Published online Feb 26, 2021. doi: 10.12998/wjcc.v9.i6.1490
Peer-review started: November 23, 2020
First decision: November 29, 2020
Revised: December 13, 2020
Accepted: December 28, 2020
Article in press: December 28, 2020
Published online: February 26, 2021
Processing time: 74 Days and 19.4 Hours
Gastrointestinal stromal tumor (GIST) usually originates in the stomach, followed by the small intestine, rectum, and other parts of the gastrointestinal tract. The most common sites of metastasis are the liver and peritoneum, whereas spinal metastases from GIST are extremely rare.
We found a case of GIST with the first presentation of multilevel spinal metastases involving the thoracic and lumbar vertebrae. A 61-year-old Chinese man presented to our clinic because of pain in his lower back and hip for 10 d without cause. Subsequently, computed tomography (CT) and magnetic resonance imaging (MRI) revealed abnormal signals in the vertebral appendages of T12 and L4 accompanied by spinal canal stenosis, which was considered as tumor metastasis. As there were no metastases to vital organs, posterior thoracic and lumbar spinal decompression + adnexal mass resection + pedicle internal fixation was adopted to achieve local cure and prevent nerve compression. The results of histopathological studies were consistent with the metastasis of GIST. No local recurrence or new metastases were found at the 6-mo follow-up at the surgical site. The patient has no neurological symptoms at present. It is worth mentioning that a rectal mass was found and surgically removed 1 mo after the patient was discharged from hospital, and the pathological diagnosis of the mass was GIST.
By reviewing 26 previously reported cases of spinal metastasis in GIST, it was found that spinal metastasis of GIST has become more common in recent years, so the possibility of early spinal metastasis should be recognized. CT and MRI are of great value in the diagnosis of spinal metastatic tumors, and pathological biopsy is the gold standard for the diagnosis of metastatic tumors. It is safe and feasible to treat isolated spinal metastasis in GIST by excising metastatic masses, decompressing the spinal canal, and stabilizing the spine.
Core Tip: Gastrointestinal stromal tumor (GIST) is the most common mesenchymal tumor in the digestive tract and originates from Cajal stromal cells or related stem cells. GIST metastasis usually occurs in the liver (28%), mesentery and omentum (30%), and less often in the lungs (7%), subcutaneous tissue (4.7%), and lymph nodes (4.7%), whereas GIST bone metastasis is very rare (only 0.47%). We report a case of GIST in a 61-year-old man with multisegmental spinal metastasis as the first presentation and review the literature. As far as we know, this is the first report of a GIST with the first presentation of multisegmental spinal metastases from the thoracolumbar spine. This case highlights the importance of resection of metastatic tumors of the spine as an effective treatment for GIST.
- Citation: Kong Y, Ma XW, Zhang QQ, Zhao Y, Feng HL. Gastrointestinal stromal tumor with multisegmental spinal metastases as first presentation: A case report and review of the literature. World J Clin Cases 2021; 9(6): 1490-1498
- URL: https://www.wjgnet.com/2307-8960/full/v9/i6/1490.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i6.1490
Gastrointestinal stromal tumor (GIST) is the most common mesenchymal tumor in the digestive tract. It originates from Cajal stromal cells or related stem cells and is usually located in the stomach, small intestine, colon, and rectum[1,2]. Although GIST is rare, accounting for only 1 to 2 percent of gastrointestinal tumors, it accounts for 60% of all gastric stromal tumors[3,4]. Because GIST does not respond to conventional chemotherapy and radiation therapy, the gold standard for the treatment of GIST is surgical resection[5]. In addition, the use of Imatinib mesylate, a selective tyrosine kinase receptor inhibitor (TKI), significantly reduced the morbidity and mortality associated with GIST[6-8]. GIST metastasis usually occurs in the liver (28%), mesentery and omentum (30%), and less often in the lungs (7%), subcutaneous tissue (4.7%), and lymph nodes (4.7%)[9,10], whereas GIST bone metastasis is very rare (only 0.47%)[11]. Spinal metastases are especially rare in GIST, and few cases have been reported in the previous literature[12,13].
Bone is the most common site of metastatic cancer, with 60% of metastatic tumors occurring in the spine[14,15]. Spinal metastases from cancer are a common oncology challenge, as 20 to 40 percent of cancer patients are affected in the course of the disease, and up to 20% of those suffer from spinal cord compression and become paralyzed. The incidence of thoracic spine was the highest (70%), followed by lumbar spine (20%) and cervical spine (10%). Breast cancer, lung cancer, and prostate cancer were the most common primary lesions in patients with bone metastases[16,17]. Due to the close relations among the vertebrae, spinal cord, and nerves, besides ache, spinal metastases can also cause spinal deformities, nerve or spinal cord compression, and even paralysis.
Bone metastasis of GIST is very rare. By reviewing the literature, we found that only 26 cases of GIST spine metastasis have been reported so far. We herein report a case of GIST in a 61-year-old man with multisegmental spinal metastasis as the first presentation and review the literature. As far as we know, this is the first report of a GIST with the first presentation of multisegmental spinal metastases in the thoracolumbar spine.
A 61-year-old Chinese man had pain in his lower back and buttocks for 10 d without incentive, and no relief after rest.
Although the patient received oral non-steroidal anti-inflammatory drugs, no significant effect was observed. Then, he went to Hebei Medical University Fourth Affiliated Hospital to seek further treatment.
The patient had an anal leiomyoma resection about 8 years ago.
The patient's other medical history was not noteworthy.
The physical examination showed that the patient had percussion pain on the 11th and 12th thoracic vertebrae and percussion pain on the spinous processes of the 4th and 5th lumbar vertebrae, which both radiated to the buttocks and both lower limbs. As a result, the thoracolumbar movement was restricted, and muscle strength of both lower limbs was grade 4 (according to Manual Muscle Testing). There was no obvious abnormality in the saddle area and lower limbs. The physiological radiation existed, and pathological signs were not elicited. According to the Frankel grading standard of spinal cord injury, the patient was diagnosed with grade D.
Laboratory testing showed a high level of C-reactive protein (11.70 mm/L, reference range 0-6.0 mm/L), high erythrocyte sedimentation rate (29.00 mm/h, reference range 0-15 mm/h), high neutrophil count (6.45 × 109/L, reference range 1.8-6.3 × 109/L), and low lymphocyte count (0.86 × 109/L, reference range 1.1-3.2 × 109/L).
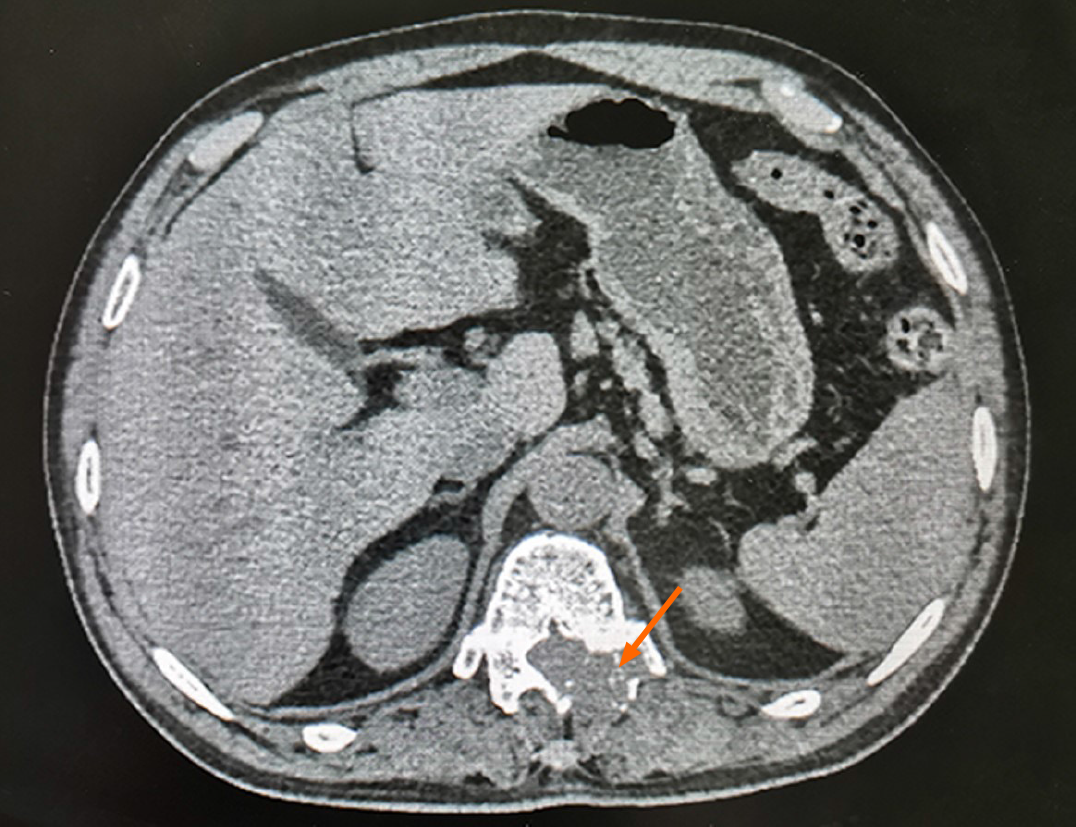
computed tomography (CT) showed bone destruction in the left pedicle of T12 (Figure 1). Liver and kidney function, electrolyte, coagulation function, routine urine tests, and cardiopulmonary function were normal. In order to further evaluate the patient's condition, the patient underwent magnetic resonance imaging (MRI) examination, and the results showed abnormal signals in the vertebral appendages of T12 and L4 accompanied by spinal canal stenosis, and metastasis was considered (Figure 2).
The final diagnosis of the presented case was multiple spinal mass.
As there were no metastases to vital organs, surgical treatment was adopted to achieve local cure and prevent nerve compression. After successful general intravenous anesthesia, the patient was placed in a prone position. Surgical exploration showed that L4 vertebral spinous process and vertebral lamina had obvious bone destruction, and tumor tissues were infiltrated. T12 vertebral spinous process and left vertebral pedicle tumor were significantly invaded, with bone destruction and dural sac compression. Spinal canal decompression and pedicle internal fixation were performed. Visual inspection using the intraoperative fluoroscopy showed optimal position of all pedicle screws. Intraoperative blood loss was approximately 550 mL. After the operation, the patient returned to the ward safely with stable vital signs and no obvious abnormalities in the heart, lung, and abdomen. The patient had normal upper and lower limb movements.
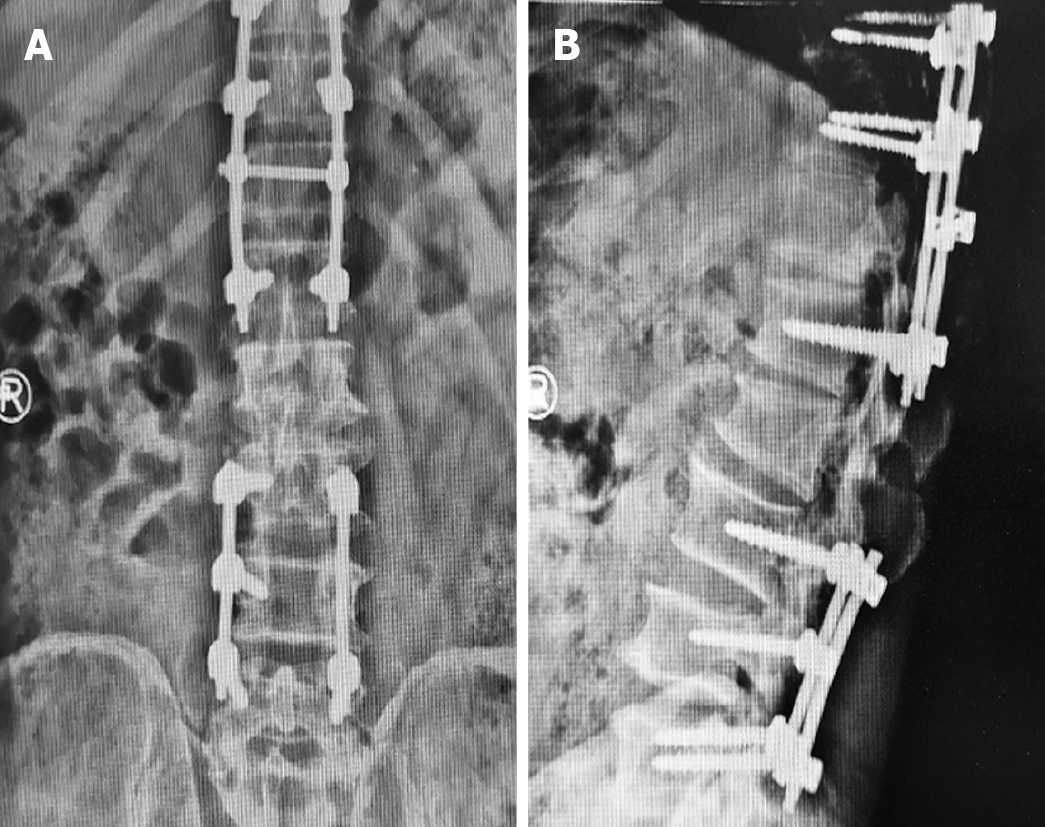
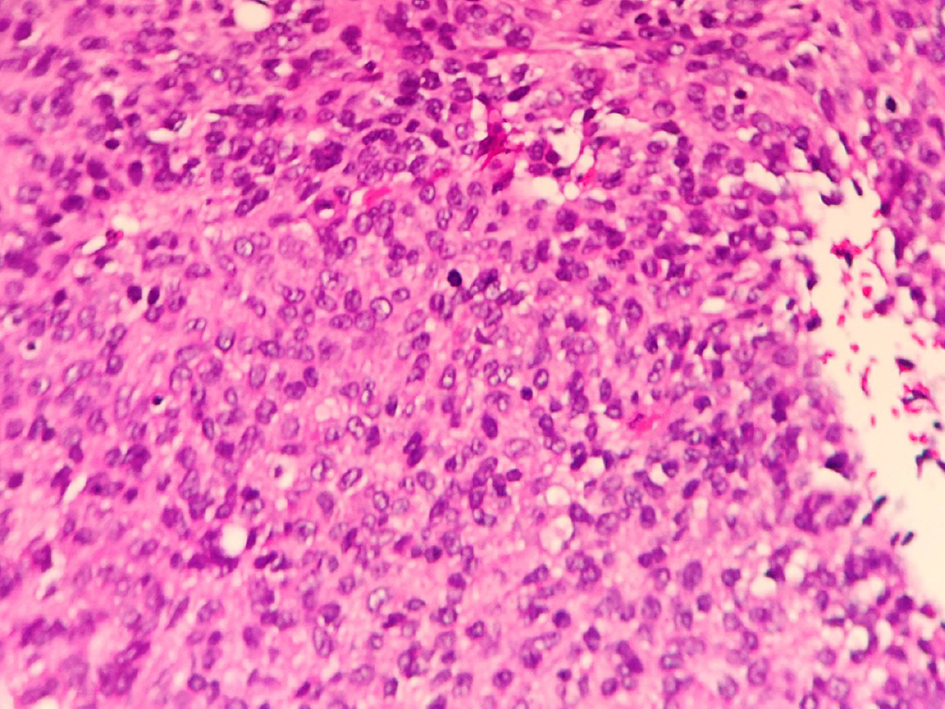
X-ray examination confirmed that the implant was in the correct position and there were no signs of screw and rod displacement (Figure 3). The results of histopathological studies were consistent with the metastasis of GIST. The results of immunohistochemistry suggested positive staining for Vimentin, indicating a mesenchymal origin. CD34, CD117, and CD31 were all positive, and Ki-67 positive cells accounted for 20%. According to immunohistochemical and morphological changes, it was consistent with GIST (Figure 4). CKIT and PDGFRA gene tests were performed on the patient, and the test results showed a mutation in exon 11 of c-KIT gene [KIT exon 11 C.1667_1672delagtGGa (p.W557_K558del)]. No mutation was found in exons 9, 13, and 17 of c-Kit and PDGRFA. The wound healed at the first stage after the operation without postoperative complications. One week after the operation, the patient was discharged from hospital and we followed the patient for 6 mo. Percussive pain in the lower back and radiating pain in both lower extremities disappeared. According to the Frankel grading standard of spinal cord injury, the patient was diagnosed with grade E. At the 6-mo follow-up, no local recurrence or new metastasis was observed on CT or MRI. It is worth mentioning that a rectal mass was found and surgically removed 1 mo after the patient was discharged from hospital, and the pathological diagnosis of the mass was GIST.
GIST is the most common stromal tumor in the gastrointestinal tract, which has a potential tendency of malignancy[18,19]. GIST metastasis usually occurs in the liver, mesentery, and omentum, whereas GIST bone metastasis is very rare. We report a case of GIST with the first presentation of multilevel spinal metastases involving the thoracic and lumbar vertebrae. What makes this case unique is that GIST metastasized to thoracic and lumbar vertebrae as the first manifestation. This is the first report of GIST with multi-segment spinal metastasis (thoracic and lumbar) as the first manifestation.
GIST is a mesenchymal neoplasm that arises in the gastrointestinal tract. GIST is a fusiform (70%), epithelioid (20%), or mixed mesenchymal tumor of the digestive tract that secretes CD117 (c-KIT). Approximately 18% of patients with GIST, especially those in the small intestine, had no symptoms at all[2,20]. Symptomatic patients may experience nonspecific symptoms such as nausea, vomiting, bloating, early satiety, and abdominal pain, but there is rarely a significant abdominal mass[20]. GIST metastasis usually occurs in the liver, mesentery, and omentum, whereas GIST bone metastasis is very rare (only 0.47%). GIST bone metastasis involves the spine, pelvis, ribs, humerus, clavicle, and other sites[21,22]. The most common symptoms of bone metastasis in GIST are local pain and limb weakness, followed by pathological fractures or no symptoms. The spine is the most common site for bony metastases of malignant tumors, and GIST is no exception. And GIST patients with spinal involvement have a worse prognosis than those without. We review the literature and find that only 26 cases of GIST spine metastasis have been reported so far (Table 1). In most cases, the spinal metastasis of GIST occurs in the late stage of the disease. Of the 26 reported cases of GIST, only four had a single segment of spinal metastasis as the first presentation[23]. However, few reports have been reported on GIST with multisegmental metastasis of the spine as the first manifestation.
| Patient | Age/sex | Primary tumor location | Location of metastases | Spinal metastases treatment |
| 1[23] | 62/M | Small intestine | Liver, spine, pelvis, rib | Zoledronic acid + radiotherapy + TKI |
| 2[23] | 82/F | Stomach | Liver, spine, pelvis | Zoledronic acid + TKI |
| 3[23] | 54/F | Small intestine | Liver, rib, spine, iliac bone | Zoledronic acid + TKI |
| 4[24] | 55/M | Sigmoid colon | Liver, spine, skull, pelvis | TKI + zoledronic acid |
| 5[22] | 56/M | Esophagus | Spine, rib | TKI + zoledronic acid |
| 6[25] | 49/M | Stomach | Liver, spleen, peritoneum, soft tissue, spine, rib, pelvis, femur, humerus | TKI |
| 7[25] | 52/F | Stomach | Liver, spleen, spine, rib, pelvis | TKI |
| 8[25] | 48/M | Stomach | Liver, spleen, spine | TKI |
| 9[25] | 51/M | Stomach | Liver, spleen, soft tissue, rib, humerus | TKI |
| 10[25] | 60/M | Small intestine | Liver, spine | TKI |
| 11[25] | 71/M | Rectum | Liver, spleen, spine, rib, pelvis, femur, humerus | TKI |
| 12[26] | 56/M | Small intestine | Liver, hip, spine, femur | TKI + radiotherapy + zoledronic acid |
| 13[26] | 70/M | Small intestine | Liver, spine | TKI + radiotherapy + zoledronic acid |
| 14[27] | 66/M | Stomach | Liver, spine, pelvis, rib, sternum, scapula | TKI |
| 15[13] | 51/M | Rectum | Spine | Resection |
| 16[28] | 69/F | Stomach | Liver, spine, subcutaneous | TKI + radiotherapy |
| 17[29] | 46/M | Stomach | Liver, spine, rib, humerus, clavicle | TKI + radiotherapy |
| 18[30] | 61/F | Stomach | Spine, liver, lung | Resection + TKI |
| 19[30] | 58/M | Small intestine | Spine, humerus, liver, peritoneum | Resection + TKI |
| 20[30] | 71/M | Small intestine | Spine, humerus, liver, pleura | Resection + TKI |
| 21[31] | 58/M | Small intestine | Liver, spine, sternoclavicular joint | TKI + radiotherapy |
| 22[32] | 37/M | Small intestine | Liver, spine | Resection + TKI + radiotherapy + chemotherapy |
| 23[33] | 54/M | Small intestine | Liver, spine | Resection + sorafenib + regorafenib |
| 24[34] | 76/F | Rectum | Spine, rib | Resection + TKI |
| 25[21] | 57/M | Rectum | Liver, lung, spine, clivus, temporal bone | TKI + radiotherapy |
| 26[35] | 83/M | Colon | Spine | Resection + radiotherapy |
Bone is a common site of metastasis in advanced malignant tumors[24]. Skeletal metastasis can cause a series of related events, such as pain and pathological fractures, which seriously affect the quality of life of patients. The occurrence of skeletal metastasis indicates that patients will have a worse prognosis. Therefore, early diagnosis of bone metastases can change the treatment plan as soon as possible and reduce the suffering of patients. As a non-invasive and repeatable examination, imaging examination is widely used in the diagnosis of tumor bone metastasis. CT, MRI, bone scintigraphy, and other imaging techniques show obvious advantages in the detection of bone metastasis in tumor patients, and have important significance in improving the early diagnosis rate of bone metastasis[25,26].
It is likely that bone metastasis in GIST will become more common due to the extensive use of imaging techniques and improved treatments such as TKI combined with surgical resection, which have greatly extended the life expectancy and overall survival rate of GIST patients. At present, although TKI treatment of GIST can significantly prolong the median survival of GIST patients, surgical resection is still the most important treatment strategy for primary GIST. GIST spinal metastases lead to neurological deficits due to nerve compression, which can lead to deterioration in functional status or survival. Previous studies have shown that the involvement of the spine in GIST bone metastasis affects the prognosis of patients. The average survival of patients with spinal involvement was 41.78 mo, while that of patients without spinal involvement was 82.49 mo. In addition, patients treated with surgery combined with TKI for GIST bone metastasis had a significantly longer survival than patients treated with TKI alone[27]. What is different from previous reports is that this case is an isolated metastasis involving only thoracolumbar metastases and no other metastases, and the patient has developed symptoms of nerve compression. Therefore, we used posterior thoracic and lumbar spinal decompression, adnexal mass resection, and pedicle internal fixation to treat the spinal metastasis of GIST. However, this only alleviated pain and prevented pathologic fractures and other bone-related events. For the primary disease, the patient still needed to receive further treatment. We followed the patient for 6 mo. CT and MRI showed no local recurrence or new metastasis at the surgical site at the 6-mo follow-up. However, a rectal mass was found 1 mo after discharge. After the tumor was surgically removed, the pathological diagnosis of the mass was GIST. In addition, the patient received targeted drugs for GISTs. This patient had a good prognosis, which indicates that resection of spinal metastases and pedicle internal fixation are effective treatments for GIST.
Overall, bone metastases in GIST are rare, accounting for only 0.47% of the cases, while multisegmental metastases of the thoracolumbar spine are even rarer. The extensive use of imaging technology has shown obvious advantages in the detection of bone metastasis in tumor patients. It is of great significance to use appropriate imaging methods to improve the early diagnosis rate of bone metastasis. We found a case of GIST with the first presentation of multilevel spinal metastases involving the thoracic and lumbar vertebrae. And in this case, posterior thoracic and lumbar spinal decompression + adnexal space-occupying resection + pedicle internal fixation was adopted to treat the spinal metastasis of GIST, and satisfactory results were obtained, indicating that the resection of spinal metastatic tumor is an effective method to treat the spinal metastasis of GIST.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kiwaki T S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Kindblom LG, Remotti HE, Aldenborg F, Meis-Kindblom JM. Gastrointestinal pacemaker cell tumor (GIPACT): gastrointestinal stromal tumors show phenotypic characteristics of the interstitial cells of Cajal. Am J Pathol. 1998;152:1259-1269. [PubMed] |
| 2. | Søreide K, Sandvik OM, Søreide JA, Giljaca V, Jureckova A, Bulusu VR. Global epidemiology of gastrointestinal stromal tumours (GIST): A systematic review of population-based cohort studies. Cancer Epidemiol. 2016;40:39-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 579] [Cited by in RCA: 519] [Article Influence: 57.7] [Reference Citation Analysis (1)] |
| 3. | Miettinen M, Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med 2006; 130: 1466-1478 [PMID: 17090188 DOI: 10. 1043/1543-2165(2006)130. |
| 4. | Beltran MA, Cruces KS. Primary tumors of jejunum and ileum as a cause of intestinal obstruction: a case control study. Int J Surg. 2007;5:183-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Chen YH, Liu KH, Yeh CN, Hsu JT, Liu YY, Tsai CY, Chiu CT, Jan YY, Yeh TS. Laparoscopic resection of gastrointestinal stromal tumors: safe, efficient, and comparable oncologic outcomes. J Laparoendosc Adv Surg Tech A. 2012;22:758-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | DeMatteo RP. Nanoneoadjuvant therapy of gastrointestinal stromal tumor (GIST). Ann Surg Oncol. 2009;16:799-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Benjamin RS, Casali PG. Adjuvant Imatinib for GI Stromal Tumors: When and For How Long? J Clin Oncol. 2016;34:215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Zhang L, Feng L, Cong H, Yu Z, Wang H, Dong Y, Wang J. Multiple primary malignant neoplasms: A case report and literature review. Oncol Lett. 2019;18:4210-4220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Patnaik S, Jyotsnarani Y, Rammurti S. Radiological features of metastatic gastrointestinal stromal tumors. J Clin Imaging Sci. 2012;2:43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Lillemoe HA, Brudvik KW, Vauthey JN. Treatment Options for Metastatic Gastrointestinal Stromal Tumors to the Liver: A Review. Semin Liver Dis. 2019;39:395-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Yang DY, Wang X, Yuan WJ, Chen ZH. Metastatic pattern and prognosis of gastrointestinal stromal tumor (GIST): a SEER-based analysis. Clin Transl Oncol. 2019;21:1654-1662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 12. | Suzuki K, Yasuda T, Nagao K, Hori T, Watanabe K, Kanamori M, Kimura T. Bone metastasis of a gastrointestinal stromal tumor: A report of two cases. Oncol Lett. 2015;9:1814-1818. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Shimizu T, Murakami H, Sangsin A, Demura S, Kato S, Shinmura K, Yokogawa N, Oku N, Kitagawa R, Tsuchiya H. En bloc corpectomy for late gastrointestinal stromal tumor metastasis: a case report and review of the literature. J Med Case Rep. 2018;12:300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Bollen L, Dijkstra SPD, Bartels RHMA, de Graeff A, Poelma DLH, Brouwer T, Algra PR, Kuijlen JMA, Minnema MC, Nijboer C, Rolf C, Sluis T, Terheggen MAMB, van der Togt-van Leeuwen ACM, van der Linden YM, Taal W. Clinical management of spinal metastases-The Dutch national guideline. Eur J Cancer. 2018;104:81-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 15. | Böhm P, Huber J. The surgical treatment of bony metastases of the spine and limbs. J Bone Joint Surg Br. 2002;84:521-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 113] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 16. | Liu Y, Wang Y, Zhao L, Song R, Tan H, Wang L. Effectiveness and safety of percutaneous vertebroplasty in the treatment of spinal metastatic tumor. Pak J Med Sci. 2017;33:675-679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Witham TF, Khavkin YA, Gallia GL, Wolinsky JP, Gokaslan ZL. Surgery insight: current management of epidural spinal cord compression from metastatic spine disease. Nat Clin Pract Neurol. 