavior and tendency to metastasis is the key to treatment of melanoma of the GI tract; surgical resection and a combination of different adjuvant therapies are reasonable options.
This is a report of an extremely uncommon case of esophago-gastric melanoma with an interesting finding, and it will definitely contribute to the quite scarce literature regarding the primary melanoma of the GI tract.
P- Reviewer: Mazzocchi M, Zielinski J S- Editor: Yu J L- Editor: A E- Editor: Liu XM
| 1. | Baur EH. Ein Fall von primarem melanom des esophagus. Arb Geb Pathol Anat Inst Tubingen. 1906;5:343-354. |
| 2. | Sabanathan S, Eng J, Pradhan GN. Primary malignant melanoma of the esophagus. Am J Gastroenterol. 1989;84:1475-1481. [PubMed] |
| 3. | Scotto J, Fraumeni JF, Lee JA. Melanomas of the eye and other noncutaneous sites: epidemiologic aspects. J Natl Cancer Inst. 1976;56:489-491. [PubMed] |
| 4. | Mills SE, Cooper PH. Malignant melanoma of the digestive system. Pathol Annu. 1983;18 Pt 2:1-26. [PubMed] |
| 5. | McCormack PM, Nascimento AG, Bains MS, Knapper WH, Zaman MB. Primary melanocarcinoma of the esophagus. Clin Bull. 1979;9:162-164. [PubMed] |
| 6. | Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22:321-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1485] [Cited by in RCA: 1741] [Article Influence: 79.1] [Reference Citation Analysis (0)] |
| 7. | Mihajlovic M, Vlajkovic S, Jovanovic P, Stefanovic V. Primary mucosal melanomas: a comprehensive review. Int J Clin Exp Pathol. 2012;5:739-753. [PubMed] |
| 8. | Lohmann CM, Hwu WJ, Iversen K, Jungbluth AA, Busam KJ. Primary malignant melanoma of the oesophagus: a clinical and pathological study with emphasis on the immunophenotype of the tumours for melanocyte differentiation markers and cancer/testis antigens. Melanoma Res. 2003;13:595-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Li B, Lei W, Shao K, Zhang C, Chen Z, Shi S, He J. Characteristics and prognosis of primary malignant melanoma of the esophagus. Melanoma Res. 2007;17:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Chalkiadakis G, Wihlm JM, Morand G, Weill-Bousson M, Witz JP. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1985;39:472-475. [PubMed] |
| 11. | Edge SB, Byrd DR, Carducci MA, Compton CC, Fritz AG, Greene F, Trotti A, editors . American Joint Comission on Cancer (AJCC): Cancer Staging Manual. 7th ed. New York: Springer 2009; . |
| 12. | Volpin E, Sauvanet A, Couvelard A, Belghiti J. Primary malignant melanoma of the esophagus: a case report and review of the literature. Dis Esophagus. 2002;15:244-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 86] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Cheung MC, Perez EA, Molina MA, Jin X, Gutierrez JC, Franceschi D, Livingstone AS, Koniaris LG. Defining the role of surgery for primary gastrointestinal tract melanoma. J Gastrointest Surg. 2008;12:731-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 93] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 14. | Sakamoto H, Uedo N, Iishi H, Higashino K, Ishihara R, Mitani K, Narahara H, Tatsuta M, Mano M, Ishiguro S. Treatment of primary malignant melanoma of the esophagus with endoscopic injection of interferon-beta combined with systemic chemotherapy: a case report. Gastrointest Endosc. 2003;57:773-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Langer R, Becker K, Feith M, Friess H, Höfler H, Keller G. Genetic aberrations in primary esophageal melanomas: molecular analysis of c-KIT, PDGFR, KRAS, NRAS and BRAF in a series of 10 cases. Mod Pathol. 2011;24:495-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Asakage M, Kitayama J, Tsuno NH, Komuro Y, Kaisaki S, Hori N, Nagawa H, Tsuno NH, Hori N, Takahashi K. Primary malignant melanoma of the esophagus treated by esophagectomy and adjuvant dendritic-cell therapy. J Gastroenterol. 2005;40:545-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Nakahara T, Kita A, Yamanaka K, Mori M, Amino N, Takeuchi M, Tominaga F, Hatakeyama S, Kinoyama I, Matsuhisa A. YM155, a novel small-molecule survivin suppressant, induces regression of established human hormone-refractory prostate tumor xenografts. Cancer Res. 2007;67:8014-8021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Fogarty GB, Tartaglia CJ, Peters LJ. Primary melanoma of the oesophagus well palliated by radiotherapy. Br J Radiol. 2004;77:1050-1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Joob AW, Haines GK, Kies MS, Shields TW. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1995;60:217-222. [PubMed] |
| 20. | Sudhamshu K C T, Matsutani S, Hishikawa E, Nikaido T, Taro A, Hiromitsu S. Primary malignant melanoma of the esophagus treated with heavy-ion radiotherapy. J Clin Gastroenterol. 2003;37:151-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Hulshof MC, Van Haaren PM, Zum Vörde Sive Vörding PJ, Krishnadath S, Marsman WA, Van Berge Henegouwen MI, Geijsen ED, Crezee J. Radiotherapy combined with hyperthermia for primary malignant melanomas of the esophagus. Dis Esophagus. 2010;23:E42-E47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |