Published online Mar 6, 2021. doi: 10.12998/wjcc.v9.i7.1543
Peer-review started: August 4, 2020
First decision: December 14, 2020
Revised: December 27, 2020
Accepted: January 20, 2021
Article in press: January 20, 2021
Published online: March 6, 2021
Processing time: 208 Days and 13.8 Hours
Tonsillectomy is the most common procedure for treatment of pediatric recurrent acute tonsillitis and tonsillar enlargement that contributes to obstructive sleep apnea hypopnea syndrome. Postoperative hemorrhage of tonsillectomy is a life-threatening complication.
To identify the risk factors that may contribute to primary and secondary post-operative hemorrhage in pediatric tonsillectomy.
The clinical data from 5015 children, 3443 males and 1572 females, aged 1.92-17.08 years, with recurrent tonsillitis and/or tonsil hypertrophy who underwent tonsillectomy in our hospital from January 2009 to December 2018 were retrospectively collected. The variables including sex, age, time of onset, diagnosis, method of tonsillectomy, experience of surgeon, time when the surgery started and monthly average air temperature were abstracted. The patients with postoperative hemorrhage were classified into two groups, the primary bleeding group and the secondary bleeding group, and their characteristics were compared with those of the nonbleeding group separately. Statistical analysis was performed by chi-square test with SPSS 20.
Ninety-two patients had post-tonsillectomy hemorrhage, and the incidence rate of post-tonsillectomy hemorrhage was 1.83%. The mean age was 5.75 years. Cases of primary hemorrhage accounted for approximately 33.70% (31/92), and cases of secondary hemorrhage occurred in 66.30% (61/92). The rate of reoperation for bleeding was 0.92%, and the rate of rehospitalization for bleeding was 0.88% in all patients. Multiple hemostasis surgery was performed in 6.52% (3/46) of patients. The method of tonsillectomy (coblation tonsillectomy) and experience of the surgeon (junior surgeon with less than 5 years of experience) were significantly associated with primary hemorrhage (χ2 = 5.830, P = 0.016, χ2= 6.621, P = 0.010, respectively). Age (over 6 years old) and time of onset (more than a 1-year history) were significantly associated with secondary hemorrhage (χ2= 15.242, P = 0.000, χ2=4.293, P = 0.038, respectively). There was no significant difference in sex, diagnosis, time when the surgery started or monthly average air temperature. There was a significant difference in the intervention measures between the primary bleeding group and the secondary bleeding group (χ2= 10.947, P = 0.001). The lower pole and middle portion were the common bleeding sites, followed by the upper pole and palatoglossal arch.
The incidence rate of post-tonsillectomy hemorrhage is low. Coblation tonsillectomy and less than 5 years’ experience of surgeon contribute to the tendency for primary hemorrhage. Age and time of onset are responsible for secondary hemorrhage.
Core Tip: This is a retrospective study to identify the risk factors that may contribute to primary and secondary postoperative hemorrhage in pediatric tonsillectomy. The incidence rate of post-tonsillectomy hemorrhage was 1.83%, and secondary hemorrhage was a major component. Coblation tonsillectomy and less than 5 years’ experience of surgeon contributed to the tendency for primary hemorrhage. Age and time of onset were responsible for secondary hemorrhage. Surgeons should always pay attention to postoperative hemorrhage after tonsillectomy and its accompanying serious consequences.
- Citation: Xu B, Jin HY, Wu K, Chen C, Li L, Zhang Y, Gu WZ, Chen C. Primary and secondary postoperative hemorrhage in pediatric tonsillectomy. World J Clin Cases 2021; 9(7): 1543-1553
- URL: https://www.wjgnet.com/2307-8960/full/v9/i7/1543.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i7.1543
Tonsillectomy is the most common procedure for pediatric recurrent acute tonsillitis and tonsillar enlargement that contributes to obstructive sleep apnea hypopnea syndrome (OSAHS)[1]. Acute tonsillitis may occur at any age, and the incidence peak is observed in school aged children. It is responsible for approximately 5% of emergency medical consultations[2]. The main pathogenic bacteria are group A β-hemolytic streptococcus, followed by Staphylococcus aureus and Haemophilus influenzae. Recurrent acute tonsillitis causes frequent episodes of sore throat and fever, making patients suffer from a considerable disease burden[3]. The prevalence of OSAHS is 1.2% in elementary school children[4]. The most common symptoms associated with OSAHS include snoring, episodes of apnea, daytime sleepiness, depressed mood and irritability resulting in reduced quality of life. Meanwhile, the increased blood pressure, caused by the physiologic stresses of upper airway obstruction, can increase the risk of cardiovascular and cerebrovascular accidents[5]. Therefore, tonsillectomy is beneficial to protect the health and improve the quality of life of patients with surgical indications[6].
The exact number of pediatric tonsillectomies performed annually on a global scale is substantial and indistinct. More than 530000 children under 15 years of age undergo tonsillectomy every year in the United States[7]. Although tonsillectomy is a well-tolerated surgery, postoperative hemorrhage is still a common complication[8], even minor bleeding is often persistent and develops into severe hemorrhage[9]. Lethal post-tonsillectomy hemorrhage is unexpected and unpredictable and requires immediate and adequate treatment[10]. It can result in significant morbidities, such as shock, airway obstruction and the need for blood transfusion. There are currently no accurate data for predicting the surgical risk of life-threatening post-tonsillectomy hemorrhage and decreasing significantly these substantial complications. Here, we review our experience with postoperative hemorrhage after tonsillectomy over the past decade and explore the characteristics of the cases.
A retrospective analytical study was performed in 5015 consecutive patients who were hospitalized in the Otolaryngology Department of our hospital and underwent tonsillectomy from January 2009 to December 2018. There were 3443 males and 1572 females, aged from 1.92 to 17.08 years. The study was reviewed and approved by the Ethics Committee of Children's Hospital, Zhejiang University School of Medicine (2020-IRB-061). Written informed consents were obtained from the parents of patients. Tonsillectomy was performed in children who suffered from tonsillar infection and/or tonsillar enlargement leading to airway obstruction and sleep disorders.
Before the operation, routine preoperative examinations were performed to ensure that the values of the hematologic assay, blood biochemistry and coagulation tests were all within the normal range. The surgeon explained the operation risks to the parents of the children in detail, and the parents made the decision regarding the operation method of tonsillectomy (monopolar electrical tonsillectomy or coblation tonsillectomy) according to their own wishes.
Tonsillectomy is defined as complete resection of the tonsils in our study. In the method of monopolar electrical tonsillectomy, the children underwent orotracheal intubation with a reinforced endotracheal tube under general anesthesia and were maintained in the supine position during the operation. The mouth was opened with a Davis-Boyle mouth gag. The soft palate was retracted using one pediatric catheter (8F or 10F). Pericapsular dissection was performed from the superior to the inferior poles of the tonsils under a headlight. The tonsils were dissected away from the muscular wall towards the lower pole via monopolar electrocautery. Then, the tonsils were removed completely from the tonsillar fossa. Electrocoagulation was used to maintain hemostasis. In the method of coblation tonsillectomy, the procedure was similar for the surgical removal of the tonsillar tissue and hemostasis, but the surgical instruments were different.
After the operation was finished and extubation was complete, the vital signs of the children were closely observed for an adequate amount of time in the postoperative recovery room; and then, the children returned to a regular hospital room for 1-2 d. Discharged patients were followed for at least half a month.
The patients were informed that effective measures should be performed immediately upon postoperative hemorrhage, including bedside therapy (gargling with iced water or 1% hydrogen peroxide solution or compression with a 1:10000 adrenalin cotton ball) and emergency surgery (bipolar coagulation, suturing of the tonsil pillars under general anesthesia or selective embolization of carotid artery).
All patients with bleeding were divided into two groups, the primary and secondary bleeding groups, and their characteristics were compared with those of the nonbleeding group. Descriptive statistical methods were used for the data, including percentage, mean ± SD criteria and interquartile range (IQR). Statistical analysis was performed by chi-square test with SPSS 20 (Armonk, NY, United States).
A total of 5015 children who underwent tonsillectomy under general anesthesia were included in this study. There were 3343 males and 1572 females, with a male/female ratio of 2.13:1. The mean age was 5.75 (IQR 4.67, 7.33) years. Ninety-two of them had post-tonsillectomy hemorrhage, and the incidence rate was 1.83% (92/5015). Thirty-one patients had primary hemorrhage (occurring within the first 24 h after surgery), which accounted for approximately 33.70% (31/92) of the patients with post-tonsillectomy hemorrhage. The mean age was 6.49 ± 2.26 years. Sixty-one patients had secondary hemorrhage (beyond 24 h after surgery), which accounted for approximately 66.30% (61/92). The mean age was 7.31 ± 2.39 years.
The mean hospitalization time of all patients was 5 d (IQR 4, 6). There were 44 cases of secondary hospitalization in the secondary bleeding group. The mean time of postoperative hemorrhage after tonsillectomy in the primary bleeding group was 8 h (range 0.5 to 22.0); the mean time in the secondary bleeding group was 6 d (range 1.3 to 15.0). The rate of reoperation for bleeding was 0.92% (46/5015), and the rate of rehospitalization for bleeding was 0.88% (44/5015) in all patients. Multiple hemostasis surgery was performed in 6.52% (3/46) of patients, including two who experienced reoperation and one who underwent a third hemostasis surgery.
The method of tonsillectomy (coblation tonsillectomy) and experience of the surgeon (junior surgeon with less than 5 years of experience) were significantly associated with primary hemorrhage (χ2=5.830, P = 0.016, χ2= 6.621, P = 0.010, respectively). Age (> 6 years) and time of onset (> 1 year) were significantly associated with secondary hemorrhage (χ2= 15.242, P = 0.000, χ2= 4.293, P = 0.038, respectively). There was no significant difference in sex, diagnosis and time when the surgery started or monthly average air temperature (Table 1).
| Variables | Non-bleeding group, n = 4923 | Primary bleeding group, n = 31 | Secondary bleeding group, n = 61 | ||||
| n | χ2 | P value | n | χ2 | P value | ||
| Sex | |||||||
| Female | 1543 | 10 | 0.012 | 0.913 | 19 | 0.01 | 0.974 |
| Male | 3380 | 21 | 42 | ||||
| Age in yr | |||||||
| ≤ 6 | 2763 | 18 | 0.047 | 0.828 | 19 | 15.242 | 0.000a |
| > 6 | 2160 | 13 | 42 | ||||
| Time of onset in yr | |||||||
| ≤ 1 | 1759 | 10 | 0.162 | 0.688 | 14 | 4.293 | 0.038a |
| > 1 | 3164 | 21 | 47 | ||||
| Diagnosis | |||||||
| Chronic tonsillitis | 1200 | 8 | 0.034 | 0.853 | 19 | 1.496 | 0.221 |
| Tonsil hypertrophy | 3723 | 23 | 42 | ||||
| Tonsillectomy | |||||||
| Monopolar electrical tonsillectomy | 2500 | 9 | 5.830 | 0.016a | 24 | 3.154 | 0.076 |
| Coblation tonsillectomy | 2423 | 22 | 37 | ||||
| Surgeon | |||||||
| Junior surgeon | 1905 | 19 | 6.621 | 0.010a | 25 | 0.133 | 0.715 |
| Senior surgeon | 3018 | 12 | 36 | ||||
| Time when the surgery started | |||||||
| Before noon | 2010 | 10 | 0.937 | 0.333 | 23 | 0.243 | 0.622 |
| After noon | 2913 | 21 | 38 | ||||
| Monthly average air temperature | |||||||
| ≤ 20 °C | 2315 | 15 | 0.023 | 0.880 | 24 | 1.427 | 0.232 |
| > 20 °C | 2608 | 16 | 37 | ||||
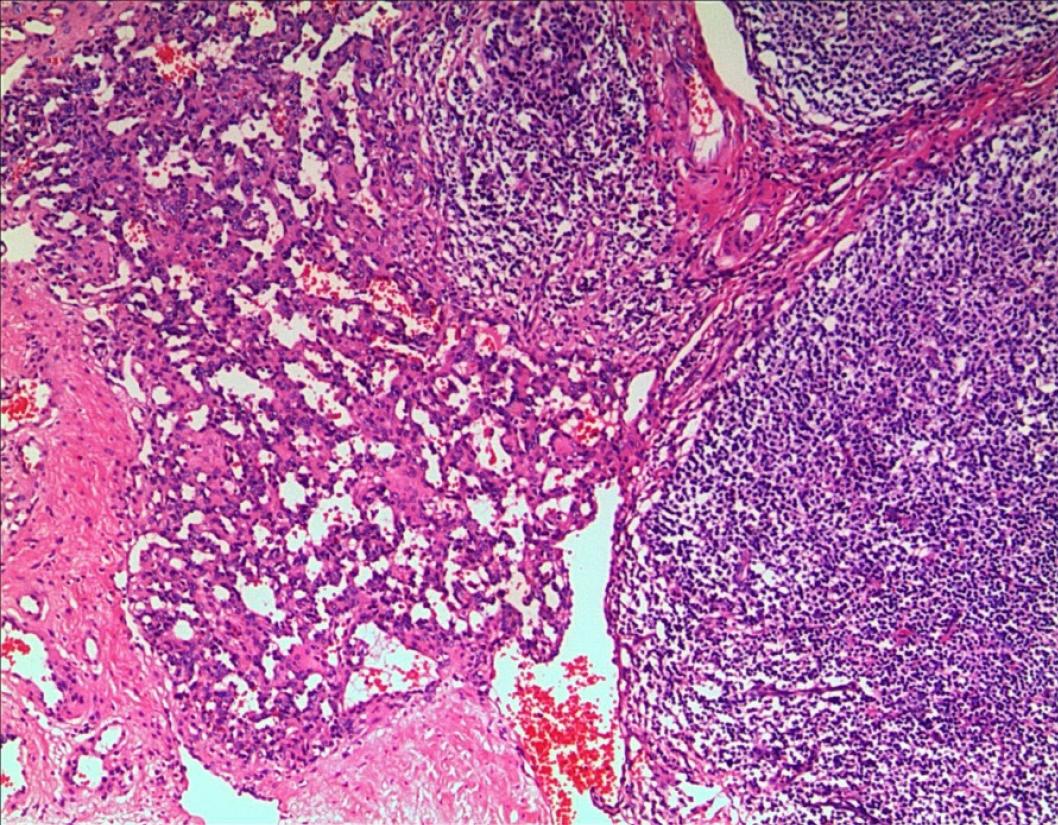
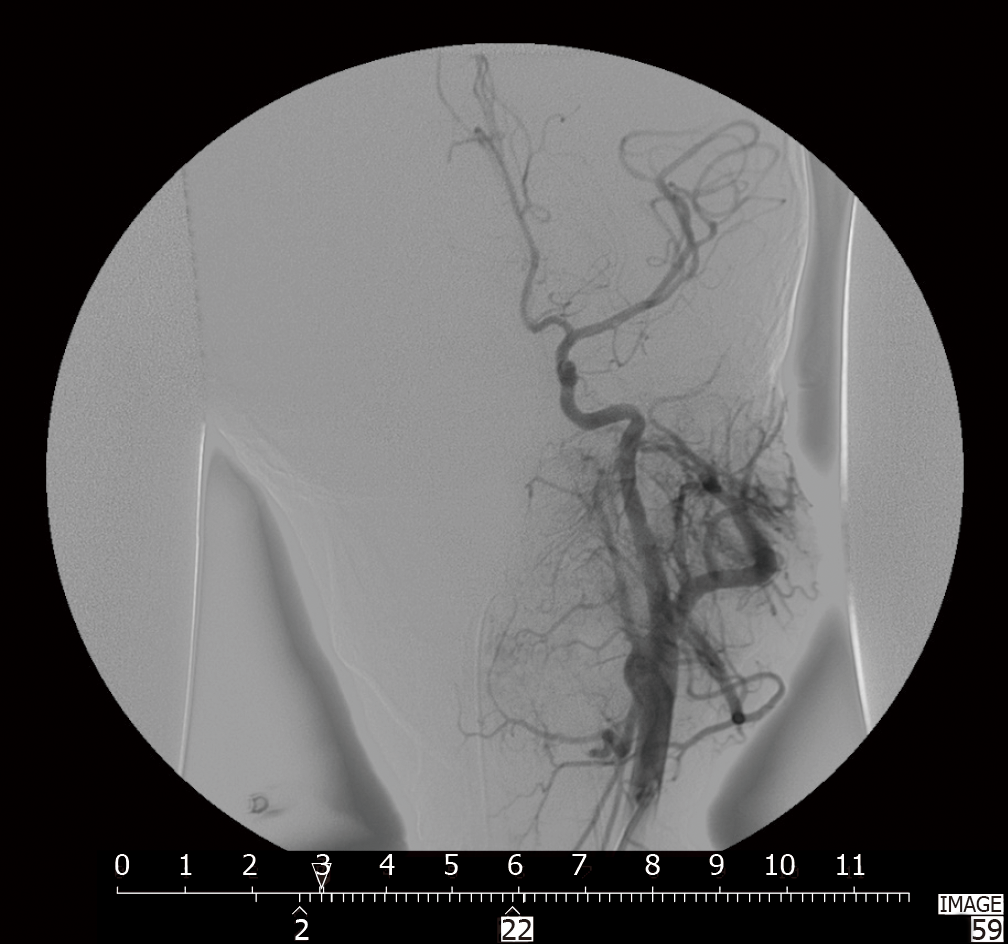
According to the classification of hemorrhage proposed by Windfuhr et al[11], the treatments for postoperative hemorrhage after tonsillectomy are shown in Table 2. The intervention measures were divided into bedside therapy (grade 1 or grade 2) and therapy in the operating theatre (grade 3 and grade 4). There was a significant difference in intervention measures between the primary bleeding group and the secondary bleeding group (χ2= 10.947, P = 0.001). Four patients suffered from hemorrhage and required blood transfusion; two of these patients and two other patients had to undergo treatment in the intensive care unit. One of them was an 11-year-old boy who had congenital hemangioma of the parapharyngeal space involving the left tonsil, which was confirmed by radiography and pathology.
In the primary hemorrhage group, the petechiae of five patients were in the bilateral tonsillar fossa, 15 were in the left fossa and 11 were in the right fossa. In the secondary hemorrhage group, the petechiae of seven patients were in the bilateral tonsillar fossa, 25 were in the left fossa and 29 were in the right fossa. The positions of post-tonsillectomy hemorrhage confirmed in sequence were the lower pole, middle portion, upper pole, palatoglossal arch and palatopharyngeal arch (Table 3).
| Position | Number | |
| Primary hemorrhage (n = 23) | Upper pole | 4 |
| Middle portion | 8 | |
| Lower pole | 14 | |
| Palatoglossal arch | 2 | |
| Palatopharyngeal arch | 1 | |
| Secondary hemorrhage (n = 23) | Upper pole | 5 |
| Middle portion | 9 | |
| Lower pole | 9 | |
| Palatoglossal arch | 3 | |
| Palatopharyngeal arch | 1 |
Post-tonsillectomy hemorrhage is the most frequently encountered complication after tonsillectomy, in addition to pain, dehydration, airway obstruction, vomiting and pulmonary edema. Certain morbidity and potential mortality are associated with hemorrhage following tonsillectomy. The reported rates of post-tonsillectomy hemorrhage in the literature vary widely among different medical centers. According to recent findings, the rate is approximately 4% in children who experience postoperative hemorrhage, and there is a wide range (from 2.61% to 15%) in the general population[12-16]. In our department, the incidence rate of post-tonsillectomy hemorrhage was 1.83%, which is lower than most reports in the literature.
The frequency of post-tonsillectomy hemorrhage requiring operative control ranges between 0.2% and 5.7% in children[17-19]. Our result was 0.92% and is comparable to the results of Osborne et al[20] (0.91%). It was reported that 7.1% of all patients with bleeding had multiple episodes of hemorrhage[15]. Multiple hemostasis surgery occurred in 6.52% of our patients.
The reasons for the large difference in the incidence of post-tonsillectomy hemorrhage is related to various and complicated factors. The findings of a multivariate logistic regression model indicated that age and sex were risk factors for post-tonsillectomy hemorrhage and that the risk of severe bleeding was significantly higher in children aged > 6 years and in males[13]. Our results strongly indicated that an age > 6 years contributed to a risk of secondary hemorrhage but did not contribute to a risk of primary hemorrhage. Another study also indicated that older age was significantly associated with an increased risk of multiple hemorrhages[15]. In our study, the ages of the two patients with two hemorrhages were 6.08 and 7.75 years, and the age of the one patient with three hemorrhages was 9.92 years. Sex was irrelevant as a contributing risk factor in our study, as shown in another report[21], but the time of onset was closely related to secondary hemorrhage.
It is believed that patients who experience more episodes of tonsillitis may have larger scars of the tonsillar bed and a more challenging anatomy, thus increasing the risk of postoperative bleeding[20]. A history of recurrent tonsillitis has been identified as a potential risk factor for post-tonsillectomy hemorrhage[22]. Children with a diagnosis of recurrent tonsillitis are more likely to experience postoperative bleeding than patients with OSAHS[23]. In our study, we did not detect a significant difference between the diagnoses of chronic tonsillitis and tonsillar hypertrophy. The likely explanation for this finding is that children with mild or short-lived inflammation have clearer anatomical structure exposure than adults[24]. We found that the method of tonsillectomy and experience of the surgeon appeared to play a significant role in the primary bleeding group. Meanwhile, coblation tonsillectomy was significantly associated with primary hemorrhage. In some studies, there is no strong evidence to suggest that the coblation technique exhibits any benefit or increases the risk of primary and secondary hemorrhage when compared to other techniques[25]. Nevertheless, another study found that the coblation technique was associated with higher incidence of secondary tonsillectomy hemorrhage[26]. Coblation patients have higher rates of postoperative bleeding than electric monopolar cautery patients[23]. It has been verified that primary bleeding is usually attributed to the type of surgical technique[9]. We believe that differences in the degree of surgeon experience and specific temperatures based on cut and coagulation settings could influence surgical outcomes. In our study, there was a significant difference between junior surgeons (with less than 5 years of experience) and senior surgeons (with more than 5 years of experience), linking familiarity with the anatomy of the peritonsillar space and the mastering of operation proficiency. It has also been found that air temperature has a high risk for bleeding, especially during warmer seasons[27]. However, there was no statistically significant positive association when we compared the monthly average air temperature of the bleeding group with that of the non-bleeding group, which was the same as the time when the operation started on the day of surgery.
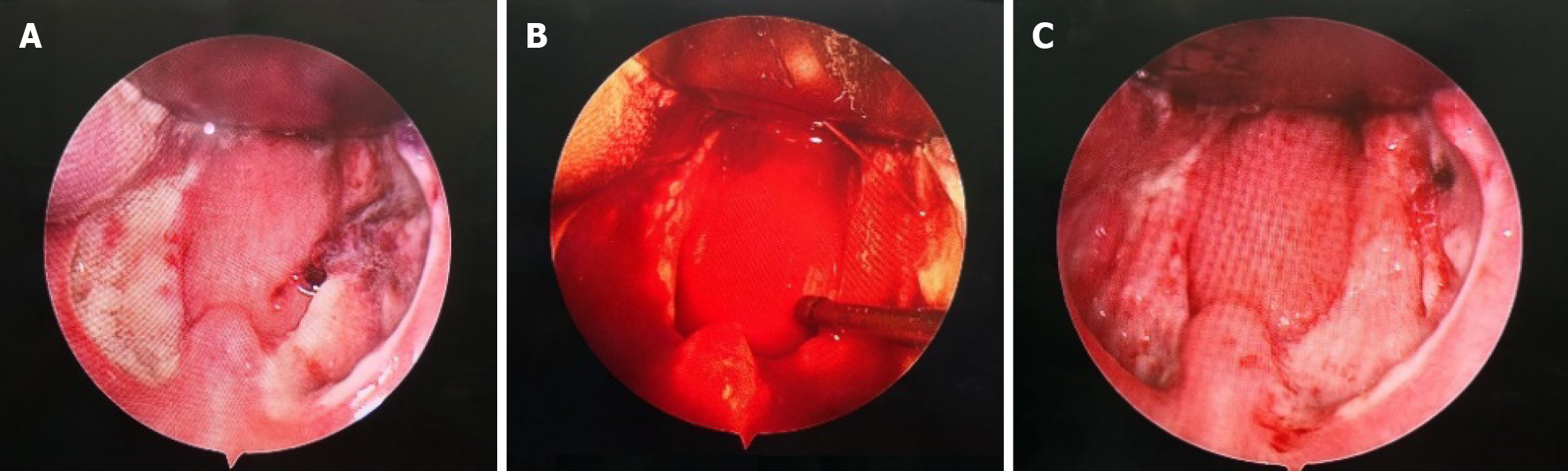
When post-tonsillectomy hemorrhage is encountered, the choice of whether to proceed to operative intervention relies on physical examination findings and the experience of the surgeon[28]. Nearly 60% of children with secondary post-tonsillectomy hemorrhage required an intervention[29]. Electrocautery, especially bipolar coagulation, is considered the most commonly used technique[30]. When it is infeasible to clear the clot in the wound, the bleeding point should be checked in detail, and cotton balls dipped in 1:10000 adrenalin should be packed or electrocautery should be conducted to achieve hemostasis; for uncooperative children, hemostasis under general anesthesia is an optimum choice[28].
During surgery, the lower pole and middle portion were common bleeding sites, followed by the upper pole and palatoglossal arch. No pericapsular dissection plane could be identified in the lower poles of the tonsils adjacent to the root of the tongue, and poor vision exposure of the operative field under the Davis-Boyle mouth gag increased the difficulty of the operation and the risk of potential bleeding. We found that the blood vessels in the middle of the tonsillar fossa were relatively abundant and thick, and inadequate hemostasis during the operation might also lead to postoperative bleeding. The laryngeal mirror was helpful to inspect the bleeding points in the upper pole and palatoglossal arch, which may not be directly visible, so that these hidden bleeding points could be cauterized[31]. Our data suggest that the experience of trained surgeons likely has a greater impact on the rate of bleeding after tonsillectomy than the techniques used[32]. The potential coagulation disorder and abnormal vascular anatomy should be given more attention in difficult-to-control intraoperative bleeding and recurrent post-tonsillectomy bleeding[9,33]. In our study, a congenital hemangioma of the parapharyngeal space involving the left tonsil that was confirmed by digital subtraction angiography and pathology in an 11-year-old boy who did not demonstrate any distinct symptoms until tonsillectomy was completed (Figures 1 and 2). Tracheotomy had to be implemented to address dyspnea for bleeding. The patient was ultimately cured by selective embolization. This was the most valuable experience and lesson for us in terms of realizing surgical safety.
Secondary bleeding was mostly due to wound infection or the underlying muscle and vessels exposed after the initial eschar sloughed. Fibrin clots are usually separated from the tonsillar fossa on the 5th to 7th d after surgery, leaving a thin layer of new stroma and epithelium. This is the time point of relative exposure of the vascular bed and the highest risk point of massive hemorrhage[9]. The average time from tonsillectomy to bleeding in the secondary bleeding group was 6 d in our study. In the healing process of oral keratinocytes separated from muscle epithelium secondary to muscle, contraction of the wound bottom and neovascularization occur at the same time, increasing the risk of bleeding[34].
The mortality rate of post-tonsillectomy hemorrhage is approximately 1:30000 in children[35] and 0.1% in adults[36]. Fortunately, there were no deaths in the last decade, and even longer time in our department, due to post-tonsillectomy hemorrhage. The paucity of the current data could not allow accurate and reliable calculation of the significant trend of risk of life-threatening post-tonsillectomy hemorrhage. Hospitalization was unable to prevent lethal outcomes for the selected population[10]. Secondary hemorrhage remains a substantial complication for tonsillectomy, particularly life-threatening arterial hemorrhage postoperatively[9]. Repeated bleeding is considered a warning sign of a severe condition, and patients presenting with a tonsillar clot but no active bleeding should be taken seriously[37]. The tonsillar clot might cover the real situation of bleeding and lead to serious results. Sometimes, lethal arterial hemorrhage was concealed under the tonsillar clot (Figure 3). We did prefer to control bleeding in the operating room more than bedside treatment. It is ideal for surgeons to select the surgical procedure they are most familiar with to prevent bleeding, regardless of whether electrocoagulation or suturing of the tonsil pillars is considered the common measure[38,39]. The incidence rate of postoperative hemorrhage is an important quality and safety indicator in tonsillectomy and should not be ignored[40]. It is necessary to review the experience of primary and secondary hemorrhage of tonsillectomy every year[41].
The incidence rate of post-tonsillectomy hemorrhage is low, and lethal hemorrhage rarely occurs. The risks of postoperative hemorrhage should be given more attention. Coblation tonsillectomy and less than 5 years’ experience of surgeon contributed to the tendency of primary hemorrhage. Age and time of onset were associated with secondary hemorrhage. Furthermore, abnormal vascular anatomy and arterial hemorrhage concealed by clots are usually overlooked and might have serious consequences. Surgeons should realize that experienced surgeons rely on adequate preoperative preparation, solid knowledge of anatomy and high vigilance for postoperative complications to ensure patient safety. This study is limited by the fact that it was performed in one medical center; thus, multicenter research is warranted.
Tonsillectomy is the most common procedure for pediatric recurrent acute tonsillitis and tonsillar enlargement that contributes to obstructive sleep apnea hypopnea syndrome. Postoperative hemorrhage of tonsillectomy is a life-threatening compli-cation.
To improve the management of postoperative hemorrhage of tonsillectomy.
To identify the risk factors that may contribute to primary and secondary post-operative hemorrhage in pediatric tonsillectomy.
A retrospective analytical study was performed, which included clinical data from 5015 consecutive patients who underwent tonsillectomy from January 2009 to December 2018. Characteristics of the patients from the primary bleeding group and the secondary bleeding group were compared with those of the nonbleeding group separately.
The method of tonsillectomy and experience of the surgeon were significantly associated with primary hemorrhage, while age and time of onset were significantly associated with secondary hemorrhage. There was a significant difference in the intervention measures between the primary bleeding group and the secondary bleeding group.
Coblation tonsillectomy and junior surgeons contribute to the tendency for primary hemorrhage. Age and time of onset are responsible for secondary hemorrhage.
The incidence rate of post-tonsillectomy hemorrhage is low, and lethal hemorrhage rarely occurs. The risks of postoperative hemorrhage should be given more attention.
The authors thank Liang JF for helping with the statistical analysis in the Information Centre, Children's Hospital, Zhejiang University School of Medicine.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koustas E, Malik S S-Editor: Gao CC L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Ding XX, Zhao LQ, Cui XG, Yin Y, Yang HA. Clinical observation of soft palate-pharyngoplasty in the treatment of obstructive sleep apnea hypopnea syndrome in children. World J Clin Cases. 2020;8:679-688. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Windfuhr JP, Toepfner N, Steffen G, Waldfahrer F, Berner R. Clinical practice guideline: tonsillitis I. Diagnostics and nonsurgical management. Eur Arch Otorhinolaryngol. 2016;273:973-987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 3. | Burton MJ, Glasziou PP, Chong LY, Venekamp RP. Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis. Cochrane Database Syst Rev. 2014: CD001802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 4. | Bixler EO, Vgontzas AN, Lin HM, Liao D, Calhoun S, Vela-Bueno A, Fedok F, Vlasic V, Graff G. Sleep disordered breathing in children in a general population sample: prevalence and risk factors. Sleep. 2009;32:731-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 466] [Cited by in RCA: 466] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 5. | Patel SR. Obstructive Sleep Apnea. Ann Intern Med. 2019;171:ITC81-ITC96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 162] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 6. | Ehsan Z, Ishman SL. Pediatric Obstructive Sleep Apnea. Otolaryngol Clin North Am. 2016;49:1449-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 7. | Mitka M. Guideline cites appropriateness criteria for performing tonsillectomy in children. JAMA. 2011;305:661-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Lawlor CM, Riley CA, Carter JM, Rodriguez KH. Association Between Age and Weight as Risk Factors for Complication After Tonsillectomy in Healthy Children. JAMA Otolaryngol Head Neck Surg. 2018;144:399-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | Wall JJ, Tay KY. Postoperative Tonsillectomy Hemorrhage. Emerg Med Clin North Am. 2018;36:415-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Windfuhr JP, Schloendorff G, Baburi D, Kremer B. Lethal outcome of post-tonsillectomy hemorrhage. Eur Arch Otorhinolaryngol. 2008;265:1527-1534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Windfuhr J, Seehafer M. Classification of haemorrhage following tonsillectomy. J Laryngol Otol. 2001;115:457-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Østvoll E, Sunnergren O, Stalfors J. Increasing Readmission Rates for Hemorrhage after Tonsil Surgery: A Longitudinal (26 Years) National Study. Otolaryngol Head Neck Surg. 2018;158:167-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Sarny S, Ossimitz G, Habermann W, Stammberger H. Hemorrhage following tonsil surgery: a multicenter prospective study. Laryngoscope. 2011;121:2553-2560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 124] [Article Influence: 9.5] [Reference Citation Analysis (1)] |
| 14. | Shelton FR, Ishii H, Mella S, Chew D, Winterbottom J, Walijee H, Brown R, Chisholm EJ. Implementing a standardised discharge analgesia guideline to reduce paediatric post tonsillectomy pain. Int J Pediatr Otorhinolaryngol. 2018;111:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | McKeon M, Kirsh E, Kawai K, Roberson D, Watters K. Risk Factors for Multiple Hemorrhages Following Tonsil Surgery in Children. Laryngoscope. 2019;129:2765-2770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Sakki A, Mäkinen LK, Roine RP, Nokso-Koivisto J. Changing trends in pediatric tonsil surgery. Int J Pediatr Otorhinolaryngol. 2019;118:84-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Francis DO, Fonnesbeck C, Sathe N, McPheeters M, Krishnaswami S, Chinnadurai S. Postoperative Bleeding and Associated Utilization following Tonsillectomy in Children. Otolaryngol Head Neck Surg. 2017;156:442-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 18. | Tolska HK, Takala AJ, Jero J. Peritonsillar infiltration of lidocaine with adrenaline is associated with increased risk of secondary post-tonsillectomy haemorrhage. J Laryngol Otol. 2018;132:911-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Morris S, Hassin E, Borschmann M. Overnight in-hospital observation following tonsillectomy: retrospective study of post-operative intervention. J Laryngol Otol. 2018;132:46-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Osborne MS, Clark M. The surgical arrest of post-tonsillectomy haemorrhage: Hospital Episode Statistics 12 years on. Ann R Coll Surg Engl. 2018;100:406-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Windfuhr JP, Schloendorff G, Baburi D, Kremer B. Serious post-tonsillectomy hemorrhage with and without lethal outcome in children and adolescents. Int J Pediatr Otorhinolaryngol. 2008;72:1029-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Windfuhr JP, Chen YS, Remmert S. Hemorrhage following tonsillectomy and adenoidectomy in 15,218 patients. Otolaryngol Head Neck Surg. 2005;132:281-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 209] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 23. | Lane JC, Dworkin-Valenti J, Chiodo L, Haupert M. Postoperative tonsillectomy bleeding complications in children: A comparison of three surgical techniques. Int J Pediatr Otorhinolaryngol. 2016;88:184-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Lou ZC, Lou ZH. Post-tonsillectomy hemorrhage: Underlying factors and prevention. Am J Otolaryngol. 2018;39:230-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Metcalfe C, Muzaffar J, Daultrey C, Coulson C. Coblation tonsillectomy: a systematic review and descriptive analysis. Eur Arch Otorhinolaryngol. 2017;274:2637-2647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | El-Taher M, Aref Z. Coblation Versus Conventional Tonsillectomy: A Double Blind Randomized Controlled Trial. Indian J Otolaryngol Head Neck Surg. 2019;71:172-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Mendel R, Yitshak-Sade M, Nash M, Joshua BZ. Assessment of the Association Between Post-tonsillectomy Hemorrhage and Weather Conditions. Isr Med Assoc J. 2018;20:349-353. [PubMed] |
| 28. | Clark CM, Schubart JR, Carr MM. Trends in the management of secondary post-tonsillectomy hemorrhage in children. Int J Pediatr Otorhinolaryngol. 2018;108:196-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 29. | Arora R, Saraiya S, Niu X, Thomas RL, Kannikeswaran N. Post tonsillectomy hemorrhage: who needs intervention? Int J Pediatr Otorhinolaryngol. 2015;79:165-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 30. | Lechner M, Chandrasekharan D, Vithlani R, Sutton L, Grandidge C, Elmiyeh B. Evaluation of a newly introduced tonsillectomy operation record for the analysis of regional post-tonsillectomy bleed data: a quality improvement project at the London North West Healthcare NHS Trust. BMJ Open Qual. 2017;6:e000055. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Walijee H, Krishnan M, Sharma R, De S. Indirect visualisation of the upper pole during tonsillectomy. J Laryngol Otol. 2018;132:461-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 32. | Hinton-Bayre AD, Noonan K, Ling S, Vijayasekaran S. Experience is more important than technology in paediatric post-tonsillectomy bleeding. J Laryngol Otol. 2017;131:S35-S40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 33. | van der Meer G, Gruber M, Mahadevan M. Recurrent post tonsillectomy bleeds: Presentation and characteristics in the paediatric population. Int J Pediatr Otorhinolaryngol. 2017;98:68-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 34. | Beswick DM, Santa Maria C, Ayoub NF, Capasso R, Santa Maria PL. Epithelial separation theory for post-tonsillectomy secondary hemorrhage: evidence in a mouse model and potential heparin-binding epidermal growth factor-like growth factor therapy. Eur Arch Otorhinolaryngol. 2018;275:569-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Greig SR. Current perspectives on the role of tonsillectomy. J Paediatr Child Health. 2017;53:1065-1070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Hsueh WY, Hsu WC, Ko JY, Yeh TH, Lee CH, Kang KT. Postoperative hemorrhage following tonsillectomy in adults: Analysis of population-based inpatient cohort in Taiwan. Auris Nasus Larynx. 2019;46:397-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 37. | El Rassi E, de Alarcon A, Lam D. Practice patterns in the management of post-tonsillectomy hemorrhage: An American Society of Pediatric Otolaryngology survey. Int J Pediatr Otorhinolaryngol. 2017;102:108-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 38. | Reusser NM, Bender RW, Agrawal NA, Albright JT, Duncan NO, Edmonds JL. Post-tonsillectomy hemorrhage rates in children compared by surgical technique. Ear Nose Throat J. 2017;96:E7-E11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 39. | Kim JS, Kim BG, Kim DH, Hwang SH. Efficacy of pillar suture for post-tonsillectomy morbidity in children: a meta-analysis. Braz J Otorhinolaryngol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 40. | Odhagen E, Sunnergren O, Söderman AH, Thor J, Stalfors J. Reducing post-tonsillectomy haemorrhage rates through a quality improvement project using a Swedish National quality register: a case study. Eur Arch Otorhinolaryngol. 2018;275:1631-1639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 41. | Baugh RF, Archer SM, Mitchell RB, Rosenfeld RM, Amin R, Burns JJ, Darrow DH, Giordano T, Litman RS, Li KK, Mannix ME, Schwartz RH, Setzen G, Wald ER, Wall E, Sandberg G, Patel MM; American Academy of Otolaryngology-Head and Neck Surgery Foundation. Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2011;144:S1-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 628] [Cited by in RCA: 616] [Article Influence: 44.0] [Reference Citation Analysis (0)] |