2006;2:87-94; quiz 116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 177] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 18. | Ozan E, Oztekin O, Alacacioğlu A, Aykaş A, Postaci H, Adibelli Z. Esophageal gastrointestinal stromal tumor with pulmonary and bone metastases. Diagn Interv Radiol. 2010;16:217-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Nannini M, Biasco G, Di Scioscio V, Di Battista M, Zompatori M, Catena F, Castellucci P, Paterini P, Dei Tos AP, Stella F, Maleddu A, Pantaleo MA. Clinical, radiological and biological features of lung metastases in gastrointestinal stromal tumors (case reports). Oncol Rep. 2011;25:113-120. [PubMed] |
| 20. | Scherübl H, Faiss S, Knoefel WT, Wardelmann E. Management of early asymptomatic gastrointestinal stromal tumors of the stomach. World J Gastrointest Endosc. 2014;6:266-271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 21. | Barrière J, Thariat J, Vandenbos F, Bondiau PY, Peyrottes I, Peyrade F. Diplopia as the first symptom of an aggressive metastatic rectal stromal tumor. Onkologie. 2009;32:345-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Waterman BR, Kusnezov N, Dunn JC, Hakim MN. Aggressive gastrointestinal stromal tumor with spinal metastases: a case report. Mil Med. 2015;180:e618-e621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Di Scioscio V, Greco L, Pallotti MC, Pantaleo MA, Maleddu A, Nannini M, Bazzocchi A, Di Battista M, Mandrioli A, Lolli C, Saponara M, Giorgio G, Biasco G, Zompatori M. Three cases of bone metastases in patients with gastrointestinal stromal tumors. Rare Tumors. 2011;3:e17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Jain A, Dubashi B; Mangaladevi; Chandra SS; Halanaik D. Mesentric gastrointestinal stromal tumor with bone metastases. Indian J Cancer. 2011;48:383-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Jati A, Tatlı S, Morgan JA, Glickman JN, Demetri GD, Van den Abbele A, Silverman SG. Imaging features of bone metastases in patients with gastrointestinal stromal tumors. Diagn Interv Radiol. 2012;18:391-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Aktan M, Koc M, Yavuz BB, Kanyilmaz G. Two cases of gastrointestinal stromal tumor of the small intestine with liver and bone metastasis. Ann Transl Med. 2015;3:259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 27. | Rochigneux P, Mescam-Mancini L, Perrot D, Bories E, Moureau-Zabotto L, Sarran A, Guiramand J, Bertucci F. Gastrointestinal Stromal Tumour with Synchronous Bone Metastases: A Case Report and Literature Review. Case Rep Oncol. 2017;10:66-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Feki J, Bouzguenda R, Ayedi L, Bradi M, Boudawara T, Daoud J, Frikha M. Bone metastases from gastrointestinal stromal tumor: a case report. Case Rep Oncol Med. 2012;2012:509845. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Slimack NP, Liu JC, Koski T, McClendon J Jr, O'Shaughnessy BA. Metastatic gastrointestinal stromal tumor to the thoracic and lumbar spine: first reported case and surgical treatment. Spine J. 2012;12:e7-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | Ishi Y, Nakayama N, Kobayashi H, Yamaguchi S, Terasaka S, Houkin K. Successful Removal of a Metastatic Gastrointestinal Stromal Tumor in the Craniovertebral Junction using an Occipital Artery to Posterior Inferior Cerebellar Artery Bypass. Case Rep Neurol. 2014;6:139-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Kosemehmetoglu K, Kaygusuz G, Fritchie K, Aydin O, Yapicier O, Coskun O, Karatayli E, Boyacigil S, Guler G, Dervisoglu S, Kuzu I. Clinical and pathological characteristics of gastrointestinal stromal tumor (GIST) metastatic to bone. Virchows Arch. 2017;471:77-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 32. | Bor-Ren H, Hsien-Chih C, Tai-Ngar L, Wen-Ching T. Epidural metastases from a gastrointestinal stromal tumour. J Clin Neurosci. 2008;15:82-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 33. | Houssami N, Costelloe CM. Imaging bone metastases in breast cancer: evidence on comparative test accuracy. Ann Oncol. 2012;23:834-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 34. | Costelloe CM, Rohren EM, Madewell JE, Hamaoka T, Theriault RL, Yu TK, Lewis VO, Ma J, Stafford RJ, Tari AM, Hortobagyi GN, Ueno NT. Imaging bone metastases in breast cancer: techniques and recommendations for diagnosis. Lancet Oncol. 2009;10:606-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 122] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 35. | Choi J, Raghavan M. Diagnostic imaging and image-guided therapy of skeletal metastases. Cancer Control. 2012;19:102-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |