Published online Dec 18, 2024. doi: 10.13105/wjma.v12.i4.97779
Revised: November 1, 2024
Accepted: December 5, 2024
Published online: December 18, 2024
Processing time: 187 Days and 5.5 Hours
Diabetes-related distress (DRD) is a common psychological disorder specifically associated with diabetes, its cross-talk with depression, and glycated hemoglobin (HbA1c) was discussed controversially. Interventions addressing DRD were shown to improve HbA1c. However, the primary concern is to investigate the association of DRD with glycemic control. No meta-analyses have compared the effects of depression and diabetes distress on HbA1c.
To assess the relationship between DRD, depression, and glycemic control.
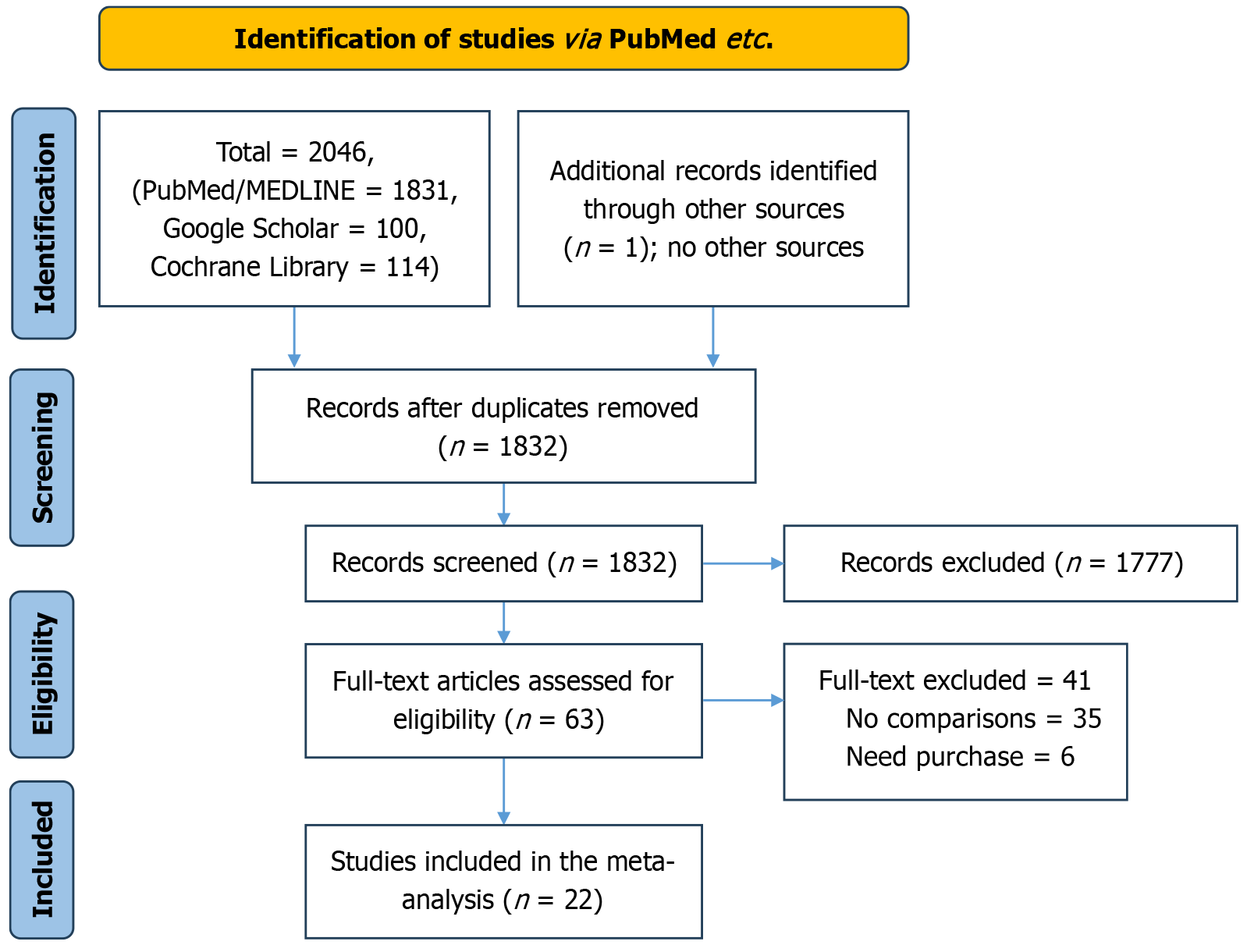
We systematically searched PubMed MEDLINE, Google Scholar, and Cochrane Library from inception up to May 2024. The keywords diabetes distress, depre
Out of the 2046 studies retrieved, 55 full texts were screened and 22 studies were included in the final meta-analysis. Diabetes distress was associated with poor glycemic control, odd ratio = 0.42, 95% confidence interval (CI): 0.17-0.67, and P value < 0.001, and odd ratio = 0.52, 95%CI: 0.38-0.72, and P value < 0.001 respec
DRD negatively influenced the HbA1c and glycemic control more than depression. Further studies using more specific measures (ecological momentary assessment) to assess DRD are recommended.
Core Tip: Literature on the effects of diabetes distress is scarce, the available meta-analyses focused on interventions to tackle diabetes (to improve glycemic control) distress instead of investigating the direct influence of diabetes distress on the same. However, the association of depression with glycemic control was touched before. However, this is the first meta-analysis to compare the effects of diabetes distress and depression on glycated hemoglobin (HbA1c). We found an association between diabetes distress, depression, and HbA1c with a higher impact of distress arm compared to depression. Due to the overlap between the symptoms of diabetes distress and depression, diabetes distress could mediate the association between depression and HbA1c. Although the reverse could be true, diabetes distress is commoner than depression. The current findings challenged the scientific community and recommended screening for both diabetes distress and depression among patients with diabetes mellitus and poor glycemic control. In addition, we suggested future studies using continuous glucose monitoring and ecological momentary assessment to evaluate the association of diabetes distress, depression, and glycemic control.
- Citation: Mirghani HO. Diabetes distress, the mediator of the poor glycemic control and depression: A meta-analysis. World J Meta-Anal 2024; 12(4): 97779
- URL: https://www.wjgnet.com/2308-3840/full/v12/i4/97779.htm
- DOI: https://dx.doi.org/10.13105/wjma.v12.i4.97779
Diabetes mellitus is a chronic disabling disease with lethal complications; the disease is approaching an epidemic and is rapidly spreading with 463 million people suffering from it in the year 2017, this number is projected to be 700 million by 2045. Diabetes management is complex, time-consuming, and distressful to the patients[1,2]. Because of this, nearly 40% of patients with type 2 diabetes experience psychological problems including diabetes distress, anxiety, and depression[3]. Diabetes-related distress (DRD) is a psychological reaction (negative) among people living with diabetes and is special to diabetes rather than other psychological diseases[4]. DRD is common and nearly half of patients with diabetes are affected with negative influence on the patient’s emotion and quality of life. Importantly, DRD is usually undiagnosed despite its high prevalence and negative effects on diabetes management[5]. The association between diabetes distress, glycemic control, and microvascular complications was discussed controversially, some studies found an association, while others found no relationship[6,7]. However, DRD’s negative effects on diabetes self-care, medication adherence, diabetes severity, and burden were documented. Non-compliance to diabetes medications and diabetes distress were indirectly correlated and might influence diabetes self-management[8,9]. The debate observed in the relationship between diabetes distress and diabetes outcomes could be explained in part by the overlap between diabetes distress and depression, both conditions are highly prevalent among patients with diabetes[10].
Depression affects one in five patients with diabetes and is associated with poor glycemic control, depression is closely related to diabetes distress and could mediate the poor glycemic control observed among distressed patients with diabetes, but the cross-talk between diabetes distress and depression is controversial and literature on this important medical issue scarce[11].
Importantly, diabetes distress might initiate a vicious cycle of increasing diabetes severity, more complex diabetes therapy, polypharmacy, depression, and hence more diabetes distress[12,13]. Surprisingly, most of the recent reviews focused on interventions to mitigate DRD to improve glycemic control[14,15], while the logical first step is to assess the rationale behind the intervention which is the effect of diabetes distress on glycated hemoglobin (HbA1c). To the best of our knowledge, few studies have assessed the effects of DRD on glycemic control and no meta-analysis has compared diabetes distress and depression effects on the HbA1c. Thus, we aimed to assess the effects of DRD on glycemic control and to compare its influence on HbA1c with that of depression.
We conducted this systematic review with great adherence to the PRISMA guidelines during March and April 2024 to assess and compare the effects of DRD on glycemic control among patients with diabetes.
Studies were included if they were retrospective studies, prospective cohorts, cross-sectional studies, and case-control studies. Case series, editorials, opinions, protocols with no results, and editorials were excluded. The effect of depression on glycemic control was extensively touched before[16-19]; therefore, studies assessing the same were not included in the present meta-analysis.
To assess diabetes distress and depression effects on glycemic control, and HbA1c. To compare the effects of diabetes distress and depression on glycemic control, no tests were specified for the diagnosis of depression and diabetes distress.
A systematic literature search was conducted in PubMed MEDLINE, Cochrane Library, and Google Scholar from the date of the first inception up to April 2024. The reviewer searched the databases for relevant articles. The keywords diabetes distress, depre
| Ref. | Country | Study type | Diabetes distress HbA1c | Total number | Controls HbA1c | Total number | Results |
| Al-Ozairi et al[21] | Kuwait | Cross-sectional | 9.2 ± 3.5 | 69 | 8.4 ± 2.49 | 396 | Sig. |
| Alzughbi et al[22] | Saudi Arabia | Cross-sectional | 9.4 ± 1.7 | 67 | 8.7 ± 1.7 | 233 | Sig. |
| Ascher-Svanum et al[23] | Five European countries | Prospective | 9.91 ± 2.09 | 289 | 9.39 ± 1.97 | 677 | Sig. |
| Asuzu et al[24] | United States | Cross-sectional | 7.9 ± 1.8 | 615 | 8.66 ± 1.8 | 615 | Not sig. |
| Chen et al[25] | Taiwan | Cross-sectional | 10.98 + 7.56 | 255 | 10.39 + 2.09 | 255 | Not sig. |
| Cummings et al[26] | United States | Prospective | 9.4 ± 0.3 | 45 | 8.8 ± 0.2 | 84 | Sig. |
| Davis et al[27] | Australia | Prospective | 6.87 ± 0.7 | 435 | 7.6 ± 0.8 | 93 | Sig. |
| Guo et al[28] | Singapore | Cross-sectional | 9.7 ± 1.4 | 62 | 9.4 ± 1.5 | 294 | Not sig. |
| Hayashino et al[29] | Japan | Retrospective | 7.9 ± 1.4 | 371 | 7.5 ± 1.1 | 2747 | Not sig. |
| Ismail et al[30] | United Kingdom | Prospective | 7.20 ± 1.61 | 111 | 6.98 ± 1.40 | 1540 | Sig. |
| Khan and Choudhary[31] | United Kingdom | Cross-sectional | 8.7 ± 1.8 | 24 | 7.7 ± 0.9 | 59 | Sig. |
| Matsuba et al[32] | Three Asian countries | Cross-sectional | 8.68 ± 1.63 | 671 | 7.77 ± 1.63 | 671 | Sig. |
| Nguyen et al[33] | Vietnam | Cross-sectional | 7.7 ± 1.4 | 14 | 7.1 ± 1.5 | 98 | Sig. |
| Pandit et al[12] | United States | Prospective | 9.3 ± 2.0 | 94 | 7.8 ± 1.7 | 391 | Sig. |
| Park et al[34] | Korea | Retrospective | 7.27 ± 0.7 | 589 | 6.97 ± 0.6 | 1293 | Sig. |
| Schmitt et al[35] | Germany | Cross-sectional | 8.8 ± 1.5 | 42 | 8.6 ± 1.7 | 221 | Not sig. |
| Sidhu and Tang[36] | Canada | Cross-sectional | 7.0 ± 0.9 | 20 | 7.0 ± 1.1 | 19 | Not sig. |
| Totesora et al[37] | Philippines | Cross-sectional | 9.0 ± 2.5 | 40 | 7.7 ± 1.7 | 47 | Sig. |
| Ref. | Country | Study type | Diabetes distress glycemic control | Total number | Controls, glycemic control | Total number | Results |
| Bhaskara et al[38] | Indonesia | Cross-sectional | 53 | 75 | 19 | 49 | Sig. |
| Huynh et al[39] | Vietnam | Cross-sectional | 118 | 152 | 236 | 365 | Sig. |
| Lim et al[40] | Singapore | Cross-sectional | 58 | 146 | 91 | 379 | Sig. |
| Sasi et al[41] | India | Cross-sectional | 144 | 270 | 126 | 270 | Sig. |
| Totesora et al[37] | Philippines | Cross-sectional | 28 | 40 | 27 | 47 | Sig. |
| Ref. | Country | Study type | Diabetes distress HbA1c | Total number | Depression HbA1c | Total number | Results |
| Al-Ozairi et al[21] | Kuwait | Cross-sectional | 9.2 ± 3.5 | 69 | 8.7 ± 2 | 44 | Sig. |
| Ascher-Svanum et al[23] | United States | Prospective | 9.91 ± 2.09 | 289 | 9.62 ± 2.02 | 485 | Not sig. |
| Davis et al[27] | Australia | Prospective | 6.87 ± 0.7 | 435 | 7.5 ± 1.28 | 50 | Sig. |
| Hayashino et al[29] | Japan | Retrospective | 7.9 ± 1.4 | 371 | 7.6 ± 1.2 | 862 | Sig. |
| Ismail et al[30] | United Kingdom | Prospective | 7.20 ± 1.61 | 111 | 7.11 ± 1.37 | 232 | Not sig. |
| Nanayakkara et al[13] | Australia | Retrospective | 9.3 ± 2.1 | 177 | 8.85 ± 2.0 | 698 | Sig. |
| Sidhu and Tang[36] | Canada | Cross-sectional | 7.0 ± 0.9 | 21 | 7.0 ± 0.9 | 6 | Not sig. |
The Newcastle Ottawa scale[20] was used to assess the quality of the included studies. All the included studies are of good quality (Table 4).
| Ref. | Questionnaires used | Selection bias | Comparability bias | Outcome | Total score |
| Al-Ozairi et al[21] | The PAID, patient health questionnaire-9 | 5 | 1 | 2 | 8 |
| Alzughbi et al[22] | The 17-item diabetes distress scale and the patient health questionnaire-9 | 5 | 1 | 2 | 8 |
| Ascher-Svanum et al[23] | Severity of depressed/anxious mood (EuroQol-5D item) and diabetes-related distress (psychological distress domain of the diabetes health profile-18) | 4 | 2 | 3 | 9 |
| Asuzu et al[24] | The 17-item diabetes distress scale, and patient health questionnaire | 5 | 2 | 2 | 9 |
| Chen et al[25] | The short-form problem areas in diabetes scale, psychological factors questionnaire | 4 | 1 | 2 | 7 |
| Cummings et al[26] | The 17-item diabetes distress scale | 4 | 2 | 3 | 9 |
| Davis et al[27] | The PAID, patient health questionnaire-9 | 4 | 2 | 3 | 9 |
| Guo et al[28] | The PAID, patient health questionnaire-9 | 4 | 1 | 3 | 8 |
| Hayashino et al[29] | The PAID questionnaire, center for epidemiological studies-depression | 4 | 2 | 3 | 9 |
| Ismail et al[30] | The patient health questionnaire-9 and PAID scores | 4 | 2 | 3 | 9 |
| Khan and Choudhary[31] | Diabetes distress scale-2 | 5 | 1 | 2 | 8 |
| Matsuba et al[32] | Diabetes distress scale-25-item | 5 | 1 | 2 | 8 |
| Nguyen et al[33] | The 17-item diabetes distress scale | 5 | 1 | 1 | 8 |
| Pandit et al[12] | The 17-item diabetes distress scale | 5 | 2 | 2 | 9 |
| Park et al[34] | The problem areas in diabetes scale | 5 | 1 | 2 | 8 |
| Schmitt et al[35] | Center for epidemiologic studies depression scale, diabetes distress scale | 5 | 1 | 2 | 8 |
| Sidhu and Tang[36] | Diabetes distress scale, patient health questionnaire-9 | 5 | 1 | 2 | 8 |
| Totesora et al[37] | PAID-20 | 5 | 1 | 2 | 8 |
| Bhaskara et al[38] | Diabetes distress scale | 5 | 1 | 2 | 8 |
| Huynh et al[39] | Diabetes distress scale | 5 | 1 | 2 | 8 |
| Lim et al[40] | The problem area in diabetes | ||||
| Sasi et al[41] | Diabetes distress scale | 5 | 1 | 2 | 8 |
The HbA1c was used to measure glycemic control; some studies provide the number of patients with good glycemic control and do not provide the details of HbA1c and blood glucose levels.
The problem areas in diabetes, diabetes distress scale were used for the diagnosis of diabetes distress, while the patient health questionnaire-9, center for epidemiologic studies depression scale, psychological factors questionnaire, and severity of depressed/anxious mood [EuroQol (EQ)-5D item] were used for the diagnosis of depression (Table 4).
Diabetes distress was assessed by different-items problem areas in diabetes scale in references, while the different-items diabetes distress scale was used in references, and depression was evaluated by the patient health questionnaire-9, severity of depressed/anxious mood [EuroQol (EQ)-5D item] questionnaire, psychological factors questionnaire, and center for epidemiological studies-depression questionnaire.
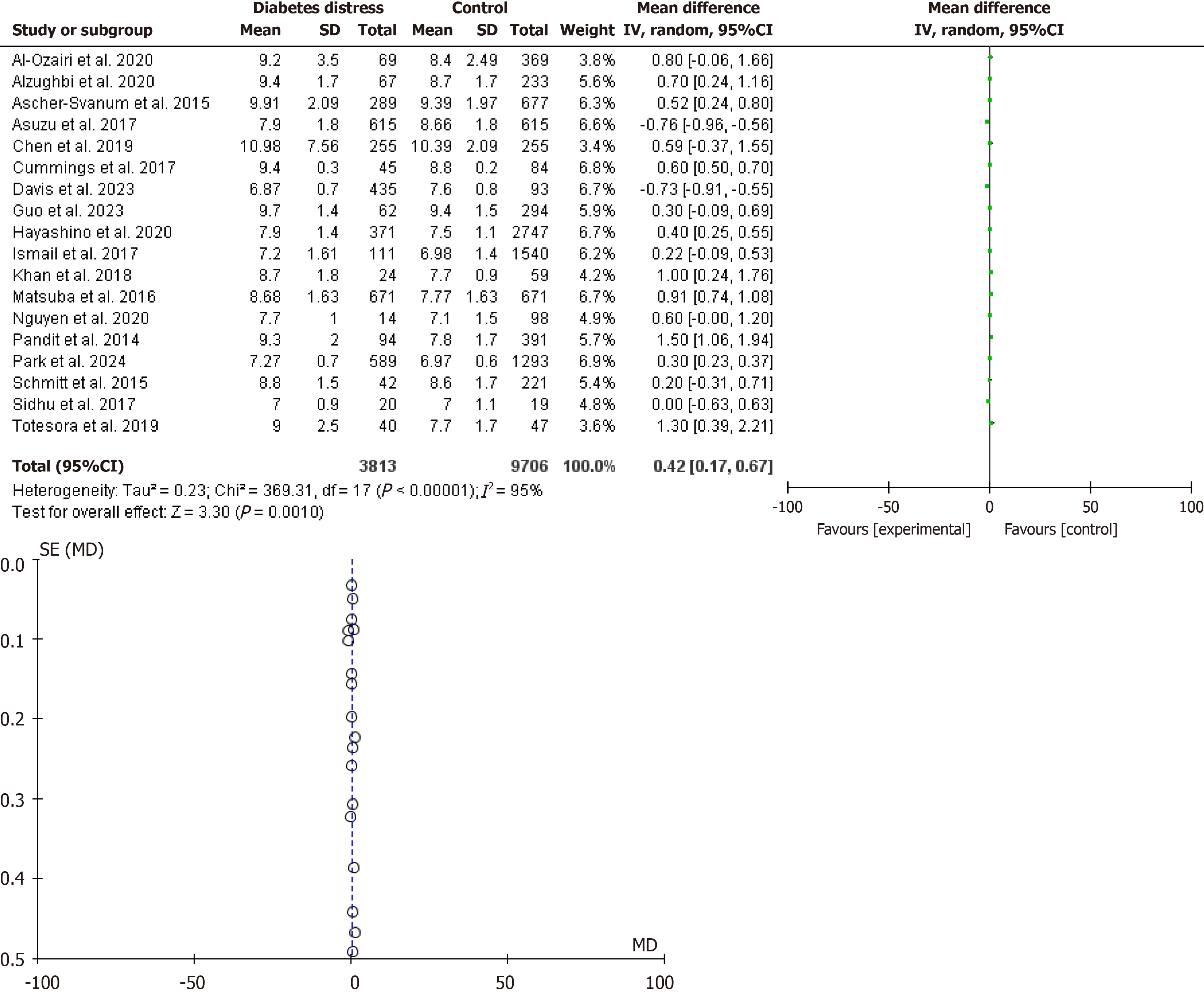
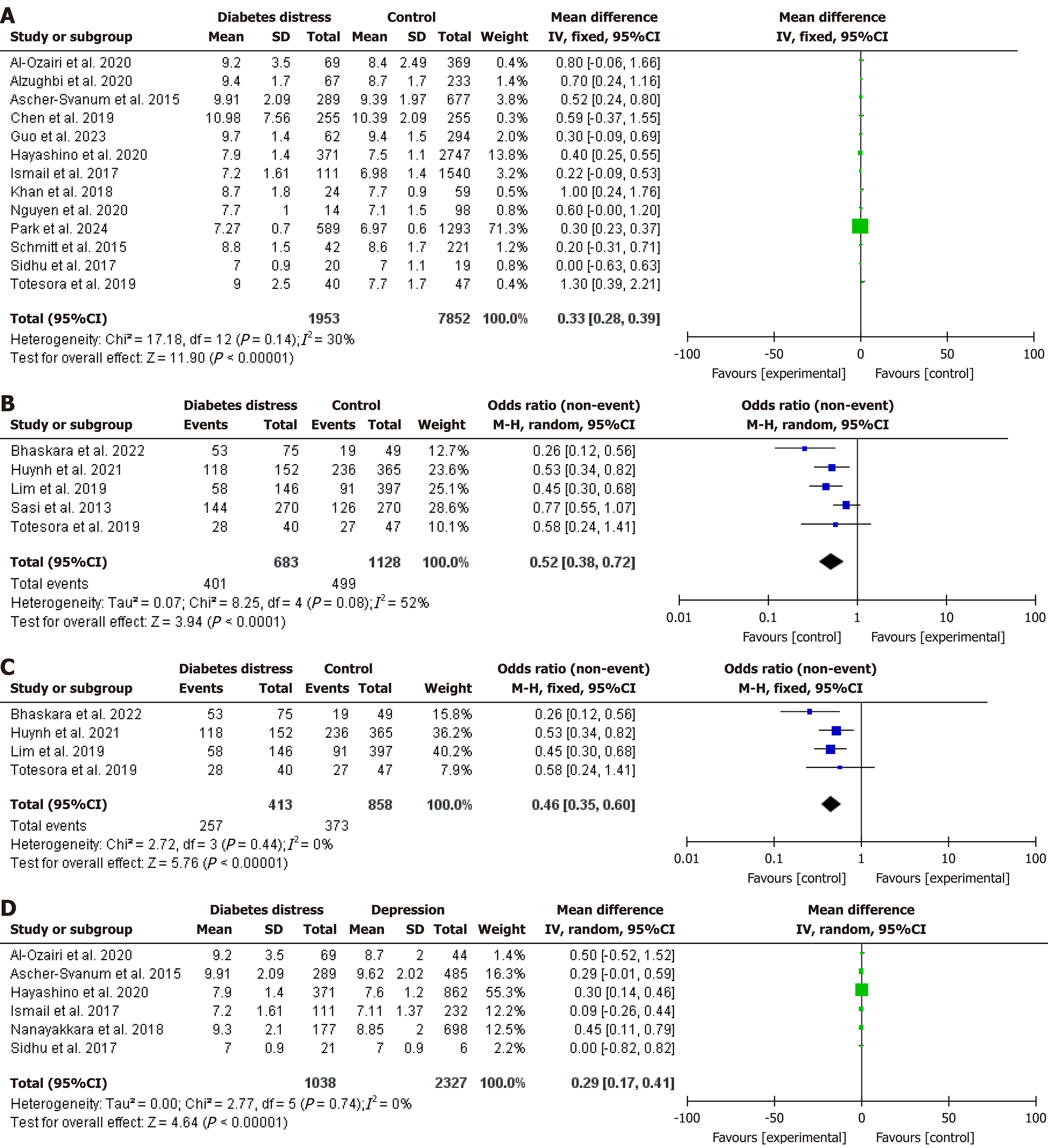
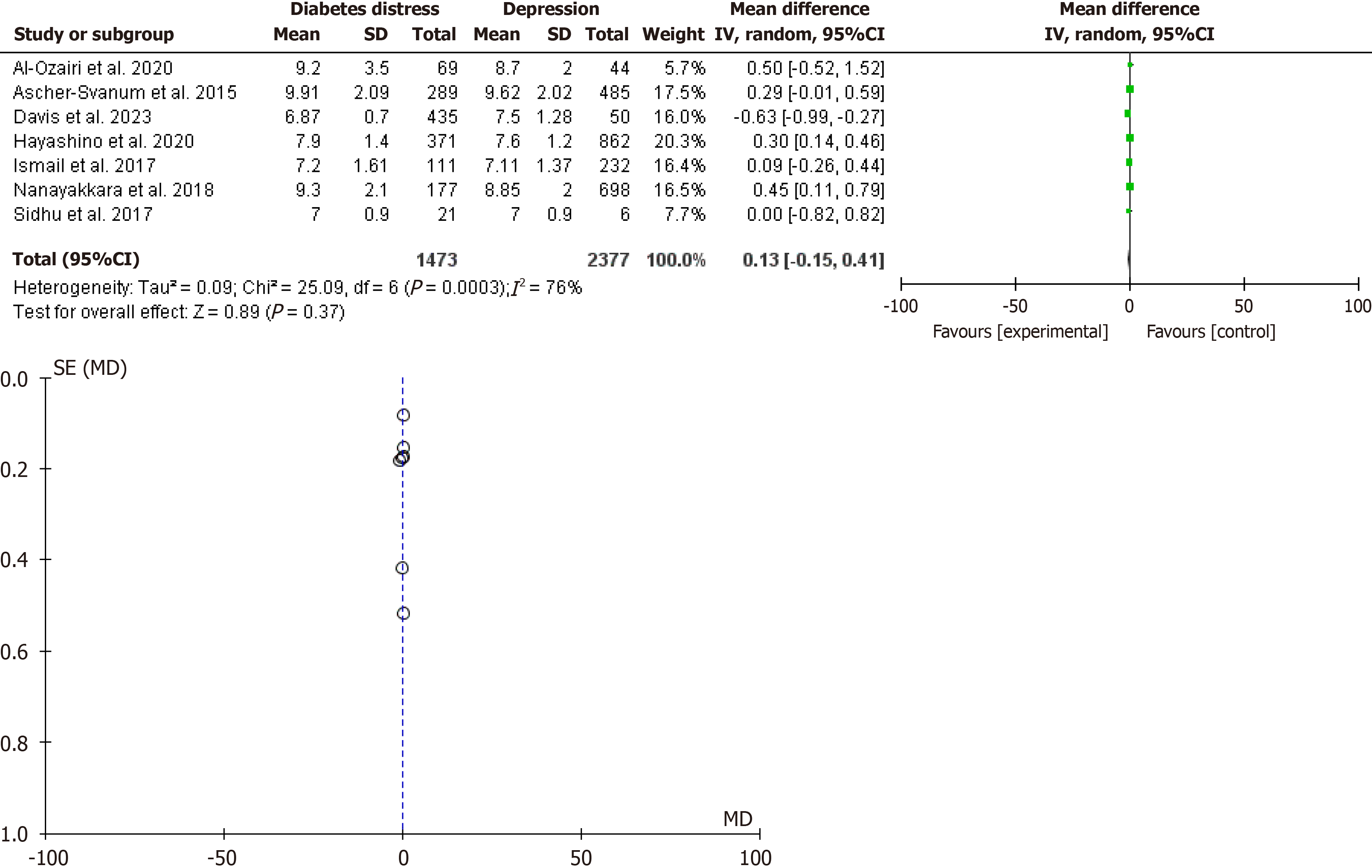
The data were analyzed by the most recent version of the RevMan system (5.4.1 United Kingdom). We pooled 30 cohorts to assess the effects of diabetes distress on glycemic control and HbA1c, of them 18 studies assessed the effects on HbA1c, five assessed glycemic control, and seven compared depression and diabetes distress regarding glycemic control. The dichotomous and continuous date data were entered manually and the fixed effect was used in the sub-analyses in Figure 3A, Figure 3C and D to address heterogeneity, while the random effect was applied when the heterogeneity was significant, Figure 2, Figure 3B, and Figure 4. A P value of < 0.05 was considered significant.
Out of the twenty-two studies included[12,21-41], five were prospective, two were retrospective studies, and fifteen were cross-sectional, fourteen studies were conducted in Asia, four from Europe, three from the United States, and one from Canada.
In the present meta-analysis, twenty-two studies were included (13519 patients with diabetes). The HbA1c was lower among patients without diabetes distress, odd ratio = 0.42, 95% confidence interval (CI): 0.17-0.67, χ2 = 269.31, and P value = 0.001. Substantial heterogeneity was observed, I2 for heterogeneity = 95%, P value for heterogeneity < 0.001 (Figure 2).
The negative effect of diabetes distress was maintained after the most possible elimination of heterogeneity, odd ratio = 0.39, 95%CI: 0.28-0.50, χ2 = 17.18, and P value < 0.001, I2 for heterogeneity = 30%, P value for heterogeneity = 0.14 (Figure 3A).
Five studies[37-41] assessed glycemic control collectively (only numbers were provided) and found poor glycemic control among patients with diabetes distress, odd ratio = 0.52, 95%CI: 0.38-0.72, χ2 = 8.25, and P value < 0.001. No significant heterogeneity was observed, I2 for heterogeneity = 52%, P value for heterogeneity = 0.08, and SD = 4 (Figure 3B). A sub-analysis to address heterogeneity was conducted, odd ratio = 0.46, 95%CI: 0.35-0.60, χ2 = 2.72, and P value < 0.001. No significant heterogeneity was observed, I2 for heterogeneity = 0%, P value for heterogeneity = 0.44, and SD = 4 (Figure 3C).
The relationship between diabetes distress, depression, and HbA1c showed contradicting results; seven studies[21,23,25,27,29,30,37] compared the effects of depression and diabetes distress (3850 patients with diabetes) and indicated no difference regarding their influence of the HbA1c, odd ratio = 0.13, 95%CI: 0.15-0.41, χ2 = 25.09, and P value = 0.37. A significant heterogeneity was observed, I2 for heterogeneity = 76%, P value for heterogeneity = 0.0003 (Figure 4). However, the results differ when heterogeneity was eliminated (6 studies remained with 3365 patients), diabetes distress negatively impacted the HbA1c substantially compared to depression, odd ratio = 0.29, 95%CI: 0.17-0.41, χ2 = 2.77, and P value < 0.001 (Figure 3D).
In the current meta-analysis, DRD was associated with higher HbA1c and poor glycemic control, odd ratio = 0.46, 95%CI: 0.26-0.66, and odd ratio = 0.52, 95%CI: 0.38-0.72 respectively. When comparing the effects of DRD and depression on the HbA1c; no significant statistical difference was found, odd ratio = 0.13, 95%CI: 0.15-0.41, the significant heterogeneity (I2 for heterogeneity = 76%), limited the above findings. Interestingly diabetes distress showed more negative effects on HbA1c compared to depression following a sub-analysis to eliminate the heterogeneity, odd ratio = 0.29, 95%CI: 0.17-0.41.
The above results imply that diabetes distress screening is vital for better glycemic control and lower rates of diabetes microvascular disease. On the other hand, diabetes distress is linked to fear of hypoglycemia. In addition, patients with diabetes distress and depression were more likely to have severe hypoglycemia than patients with diabetes distress alone[42-44]. Therefore, DRD is associated with fluctuating blood glucose with deleterious consequences. There is a piece of evidence suggesting the association between within-day and between-days glucose variability, oxidative stress, and diabetes complication[45], and Chen et al[46] found an association between glucose variability and mortality among acute coronary syndrome patients. Surprisingly, physicians usually ignore diabetes distress and do not frequently discuss it with the patients[47].
An interesting study found that people with persistently poor glycemic control had lower DRD than their counterparts with good glycemic status[48]. Therefore, psychological problems in interaction with blood glucose among patients with diabetes are complex and multidirectional. Some patients with diabetes might keep their blood glucose high to avoid hypoglycemia, thus, less attention is paid to diabetes care and they develop less DRD. Further explanations could be in the fact that hypoglycemia is not considered as a continuum of blood glucose and glycemic control is not interpreted in the light of clinical scenario[49,50].
Ehrmann and colleagues in their secondary analysis of the HypoDE Study found that contiguous glucose monitoring was an effective measure to improve glycemic control with no significant effect on diabetes distress[51]. A plausible explanation for the above findings might be living with a chronic disease seems to be more important than glycemic status at least in some. More explanation might be the reliance on HbA1c to assess the glycemic control because HbA1c retrospectively assesses mean serum glucose during the past 8-12 weeks. In contrast, continuous glucose monitoring provides more details including hypoglycemia and time in the range[52-54].
Depression, which is common among patients with diabetes, could play an important role in the effects of diabetes distress and glycemic control. Previous evidence suggested that diabetes distress mediated the poor glycemic control observed among patients with depression[55]; further studies showed that patients with diabetes distress and diabetes complications had higher rates of depression than their counterparts with distress or diabetes complications alone. However, the conclusion depends on observational studies[56,57]. This meta-analysis could potentially be the first to compare the effects of depression and diabetes distress on glycemic control and confirm the above observation. We found a greater influence on DRD compared to depression. Because DRD is commoner than depression, physicians might need to screen patients with diabetes and target diabetes distress to avoid microvascular complications. Our findings may improve the quality of diabetes care by shedding light on the significance of screening patients with diabetes for distress and depression. The current conclusion calls for collaboration with psychiatrists and psychologists for better outcomes in the face of the diabetes surge.
The strength of this meta-analysis is that it is the first to compare the effects of diabetes distress and depression on glycemic control. In addition, an updated view of diabetes distress’s influence on glycemic control was provided. However, the high heterogeneity observed limited this study. In addition, DRD and depression diagnoses were based on questionnaires that were more prone to subjectivity.
The use of questionnaires as measures of diabetes distress and depression inappropriately reflects the current situation and context. Questionnaires are prone to bias and give retrospective information irrespective of the frequency and duration of psychological distress[58,59]. Traditional questionnaires are shortcomings and cannot mirror the day-to-day variation of diabetes distress; ecological momentary assessment via smartphone can overcome the limitations of traditional questionnaires and reflect the extent and severity of diabetes distress[60]. The ecological momentary assessment reflects the varying degrees of DRD and diabetes burden contextually in contrast to the stable (trait-like) questionnaire evaluation. Therefore, combining ecological momentary assessment and continuous glucose monitoring reflects the real world of the psychological status of patients living with diabetes, and allows for an individualized approach[61,62]. Selecting which aspect of glycemic status (hyperglycemia, hypoglycemia, and glucose variability) is associated with diabetes distress is vital.
Diabetes distress was associated with poor glycemic control and higher HbA1c. Diabetes distress had a higher impact on glycemic control compared to depression. Physicians might need to screen for both depression and diabetes distress among patients with poor glycemic control. Further studies applying continuous glucose monitoring and ecological momentary assessment are needed to evaluate the association of diabetes distress, depression, and glycemic control. Future studies could also assess the overlap between depression symptoms and those of diabetes distress.
We would like to acknowledge Dr. Farah I, Biostatistician, Faculty of Science, Tabuk, Saudi Arabia for data analysis.
| 1. | ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Cusi K, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Leon J, Lyons SK, Perry ML, Prahalad P, Pratley RE, Seley JJ, Stanton RC, Gabbay RA; on behalf of the American Diabetes Association. 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S49-S67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 128] [Article Influence: 64.0] [Reference Citation Analysis (1)] |
| 2. | Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R; IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5345] [Cited by in RCA: 5874] [Article Influence: 979.0] [Reference Citation Analysis (8)] |
| 3. | Hiasat DA, Salih MB, Abu Jaber AH, Abubaker OF, Qandeel YA, Saleem BA, Aburumman SI, Al-Sayyed ARH, Hussein TI, Hyassat D. The prevalence of diabetes distress among patients with type 2 diabetes in Jordan. J Taibah Univ Med Sci. 2023;18:1237-1243. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Luzuriaga M, Leite R, Ahmed H, Saab PG, Garg R. Complexity of antidiabetic medication regimen is associated with increased diabetes-related distress in persons with type 2 diabetes mellitus. BMJ Open Diabetes Res Care. 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Khashayar P, Shirzad N, Zarbini A, Esteghamati A, Hemmatabadi M, Sharafi E. Diabetes-related distress and its association with the complications of diabetes in Iran. J Diabetes Metab Disord. 2022;21:1569-1575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 6. | Boehmer K, Lakkad M, Johnson C, Painter JT. Depression and diabetes distress in patients with diabetes. Prim Care Diabetes. 2023;17:105-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 7. | Grulovic N, Rojnic Kuzman M, Baretic M. Prevalence and predictors of diabetes-related distress in adults with type 1 diabetes. Sci Rep. 2022;12:15758. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 8. | Mirghani HO. An evaluation of adherence to anti-diabetic medications among type 2 diabetic patients in a Sudanese outpatient clinic. Pan Afr Med J. 2019;34:34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Fayed A, AlRadini F, Alzuhairi RM, Aljuhani AE, Alrashid HR, Alwazae MM, Alghamdi NR. Relation between diabetes related distress and glycemic control: The mediating effect of adherence to treatment. Prim Care Diabetes. 2022;16:293-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 10. | Devarajooh C, Chinna K. Depression, distress and self-efficacy: The impact on diabetes self-care practices. PLoS One. 2017;12:e0175096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 11. | Snoek FJ, Bremmer MA, Hermanns N. Constructs of depression and distress in diabetes: time for an appraisal. Lancet Diabetes Endocrinol. 2015;3:450-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 293] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 12. | Pandit AU, Bailey SC, Curtis LM, Seligman HK, Davis TC, Parker RM, Schillinger D, DeWalt D, Fleming D, Mohr DC, Wolf MS. Disease-related distress, self-care and clinical outcomes among low-income patients with diabetes. J Epidemiol Community Health. 2014;68:557-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 82] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 13. | Nanayakkara N, Pease A, Ranasinha S, Wischer N, Andrikopoulos S, Speight J, de Courten B, Zoungas S. Depression and diabetes distress in adults with type 2 diabetes: results from the Australian National Diabetes Audit (ANDA) 2016. Sci Rep. 2018;8:7846. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 86] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 14. | Jenkinson E, Knoop I, Hudson JL, Moss-Morris R, Hackett RA. The effectiveness of cognitive behavioural therapy and third-wave cognitive behavioural interventions on diabetes-related distress: A systematic review and meta-analysis. Diabet Med. 2022;39:e14948. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Perrin N, Bodicoat DH, Davies MJ, Robertson N, Snoek FJ, Khunti K. Effectiveness of psychoeducational interventions for the treatment of diabetes-specific emotional distress and glycaemic control in people with type 2 diabetes: A systematic review and meta-analysis. Prim Care Diabetes. 2019;13:556-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 16. | Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. 2014;14:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 770] [Cited by in RCA: 1626] [Article Influence: 147.8] [Reference Citation Analysis (0)] |
| 17. | Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care. 2000;23:934-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1160] [Cited by in RCA: 1165] [Article Influence: 46.6] [Reference Citation Analysis (0)] |
| 18. | Harding KA, Pushpanathan ME, Whitworth SR, Nanthakumar S, Bucks RS, Skinner TC. Depression prevalence in Type 2 diabetes is not related to diabetes-depression symptom overlap but is related to symptom dimensions within patient self-report measures: a meta-analysis. Diabet Med. 2019;36:1600-1611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Beran M, Muzambi R, Geraets A, Albertorio-Diaz JR, Adriaanse MC, Iversen MM, Kokoszka A, Nefs G, Nouwen A, Pouwer F, Huber JW, Schmitt A, Schram MT; European Depression in Diabetes (EDID) Research Consortium. The bidirectional longitudinal association between depressive symptoms and HbA(1c) : A systematic review and meta-analysis. Diabet Med. 2022;39:e14671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 41] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 20. | Brown SA, García AA, Brown A, Becker BJ, Conn VS, Ramírez G, Winter MA, Sumlin LL, Garcia TJ, Cuevas HE. Biobehavioral determinants of glycemic control in type 2 diabetes: A systematic review and meta-analysis. Patient Educ Couns. 2016;99:1558-1567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 21. | Al-Ozairi E, Al Ozairi A, Blythe C, Taghadom E, Ismail K. The Epidemiology of Depression and Diabetes Distress in Type 2 Diabetes in Kuwait. J Diabetes Res. 2020;2020:7414050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Alzughbi T, Badedi M, Darraj H, Hummadi A, Jaddoh S, Solan Y, Sabai A. Diabetes-Related Distress and Depression in Saudis with Type 2 Diabetes. Psychol Res Behav Manag. 2020;13:453-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 23. | Ascher-Svanum H, Zagar A, Jiang D, Schuster D, Schmitt H, Dennehy EB, Kendall DM, Raskin J, Heine RJ. Associations Between Glycemic Control, Depressed Mood, Clinical Depression, and Diabetes Distress Before and After Insulin Initiation: An Exploratory, Post Hoc Analysis. Diabetes Ther. 2015;6:303-316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Asuzu CC, Walker RJ, Williams JS, Egede LE. Pathways for the relationship between diabetes distress, depression, fatalism and glycemic control in adults with type 2 diabetes. J Diabetes Complications. 2017;31:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 25. | Chen SY, Hsu HC, Wang RH, Lee YJ, Hsieh CH. Glycemic Control in Insulin-Treated Patients With Type 2 Diabetes: Empowerment Perceptions and Diabetes Distress as Important Determinants. Biol Res Nurs. 2019;21:182-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Cummings DM, Lutes LD, Littlewood K, Solar C, Hambidge B, Gatlin P. Impact of Distress Reduction on Behavioral Correlates and A1C in African American Women with Uncontrolled Type 2 Diabetes: Results from EMPOWER. Ethn Dis. 2017;27:155-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Davis WA, Bruce DG, Davis TME, Starkstein SE. The Clinical Relevance of Diabetes Distress versus Major Depression in Type 2 Diabetes: A Latent Class Analysis from the Fremantle Diabetes Study Phase II. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 28. | Guo X, Wong PNF, Koh YLE, Tan NC. Factors associated with diabetes-related distress among Asian patients with poorly controlled type-2 diabetes mellitus: a cross-sectional study in primary care. BMC Prim Care. 2023;24:54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 29. | Hayashino Y, Okamura S, Tsujii S, Ishii H; Diabetes Distress and Care Registry at Tenri Study Group. The joint association of diabetes distress and depressive symptoms with all-cause mortality in Japanese individuals with type 2 diabetes: a prospective cohort study (Diabetes Distress and Care Registry in Tenri [DDCRT 20]). Diabetologia. 2020;63:2595-2604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Ismail K, Moulton CD, Winkley K, Pickup JC, Thomas SM, Sherwood RA, Stahl D, Amiel SA. The association of depressive symptoms and diabetes distress with glycaemic control and diabetes complications over 2 years in newly diagnosed type 2 diabetes: a prospective cohort study. Diabetologia. 2017;60:2092-2102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 31. | Khan A, Choudhary P. Investigating the Association Between Diabetes Distress and Self-Management Behaviors. J Diabetes Sci Technol. 2018;12:1116-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Matsuba I, Sawa T, Kawata T, Kanamori A, Jiang D, Machimura H, Takeda H, Han JH, Wang K, Tanaka K, Shen L, Ajima M, Kaneshiro M, Kim SW, Umezawa S, Asakura T, Suzuki S, Kim SC. Cross-National Variation in Glycemic Control and Diabetes-Related Distress Among East Asian Patients Using Insulin: Results from the MOSAIc Study. Diabetes Ther. 2016;7:349-360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Nguyen VB, Tran TT, Dang TL, Nguyen VVH, Tran BT, Le CV, Toan ND. Diabetes-Related Distress and Its Associated Factors Among Patients with Diabetes in Vietnam. Psychol Res Behav Manag. 2020;13:1181-1189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 34. | Park HS, Cho Y, Seo DH, Ahn SH, Hong S, Suh YJ, Chon S, Woo JT, Baik SH, Lee KW, Kim SH. Impact of diabetes distress on glycemic control and diabetic complications in type 2 diabetes mellitus. Sci Rep. 2024;14:5568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 35. | Schmitt A, Reimer A, Kulzer B, Haak T, Gahr A, Hermanns N. Negative association between depression and diabetes control only when accompanied by diabetes-specific distress. J Behav Med. 2015;38:556-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 36. | Sidhu R, Tang TS. Diabetes Distress and Depression in South Asian Canadians with Type 2 Diabetes. Can J Diabetes. 2017;41:69-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 37. | Totesora D, Ramos-Rivera MI, Villegas-Florencio MQ, Reyes-Sia PN. Association of Diabetes-related Emotional Distress with Diabetes Self-care and Glycemic Control among Adult Filipinos with Type 2 Diabetes Mellitus at a Tertiary Hospital in Manila, Philippines. J ASEAN Fed Endocr Soc. 2019;34:189-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 38. | Bhaskara G, Budhiarta AAG, Gotera W, Saraswati MR, Dwipayana IMP, Semadi IMS, Nugraha IBA, Wardani IAK, Suastika K. Factors Associated with Diabetes-Related Distress in Type 2 Diabetes Mellitus Patients. Diabetes Metab Syndr Obes. 2022;15:2077-2085. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 39. | Huynh G, Tran TT, Do THT, Truong TTD, Ong PT, Nguyen TNH, Pham LA. Diabetes-Related Distress Among People with Type 2 Diabetes in Ho Chi Minh City, Vietnam: Prevalence and Associated Factors. Diabetes Metab Syndr Obes. 2021;14:683-690. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 40. | Lim SM, Siaw MYL, Tsou KYK, Kng KK, Lee JY. Risk factors and quality of life of patients with high diabetes-related distress in primary care: a cross-sectional, multicenter study. Qual Life Res. 2019;28:491-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 41. | Sasi ST, Kodali M, Burra KC, Muppala BS, Gutta P, Bethanbhatla MK. Self Care Activities, Diabetic Distress and other Factors which Affected the Glycaemic Control in a Tertiary Care Teaching Hospital in South India. J Clin Diagn Res. 2013;7:857-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 42. | Pieri BA, Bergin-Cartwright GAI, Simpson A, Collins J, Reid A, Karalliedde J, Brackenridge A, Hotopf M, Hussain S. Symptoms of Anxiety and Depression Are Independently Associated With Impaired Awareness of Hypoglycemia in Type 1 Diabetes. Diabetes Care. 2022;45:2456-2460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 43. | Al Sayah F, Yeung RO, Johnson JA. Association of Depressive Symptoms and Diabetes Distress With Severe Hypoglycemia in Adults With Type 2 Diabetes. Can J Diabetes. 2019;43:316-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 44. | Schmidt CB, van Loon BJP, Vergouwen ACM, Snoek FJ, Honig A. Systematic review and meta-analysis of psychological interventions in people with diabetes and elevated diabetes-distress. Diabet Med. 2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 105] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 45. | Martinez M, Santamarina J, Pavesi A, Musso C, Umpierrez GE. Glycemic variability and cardiovascular disease in patients with type 2 diabetes. BMJ Open Diabetes Res Care. 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 87] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 46. | Chen J, Huang W, Liang N. Blood glucose fluctuation and in-hospital mortality among patients with acute myocardial infarction: eICU collaborative research database. PLoS One. 2024;19:e0300323. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 47. | Byrne JL, Davies MJ, Willaing I, Holt RIG, Carey ME, Daly H, Skovlund S, Peyrot M. Deficiencies in postgraduate training for healthcare professionals who provide diabetes education and support: results from the Diabetes Attitudes, Wishes and Needs (DAWN2) study. Diabet Med. 2017;34:1074-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 48. | Bazelmans E, Netea-Maier RT, Vercoulen JH, Tack CJ. Surprisingly few psychological problems and diabetes-related distress in patients with poor glycaemic control. Neth J Med. 2016;74:16-21. [PubMed] |
| 49. | Güemes M, Rahman SA, Hussain K. What is a normal blood glucose? Arch Dis Child. 2016;101:569-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 116] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 50. | McCall AL, Lieb DC, Gianchandani R, MacMaster H, Maynard GA, Murad MH, Seaquist E, Wolfsdorf JI, Wright RF, Wiercioch W. Management of Individuals With Diabetes at High Risk for Hypoglycemia: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2023;108:529-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 48] [Reference Citation Analysis (0)] |
| 51. | Ehrmann D, Heinemann L, Freckmann G, Waldenmaier D, Faber-Heinemann G, Hermanns N. The Effects and Effect Sizes of Real-Time Continuous Glucose Monitoring on Patient-Reported Outcomes: A Secondary Analysis of the HypoDE Study. Diabetes Technol Ther. 2019;21:86-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 52. | Pinsker JE, Müller L, Constantin A, Leas S, Manning M, McElwee Malloy M, Singh H, Habif S. Real-World Patient-Reported Outcomes and Glycemic Results with Initiation of Control-IQ Technology. Diabetes Technol Ther. 2021;23:120-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 105] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 53. | Jackson MA, Ahmann A, Shah VN. Type 2 Diabetes and the Use of Real-Time Continuous Glucose Monitoring. Diabetes Technol Ther. 2021;23:S27-S34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 51] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 54. | Yazdanpanah S, Rabiee M, Tahriri M, Abdolrahim M, Rajab A, Jazayeri HE, Tayebi L. Evaluation of glycated albumin (GA) and GA/HbA1c ratio for diagnosis of diabetes and glycemic control: A comprehensive review. Crit Rev Clin Lab Sci. 2017;54:219-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 126] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 55. | Fisher L, Gonzalez JS, Polonsky WH. The confusing tale of depression and distress in patients with diabetes: a call for greater clarity and precision. Diabet Med. 2014;31:764-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 309] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 56. | Yang QQ, Sun JW, Shao D, Zhang HH, Bai CF, Cao FL. The Association between Diabetes Complications, Diabetes Distress, and Depressive Symptoms in Patients with Type 2 Diabetes Mellitus. Clin Nurs Res. 2021;30:293-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 57. | Gonzalez JS, Delahanty LM, Safren SA, Meigs JB, Grant RW. Differentiating symptoms of depression from diabetes-specific distress: relationships with self-care in type 2 diabetes. Diabetologia. 2008;51:1822-1825. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 86] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 58. | Solhan MB, Trull TJ, Jahng S, Wood PK. Clinical assessment of affective instability: comparing EMA indices, questionnaire reports, and retrospective recall. Psychol Assess. 2009;21:425-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 241] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 59. | Schmitt A, Bendig E, Baumeister H, Hermanns N, Kulzer B. Associations of depression and diabetes distress with self-management behavior and glycemic control. Health Psychol. 2021;40:113-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 60. | Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2845] [Cited by in RCA: 3471] [Article Influence: 204.2] [Reference Citation Analysis (0)] |
| 61. | McDonald S, Quinn F, Vieira R, O'Brien N, White M, Johnston DW, Sniehotta FF. The state of the art and future opportunities for using longitudinal n-of-1 methods in health behaviour research: a systematic literature overview. Health Psychol Rev. 2017;11:307-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 98] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 62. | Weiss GB. Phospholipids, calcium binding and arterial smooth muscle membranes. Prog Clin Biol Res. 1986;219:123-132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 33] [Article Influence: 11.0] [Reference Citation Analysis (0)] |