Published online Mar 6, 2021. doi: 10.12998/wjcc.v9.i7.1654
Peer-review started: August 9, 2020
First decision: December 14, 2020
Revised: December 14, 2020
Accepted: January 22, 2021
Article in press: January 22, 2021
Published online: March 6, 2021
Processing time: 203 Days and 22.2 Hours
Primary non-Hodgkin’s lymphoma of the frontal sinus is extremely rare. In addition, Epstein-Barr virus (EBV) has been reported to play a role in the development of human immunodeficiency virus (HIV)-related malignant lymphomas. To the best of our knowledge, there is no report for the HIV-associated, EBV-positive primary diffuse large B-cell lymphoma (DLBCL) in the frontal sinus.
We present a unique case of HIV-associated, EBV-positive DLBCL in the frontal sinus in a 46-year-old man. Computed tomography of paranasal sinuses revealed dense opacification of the right frontal sinus with combined soft tissue swelling. Based on the clinical and radiological findings, the initial diagnosis was complicated frontal sinusitis, presenting Pott’s puffy tumor. Unexpectedly, HIV testing was positive on preoperative laboratory test, and the frontal sinus lesion was confirmed as EBV-positive DLBCL on biopsy.
Through this article, we suggest that EBV-positive DLBCL should be considered as possible diagnosis for patients with nonspecific space-occupying lesion of the paranasal sinuses. We also highlight an importance of clinical suspicion in diagnosing HIV infection because HIV serology is not routinely tested in patients with paranasal sinus problem.
Core Tip: Primary diffuse large B-cell lymphoma in the frontal sinus is extremely rare. It can mimic complicated sinusitis and may be easily overlooked at the initial diagnostic workflow in the clinical practice. When we meet the frontal sinus opacification with combined overlying soft tissue swelling, it is important for the radiologists and clinicians to include the following disease entity in the differential diagnosis based on imaging findings; complicated sinusitis (Pott’s puffy tumor), unilateral non-Hodgkin’s lymphoma and destructive metastasis. Awareness and clinical suspicion of this disease are necessary for making an accurate diagnosis and appropriate treatment, particularly in patients with a history of sinusitis which does not response to medical treatment, or in human immunodeficiency virus-positive patients.
- Citation: Yoon S, Ryu KH, Baek HJ, An HJ, Joo YH. Epstein-Barr virus-positive diffuse large B-cell lymphoma with human immunodeficiency virus mimicking complicated frontal sinusitis: A case report. World J Clin Cases 2021; 9(7): 1654-1660
- URL: https://www.wjgnet.com/2307-8960/full/v9/i7/1654.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i7.1654
Primary non-Hodgkin’s lymphoma (NHL) in the nasal cavity and paranasal sinuses is very rare[1-3]. Of these, diffuse large B-cell lymphoma (DLBCL) is the most common subtype worldwide; however, to date, only 18 cases of primary DLBCL in the frontal sinus have been reported in the literature[4-8]. In addition, malignant lymphomas occur higher rates in patients with human immunodeficiency virus (HIV) infection compared with the general population, and the most common subtype is DLBCL[9,10]. Also, Epstein-Barr virus (EBV) has been reported to play a role in the development of HIV-related malignant lymphomas, and has been identified in 30%-90% of DLBCL[11]. Although 18 cases of primary DLBCL in the frontal sinus have been reported[4-8], there is no report for the HIV-associated, EBV-positive DLBCL in the frontal sinus with its radiological findings. Herein, we share our experience with a unique case of the HIV-associated, EBV-positive DLBCL in the frontal sinus, mimicking complicated sinusitis because of its atypical imaging feature in immunocompromised patient. We also highlight the importance of clinical suspicion in diagnosing HIV-associated lymphoma in patients with a paranasal sinus problem.
A 44-year-old male presented with the right forehead pain.
He had right forehead pain for 1 mo, and soft tissue swelling in the right forehead and right ptosis for 2 wk.
His medical history was unremarkable and there was no history of fever and palpable cervical lymphadenopathy, but he described mild weight loss and fatigue.
The patient’s personal and family history was unremarkable.
Physical examination revealed hard, immobile, tender mass on his right forehead.
His laboratory findings showed increased erythrocyte sedimentation rate (ESR, 108 mm/h; normal range, 0-9 mm/h) and C-reactive protein (CRP, 7.4 mg/L; normal range 0.0-5.0 mg/L) with mild anemia and slightly decreased count of white blood cell.
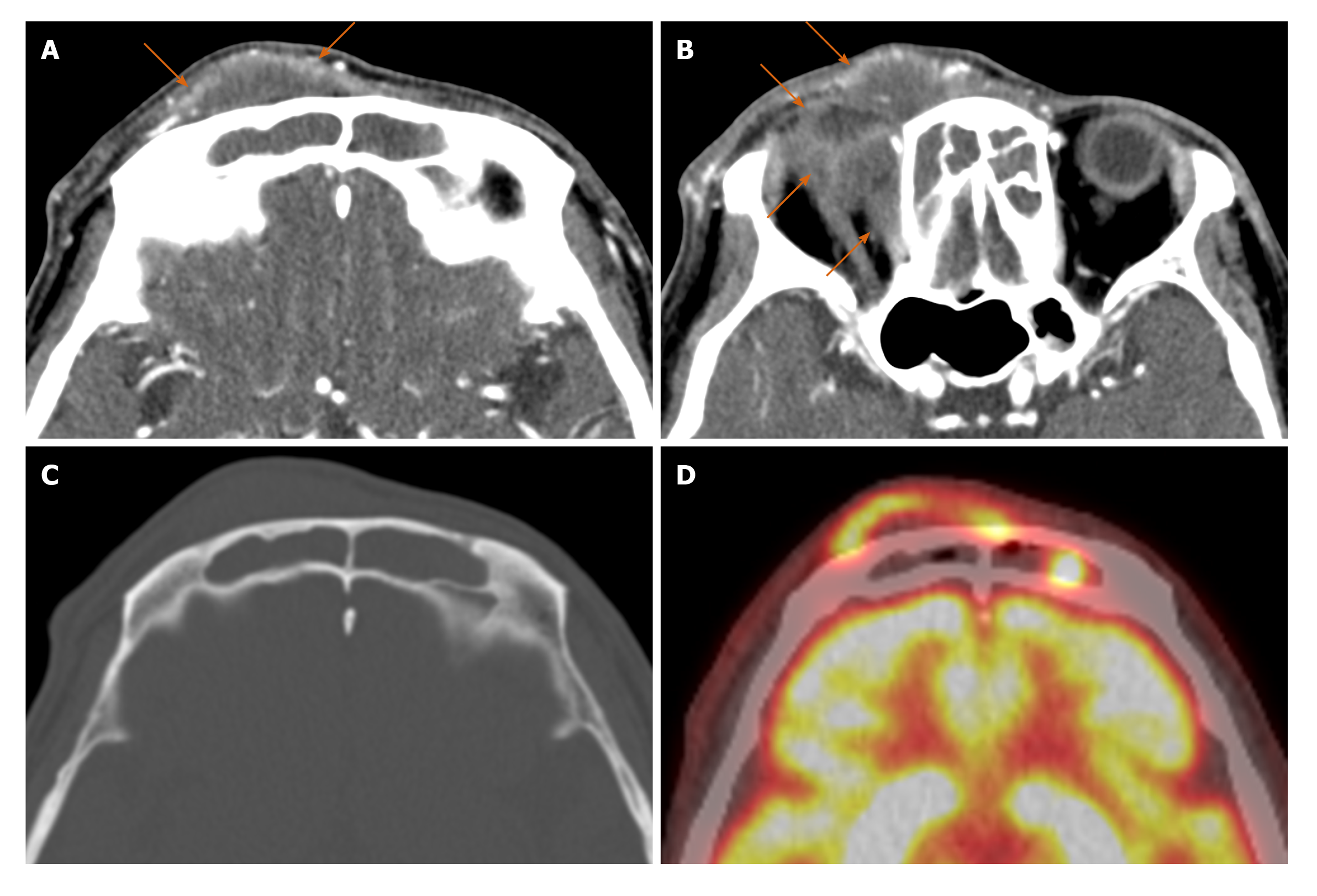
Computed tomography (CT) of paranasal sinuses was performed and the images revealed dense opacification of the right frontal sinus with combined soft tissue swelling (Figure 1A-C). There was minimal bony erosion in the anterior wall of the right frontal sinus without enhancing solid component. Based on the clinical and radiological findings, the initial diagnosis was complicated frontal sinusitis, presenting Pott’s puffy tumor.
On preoperative laboratory tests, we found that his HIV testing was positive. HIV-1 RNA quantification (real-time polymerase chain reaction) revealed HIV-1 RNA was 3.31 × 105 copies/mL (normal range < 20) and 5.627 × 105 IU/mL (normal range < 34). Lymphocyte subset test showed CD4 13.2%, CD3 84.3%, CD8 66.4% with white blood cell 3.44 × 103/µL, and lymphocyte 32.3%. His CD4 lymphocyte count was 147 cells/µL. Antiretroviral therapy was initiated with a combination of tenofovir alafenamide, elvitegravir, emtricitabine and cobicistat. Co-trimoxazole and acyclovir were administered for prophylaxis of opportunistic infections.
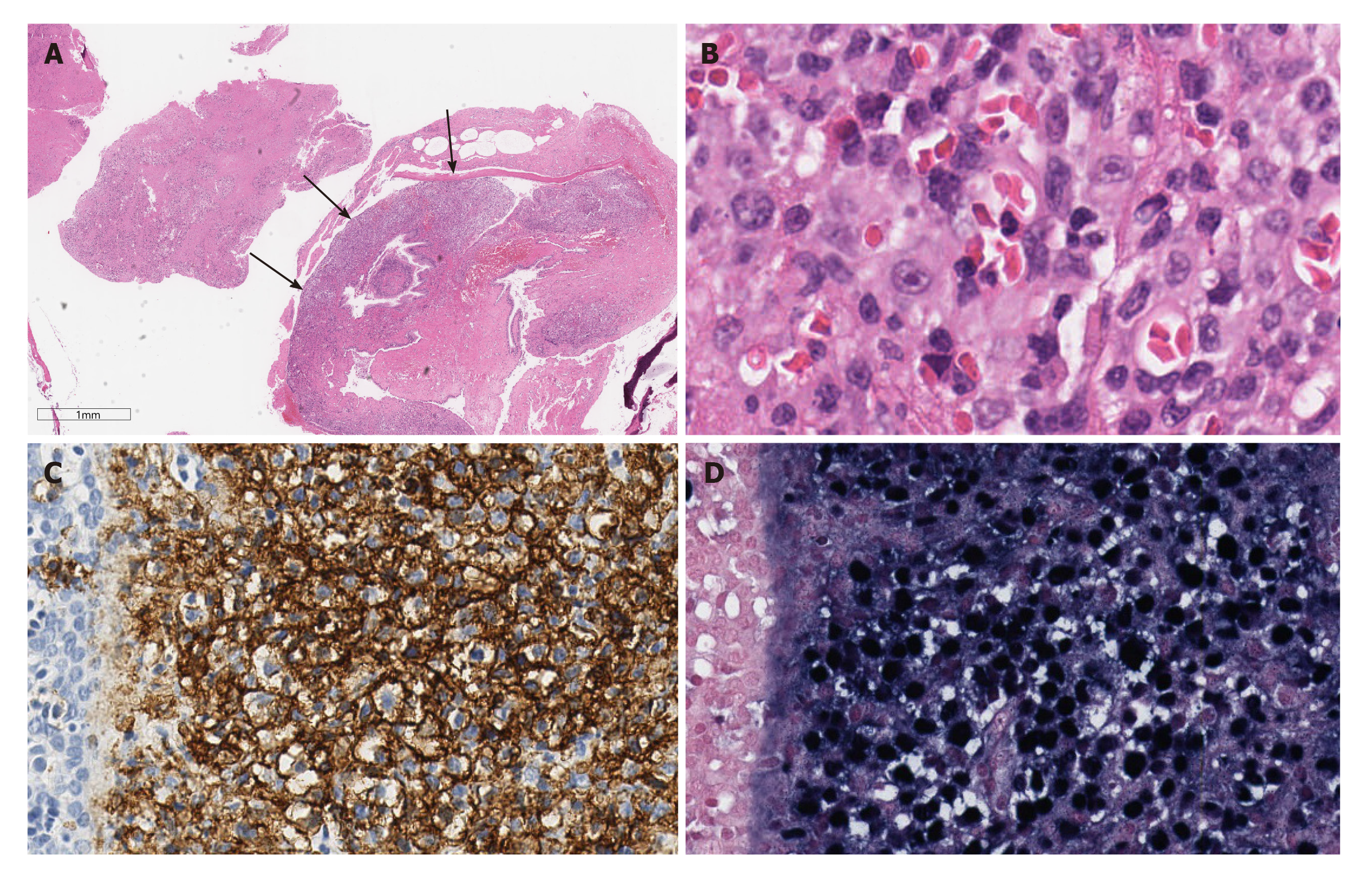
Then, biopsy was performed by endoscopic sinus surgery under general anesthesia to rule out malignant tumor. The histopathological examination showed an infiltrate of large atypical lymphocytes associated with necrosis, and admixed small lymphocyte. Immunohistochemical staining results showed large atypical lymphoid cells expressing CD20, BCL-2 (90%), CD79a, Ki-67 (80%) and MUM-1 (35%) (Figure 2). ALK1, BCL-6, CD3, CD5, CD10, CD15, CD30, CD56, CD138, Granzyme B, PAS and GMS were negative. In situ hybridization for EBV was positive, and the result of polymerase chain reaction test for EBV was also positive in the specimen, showing 1.70 × 104 copies/mL. Finally, the lesion was confirmed as EBV-positive DLBCL.
Additional F-18 fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT was performed for evaluating initial stage, and the lesions showed high FDG uptake with maximum standardized uptake value of 14.4 g/mL (Figure 1D). There was no significant hypermetabolic lesion to suggest lymphoma involvement beneath the diaphragm on F-18 FDG PET/CT. He was at stage II according to the Ann Arbor staging system, and international prognostic index was 1 point.
EBV-positive DLBCL in frontal sinus.
The patient underwent chemotherapy for treatment of DLBCL.
About 4 mo after the diagnosis of EBV-positive DLBCL, the patient passed away in 2 wk of chemotherapy from pneumonia and sepsis by cytomegalovirus infection.
Primary malignancies in the frontal sinus are rare, reportedly accounting for about 1.0% of sinonasal malignancies[12]. In the previous study[12], squamous cell neoplasm was the most common histologic subtype (39.8%), followed by NHL (18.7%), epithelial neoplasm not otherwise specified (10.5%) and adenocarcinoma (9.9%). Manifestations of frontal sinus malignancies are often nonspecific, thus leading to a misdiagnosis for benign diseases such as sinusitis, mucocele, or osteomyelitis. It is known that the overall prognosis for patients with frontal sinus malignancies was poor, with a 5-year survival rate of 31%-50%[13].
Of the primary sinonasal malignancies, NHL is rare, estimated to be between 0.2% and 2.0% of all NHLs[1,2]. Most of them occur in the maxillary sinuses, followed by the ethmoid sinuses and the nasal cavity. NHL in frontal sinus is an extremely rare condition[3]. DLBCL is the most common subtype of NHL worldwide, generally representing 30%-40% of all cases in different geographic regions[8]. To date, only 18 cases of primary DLBCL in the frontal sinus have been reported in the existing English-language literature[4-7]. Therefore, knowledge of the frontal sinus DLBCL is limited.
Diagnosis of paranasal lymphoma is usually delayed in daily practice because the early stage is often asymptomatic or nonspecific, and a complete investigation is postponed until the tumor mass produces obvious symptoms[14]. The previous studies demonstrated that clinical manifestation of DLBCL in the frontal sinus were common symptoms owing to the direct effect of tumor mass such as frontal headache, facial swelling, nasal discharge or nasal obstruction[4-7]. In the previous studies, imaging findings showed nonspecific opacification of the involved sinus with or without expansion or enhancement. In the current case, CT images demonstrated dense opacification of the right frontal sinus with minimal bony erosion and combined overlying soft tissue swelling, but with no definitely enhancing component. These findings were common radiological features of complicated sinusitis, therefore, not leading to a diagnosis of malignant lymphoma. In addition to CT findings, increased ESR and CRP of serum inflammatory markers made the diagnosis more indicative of nontumorous inflammatory conditions in our case.
In addition, it is well-known that HIV-infected patients have higher rates of malignant lymphomas compared with the general population, and DLBCL is the most common subtype of lymphoma in HIV patients[9,10]. HIV contributes to lympho-magenesis by several different mechanisms as follows: genetic alterations, induction of chronic B-cell activation by immune dysfunction, and loss of immunoregulatory control of oncogenic herpesviruses like EBV and Kaposi sarcoma-associated herpes-virus[15]. In addition, EBV, also known as human herpesvirus 4, is one of the most common human viruses, with about 95% of the world’s population showing an asymptomatic life-long carrier status. EBV infects memory B cells, which are the EBV reservoir in healthy individuals, and the disruption of this regulated balance between virus and host immune system can result in EBV-associated B cell lympho-proliferation[16]. In HIV patients, EBV has been reported to play a role in the development of HIV-related malignant lymphomas which has been identified in 30%-90% of DLBCL[11,17-19]. On imaging study, most EBV-related lymphomas show atypical image features including propensity for extranodal involvement and extensive tumor necrosis[20]. Therefore, EBV-related sinonasal lymphoma is more difficult to diagnose on imaging study owing to its atypical imaging features as in this case, compared to typical lymphoma that exhibit homogeneous nature. In the present case, we found that HIV testing was positive on preoperative laboratory tests before the endoscopic sinus biopsy. In addition to clinical rarity of the primary frontal sinus DLBCL, our case suggests that clinical suspicion is the most important for diagnosing HIV-associated, EBV-positive DLBCL because HIV serology is not routinely tested in patients with paranasal sinus problem.
DLBCL is very rare but can occur in the frontal sinus. Like the present case, it can mimic complicated sinusitis and may be easily overlooked at the initial diagnostic workflow in the clinical practice. When we meet the frontal sinus opacification with combined overlying soft tissue swelling, it is important for the radiologists and clinicians to include the following disease entity in the differential diagnosis based on imaging findings; complicated sinusitis (Pott’s puffy tumor), unilateral NHL and destructive metastasis. Awareness and clinical suspicion of this disease are necessary for making an accurate diagnosis and appropriate treatment, particularly in patients with a history of sinusitis which does not respond to medical treatment, or in HIV-positive patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhuo ZQ S-Editor: Chen XF L-Editor: A P-Editor: Wang LYT
| 1. | Fellbaum C, Hansmann ML, Lennert K. Malignant lymphomas of the nasal cavity and paranasal sinuses. Virchows Arch A Pathol Anat Histopathol. 1989;414:399-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 78] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Cleary KR, Batsakis JG. Sinonasal lymphomas. Ann Otol Rhinol Laryngol. 1994;103:911-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 65] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Quraishi MS, Bessell EM, Clark D, Jones NS, Bradley PJ. Non-Hodgkin's lymphoma of the sinonasal tract. Laryngoscope. 2000;110:1489-1492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 66] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Yang JP, Hu CM, Zhong W, Wang ZG. Primary diffuse large B-cell lymphoma of the frontal sinus. J Biol Regul Homeost Agents. 2017;31:447-451. [PubMed] |
| 5. | Knudson SA, Day KM, Harshbarger RJ. Pediatric Diffuse Large B-Cell Lymphoma of the Frontal Sinus: A Case Report. Cleft Palate Craniofac J. 2019;56:1089-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Khan NR, Lakičević G, Callihan TR, Burruss G, Arnautović K. Diffuse Large B-Cell Lymphoma of the Frontal Sinus Presenting as a Pott Puffy Tumor: Case Report. J Neurol Surg Rep. 2015;76:e23-e27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Nagafuji H, Yokoi H, Ohara A, Fujiwara M, Takayama N, Saito K. Primary diffuse large B-cell lymphoma of the frontal sinus: A case report and literature review. Radiol Case Rep. 2018;13:635-639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Li S, Young KH, Medeiros LJ. Diffuse large B-cell lymphoma. Pathology. 2018;50:74-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 459] [Cited by in RCA: 434] [Article Influence: 62.0] [Reference Citation Analysis (0)] |
| 9. | Grulich AE, Vajdic CM. The epidemiology of cancers in human immunodeficiency virus infection and after organ transplantation. Semin Oncol. 2015;42:247-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Said J, Cesarman E, Rosenwald A, Harris NL. Lymphomas associated with HIV infection. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW, editors. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Revised 4th ed. IARC: Lyon, 2017: 449-452. |
| 11. | Linke-Serinsöz E, Fend F, Quintanilla-Martinez L. Human immunodeficiency virus (HIV) and Epstein-Barr virus (EBV) related lymphomas, pathology view point. Semin Diagn Pathol. 2017;34:352-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 12. | Dutta R, Dubal PM, Svider PF, Liu JK, Baredes S, Eloy JA. Sinonasal malignancies: A population-based analysis of site-specific incidence and survival. Laryngoscope. 2015;125:2491-2497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 125] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 13. | Bhojwani A, Unsal A, Dubal PM, Echanique KA, Baredes S, Liu JK, Eloy JA. Frontal Sinus Malignancies: A Population-Based Analysis of Incidence and Survival. Otolaryngol Head Neck Surg. 2016;154:735-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Logsdon MD, Ha CS, Kavadi VS, Cabanillas F, Hess MA, Cox JD. Lymphoma of the nasal cavity and paranasal sinuses: improved outcome and altered prognostic factors with combined modality therapy. Cancer. 1997;80:477-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Marques-Piubelli ML, Salas YI, Pachas C, Becker-Hecker R, Vega F, Miranda RN. Epstein-Barr virus-associated B-cell lymphoproliferative disorders and lymphomas: a review. Pathology. 2020;52:40-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 16. | Young LS, Yap LF, Murray PG. Epstein-Barr virus: more than 50 years old and still providing surprises. Nat Rev Cancer. 2016;16:789-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 451] [Cited by in RCA: 608] [Article Influence: 67.6] [Reference Citation Analysis (0)] |
| 17. | Gloghini A, Dolcetti R, Carbone A. Lymphomas occurring specifically in HIV-infected patients: from pathogenesis to pathology. Semin Cancer Biol. 2013;23:457-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 18. | Petrara MR, Freguja R, Gianesin K, Zanchetta M, De Rossi A. Epstein-Barr virus-driven lymphomagenesis in the context of human immunodeficiency virus type 1 infection. Front Microbiol. 2013;4:311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Carbone A, Cesarman E, Spina M, Gloghini A, Schulz TF. HIV-associated lymphomas and gamma-herpesviruses. Blood. 2009;113:1213-1224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 230] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 20. | Sauter A, Faul C, Bitzer M, Bares R, Kraus S, Fenchel M, Horger M. Imaging findings in immunosuppressed patients with Epstein Barr virus-related B cell malignant lymphoma. AJR Am J Roentgenol. 2010;194:W141-W149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |