Published online Sep 28, 2014. doi: 10.3748/wjg.v20.i36.13133
Revised: January 18, 2014
Accepted: June 20, 2014
Published online: September 28, 2014
Processing time: 295 Days and 7.2 Hours
AIM: To investigate the clinical differences between small intestinal injuries in low-dose aspirin (LDA) users and in non-steroidal anti-inflammatory drug (NSAID) users who were examined by capsule endoscopy (CE) for obscure gastrointestinal bleeding (OGIB).
METHODS: A total of 181 patients who underwent CE for OGIB were included in this study. Based on clinical records, laboratory data such as hemoglobin levels, major symptoms, underlying diseases, the types and duration of LDA and NSAID use, and endoscopic characteristics of CE were reviewed.
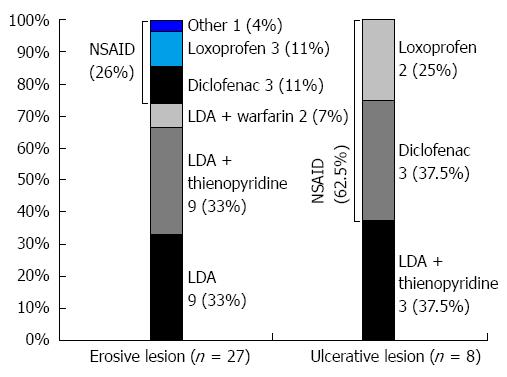
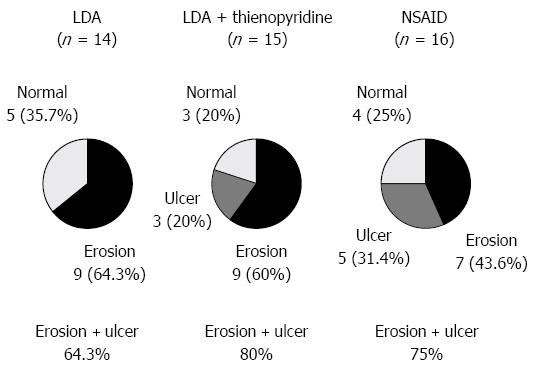
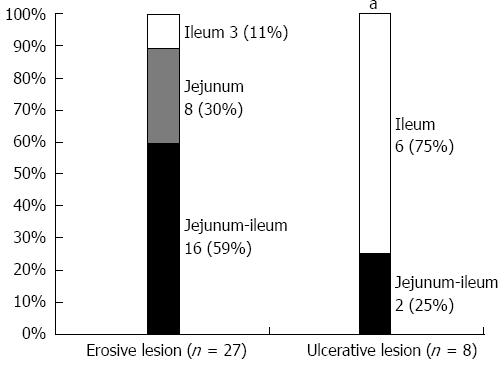
RESULTS: Out of a total of 45 cases of erosive lesions, 27 cases were taking LDA or NSAIDs (7 were on NSAIDs, 9 were on LDA alone, 9 were on LDA and thienopyridine, and 2 were on LDA and warfarin).The prevalence of ulcers or erosion during chronic use of LDA, LDA and the anti-platelet drug thienopyridine (clopidogrel or ticlopidine), and NSAIDs were 64.3%, 80.0%, and 75.0%, respectively. Erosive lesions were observed predominantly in chronic LDA users, while ulcerative lesions were detected mainly in NSAID users. However, concomitant use of thienopyridine such as clopidogrel with LDA increased the proportion of ulcers. The erosive lesions were located in the whole of the small intestine (jejunum and ileum), whereas ulcerative lesions were mainly observed in the ileum (P < 0.05).
CONCLUSION: Our CE findings indicate that chronic LDA users and NSAID users show different types and locations of small-bowel mucosal injuries. The concomitant use of anti-platelet drugs with LDA tends to exacerbate the injuries from LDA-type to NSAID-type injuries.
Core tip: The aim of this study is that to clarify the clinical feature of ulcerative or erosive lesion of small intestine in the long-term non-steroidal anti-inflammatory drug (NSAID) users who were examined by capsule endoscopy for obscure gastrointestinal bleeding. The ulcerative lesions were predominantly located in both jejunum and ileum or just in ileum while erosive lesions were predominantly found in both jejunum and ileum or just in jejunum significantly. These findings indicate the possibility that distribution of NSAID-induced small intestinal lesion differ according to the types of mucosal injury.
- Citation: Iwamoto J, Mizokami Y, Saito Y, Shimokobe K, Honda A, Ikegami T, Matsuzaki Y. Small-bowel mucosal injuries in low-dose aspirin users with obscure gastrointestinal bleeding. World J Gastroenterol 2014; 20(36): 13133-13138
- URL: https://www.wjgnet.com/1007-9327/full/v20/i36/13133.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i36.13133
It has been demonstrated that low-dose aspirin (LDA) and non-steroidal anti-inflammatory drugs (NSAIDs) increase the risk of gastroduodenal mucosal injury[1,2]. Recent reports using new methods of investigating the small intestine, such as double balloon endoscopy (DBE)[3] and capsule endoscopy (CE)[4], have also shown that NSAIDs can cause mucosal damage in the small intestine[5-8]. Obscure gastrointestinal bleeding (OGIB) is defined as bleeding of unknown origin that persists or recurs after a negative initial or primary upper endoscopy and colonoscopy and radiologic evaluation of the small bowel[9,10]. The clinical features of the ulcerative or erosive lesions of the small intestine in long-term NSAID users who were examined subsequently by CE for OGIB have not been sufficiently reported.
In the present study, 181 OGIB cases were examined with CE and were investigated with the following aims: to evaluate the prevalence of ulcerative or erosive lesions in the small intestine in chronic LDA or NSAID users in OGIB cases, to analyze the clinical features including endoscopic findings of these lesions, and to analyze the clinical course of these cases.
Between June 2007 and September 2013, 181 patients who underwent CE for OGIB at Tokyo Medical University Ibaraki Medical Center were analyzed in this study.
CE was performed using a PillCam SB (Given Imaging). Patients fasted for 10 h before capsule ingestion. Drinking clear fluids was allowed 2 h and eating a light snack was allowed 4 h after ingestion of the capsule. The data recorder was removed 8 h later, and the patients were subsequently discharged. Data were downloaded and interpreted by experienced endoscopists. The patients were asked to report any adverse events and to confirm excretion of the capsule in their stool.
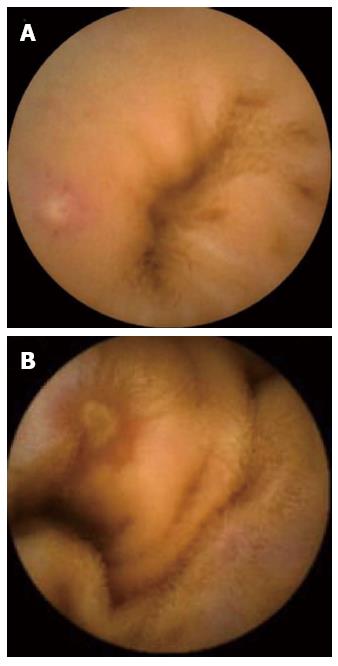
Based on clinical records, laboratory data such as hemoglobin levels, major symptoms, underlying diseases, the types and duration of NSAIDs, and endoscopic characteristics of CE were reviewed. The morphologies of the lesions were classified into red spots, small erosion, large erosion, or ulcers as previously reported[7]. A red spot was defined as a red spot or crimson area of mucosa with presentation of villous architecture. A small erosion was defined as a circumscribed area of mucosal disruption denuded of villi with or without exudates or red color with a diameter equivalent to that of a valvulae conniventes. Large erosions were defined as circumscribed breaks in the mucosa larger than the equivalent diameter of a valvulae conniventes. In the present study, red spots, small erosion, and large erosion were included in the CE erosion results (Figure 1A). Ulcers were defined as large erosion with a central area with exudates[7] (Figure 1B).
The small bowel was divided into two segments (proximal and distal) equally on the basis of each subject’s small bowel transit time.
The continuous variables were expressed as mean values ± SD. We compared the categorical variables using the Fisher’s exact test and the continuous variables using the Mann-Whitney test. A P value of less than 0.05 was considered statistically significant.
Out of a total of 181 CE cases for OGIB, 13 cases (7.2%) were diagnosed as ulcerative lesions and 45 cases (24.9%) as erosive lesions of the small intestine. Out of a total of 13 cases of ulcerative lesions, 8 cases were taking LDA or NSAIDs (5 were on NSAIDs while 3 were on LDA and the anti-platelet drug, thienopyridine; clopidogrel). Out of a total of 45 cases of erosive lesions, 27 cases were taking LDA or NSAIDs (7 were on NSAIDs, 9 were on LDA alone, 9 were on LDA and thienopyridine, and 2 were on LDA and warfarin). Erosive lesions were observed predominantly in chronic LDA users, whereas ulcerative lesions were detected mainly in NSAID users (Figure 2).
The prevalence of ulcers or erosion during chronic use of LDA, LDA and thienopyridine, and NSAIDs was 64.3%, 80.0%, and 75.0%, respectively (Figure 3). The concomitant use of thienopyridine (clopidogrel) with LDA increased the proportion of ulcers from 0% to 20%.
The locations of erosive and ulcerative lesions are shown in Figure 4. The erosive lesions were located in the entire small intestine (jejunum and ileum), whereas ulcerative lesions were observed mainly in the ileum (P < 0.05).
Details of the characteristics of ulcerative lesions of chronic LDA or NSAID users are summarized in Table 1. In 4 of the 8 ulceration cases, LDA or NSAID was withdrawn. In 4 patients who had continued the LDA (n = 3) or NSAID (n = 1), 3 cases used prostaglandin and one case used rebamipide. Eventually, significant improvement of the ulcerative lesions was confirmed in all 4 cases with clinical course or CE finding.
| Age | Gender | UD | Species (duration) | Symptom | Hemoglobin (g/dL) | Location | Number | Treatment | Clinical course |
| 67 | F | Headache | Loxoprofen (6M) | Tarry stool/anemia | 9.5 | Ileum | Multiple | Withdrawal of NSAID | Improved |
| 83 | M | OD | Diclofenac (6M) | FOBT (+) anemia | 11.5 | Jejunu Ileum | Multiple | Withdrawal of NSAID | Improved |
| 59 | M | ID | LDA + clopidogrel (6M) | Tarry stool/anemia | 10.3 | Ileum | Multiple | Continuation of LDA PG | Improved |
| 70 | M | CD | LDA + clopidogrel (2Y) | Tarry stool/anemia | 9.3 | Jejunum Ileum | Multiple | Continuation of LDA PG | Improved |
| 79 | F | RA | Diclofenac (4Y) | Tarry stool/anemia | 8.3 | Ileum | Multiple | Continuation of NSAID rebamipide | Improved |
| 74 | F | ID | LDA + clopidogrel (1Y) | Anemia/abdominal pain | 9.3 | Ileum | Multiple | Continuation of LDA PG | Improved |
| 63 | M | OD | Loxoprofen (6Y) | Tarry stool/anemia | 11.2 | Ileum | Multiple | Withdrawal of NSAID | Improved |
| 73 | F | OD | Diclofenac (5Y) | Tarry stool/anemia | 10.4 | Ileum | Multiple | Withdrawal of NSAID | Improved |
| 10.0 ± 1.0 |
The damage to the gastric and duodenal mucosa caused by NSAIDs is well established, and there has been increasing recognition of the damage caused to the mucosa of the small intestine by NSAID treatment[1,2,5-8]. The pathogenesis of NSAID-induced small intestinal damage has been investigated, and a number of mechanisms have been implicated, including the toll-like receptor 4/MyD88-dependent pathway[11], dual inhibition of COX enzymes[12], enterohepatic circulation of NSAIDs[13], mitochondrial damage[14], and ischemia-reperfusion injury[15].
The prevalence of NSAID-induced small bowel lesions in the cases who had undergone CE or BDE for OGIB has also been investigated. A previous report has shown that among the 108 cases that underwent DBE for OGIB, 5 cases (4.6%) were diagnosed with NSAID–associated ulcers of the small intestine (5). A multicenter study has shown that 31 cases (4.7%) were diagnosed with NSAID-induced ulcerative lesions among 661 cases who underwent DBE for OGIB (6). In our present study, 4.4% and 14.9% of the cases were diagnosed with ulcerative lesion and erosive lesions for chronic LDA or NSAID users in OGIB cases by CE, respectively. Collectively, 19.3% of the cases were diagnosed with mucosal lesions with long-term LDA or NSAID treatment in OGIB cases by CE. The prevalence of NSAID-induced mucosal injury among chronic NSAID users has been reported in several studies[7,16,17]. Small intestinal ulceration was found in 21 patients (8.4%) among 249 long-term NSAID users and just 3 patients (0.6%) among 464 non-users in a previous investigation where the stomach, duodenum, and small intestine of 713 post-mortem patients were examined (16). Another recent study using video capsule endoscopy has demonstrated occurrence of small bowel injury in 71% of NSAID users compared with 10% of the controls, indicating that NSAID damage is more frequent and extensive than suggested by ileoscopy performed at the time of colonoscopy[7].
The clinical features of NSAID-induced small bowel lesions have been documented. Hayashi et al[18] analyzed 7 patients with small bowel lesions while taking NSAIDs out of 61 patients who had undergone BDE for OGIB. The results have shown that ulcers or erosions were observed in the ileum in six patients (86%) and in the jejunum in one patient (14%). Another previous report has shown that 12 (57.1%) out of 21 small bowel lesions in chronic NSAID users were found in the ileum[16]. On the other hand, investigating the distribution of CE-detected small bowel lesions revealed that the lesions were found in the proximal, middle, and distal small bowel, suggesting that there were no significant tendencies in the distribution of small bowel lesions[8]. The distribution and types of small intestinal injury due to NSAIDs have been studied, and it has been shown that in the majority of denuded areas located in the proximal part, erosions were found throughout the small intestine, and all of the ulcers were in the distal part, suggesting that the distribution differed according to the type of mucosal injury during short-term NSAID medication[19]. Our results demonstrate differences in the distribution between ulcers and erosion in patients taking long-term LDA or NSAIDs, indicating that ulcers are located mainly in the ileum, whereas erosion was located throughout the small intestine.
LDA is used as a preventive treatment for ischemic heart disease and ischemic cerebrovascular disease[20]. Recent reports have indicated that low-dose aspirin causes not only gastroduodenal mucosal injury but also small bowel injury with high frequency[21,22]. Hayashi et al[22] have reported that 8 (44%) of 18 patients diagnosed with NSAID-induced small bowel injury by DBE were taking low-dose aspirin. Watanabe et al[23] have investigated small bowel injury with CE in 11 patients who developed gastric ulcers while undergoing low-dose aspirin. The study showed that red spots were found in 100% of the patients and mucosal breaks were found in 90.9% of the patients, indicating that very high incidences of small bowel injury were found in the patients who developed gastric ulcers while undergoing low-dose aspirin treatment. In our results, there were more patients taking LDA in the erosion cases than in the ulcer cases, suggesting the possibility that the characteristic endoscopic features of LDA-induced mucosal injury in the small intestine were smaller in size than in the case of NSAID-induced mucosal injury.
It has been demonstrated that co-administration of prostaglandin and rebamipide reduced the incidence of NSAID-induced small intestinal lesions[24,25]. In our study, NSAIDs were withdrawn if possible. However, in some cases, especially in the case of LDA and the anti-platelet drug, thienopyridine, it was not possible to withdraw the LDA. In these cases, the prostaglandin or rebamipide was used concomitantly and has shown improved clinical course or CE findings after the treatment. These findings suggest that prostaglandin or rebamipide is effective for treating LDA or NSAID-induced mucosal injury of the small intestine.
In conclusion, our CE study demonstrated that erosive lesions were located in the entire small intestine (jejunum and ileum), and such lesions were observed predominantly in chronic LDA users. In contrast, ulcerative lesions were located mainly in the ileum and were found in NSAID users. However, concomitant use of thienopyridine such as clopidogrel with LDA appeared to increase ulcerative lesions in patients without using NSAIDs, which suggests that small-bowel mucosal injuries can be changed from LDA type to NSAID type by the additional use of anti-platelet drugs.
It has been demonstrated that low-dose aspirin (LDA) and non-steroidal anti-inflammatory drugs (NSAIDs) increase the risk of gastroduodenal mucosal injury.
Recent reports have indicated that low-dose aspirin causes not only gastroduodenal mucosal injury but also small bowel injury with high frequency.
It has been demonstrated that co-administration of prostaglandin and rebamipide reduced the incidence of NSAID-induced small intestinal lesions[24,25]. In this study, NSAIDs were withdrawn if possible.
The concomitant use of anti-platelet drugs with LDA tends to exacerbate the injuries from LDA-type to NSAID-type injuries.
This retrospective study analyzed the clinical feature of small intestinal mucosal lesion of the chronic NSAID users in the cases of obscure gastrointestinal bleeding.
P- Reviewer: Calabrese C, Holt RJ, Koulaouzidis A S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Singh G, Ramey DR, Morfeld D, Shi H, Hatoum HT, Fries JF. Gastrointestinal tract complications of nonsteroidal anti-inflammatory drug treatment in rheumatoid arthritis. A prospective observational cohort study. Arch Intern Med. 1996;156:1530-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 177] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 2. | García Rodríguez LA, Hernández-Díaz S. Relative risk of upper gastrointestinal complications among users of acetaminophen and nonsteroidal anti-inflammatory drugs. Epidemiology. 2001;12:570-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 181] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 3. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 861] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 4. | Iddan G, Meron G, Glukhovsky A, Swain P. Wireless capsule endoscopy. Nature. 2000;405:417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 134] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Tanaka S, Mitsui K, Yamada Y, Ehara A, Kobayashi T, Seo T, Tatsuguchi A, Fujimori S, Gudis K, Sakamoto C. Diagnostic yield of double-balloon endoscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2008;68:683-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Matsumoto T, Kudo T, Esaki M, Yano T, Yamamoto H, Sakamoto C, Goto H, Nakase H, Tanaka S, Matsui T. Prevalence of non-steroidal anti-inflammatory drug-induced enteropathy determined by double-balloon endoscopy: a Japanese multicenter study. Scand J Gastroenterol. 2008;43:490-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 91] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 7. | Graham DY, Opekun AR, Willingham FF, Qureshi WA. Visible small-intestinal mucosal injury in chronic NSAID users. Clin Gastroenterol Hepatol. 2005;3:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 404] [Cited by in RCA: 391] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 8. | Maiden L, Thjodleifsson B, Theodors A, Gonzalez J, Bjarnason I. A quantitative analysis of NSAID-induced small bowel pathology by capsule enteroscopy. Gastroenterology. 2005;128:1172-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 353] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 9. | Zuckerman GR, Prakash C, Askin MP, Lewis BS. AGA technical review on the evaluation and management of occult and obscure gastrointestinal bleeding. Gastroenterology. 2000;118:201-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 321] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 10. | Raju GS, Gerson L, Das A, Lewis B. American Gastroenterological Association (AGA) Institute technical review on obscure gastrointestinal bleeding. Gastroenterology. 2007;133:1697-1717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 379] [Cited by in RCA: 338] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 11. | Watanabe T, Higuchi K, Kobata A, Nishio H, Tanigawa T, Shiba M, Tominaga K, Fujiwara Y, Oshitani N, Asahara T. Non-steroidal anti-inflammatory drug-induced small intestinal damage is Toll-like receptor 4 dependent. Gut. 2008;57:181-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 170] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 12. | Sigthorsson G, Simpson RJ, Walley M, Anthony A, Foster R, Hotz-Behoftsitz C, Palizban A, Pombo J, Watts J, Morham SG. COX-1 and 2, intestinal integrity, and pathogenesis of nonsteroidal anti-inflammatory drug enteropathy in mice. Gastroenterology. 2002;122:1913-1923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 143] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 13. | Reuter BK, Davies NM, Wallace JL. Nonsteroidal anti-inflammatory drug enteropathy in rats: role of permeability, bacteria, and enterohepatic circulation. Gastroenterology. 1997;112:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 230] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 14. | Somasundaram S, Rafi S, Hayllar J, Sigthorsson G, Jacob M, Price AB, Macpherson A, Mahmod T, Scott D, Wrigglesworth JM. Mitochondrial damage: a possible mechanism of the “topical” phase of NSAID induced injury to the rat intestine. Gut. 1997;41:344-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 241] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 15. | Anthony A, Pounder RE, Dhillon AP, Wakefield AJ. Vascular anatomy defines sites of indomethacin induced jejunal ulceration along the mesenteric margin. Gut. 1997;41:763-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Allison MC, Howatson AG, Torrance CJ, Lee FD, Russell RI. Gastrointestinal damage associated with the use of nonsteroidal antiinflammatory drugs. N Engl J Med. 1992;327:749-754. [PubMed] |
| 17. | Morris AJ, MacKenzie JF. Small-bowel enteroscopy and NSAID ulceration. Lancet. 1991;337:1550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Hayashi Y, Yamamoto H, Kita H, Sunada K, Sato H, Yano T, Iwamoto M, Sekine Y, Miyata T, Kuno A. Non-steroidal anti-inflammatory drug-induced small bowel injuries identified by double-balloon endoscopy. World J Gastroenterol. 2005;11:4861-4864. [PubMed] |
| 19. | Fujimori S, Gudis K, Takahashi Y, Seo T, Yamada Y, Ehara A, Kobayashi T, Mitsui K, Yonezawa M, Tanaka S. Distribution of small intestinal mucosal injuries as a result of NSAID administration. Eur J Clin Invest. 2010;40:504-510. [PubMed] |
| 20. | Collaborative overview of randomised trials of antiplatelet therapy--I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists’ Collaboration. BMJ. 1994;308:81-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2844] [Cited by in RCA: 2476] [Article Influence: 79.9] [Reference Citation Analysis (0)] |
| 21. | Leung WK, Bjarnason I, Wong VW, Sung JJ, Chan FK. Small bowel enteropathy associated with chronic low-dose aspirin therapy. Lancet. 2007;369:614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Hayashi Y, Yamamoto H, Taguchi H, Sunada K, Miyata T, Yano T, Arashiro M, Sugano K. Nonsteroidal anti-inflammatory drug-induced small-bowel lesions identified by double-balloon endoscopy: endoscopic features of the lesions and endoscopic treatments for diaphragm disease. J Gastroenterol. 2009;44 Suppl 19:57-63. [PubMed] |
| 23. | Watanabe T, Sugimori S, Kameda N, Machida H, Okazaki H, Tanigawa T, Watanabe K, Tominaga K, Fujiwara Y, Oshitani N. Small bowel injury by low-dose enteric-coated aspirin and treatment with misoprostol: a pilot study. Clin Gastroenterol Hepatol. 2008;6:1279-1282. [PubMed] |
| 24. | Niwa Y, Nakamura M, Ohmiya N, Maeda O, Ando T, Itoh A, Hirooka Y, Goto H. Efficacy of rebamipide for diclofenac-induced small-intestinal mucosal injuries in healthy subjects: a prospective, randomized, double-blinded, placebo-controlled, cross-over study. J Gastroenterol. 2008;43:270-276. [PubMed] |
| 25. | Fujimori S, Seo T, Gudis K, Ehara A, Kobayashi T, Mitsui K, Yonezawa M, Tanaka S, Tatsuguchi A, Sakamoto C. Prevention of nonsteroidal anti-inflammatory drug-induced small-intestinal injury by prostaglandin: a pilot randomized controlled trial evaluated by capsule endoscopy. Gastrointest Endosc. 2009;69:1339-1346. [PubMed] |