Published online Apr 26, 2016. doi: 10.13105/wjma.v4.i2.55
Peer-review started: December 1, 2015
First decision: December 28, 2015
Revised: February 2, 2016
Accepted: February 23, 2016
Article in press: February 24, 2016
Published online: April 26, 2016
Processing time: 135 Days and 13.7 Hours
AIM: To obtain the diagnostic performance of percutaneous transthoracic needle biopsy (PTNB) under Computed tomography (CT) fluoroscopy guidance for lung ground-glass opacity (GGO).
METHODS: We searched for English- and Chinese-language studies in PubMed, EMBASE, EBSCO, OVID, and CNKI (China National Knowledge Infrastructure) database. Data were calculated with Meta-Disc version 1.4 and Rev Man version 5.2 software. From the pooled data, we calculated sensitivity (Sen), specificity (Spe), positive likelihood ratio (+LR), negative likelihood ratio (-LR), and diagnostic odds ratio (DOR). Summary receiver operating characteristic (SROC) curves were constructed and incidence of complications was recorded.
RESULTS: Four documents included in this present meta-analysis met the criteria for analysis. The pooled Sen, Spe, +LR, -LR and DOR with 95%CI were 0.91 (0.86-0.95), 1.0 (0.91-1.0), 18.64 (4.83-71.93), 0.11 (0.05-0.26) and 153.17 (30.78-762.33), respectively. The area under the SROC curve was 0.98. The incidence of pneumothorax and hemoptysis was 17.86%-51.80% and 10.50%-19.40%, respectively.
CONCLUSION: CT fluoroscopy-guided PTNB, which has an acceptable incidence of complications, can be used as a primary examination method for lung GGO, with moderate sensitivity and specificity.
Core tip: There is no consensus in the literature about the diagnostic performance of percutaneous transthoracic needle biopsy (PTNB) under Computed tomography (CT) fluoroscopy guidance for lung ground-glass opacity (GGO). We performed a meta-analysis to obtain the diagnostic performance of CT fluoroscopy-guided PTNB of lung GGO in terms of pooled sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, diagnostic odds ratio and incidence of complications. We also generated a summary receiver operating characteristic curve as a way of summarizing the global test performance of CT fluoroscopy-guided PTNB.
- Citation: Yan GW, Yan GW, Sun QQ, Niu XK, Li B, Bhetuwal A, Xu XX, Du Y, Yang HF. Computed tomography fluoroscopy guided percutaneous lung biopsy for ground-glass opacity pulmonary lesions: A meta-analysis. World J Meta-Anal 2016; 4(2): 55-62
- URL: https://www.wjgnet.com/2308-3840/full/v4/i2/55.htm
- DOI: https://dx.doi.org/10.13105/wjma.v4.i2.55
Ground-glass opacity (GGO) in lung parenchyma is a image manifestation on thin-section Computed tomography (CT) that is defined as “hazy increased attenuation of the lung with preservation of bronchial and vascular margins”[1]. As prevalence of lung cancer screening with low-dose CT rises, so has the detection of pulmonary lesions that manifest as GGO nodules[2,3]. Since, GGO, not being a specific imaging finding, many differential diagnoses such as bronchoalveolar carcinoma, adenocarcinoma, atypical adenomatous hyperplasia, focal fibrosis and inflammatory diseases must be taken into consideration[4,5]. As a result, the importance of diagnosing lung GGO cannot be ignored once observation, clinical follow-up or chemotherapeutic therapy has ruled out the benign or inflammatory nature of the lesion. However, controversy does exist on whether PTNB should be attempted for the persistent presence of lung GGO or not.
Recent efforts[6-9] utilizing PTNB under the guidance of CT fluoroscopy have been attempted to increase the diagnostic accuracy of lung GGO but contain only few enrolled subjects. The objective of this article was to obtain the diagnostic performance of CT fluoroscopy guided PTNB for lung GGO with a meta-analysis, which, as far as the authors’ understanding, has not been reported previously.
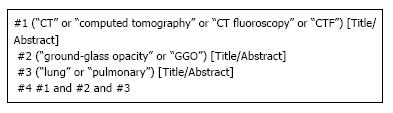
We searched PubMed, EMBASE, OVID, EBSCO, and CNKI (China National Knowledge Infrastructure) databases without publication date or language restrictions, from inception to August 2015, using the search terms “CT”, “computed tomography”, “CT fluoroscopy”, “CTF”, “ground-glass opacity”, “GGO”, “lung”, and “pulmonary”. Search terms were present in the title or abstract of the articles. The detailed search strategy of PubMed is shown in Figure 1.
A system documentation retrieval of human articles was accomplished by two independent observers to find out studies about the diagnostic value of CT fluoroscopy-guided PTNB in patients with GGO. All case reports, letters, comments, and review articles were eliminated. Subsequently, studies, on the basis of their title and abstract, was either included or discarded.
Studies that complied with the following criteria were also included in this study: (1) Adequate data to calculate the number of true positive (tp), false positive (fp), false negative (fn), and true negative (tn) results; (2) definite criteria to define a positive imaging result were documented; and (3) clinical follow-up or clinical observation for at least one year and/or surgery.
Other potentially eligible studies were identified by manually searching the reference lists of the articles enrolled in this meta-analysis. Any differences of opinion in selecting the studies between the two reviewers were resolved through discussion. If there was any unresolved studies advices were sought from another two reviewers experienced in study selection and data extraction in more than six meta-analyses or systematic reviews.
A 2 × 2 table was created to input following data extracted from each study included in the present meta-analysis: (1) true positive results (subjects with disease diagnosed correctly from the standard test); (2) false positive results (subjects without disease diagnosed as diseased from the standard test); (3) false negative results (subjects with disease diagnosed as without disease from the standard test); (4) true negative results (subjects without disease diagnosed correctly as without disease from the standard test); and (5) other clinical characteristics of the studies (including author, year of publication, lesion size, and complications).
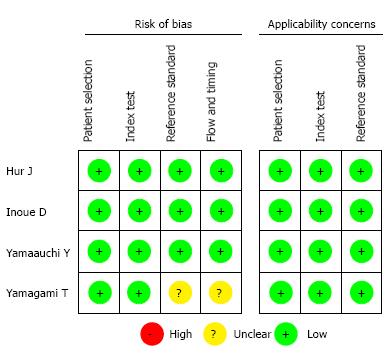
Methodological quality was evaluated on the basis of the Quality Assessment of Studies of Diagnostic Accuracy included on Systematic Reviews (QUADAS-2) guidelines independently by the same two reviewers who had performed the literature search. The quality of studies of diagnostic accuracy was specifically evaluated by the evidence-based tool above. Any dispute was resolved through discussion among the reviewers. A more detailed description of each item and a guideline on how to use the QUADAS-2 tool are provided by Whiting et al[10].
The data integration for the accuracy of CT fluoroscopy-guided PTNB for lung GGO lesions was made by calculating pooled estimates of sensitivity (Sen), specificity (Spe), positive likelihood ratio (+LR), negative likelihood ratio (-LR), and diagnostic odds ratio (DOR) at a patient level. We also generated a summary receiver operating characteristic (SROC) curve as a way of summarizing the global test performance from different diagnostic studies. The pooled Sen, Spe, +LR, -LR, DOR, and SROC across studies were calculated by using a random or fixed effect model according to the heterogeneity. Heterogeneity across studies was evaluated by using the χ2 and Fisher’s exact tests. Threshold effect was assessed by using the Spearman rank correlation test. Subgroup analysis was also performed if necessary. Statistical analyses in this present meta-analysis were all carried out with Meta-disc software (version 1.4). P < 0.05 was considered statistically significant.
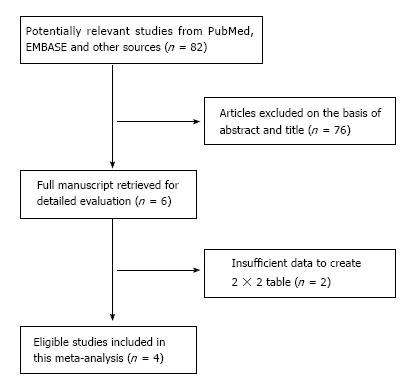
Literature search revealed 82 articles which, after reading the titles and abstracts of the searched articles, 76 documents were discarded as they did not meet the inclusion criteria. After closer inspection of full text, 2 out of six were again discarded for the causes provided in Figure 2. Finally, the remaining four studies which fulfilled the inclusion criteria were included in this meta-analysis[6-9]. All 4 studies were published in English. Table 1 shows the basic characteristics of the included four studies. Methodological quality of the four studies, as evaluated by the QUADAS-2 tool, is shown in Figure 3.
| Ref. | Year | Lesion size (mm) | tp | fp | fn | tn | All | Complications |
| Hur et al[6] | 2009 | ≤ 10 | 4 | 0 | 2 | 4 | 10 | Pneumothorax (5); |
| 11-20 | 5 | 0 | 2 | 3 | 10 | Hemoptysis (3); Thoracostomy tube insertion (2) | ||
| > 20 | 3 | 0 | 1 | 4 | 8 | |||
| All | 12 | 0 | 5 | 11 | 28 | |||
| Yamauchi et al[7] | 2011 | ≤ 10 | 6 | 0 | 1 | 1 | 8 | Pneumothorax (14); Hemoptysis (13); Thoracostomy tube insertion (0) |
| 11-20 | 36 | 0 | 1 | 5 | 42 | |||
| > 20 | 17 | 0 | 0 | 0 | 17 | |||
| All | 59 | 0 | 2 | 6 | 67 | |||
| Inoue et al[8] | 2012 | ≤ 10 | 21 | 0 | 1 | 2 | 24 | Pneumothorax (30); Hemoptysis (7); Thoracostomy tube insertion (1); Air embolism (1) |
| 11-20 | 36 | 0 | 2 | 3 | 41 | |||
| > 20 | 1 | 0 | 0 | 0 | 1 | |||
| All | 58 | 0 | 3 | 5 | 66 | |||
| Yamagami et al[9] | 2013 | ≤ 10 | 16 | 0 | 4 | 11 | 31 | Pneumothorax (44); Hemoptysis (9); Thoracostomy tube insertion (3) |
| 11-20 | 30 | 0 | 4 | 6 | 40 | |||
| > 20 | 12 | 0 | 0 | 2 | 14 | |||
| All | 58 | 0 | 8 | 19 | 85 |
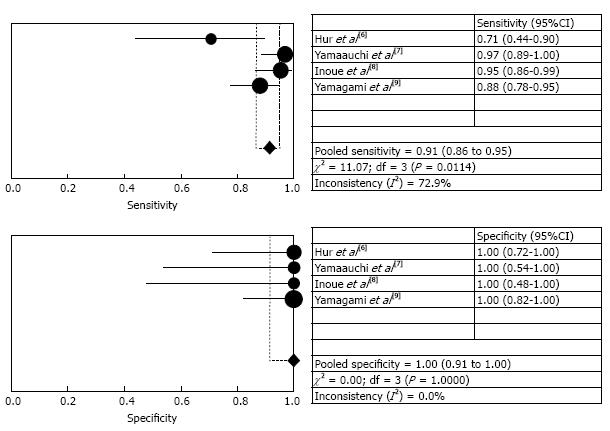
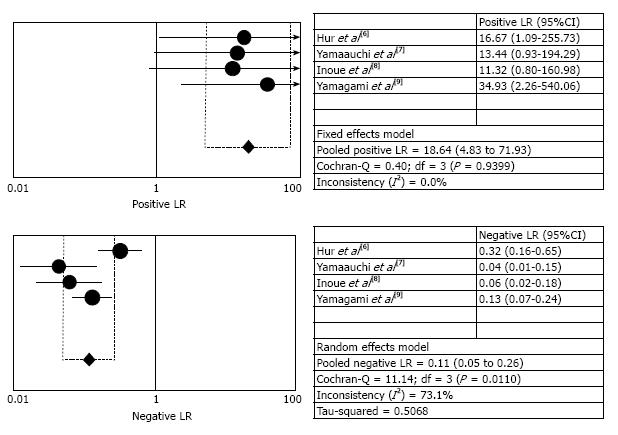
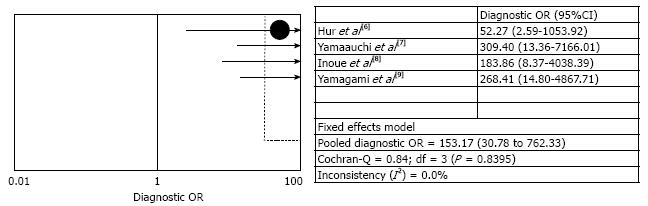
The pooled sensitivity with 95%CI was 0.91 (0.86-0.95), ranging from 0.71 to 0.88. However, the pooled specificity with 95%CI was 1.00 (0.91-1.00), and the specificities in the four studies were all reported as 1.00. The +LR, -LR and DOR with 95%CI was 18.64 (4.83-71.93), 0.11 (0.05-0.26), and 153.17 (30.78-762.33), respectively. χ2 values of Sen, Spe, +LR, -LR, and DOR were 11.07 (P = 0.01), 0.0 (P = 1.0), 0.40 (P = 0.94), 11.14 (P = 0.01), and 0.84 (P = 0.84), respectively, indicating that there are some degree of heterogeneity among the four documents.
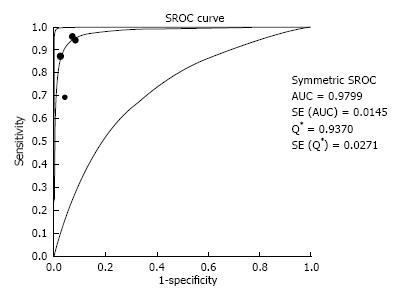
Forest plots (Figure 4) reveals the detailed sensitivity and specificity with 95%CI of each individual study. The detailed +LR and -LR with 95%CI for each individual study are shown in Forest plots (Figure 5). Figure 6 is the Forest plot of the DOR. The SROC curve showed a good overall diagnostic performance for CT fluoroscopy-guided PTNB for all studies combined (Figure 7). In this meta-analysis, Q-value of the maximum joint sensitivity and specificity was 0.94. The area under the SROC curve (AUC) was 0.98, which indicated a relatively high level of overall accuracy.
Subgroup analysis was performed according to the size of the lesions and pooled indexes (Sen, Spe, +LR, -LR, DOR and SROC) with 95%CI are summarized in Table 2.
| Size | Sen | Spe | +LR | -LR | DOR | SROC |
| All | 0.91 (0.86-0.95) | 1.0 (0.91-1.0) | 18.64 (4.83-71.93) | 0.11 (0.05-0.26) | 153.17 (30.78-762.33) | 0.98 |
| ≤ 10 mm | 0.85 (0.73-0.94) | 1.0 (0.81-1.0) | 8.03 (2.21-29.18) | 0.24 (0.14-0.41) | 37.94 (7.48-192.37) | 0.92 |
| 11-20 mm | 0.92 (0.86-0.96) | 1.0 (0.80-1.0) | 9.35 (2.45-35.71) | 0.13 (0.08-0.22) | 67.98 (13.06-353.87) | 0.96 |
| > 20 mm | 0.94 (0.70-1.0) | 1.0 (0.54-1.0) | 6.24 (0.97-40.0) | 0.20 (0.07-0.60)a | 38.93 (2.80-541.16)b | -c |
The incidence of pneumothorax ranged from 17.86% to 51.80%, and was reported in all four studies, with six patients requiring chest tube drainage. The incidence of hemoptysis ranged from 10.50% to 19.40% without any patients requiring treatment for it. Systemic air embolism occurred in one case as reported in the study by Inoue et al[8]. Apart from these, there were no other complications or adverse effects reported in the four studies included in the meta-analysis.
Bronchoscopy is one option for examination of patients with suspected lung masses. It can be used for tissue sampling, evaluating the nature and extent of a lung mass or a lesion and guiding therapy. However, in the case of a non-diagnostic bronchoscopy (i.e., failure to obtain a histopathological diagnosis from lung lesion), image-guided PTNB is usually performed. Among these interventional techniques, lung biopsy under CT guidance has widespread acceptance as a preferred modality for the diagnosis of pulmonary masses. Its diagnostic accuracy is 92.9%-95% and the incidence of adverse effects is within an acceptable range[11-13]. Compared with techniques under conventional CT guidance, as it was reported, “CT fluoroscopy-guided PTNB allows continuous monitoring of the needle as it progresses toward the target lesion, enabling manipulation in response to respiratory movements”[14,15].
Nevertheless, diagnostic performance of PTNB under CT fluoroscopy guidance for the diagnosis of pulmonary GGO nodules is not well established. This meta-analysis investigated the overall diagnostic performance of CT fluoroscopy-guided PTNB in the differential diagnosis of GGO lesions with a high Sen and Spe, 0.91 (95%CI: 0.86-0.95) and 1.00 (95%CI: 0.91-1.00), respectively. The SROC curve stands for a global summary of test efficacy and indicates the trade-off between Sen and Spe[16]. Our meta-analysis, according to the SROC curve, indicated that the maximum joint Sen and Spe was 0.94 and the AUC was 0.98, suggesting a high level of overall diagnostic efficacy. We conclude that CT fluoroscopy-guided PTNB plays an important role in the diagnosis of GGO lesions. DOR which, combines the data from Sen and Spe into a single value, is another reference of test accuracy[17]. In our meta-analysis, the DOR with 95%CI was 153.17 (30.78-762.33), indicating that CT fluoroscopy-guided PTNB was valuable in the diagnosis of GGO lesions. Subgroup analysis was performed according to the size of the lesions, and the pooled parameters were still good, indicating that CT fluoroscopy-guided PTNB was valuable in the diagnosis of GGO lesions regardless of their size.
The rate of complications was thought to be within an acceptable range. Pneumothorax, with an incidence of 17.86%-51.8%, was the most frequently encountered complication of CT fluoroscopy-guided PTNB[6-9]. Out of the 246 patients, only six required chest tube drainage. The incidence of hemoptysis ranged from 10.5% to 19.4%, without any of the patients requiring treatment. Yamagami et al[9], in the largest study, reported that the incidence of pneumothorax and hemoptysis was 51.8% and 10.6%, respectively. Inoue et al[8] reported one case of systemic air embolism. Even though an exact reason behind it could not be determined, there is a possibility of creating needle-induced fistula between the bronchus and the pulmonary vein in GGO lesion biopsy more than during solid lesion biopsy since GGO lesions preserve the bronchus and pulmonary vessels located inside them[8]. Hence, taking the results of Sen, Spe, DOR, +LR, and -LR into account, it is reasonable to think that CT fluoroscopy-guided PTNB can be used as one of the primary examination procedures for lung GGO lesions.
With respect to influencing factors for pneumothorax, there were significant differences reported, including patient age, sex, lesion location, number of pleural passages, and emphysema along the needle pathway[6-9,18]. Influencing factors for hemoptysis included patient age and sex, lesion location, nodule type, and distance from the pleura to the target lesion. Ground-glass nodules and deeper-located lesions were significant independent risk factors for hemoptysis[6-9,18]. In addition, the needle–pleural angle is another predictor of pneumothorax as reported by Li et al[19] and Niu et al[20]. De Filippo et al[21] reported that non-calcified density (the higher the density, the better the accuracy) was a positive predictive factor for diagnostic accuracy. The diagnostic performance of PTNB under CT guidance can be elevated by the use of multiplanar reformatting imaging, which is useful for planning the path of the needle while performing needle aspiration.
The diagnostic outcomes of conventional CT-guided lung biopsy have been studied previously. Kim et al[22] reported the outcomes of 50 patients (< 2.0 cm vs≥ 2.0 cm and GGO component > 90% vs 50%-90%) who had been investigated with coaxial 18-gauge or 20-gauge core needles. The overall Sen, Spe, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy were 92.0%, 90.0%, 97.0%, 75.0% and 91.0%, respectively. Sensitivity and accuracy were not significantly different between the two groups of lesion size and GGO components. Lu et al[23] reported the outcomes of 49 patients investigated with coaxial 20-gauge core needles. The overall Sen, Spe, PPV, NPV, and diagnostic accuracy were 93.62%, 100%, 100%, 40.0% and 93.88%, respectively. Compared to these results[22,23], we assume that the methodologies used in the included studies[6-9] (i.e., the CT fluoroscopy and coaxial needle system) contributed to the high diagnostic accuracy observed.
This study is in accordance of the recommendation based upon the reporting of meta-analysis on diagnostic test[24]. We based this study on thorough literature searches and careful data extraction. Nevertheless, some limitations may be considered when interpreting the results. First, study includes only four articles. The limited number of patients (n = 246) may have an effect on our study. Second, the four studies did not compare directly the diagnostic accuracy of CT fluoroscopy-guided PTNB with other methods. Thus, we cannot definitively state which method is better at this time. However, studies by Rotolo et al[25] and Prosch et al[26] concluded that CT fluoroscopy systems for lung nodule biopsy are similar in terms of diagnostic performance and effective dose as cone-beam CT-guided and multislice CT systems. Finally, the publication format of four studies was English, which might resort to the so called “Tower of Babel” bias. In a word, further, larger prospective studies may be needed.
In conclusion, in spite of the difficulties mentioned above, considering the high diagnostic performance of CT fluoroscopy-guided PTNB in our study, along with the acceptable number of complications, we still have the reason to believe that this method can be recommended in clinical practice. In the end, update of systematic review and meta-analysis is possible only when further research and data is available on this topic.
In recent years, as prevalence of lung cancer screening with low-dose computed tomography (CT) rises, so has the detection of pulmonary lesions that manifest as ground-glass opacity (GGO) nodules. Recently, several efforts utilizing percutaneous transthoracic needle biopsy (PTNB) under the guidance of CT fluoroscopy have been attempted to increase the diagnostic accuracy of lung GGO. Despite this, no consensus is available in the literature about whether it is beneficial to the patient.
Because lung GGO is a nonspecific finding, it occurs in both malignant and benign lung lesions. Thus, the diagnosis of GGO lesions has become an important issue. Global research is directed towards an accurate and minimally invasive method for the diagnosis of lung GGO.
In this study, the authors investigated the value of CT fluoroscopy-guided PTNB for diagnosis of lung GGO. It is believed to be the first meta-analysis evaluating the value of CT fluoroscopy-guided PTNB for lung GGO.
The present study helps the authors understanding of the role of a minimally invasive technique for the diagnosis of lung GGO.
The aim of manuscript was to evaluate the value of CT fluoroscopy guided PTNB for the diagnosis of lung GGO with the use of meta-analysis method. The authors used the restrictive inclusion criteria, so only 4 manuscripts were included into analysis. Based on this they made some useful conclusions.
P- Reviewer: Chiang TA, Hsu WH, Roller J, Tabarkiewicz J S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246:697-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2471] [Cited by in RCA: 2674] [Article Influence: 157.3] [Reference Citation Analysis (0)] |
| 2. | Kaneko M, Eguchi K, Ohmatsu H, Kakinuma R, Naruke T, Suemasu K, Moriyama N. Peripheral lung cancer: screening and detection with low-dose spiral CT versus radiography. Radiology. 1996;201:798-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 560] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 3. | Henschke CI, McCauley DI, Yankelevitz DF, Naidich DP, McGuinness G, Miettinen OS, Libby DM, Pasmantier MW, Koizumi J, Altorki NK. Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet. 1999;354:99-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1729] [Cited by in RCA: 1623] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 4. | Collins J, Stern EJ. Ground-glass opacity at CT: the ABCs. AJR Am J Roentgenol. 1997;169:355-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 122] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Nakajima R, Yokose T, Kakinuma R, Nagai K, Nishiwaki Y, Ochiai A. Localized pure ground-glass opacity on high-resolution CT: histologic characteristics. J Comput Assist Tomogr. 2002;26:323-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 93] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Hur J, Lee HJ, Nam JE, Kim YJ, Kim TH, Choe KO, Choi BW. Diagnostic accuracy of CT fluoroscopy-guided needle aspiration biopsy of ground-glass opacity pulmonary lesions. AJR Am J Roentgenol. 2009;192:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 7. | Yamauchi Y, Izumi Y, Nakatsuka S, Inoue M, Hayashi Y, Mukai M, Nomori H. Diagnostic performance of percutaneous core needle lung biopsy under multi-CT fluoroscopic guidance for ground-glass opacity pulmonary lesions. Eur J Radiol. 2011;79:e85-e89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Inoue D, Gobara H, Hiraki T, Mimura H, Kato K, Shibamoto K, Iishi T, Matsui Y, Toyooka S, Kanazawa S. CT fluoroscopy-guided cutting needle biopsy of focal pure ground-glass opacity lung lesions: diagnostic yield in 83 lesions. Eur J Radiol. 2012;81:354-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Yamagami T, Yoshimatsu R, Miura H, Yamada K, Takahata A, Matsumoto T, Hasebe T. Diagnostic performance of percutaneous lung biopsy using automated biopsy needles under CT-fluoroscopic guidance for ground-glass opacity lesions. Br J Radiol. 2013;86:20120447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6953] [Cited by in RCA: 9478] [Article Influence: 677.0] [Reference Citation Analysis (0)] |
| 11. | Takeshita J, Masago K, Kato R, Hata A, Kaji R, Fujita S, Katakami N. CT-guided fine-needle aspiration and core needle biopsies of pulmonary lesions: a single-center experience with 750 biopsies in Japan. AJR Am J Roentgenol. 2015;204:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 12. | Geraghty PR, Kee ST, McFarlane G, Razavi MK, Sze DY, Dake MD. CT-guided transthoracic needle aspiration biopsy of pulmonary nodules: needle size and pneumothorax rate. Radiology. 2003;229:475-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 300] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 13. | Yeow KM, Tsay PK, Cheung YC, Lui KW, Pan KT, Chou AS. Factors affecting diagnostic accuracy of CT-guided coaxial cutting needle lung biopsy: retrospective analysis of 631 procedures. J Vasc Interv Radiol. 2003;14:581-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 137] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 14. | Froelich JJ, Ishaque N, Regn J, Saar B, Walthers EM, Klose KJ. Guidance of percutaneous pulmonary biopsies with real-time CT fluoroscopy. Eur J Radiol. 2002;42:74-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 59] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Gianfelice D, Lepanto L, Perreault P, Chartrand-Lefebvre C, Milette PC. Value of CT fluoroscopy for percutaneous biopsy procedures. J Vasc Interv Radiol. 2000;11:879-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Walter SD. Properties of the summary receiver operating characteristic (SROC) curve for diagnostic test data. Stat Med. 2002;21:1237-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 485] [Cited by in RCA: 512] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 17. | Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM. The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol. 2003;56:1129-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1459] [Cited by in RCA: 1673] [Article Influence: 79.7] [Reference Citation Analysis (0)] |
| 18. | Hiraki T, Mimura H, Gobara H, Iguchi T, Fujiwara H, Sakurai J, Matsui Y, Inoue D, Toyooka S, Sano Y. CT fluoroscopy-guided biopsy of 1,000 pulmonary lesions performed with 20-gauge coaxial cutting needles: diagnostic yield and risk factors for diagnostic failure. Chest. 2009;136:1612-1617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 169] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 19. | Li Y, Du Y, Yang HF, Yu JH, Xu XX. CT-guided percutaneous core needle biopsy for small (≤20 mm) pulmonary lesions. Clin Radiol. 2013;68:e43-e48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 20. | Niu XK, Bhetuwal A, Yang HF. CT-guided core needle biopsy of pleural lesions: evaluating diagnostic yield and associated complications. Korean J Radiol. 2015;16:206-212. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | De Filippo M, Saba L, Concari G, Nizzoli R, Ferrari L, Tiseo M, Ardizzoni A, Sverzellati N, Paladini I, Ganazzoli C. Predictive factors of diagnostic accuracy of CT-guided transthoracic fine-needle aspiration for solid noncalcified, subsolid and mixed pulmonary nodules. Radiol Med. 2013;118:1071-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 22. | Kim TJ, Lee JH, Lee CT, Jheon SH, Sung SW, Chung JH, Lee KW. Diagnostic accuracy of CT-guided core biopsy of ground-glass opacity pulmonary lesions. AJR Am J Roentgenol. 2008;190:234-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 23. | Lu CH, Hsiao CH, Chang YC, Lee JM, Shih JY, Wu LA, Yu CJ, Liu HM, Shih TT, Yang PC. Percutaneous computed tomography-guided coaxial core biopsy for small pulmonary lesions with ground-glass attenuation. J Thorac Oncol. 2012;7:143-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 24. | Deeks JJ. Systematic reviews in health care: Systematic reviews of evaluations of diagnostic and screening tests. BMJ. 2001;323:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 822] [Cited by in RCA: 893] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 25. | Rotolo N, Floridi C, Imperatori A, Fontana F, Ierardi AM, Mangini M, Arlant V, De Marchi G, Novario R, Dominioni L. Comparison of cone-beam CT-guided and CT fluoroscopy-guided transthoracic needle biopsy of lung nodules. Eur Radiol. 2016;26:381-389. [PubMed] |
| 26. | Prosch H, Stadler A, Schilling M, Bürklin S, Eisenhuber E, Schober E, Mostbeck G. CT fluoroscopy-guided vs. multislice CT biopsy mode-guided lung biopsies: accuracy, complications and radiation dose. Eur J Radiol. 2012;81:1029-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |