Published online Jul 28, 2015. doi: 10.3748/wjg.v21.i28.8670
Peer-review started: January 14, 2015
First decision: March 26, 2015
Revised: April 8, 2015
Accepted: May 20, 2015
Article in press: May 21, 2015
Published online: July 28, 2015
Processing time: 197 Days and 7 Hours
AIM: To evaluate the efficacy and safety of the laparoscopic approaches for parastomal hernia repair reported in the literature.
METHODS: A systematic review of PubMed and MEDLINE databases was conducted using various combination of the following keywords: stoma repair, laparoscopic, parastomal, and hernia. Case reports, studies with less than 5 patients, and articles not written in English were excluded. Eligible studies were further scrutinized with the 2011 levels of evidence from the Oxford Centre for Evidence-Based Medicine. Two authors reviewed and analyzed each study. If there was any discrepancy between scores, the study in question was referred to another author. A meta -analysis was performed using both random and fixed-effect models. Publication bias was evaluated using Begg’s funnel plot and Egger’s regression test. The primary outcome analyzed was recurrence of parastomal hernia. Secondary outcomes were mesh infection, surgical site infection, obstruction requiring reoperation, death, and other complications. Studies were grouped by operative technique where indicated. Except for recurrence, most postoperative morbidities were reported for the overall cohort and not by approach so they were analyzed across approach.
RESULTS: Fifteen articles with a total of 469 patients were deemed eligible for review. Most postoperative morbidities were reported for the overall cohort, and not by approach. The overall postoperative morbidity rate was 1.8% (95%CI: 0.8-3.2), and there was no difference between techniques. The most common postoperative complication was surgical site infection, which was seen in 3.8% (95%CI: 2.3-5.7). Infected mesh was observed in 1.7% (95%CI: 0.7-3.1), and obstruction requiring reoperation also occurred in 1.7% (95%CI: 0.7-3.0). Other complications such as ileus, pneumonia, or urinary tract infection were noted in 16.6% (95%CI: 11.9-22.1). Eighty-one recurrences were reported overall for a recurrence rate of 17.4% (95%CI: 9.5-26.9). The recurrence rate was 10.2% (95%CI: 3.9-19.0) for the modified laparoscopic Sugarbaker approach, whereas the recurrence rate was 27.9% (95%CI: 12.3-46.9) for the keyhole approach. There were no intraoperative mortalities reported and six mortalities during the postoperative course.
CONCLUSION: Laparoscopic intraperitoneal mesh repair is safe and effective for treating parastomal hernia. A modified Sugarbaker approach appears to provide the best outcomes.
Core tip: Parastomal hernia is a common morbidity following stoma creation. Outcomes following repair of such hernias are relatively poor. Given the success of laparoscopy in repairing ventral hernia, we present the current laparoscopic options for repairing the defect.
- Citation: DeAsis FJ, Lapin B, Gitelis ME, Ujiki MB. Current state of laparoscopic parastomal hernia repair: A meta-analysis. World J Gastroenterol 2015; 21(28): 8670-8677
- URL: https://www.wjgnet.com/1007-9327/full/v21/i28/8670.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i28.8670
One of the most frequent complications following stoma formation is parastomal hernia (PH), which has been reported to occur in nearly half of patients within 2 years after repair. Risk factors for PH include obesity, steroid use, increased age, and increased intra-abdominal pressure[1-4]. While patients can be managed conservatively if they are asymptomatic, 30% to 70% will eventually require surgical intervention. Common indications for repair are pain, obstruction, incarceration, and stoma appliance discomfort[2,5,6]. Options for surgical repair include stoma relocation and onlay, sublay, or intraperitoneal mesh repair[7,8]. With the success of laparoscopic mesh repair for ventral hernia, such an approach has been applied for PH repair, and several groups have reported low morbidity and recurrence[3,9-16]. The two most cited minimally invasive techniques are the Keyhole (KH) and modified Sugarbaker (SB)[17-19]. This review discusses the current options for laparoscopic parastomal hernia repair and compares the outcomes for each. The primary focus was recurrence, and the secondary focus was morbidity postoperatively.
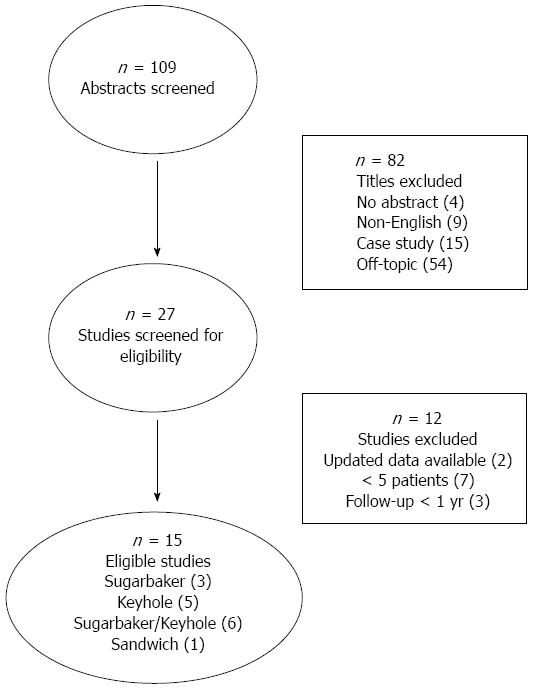
The search strategy used is detailed in Figure 1. MEDLINE and PubMed databases were queried for this review (January 1950-December 2014). The search terms used were various combinations of hernia, repair stoma, parastomal, ileostomy, colostomy, laparoscopic, Sugarbaker, non-slit, keyhole, slit, and mesh. References from other studies were cross-checked for more articles. Only papers published in English were included. For studies from the same author group, the most recent publication was chosen if the patient cohorts were overlapping. The exclusion criteria for our analysis were the following: no abstract available, case studies, experimental studies, cohort less than 5 patients, and unrelated topic. Articles were reviewed by two authors (FJD and MEG) using the 2011 levels of evidence from the Oxford Centre for Evidence-Based Medicine[20]. If there was any discrepancy between scores, the study in question was referred to another author (MBU).
The primary outcome analyzed was recurrence of parastomal hernia. Secondary outcomes were mesh infection, surgical site infection, obstruction requiring reoperation, death, and other complications. All studies were meticulously reviewed for eligibility. Publication year, study design, sample size, laparoscopic technique (Sugarbaker, keyhole, and sandwich), mesh type used, postoperative morbidity (mesh infection, surgical site infection, obstruction requiring reoperation, mortality, and other complications), and follow-up time were recorded. Studies were grouped by operative technique where indicated. Except for recurrence, most postoperative morbidities were reported for the overall cohort and not by approach so they were analyzed across approach. To increase sample size an overall complication rate was calculated as mesh infection, surgical site infection, obstruction requiring reoperation, other complications, or death.
Weighted pooled proportions with 95%CIs were generated for recurrence rates, mesh infection, surgical site infection, obstruction, other complications, mortality, and overall complication rates for each study reporting rates. The heterogeneity of each pooled estimate was assessed using the Cochran Qχ2 test and the I2 statistic. In cases with a significant Cochran’s Q test (P < 0.10) and an I2 > 50%, estimates were summarized using the DerSimonian[21] and Laird random-effects model. If significant heterogeneity was not found, a fixed-effects model was chosen for summary statistics.
Funnel plots and Egger’s regression test were used to assess the potential risk of publication bias. Statistical analyses were performed by a biostatistician using SAS 9.3 statistical software (SAS Institute, Cary, NC) and StatsDirect statistical software (StatsDirect Ltd, Altrincham, United Kingdom; http://www.statsdirect.com).
A query of Medline and PubMed databases using the aforementioned keywords yielded 108 possible studies. After initial screening, 25 full-length articles were retrieved for full assessment with our eligibility criteria as well as the Oxford levels of evidence. Upon assessment, 15 studies with a total of 469 patients were deemed eligible based on primary and secondary outcomes (Figure 1). Six studies reported results with both modified laparoscopic Sugarbaker and keyhole repair cohorts. For slit mesh Keyhole repair, there was a total of 231 patients from eleven studies. For non-slit mesh modified Sugarbaker repair, there were a total of 191 patients from nine studies. One study reported a sandwich two-mesh technique in a total of 47 patients. Eleven studies used only expanded polytetrafluoroethylene (ePTFE) mesh for repair, either Sugarbaker or keyhole[3,9,11-14,16,22-25]. One study used polypropylene mesh for keyhole repair and ePTFE for Sugarbaker repair[15]. One study used only polypropylene mesh for keyhole repair[25]. One study used a hybrid ePTFE-polypropylene mesh for keyhole repair[26]. One study used a dual layer polyvinylidene fluoride-polypropylene (PVDF-PP) mesh for sandwich repair[27]. For all repairs, the conversion rate was 3.1% (15 of 469). The primary reasons for this were bowel perforation and the presence of dense adhesions[13,22,28]. There were no intraoperative mortalities (Table 1).
| Reference | Year | Evidence level | Technique | No. of repairs | Overall complications | Mesh infection | Surgical site infection | Obstruction | Other complications | Mortality | Follow-up months |
| Safadi | 2004 | 4 | KH | 9 | 3 | 0 | 0 | 0 | 3 | 0 | 24 |
| LeBlanc | 2005 | 4 | KH/SB | 12 | 4 | 0 | 0 | 1 | 3 | 1 | 20 |
| Berger | 2007 | 4 | SB | 41 | 3 | 0 | 1 | 1 | 1 | 0 | 241 |
| Mancini | 2007 | 4 | SB | 25 | 5 | 1 | 1 | 0 | 3 | 1 | 191 |
| McLemore | 2007 | 4 | KH/SB | 19 | 11 | 0 | 2 | 1 | 8 | 0 | 20 |
| Muysoms | 2008 | 4 | KH/SB | 24 | 2 | 0 | 0 | 0 | 2 | 0 | 22 |
| Berger | 2008 | 4 | Sandwich | 47 | 4 | 0 | 0 | 0 | 4 | 0 | 20 |
| Hansson | 2008 | 4 | KH | 55 | 6 | 2 | 0 | 0 | 4 | 0 | 361 |
| Craft | 2008 | 4 | KH/SB | 21 | 8 | 2 | 1 | 1 | 4 | 0 | 14 |
| Pastor | 2009 | 4 | KH/SB | 12 | 4 | 0 | 2 | 0 | 2 | 0 | 14 |
| Jani | 2010 | 4 | KH | 9 | 2 | 0 | 0 | 0 | 2 | 0 | 13 |
| Wara | 2011 | 4 | KH | 72 | 21 | 0 | 4 | 0 | 17 | 2 | 361 |
| Asif | 2012 | 4 | KH/SB | 33 | 13 | 0 | 4 | 1 | 8 | 0 | 12 |
| Mizrahi | 2012 | 4 | KH | 29 | 6 | 0 | 1 | 1 | 4 | 1 | 28 |
| Hansson | 2013 | 4 | SB | 61 | 12 | 1 | 1 | 0 | 9 | 1 | 26 |
| Weighted pooled % (95%CI) | 24.9% (17.9%-32.7%) | 1.7% (0.7%-3.1%) | 3.8% (2.3%-5.7%) | 1.7%(0.7%-3.0%) | 16.6%(11.9%-22.1%) | 1.8%(0.8%-3.2%) | |||||
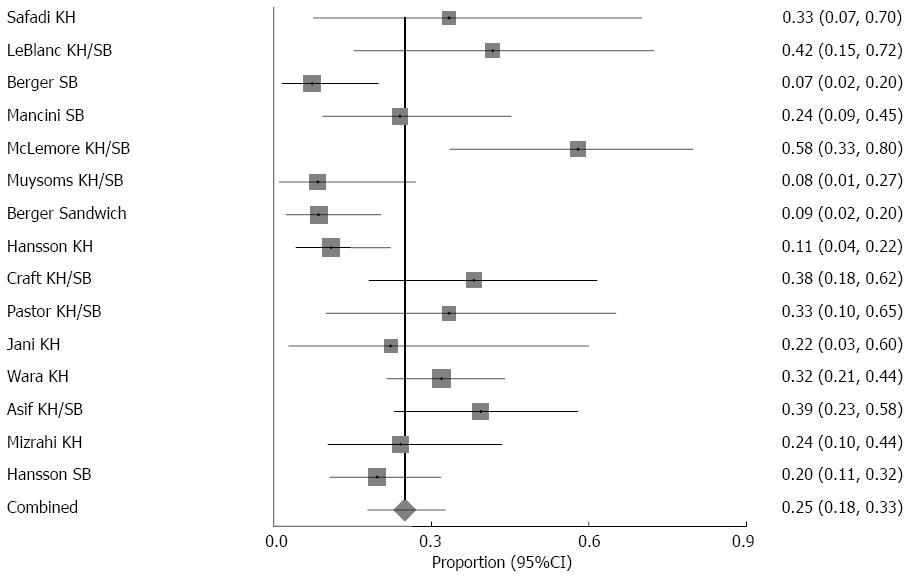
Except for recurrence, most postoperative morbidities were reported for the overall cohort, and not by approach. As such, the most common postoperative complication was surgical site infection, which was seen in 3.8% (95%CI: 2.3-5.7) (Tables 2-4, Figure 2). Infected mesh was observed in 1.7% (95%CI: 0.7-3.1). Obstruction requiring reoperation occurred in 1.7% (95%CI: 0.7-3.0). There were six mortalities during the postoperative course. Two patients died from aspiration events[9,14]. One patient died from hemorrhage secondary to unknown portal hypertension[28]. One patient died due to sepsis[23]. One patient died from multiorgan failure secondary to a hidden bowel injury[28]. One patient died from bowel obstruction secondary to lung carcinoma metastasis[25]. Other complications such as ileus, pneumonia, or urinary tract infection were noted in 16.6% (95%CI: 11.9-22.1). The overall postoperative morbidity rate was 1.8% (95%CI: 0.8-3.2) (Table 1).
| Reference | Year | Technique | No. of repairs | Recurrences |
| Safadi | 2004 | KH | 9 | 4 |
| LeBlanc | 2005 | KH/SB | 12 | 1 |
| Berger | 2007 | SB | 41 | 8 |
| Mancini | 2007 | SB | 25 | 1 |
| McLemore | 2007 | KH/SB | 19 | 2 |
| Muysoms | 2008 | KH/SB | 24 | 10 |
| Berger | 2008 | Sandwich | 47 | 1 |
| Hansson | 2008 | KH | 55 | 20 |
| Craft | 2008 | KH/SB | 21 | 1 |
| Pastor | 2009 | KH/SB | 12 | 4 |
| Jani | 2010 | KH | 9 | 0 |
| Wara | 2011 | KH | 72 | 2 |
| Asif | 2012 | KH/SB | 33 | 11 |
| Mizrahi | 2012 | KH | 29 | 13 |
| Hansson | 2013 | SB | 61 | 3 |
| Weighted pooled% (95%CI) | 17.4% (9.5%-26.9%) | |||
| Reference | Year | No. of repairs | Recurrences |
| LeBlanc | 2005 | 5 | 1 |
| Berger | 2007 | 41 | 8 |
| Mancini | 2007 | 25 | 1 |
| McLemore | 2007 | 14 | - |
| Muysoms | 2008 | 13 | 2 |
| Craft | 2008 | 15 | 0 |
| Pastor | 2009 | 3 | 2 |
| Asif | 2012 | 14 | 0 |
| Hansson | 2013 | 61 | 3 |
| Weighted pooled% (95%CI) | 10.2% (3.9%-19.0%) | ||
| Reference | Year | No. of repairs | Recurrences |
| Safadi | 2004 | 9 | 4 |
| LeBlanc | 2005 | 7 | 0 |
| McLemore | 2007 | 5 | - |
| Muysoms | 2008 | 11 | 8 |
| Hansson | 2008 | 55 | 20 |
| Craft | 2008 | 6 | 1 |
| Pastor | 2009 | 9 | 2 |
| Jani | 2010 | 9 | 0 |
| Wara | 2011 | 72 | 2 |
| Asif | 2012 | 19 | 11 |
| Mizrahi | 2012 | 29 | 13 |
| Weighted pooled% (95%CI) | 27.9% (12.3%-46.9%) | ||
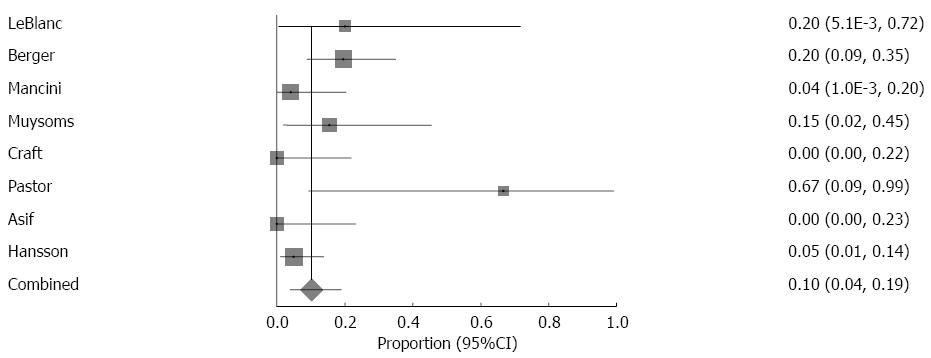
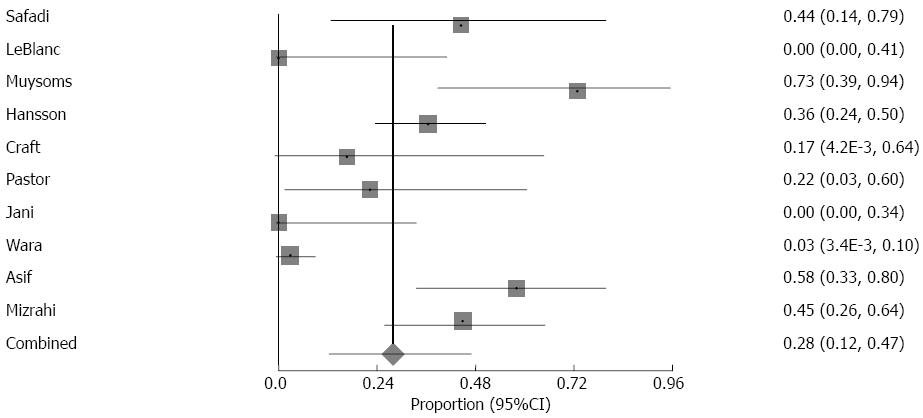
Eighty-one recurrences were reported overall for a recurrence rate of 17.4% (95%CI: 9.5-26.9) (Table 2). The recurrence rate was 10.2% (95%CI: 3.9-19.0) for the modified laparoscopic Sugarbaker approach, whereas the recurrence rate was 27.9% (95%CI: 12.3-46.9) for the keyhole approach (Table 3, Figure 3 and Table 4, Figure 4, respectively)[3,9,11-16,22-26,28]. One study did not separate recurrence by technique, so these patients were included only in the overall recurrence rate and excluded from recurrence rates by technique[11]. For the sandwich technique, which is a combination of the keyhole and the Sugarbaker approach, there was 1 recurrence out of 47 repairs[27]. For the five studies that reported both Sugarbaker and keyhole repairs, recurrence was lower for Sugarbaker in 3 studies[3,15,16], lower for Keyhole in 1[9], and equal in 1[13]. Every study had follow-up time of at least 12 mo (Table 1).
The emergence of laparoscopy for ventral hernia repair has yielded numerous benefits for patients, including quicker recovery and lower postoperative pain. As such, this approach has been applied to the repair of parastomal hernia, considering that it is minimally invasive and may possibly allow for a more precise repair, as it allows for a better view of the abdominal wall[10,22]. Key steps for the laparoscopic approach are hernia sac reduction, adhesiolysis, and proper mesh fixation. As shown in this review, the laparoscopic approach has been relatively successful for repairing parastomal hernia, since conversion rates, mesh infection, surgical site infection, and mortality rates are reasonably low. Currently, the most cited laparoscopic techniques for parastomal hernia repair are the slit mesh Keyhole technique and the non-slit mesh modified Sugarbaker technique[17-19].
The primary differences between keyhole repair and Sugarbaker repair are the orientation of the bowel and the presence of a slit in the mesh. In the modified Sugarbaker approach, the bowel is exteriorized through the side of the mesh, whereas in the Keyhole approach the bowel is inserted through a 2 to 3 cm slit in the center of mesh. Both methods apply the mesh intraperitoneally. Most studies used ePTFE as their choice of mesh, and it is thought that this is one of the reasons for the modified Sugarbaker approach having lower recurrence rates. According to Hansson et al[29], this is because ePTFE has a tendency to shrink, which subsequently widens the slit in the mesh. Because of the enlarged hole, the bowel has a higher propensity to herniate. The largest Sugarbaker and Keyhole cohorts using ePTFE mesh have both been published by Hansson and colleagues in two separate studies[22,25]. In cohorts of 55 Keyhole repairs and 61 Sugarbaker repairs, they found recurrence rates to be 36% and 5%, respectively. As such, in comparing the pooled recurrence rates for each technique, it appears that a modified Sugarbaker approach is superior to the keyhole approach given that current studies show lower recurrence rates for the modified Sugarbaker approach.
In 2011, Wara et al[28] published their long-term results using a composite ePFTE-PP mesh for laparoscopic keyhole repair. The PP side was affixed to the parietal side while the ePFTE side faced the viscera. With a cohort of 72 patients and a median follow-up of 3 years, they reported 2 recurrences for a recurrence rate of 3%. However, they also reported relatively high postoperative morbidity as 5 patients required reoperation due to mesh-related issues. As stated by the authors, it remains to be seen whether the low chance of recurrence is worth the high morbidity.
Berger et al[27] recently described their experience with a two mesh sandwich technique. Using a composite PVDF-PP mesh, they reported a recurrence rate of 2.1% (1 of 47). This technique is a combination of both the Keyhole and modified Sugarbaker approaches. The first mesh, which consists of PP, is fixated to the parietal side of the abdomen and a 2 cm gap is created in the center. The stoma is then threaded through the slit, and the mesh slit is secured by is tacks and transfascial sutures. Then, the second mesh, which is composed of PVDF, is placed under the first mesh. This mesh covers the entirety of the first mesh as well as the abdominal wall. The stoma loop is then lateralized through the side of the second mesh. While outcomes have been positive after 1 year of follow-up, more studies are needed to validate these results.
A single-port laparoscopic approach is the newest development for parastomal hernia repair. Earlier this year, two institutions reported their initial results following this approach. Tran et al[30] reported their outcomes using a single-port modified Sugarbaker technique in 5 patients. Their choice of mesh was ePTFE. With a mean follow-up of 12 mo, they report no recurrences, morbidity, or mortality. Köhler et al[31] report their outcomes with a single-port approach using their novel technique that combines stoma relocation and mesh reinforcement via an intraperitoneal onlay approach. They used a composite PVDF-PP mesh wherein the PVDF side was affixed to the viscera while the PP side was oriented to the contents of the abdomen. With a mean follow-up of 10.5 wk, they also report no recurrences, morbidity or mortality. However, two patients did require additional port insertion due to the presence of dense adhesions and scarring. Although both groups have had positive experiences so far, studies with higher power and longer follow-up are needed to assess the viability of single-port repair as a potential option.
Open stoma relocation has long been associated with poor outcomes primarily because in creating another stoma, the hernia risk is not actually reduced but instead increased further. However, there have been isolated reports of relocating the stoma laparoscopically, Garcia-Vallejo et al[32] presented a case report of a 65 year old patient whom they performed a laparoscopic stoma relocation on. After 18 mo of follow-up, the patient reports no recurrence or morbidity. As mentioned above, Köhler et al[31] recently described their single-port technique that combines stoma relocation and mesh reinforcement, reporting no recurrences or morbidity after 2.5 mo. Due to the limited amount of data, it is not possible to make a firm recommendation for laparoscopic stoma relocation at this time.
In all the laparoscopic Keyhole and Sugarbaker studies reviewed, the choice of mesh was ePTFE, as it has been shown that use of polypropylene mesh for intraperitoneal repair results in dense adhesions, which can subsequently result in mesh erosion[17,33]. The advantage of ePTFE is due to the micropores, which inhibit tissue ingrowth into the mesh thus resulting in fewer adhesions. As such, the mesh is fixated to the fascia using sutures and tacks, and it is eventually encased by fibrocollagen, fully anchoring it to the fascia[9,10,27]. There is concern that will cause the mesh to shrink as the surrounding tissue retracts, and so it advised that at least 4 cm overlap be used[25]. While ePTFE mesh is compatible with the Sugarbaker approach, it has not had the same success with the Keyhole approach. This is because of ePTFE’s propensity to shrink, which in the Keyhole method causes the mesh slit to widen. Combined with the forces from intra-abdominal pressure, recurrence becomes much more likely[22].
There have been a couple reports regarding the use of hybrid mesh types. Wara et al[28] used a ePTFE-PPM hybrid for the Keyhole approach. While it resulted in 3% recurrence, there were mesh-related complications requiring reoperation in 7% of patients. Berger[27] and Bientzle used a PVDF-PPM combination for their sandwich repairs. They reported mesh-related complications in 8% of patients (4 of 47). One was a wound infection while the other three were revisions. More data is needed before combination mesh types can be recommended.
While short-term outcomes have been relatively well-covered, there is a paucity of long-term (i.e., 5 years or more) follow-up. The longest reported for the Keyhole and Sugarbaker approaches have been 3 years and 2 years, respectively[22,25]. Thus, given the short-term success of the modified Sugarbaker approach, the next question to be answered is the longevity of repair: will patients still be recurrence and infection free? In fact, one of the concerns with ePTFE is that it is more prone to infection because it is hydrophobic and microporous[34]. While this review found low rates of infection in studies using ePTFE, outcomes were short-term, and it is possible that longer and more complete follow-up may change these results. Shrinkage of the mesh is also a concern, but Carter[35] and colleagues demonstrated minimal mesh shrinkage in the clinical setting, with an average shrinkage of 6.7% in 815 patients.
In conclusion, based on this current review, laparoscopic intraperitoneal mesh repair is an effective means for surgically treating parastomal hernia. The non-slit mesh modified Sugarbaker approach and the slit mesh Keyhole approach are currently the most reported options for laparoscopic repair. When choosing between the two, a modified Sugarbaker technique appears to be a superior method given the low recurrence rates compared to the keyhole technique if an ePTFE mesh is used. Other techniques include a single-port approach and a two mesh sandwich technique. Though these techniques have shown promising outcomes, more studies are needed to assess their efficacy. Overall, the majority of studies concerning laparoscopic intraperitoneal mesh repair for parastomal hernia have been retrospective with relatively small cohorts. Although results have been positive, the scarcity of well-powered controlled prospective, comparative studies with long-term follow-up makes it difficult to definitively recommend one laparoscopic approach over another.
Parastomal hernia repair is one of the more complex abdominal procedures. With high recurrence rates and postoperative morbidity in open repair, the need for better surgical options is crucial. Given the success of laparoscopy for ventral hernia repair, similar options for repairing parastomal hernia has arisen. Thus, it is crucial that the current laparoscopic options be analyzed.
The most reported laparoscopic options for parastomal hernia repair are the Keyhole (slit mesh) and the modified Sugarbaker (non-slit mesh) technique Other options include sandwich repair and a single port approach, though these are isolated reports.
Of the two primary laparoscopic approaches, the modified Sugarbaker approach has been shown to result in lower recurrence rates and morbidity. Expanded polytetrafluoroethylene (ePTFE) is the preferred mesh because it does not cause dense adhesions to develop.
The results of this review suggest that the modified Sugarbaker approach with ePTFE mesh should be the primary option for laparoscopic Sugarbaker repair. The sandwich technique has shown promise, but there is currently one published report about it.
Parastomal hernia occurs when abdominal content protrudes through incision created during stoma formation.
Because of the poor outcome following open surgical repair of parastomal hernia and in the abscence of hard data from controlled studies, review of promising laparoscopic methods - like the present - is needed. Selection of studies for the review and list of references are appropriate.
P- Reviewer: Garcia-Vallejo L, Wara P S- Editor: Yu J L- Editor: A E- Editor: Zhang DN
| 2. | Israelsson LA. Parastomal hernias. Surg Clin North Am. 2008;88:113-25, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 120] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 3. | Craft RO, Huguet KL, McLemore EC, Harold KL. Laparoscopic parastomal hernia repair. Hernia. 2008;12:137-140. [PubMed] |
| 4. | Londono-Schimmer EE, Leong AP, Phillips RK. Life table analysis of stomal complications following colostomy. Dis Colon Rectum. 1994;37:916-920. [PubMed] |
| 5. | López-Cano M, Lozoya-Trujillo R, Quiroga S, Sánchez JL, Vallribera F, Martí M, Jiménez LM, Armengol-Carrasco M, Espín E. Use of a prosthetic mesh to prevent parastomal hernia during laparoscopic abdominoperineal resection: a randomized controlled trial. Hernia. 2012;16:661-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 6. | Ripoche J, Basurko C, Fabbro-Perray P, Prudhomme M. Parastomal hernia. A study of the French federation of ostomy patients. J Visc Surg. 2011;148:e435-e441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 91] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 7. | Rosin JD, Bonardi RA. Paracolostomy hernia repair with Marlex mesh: a new technique. Dis Colon Rectum. 1977;20:299-302. [PubMed] |
| 8. | Ogata S, Hongo M. Bacteriophages of the genus Clostridium. Adv Appl Microbiol. 1979;25:241-273. [PubMed] |
| 9. | LeBlanc KA, Bellanger DE, Whitaker JM, Hausmann MG. Laparoscopic parastomal hernia repair. Hernia. 2005;9:140-144. [PubMed] |
| 10. | Hansson BM, de Hingh IH, Bleichrodt RP. Laparoscopic parastomal hernia repair is feasible and safe: early results of a prospective clinical study including 55 consecutive patients. Surg Endosc. 2007;21:989-993. [PubMed] |
| 11. | McLemore EC, Harold KL, Efron JE, Laxa BU, Young-Fadok TM, Heppell JP. Parastomal hernia: short-term outcome after laparoscopic and conventional repairs. Surg Innov. 2007;14:199-204. [PubMed] |
| 12. | Berger D, Bientzle M. Laparoscopic repair of parastomal hernias: a single surgeon’s experience in 66 patients. Dis Colon Rectum. 2007;50:1668-1673. [PubMed] |
| 13. | Pastor DM, Pauli EM, Koltun WA, Haluck RS, Shope TR, Poritz LS. Parastomal hernia repair: a single center experience. JSLS. 2009;13:170-175. [PubMed] |
| 14. | Mancini GJ, McClusky DA, Khaitan L, Goldenberg EA, Heniford BT, Novitsky YW, Park AE, Kavic S, LeBlanc KA, Elieson MJ. Laparoscopic parastomal hernia repair using a nonslit mesh technique. Surg Endosc. 2007;21:1487-1491. [PubMed] |
| 15. | Muysoms F. Laparoscopic repair of parastomal hernias with a modified Sugarbaker technique. Acta Chir Belg. 2007;107:476-480. [PubMed] |
| 16. | Asif A, Ruiz M, Yetasook A, Denham W, Linn J, Carbray J, Ujiki MB. Laparoscopic modified Sugarbaker technique results in superior recurrence rate. Surg Endosc. 2012;26:3430-3434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Hansson BM, Slater NJ, van der Velden AS, Groenewoud HM, Buyne OR, de Hingh IH, Bleichrodt RP. Surgical techniques for parastomal hernia repair: a systematic review of the literature. Ann Surg. 2012;255:685-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 219] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 18. | Shah NR, Craft RO, Harold KL. Parastomal hernia repair. Surg Clin North Am. 2013;93:1185-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Hotouras A, Murphy J, Thaha M, Chan CL. The persistent challenge of parastomal herniation: a review of the literature and future developments. Colorectal Dis. 2013;15:e202-e214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 20. | OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. Available from: http://www.cebm.net/index.aspx?o=5653 (accessed December 2014). |
| 21. | DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28:105-114. [PubMed] |
| 22. | Hansson BM, Bleichrodt RP, de Hingh IH. Laparoscopic parastomal hernia repair using a keyhole technique results in a high recurrence rate. Surg Endosc. 2009;23:1456-1459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 23. | Mizrahi H, Bhattacharya P, Parker MC. Laparoscopic slit mesh repair of parastomal hernia using a designated mesh: long-term results. Surg Endosc. 2012;26:267-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Safadi B. Laparoscopic repair of parastomal hernias: early results. Surg Endosc. 2004;18:676-680. [PubMed] |
| 25. | Hansson BM, Morales-Conde S, Mussack T, Valdes J, Muysoms FE, Bleichrodt RP. The laparoscopic modified Sugarbaker technique is safe and has a low recurrence rate: a multicenter cohort study. Surg Endosc. 2013;27:494-500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 26. | Jani K. Laparoscopic paracolostomy hernia repair: a retrospective case series at a tertiary care center. Surg Laparosc Endosc Percutan Tech. 2010;20:395-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Berger D, Bientzle M. Polyvinylidene fluoride: a suitable mesh material for laparoscopic incisional and parastomal hernia repair! A prospective, observational study with 344 patients. Hernia. 2009;13:167-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 83] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 28. | Wara P, Andersen LM. Long-term follow-up of laparoscopic repair of parastomal hernia using a bilayer mesh with a slit. Surg Endosc. 2011;25:526-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 29. | Hansson BM, van Nieuwenhoven EJ, Bleichrodt RP. Promising new technique in the repair of parastomal hernia. Surg Endosc. 2003;17:1789-1791. [PubMed] |
| 30. | Tran H, Turingan I, Zajkowska M, Tran K. Single-port laparoscopic parastomal hernia repair with modified sugarbaker technique. JSLS. 2014;18:34-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Köhler G, Emmanuel K, Schrittwieser R. Single-port parastomal hernia repair by using 3-D textile implants. JSLS. 2014;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | García-Vallejo L, Concheiro P, Mena E, Baltar J, Baamonde I, Folgar L. Parastomal hernia repair: laparoscopic ventral hernia meshplasty with stoma relocation. The current state and a clinical case presentation. Hernia. 2011;15:85-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 33. | Halm JA, de Wall LL, Steyerberg EW, Jeekel J, Lange JF. Intraperitoneal polypropylene mesh hernia repair complicates subsequent abdominal surgery. World J Surg. 2007;31:423-49; discussion 430. [PubMed] |
| 34. | Bleichrodt RP, Simmermacher RK, van der Lei B, Schakenraad JM. Expanded polytetrafluoroethylene patch versus polypropylene mesh for the repair of contaminated defects of the abdominal wall. Surg Gynecol Obstet. 1993;176:18-24. [PubMed] |
| 35. | Carter PR, LeBlanc KA, Hausmann MG, Whitaker JM, Rhynes VK, Kleinpeter KP, Allain BW. Does expanded polytetrafluoroethylene mesh really shrink after laparoscopic ventral hernia repair? Hernia. 2012;16:321-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |