Published online Feb 26, 2021. doi: 10.12998/wjcc.v9.i6.1439
Peer-review started: October 15, 2020
First decision: December 21, 2020
Revised: December 23, 2020
Accepted: January 5, 2021
Article in press: January 5, 2021
Published online: February 26, 2021
Processing time: 112 Days and 0.6 Hours
Postoperative discal pseudocyst (PDP) is a rare condition that presents after surgery for lumbar disc herniation. Due to the lack of information, the diagnosis and treatment of PDP remain controversial. Herein, we report a PDP case that occurred following percutaneous endoscopic lumbar discectomy and received conservative treatment. Additionally, we review all the published literature regarding PDP and propose our hypothesis regarding PDP pathology.
A 23-year-old man presented with a relapse of low back pain and numbness in his left lower extremity after undergoing percutaneous endoscopic lumbar discectomy for lumbar disc herniation. Repeat magnetic resonance imaging demonstrated a cystic lesion at the surgical site with communication with the inner disc. The patient was diagnosed as having PDP. The patient received conservative treatment, which resulted in rapid improvement and spontaneous regression of the lesion, and had a favorable outcome in follow-up.
PDP and discal cyst (DC) exhibit similarities in both histological and epidemiological characteristics, which indicates the same pathological origin of PDP and DC. The iatrogenic annular injury during discectomy might accelerate the pathological progression of DC. For patients with mild to moderate symptoms, conservative treatment can lead to great improvement, even inducing spontaneous regression. However, surgical cystectomy is necessary in patients with neurological deficits and where conservative treatment is ineffective.
Core Tip: In the present paper, we present a rare case of postoperative discal pseudocyst (PDP). At presentation, the patient showed relapse symptoms after discectomy for lumbar disc herniation. He underwent conservative treatment, and revealed excellent outcomes. We review and discuss the symptoms, previous operations, and histological findings of PDP. We found that PDP mainly occurs in physically active young Asian males and is composed of dense fibrous connective tissue without epithelial lining and bloody serous fluid as cyst wall and content, respectively, which suggested that PDP and discal cyst have the same pathogenesis.
- Citation: Fu CF, Tian ZS, Yao LY, Yao JH, Jin YZ, Liu Y, Wang YY. Postoperative discal pseudocyst and its similarities to discal cyst: A case report . World J Clin Cases 2021; 9(6): 1439-1445
- URL: https://www.wjgnet.com/2307-8960/full/v9/i6/1439.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i6.1439
Postoperative discal pseudocyst (PDP) is a rare condition that develops after surgery for lumbar disc herniation. Young et al[1] first reported PDP as an independent pathological condition in 2009 and characterized it as a cystic lesion that is attached to the site of surgery at the disc that underwent discectomy[2]. As a post-surgical condition, PDP occurs after open discectomy, percutaneous endoscopic lumbar discectomy (PELD), and micro-endoscopic discectomy. However, unlike discal cyst (DC), which is another cystic lesion occurring at the intervertebral disc, the pathogenesis of PDP remains unclear[3-5]. The two principal strategies for the treatment of PDP are conservative treatment and surgical cystectomy. Although both are reportedly effective, the indications for the treatments remain controversial. Here, we report a case with PDP that developed after PELD and underwent conservative treatment. We investigate the characteristics of PDP and DC by comparing the reported histological findings of the two conditions and further discuss the ideal treatment for PDP by reviewing all the published literature pertaining to PDP.
A 23-year-old man presented to the spine surgery clinic with mild low back pain and slight numbness in his left leg.
The patient reported recurrence of low back pain and numbness in the same area after receiving PELD surgery.
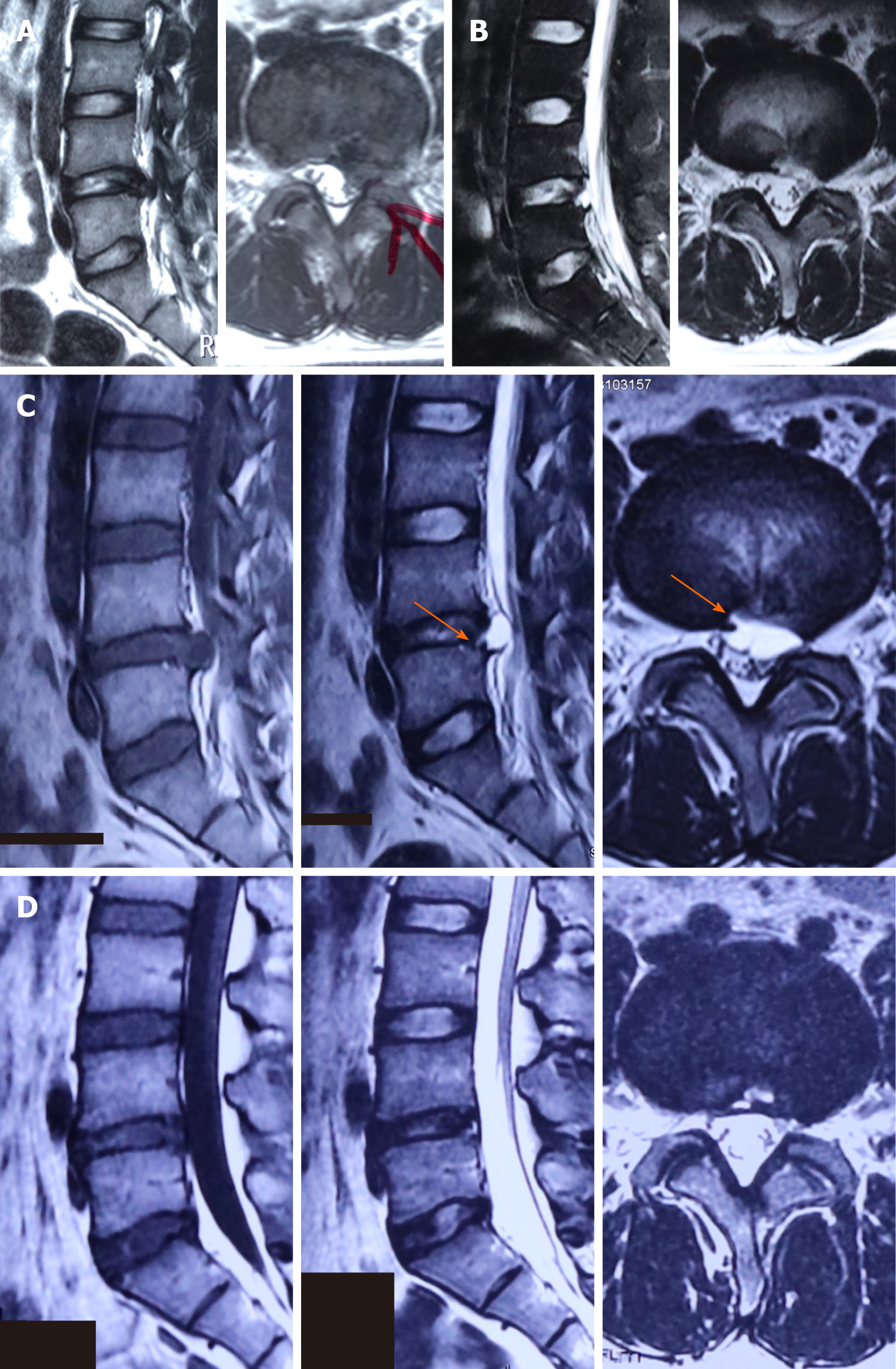
The patient was diagnosed with lumbar disc herniation at L4-5 (Figure 1A) and underwent percutaneous endoscopic lumbar discectomy. During the operation of PELD, the nerve root and dural sac were well-preserved and no cerebral fluid leakage occurred after surgery. His symptoms were relieved immediately post-surgery, and postoperative magnetic resonance imaging (MRI; 3 d after the surgery) revealed normal post-surgery changes with complete resection of the migrating disc (Figure 1B). The patient was discharged on the 5th postoperative day without any residual symptoms. However, 40 d after surgery, the patient reported recurrence of low back pain and numbness in the same area as in the pre-surgical period.
Repeat MRI demonstrated the development of a cystic lesion at the surgical site (Figure 1C). The lesion presented a hypointensive signal in T1-weighted image and hyperintensity in T2-weighted image, with a clear communication with the nucleus pulposus, which led to a diagnosis of PDP (Figure 1C).
The patient was diagnosed with PDP at the segment of L4-5.
The patient received conservative treatment, including nonsteroidal anti-inflammatory drugs (celecoxib, 200 mg, BID) and bed rest.
After 2 wk, the patient’s symptoms were effectively improved. On follow-up examinations, he reported no residual symptoms, and MRI after 6 mo showed spontaneous regression of PDP (Figure 1D).
PDP is an extremely rare post-discectomy complication, which was first reported by Young et al[1] in 2009. Subsequently, several reports have described this infrequent condition using different terms, including postoperative annular pseudocyst[1], post-discectomy pseudocyst[4], and postoperative discal pseudocyst[2]. Due to the compression of nearby nerve roots, PDP can be symptomatic, and patients usually present with recurrent-lumbar disc herniation-like symptoms within a short period after surgery, such as low back pain or radiculopathy of the lower extremities. For better understanding of PDP, we review all the reported PDP cases in addition to our case. There are a total of 36 cases (33 men, 3 women) with the development of PDP after discectomy, with an average age of 26.1 years and average onset time of 24.5 ± 10.3 d post-surgery (Table 1). All cases had PDP in the lumbar segments, predominantly at the lower lumbar disc (L4-L5 and L5-S1).
| Citation | Patients | Age/gender | Previous operation | Country | Days till symptom aggravation (d) | Days till MRI detection (d) | Treatment of PDP |
| Young et al[1], 2009 | 2 | 60/M; 38/M | MED; partial discectomy | US | 30; 60 | 390; 420 | No treatment; conservative |
| Kang et al[4] and Park et al[18] | 15 | 20-25 M, mean 22.5 | PELD | Korea | N/A | 53.7 | 5 surgical (1 OC, 4 PELC); 10 conservative |
| Chung et al[2], 2012 | 12 | 11 M, 1 F, mean 29.3 | 9/12 MED; 3/12 PELD | Korea | Mean 23.3 (range, 9–38) | Mean 31.2 (range, 14–60) | 5 surgical (UA); 7 conservative |
| Jha et al[6], 2016 | 2 | 16/M; 18/F | MED; MED | Japan | 7; 7 | 30; 60 | Conservative; conservative |
| Yu et al[3], 2016 | 1 | 27/M | Open discectomy | Korea | 14 | 21 | Conservative |
| Prasad and Menon[7], 2017 | 1 | 30/M | Discectomy | Indian | 25 | 25 | OC |
| Shiboi et al[8], 2017 | 2 | 14/F; 27/M | PELD; PELD | Japan; Japan | 30; 20 | 30; 20 | PELC; MED |
| Manabe et al[5], 2019 | 1 | 21/M | PELD | Japan | 42 | 42 | PELC |
| Present cases | 1 | 23/M | PELD | China | 40 | 40 | Conservative |
Among the PDP cases, previous operations consisted of micro-endoscopic discectomy (12 cases) and open discectomy (3 cases), and it is worth mentioning that post-PELD PDP cases (21 cases) appeared and rose rapidly along with the popularization of PELD (Table 1)[1-8]. Almost all PDP cases were reported after less-aggressive discectomy focusing on the herniated disc fragment and ruptured annulus fibrosus, which maintains the physiological function of the majority of the discal complex, and thus fulfills the requirement of containing the fluid supply. Moreover, the focal inflammatory response caused by the minimally invasive surgery with little disturbance of the surrounding tissue may contribute to pseudo-capsule formation. In the reported PDP cases, the average onset time of PDP was 24.5 ± 10.3 d, which conforms to the plasticity period of inflammation and post-surgical scar formation. Young et al[1] hypothesized that PDP is caused by fluid accumulation within a potential space that communicates with the inner annulus fibrosus and is layered by a fibrous pseudo-membrane that is reactively formed due to the inflammatory response after surgery. Based on this theory, Chung et al[2] suggested that post-surgical movement of the unfixed segment may pump fluid from the mildly degenerated disc complex to the inflammatory response area via a defective annulus fibrosis, leading to the formation of a cystic lesion. These two reports have adequately explained the formation of these cystic lesions and proposed four necessary factors for their development: (1) Mildly degenerated hydrous disc; (2) Post-surgical plasticity; (3) Residual ends of annulus fibrosus; and (4) Unfixed segment[4]. Therefore, PDP is a unique condition caused by specific circumstances after less-aggressive discectomy without fixation. To prevent it, an appropriate operation of the annulus fibrosus ends might be effective.
After reviewing the histological findings of PDP, we notice that PDP shares many features with DC, which is defined as an extradural cyst with a distinctive communication with the corresponding intervertebral disc. Hence, we review all PDP and DC cases with a histology report since 2009 (first PDP report) and identify several notable features shared by both PDP and DC (Table 2)[9-20]. First, all DC (12 cases) and PDP (2 cases) patients who underwent histological examination of the cyst wall reported that it was composed of dense fibrous connective tissue without any specific lining cell layer. Second, 8/9 cases of DC and 3/4 cases of PDP who received histological examination of the cyst content had a serous bloody fluid inside the cyst. Third, the existence of a stalk was proven in all DC (13 cases) and PDP (2 cases) patients who underwent the relevant examination. DC and PDP are not only similar in histology but also similar in epidemiological characteristics. Aydin et al[9] summarized the risk factors for DC and found that DC occurs predominantly in physically active young Asian males. These findings concur with the results of our analysis of PDP cases, in which as many as 28/36 cases were Asian males aged under 30 years (Table 1). Based on these findings and comparing the features above, we speculate that PDP and DC might be the same histological entity and have the same origin, and PDP probably is a DC that is formed post-surgery. In other words, an iatrogenic annular injury during discectomy might accelerate the pathological progression of a DC. As per this hypothesis, the controversial mechanism of the formation of DC might be to some extent uncovered, and those mechanisms that can be affected by operations are more likely to lead to DC. Supported by the presence of fibrous connective tissue, the imaging finding of an annular fissure and the communication between the intervertebral disc and cyst, Kono et al[21] first proposed the pseudo-membrane theory, which suggests that the process starts with a focal degeneration of the back disc wall and fluid formation, followed by fluid leakage into the epidural space and finally, the formation of the cyst. On the other hand, Matsumoto et al[11] reported the presence of hemosiderin deposits within the cyst wall and indicated that the cystic lesion is formed by inflammatory epidural venous plexus hemorrhage. Regarding the pathological mechanisms proposed by these two studies, both pseudo-membrane formation and communication in the annulus fibrosus can be induced by surgery; nevertheless, the routine application of drainage is more likely to retard the hematoma process than to accelerate it. Therefore, our study supports the hypothesis proposed by Kono et al[21].
| Location | Results | DC | PDP |
| Cyst wall | Dense fibrous connective tissue without specific lining cell layer | 12 cases[9-19] | 2 cases[2,7] |
| N/A | 1 case[20] | 2 cases[3,8] | |
| Content | Serous bloody fluid | 8 cases[9-11,13-15,20] | 3 cases[2,3,8] |
| Clear fluid, similar to spinal fluid | 1 case[12] | 1 case[7] | |
| N/A | 4 cases[16-19] | 0 case | |
| Communicating stalk | Confirmed | 13 cases[9-20] | 2 cases[2,3] |
| N/A | 0 case | 2 cases[7,8] |
As PDP greatly resembles DC in many aspects, the management of DC illustrates the treatment of PDP. However, the ideal treatment for DC and PDP remains controversial. Among the 36 PDP cases, 21 received conservative therapy, 14 underwent cystectomy, and 1 received no further treatment. There seem to be no universally accepted surgical indications other than the tolerance of individuals and therapeutic effect of conservative treatment[2,4]. Conservative treatments, including physical therapy, analgesics, and aspiration, were administrated to those with mild to moderate symptoms, and improvement and spontaneous regression of the lesion were detected in several patients, including our case. Zekaj et al[22] proposed that the communicating stalk is the key for prognosis estimation and that the cysts with a sharp turning stalk may have a higher probability of spontaneous regression[22], which provides another clue to surgeons for devising treatment strategies for these patients.
Patients who have neurological deficits and show little improvement after receiving conservative therapy should receive surgical cystectomy. Similar to previous surgeries, micro-endoscopic cystectomy and percutaneous endoscopic lumbar cystectomy are preferred by surgeons. Reoperation of the spinal canal is usually associated with the problem of serious adhesions. Depending on the approach of the previous surgery, the dorsal and ventral spaces of the dura might be occupied with scars and inflammatory tissue, which can lead to difficulty in dissection and requires careful operation in case of a dural tear. The main limitation of the study is the small quantity of PDP histological results, and the reason is because of the severe adhesion caused by previous surgery, thus, PDP is usually resected in unclear pieces, which leads to a lack of histological results of PDP.
In summary, PDP is a rare condition that develops after less-aggressive discectomy without fixation. Here, we have described a PDP case who underwent conservative treatment, and revealed excellent outcome. By reviewing the reported literature, we found that PDP mainly occurs in physically active young Asian males and is composed of dense fibrous connective tissue without epithelial lining and bloody serous fluid as cyst wall and content, respectively, which suggests that PDP and DC have the same pathogenesis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Berra LV S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Li JH
| 1. | Young PM, Fenton DS, Czervionke LF. Postoperative annular pseudocyst: report of two cases with an unusual complication after microdiscectomy, and successful treatment by percutaneous aspiration and steroid injection. Spine J. 2009;9:e9-e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Chung D, Cho DC, Sung JK, Choi E, Bae KJ, Park SY. Retrospective report of symptomatic postoperative discal pseudocyst after lumbar discectomy. Acta Neurochir (Wien). 2012;154:715-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Yu HJ, Park CJ, Yim KH. Successful Treatment of a Symptomatic Discal Cyst by Percutaneous C-arm Guided Aspiration. Korean J Pain. 2016;29:129-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Kang SH, Park SW. Symptomatic post-discectomy pseudocyst after endoscopic lumbar discectomy. J Korean Neurosurg Soc. 2011;49:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Manabe H, Higashino K, Sugiura K. A Rare Case of a Discal Cyst Following Percutaneous Endoscopic Lumbar Discectomy via a Transforaminal Approach. Int J Spine Surg. 2019;13:92-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Jha SC, Tonogai I, Higashino K, Sakai T, Takata Y, Goda Y, Abe M, Nagamachi A, Fukuta S, Sairyo K. Postoperative discal cyst: An unusual complication after microendoscopic discectomy in teenagers. Asian J Endosc Surg. 2016;9:89-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Prasad GL, Menon GR. Post-discectomy annular pseudocyst: A rare cause of failed back syndrome. Neurol India. 2017;65:650-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Shiboi R, Oshima Y, Kaneko T, Takano Y, Inanami H, Koga H. Different operative findings of cases predicted to be symptomatic discal pseudocysts after percutaneous endoscopic lumbar discectomy. J Spine Surg. 2017;3:233-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Aydin S, Abuzayed B, Yildirim H, Bozkus H, Vural M. Discal cysts of the lumbar spine: report of five cases and review of the literature. Eur Spine J. 2010;19:1621-1626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Kobayashi S, Takeno K, Uchida K, Yayama T, Nakajima H, Miyazaki T, Guerrero A, Baba H. Pathogenesis of the discal cysts communicating with an adjacent herniated disc. Histological and ultrastructual studies of two cases. Joint Bone Spine. 2010;77:184-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Matsumoto M, Watanabe K, Tsuji T, Ishii K, Takaishi H, Nakamura M, Toyama Y, Chiba K. Microendoscopic resection of lumbar discal cysts. Minim Invasive Neurosurg. 2010;53:69-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Lin N, Schirmer CM, Proctor MR. Presentation and progression of a disc cyst in a pediatric patient. J Neurosurg Pediatr. 2011;7:209-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Hyung-Jun K, Dae-Yong K, Tae-Ho K, Ho-Sang P, Jae-Sung K, Jae-Won J, Jung-Kil L. Lumbar discal cyst causing bilateral radiculopathy. Surg Neurol Int. 2011;2:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Shibata S, Hanakita J, Takahashi T, Minami M, Kuraishi K, Watanabe M. Bilateral discal cysts managed by partial hemilaminectomy and microscopic resection of hemilateral cyst. Spine (Phila Pa 1976). 2011;36:E1655-E1658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Khalatbari MR, Moharamzad Y. Discal cyst in pediatric patients: case report and review of the literature. Neuropediatrics. 2012;43:289-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Ha SW, Ju CI, Kim SW, Lee S, Kim YH, Kim HS. Clinical outcomes of percutaneous endoscopic surgery for lumbar discal cyst. J Korean Neurosurg Soc. 2012;51:208-214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Bansil R, Hirano Y, Sakuma H, Watanabe K. Transition of a herniated lumbar disc to lumbar discal cyst: A case report. Surg Neurol Int. 2016;7:S701-S704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Park JW, Lee BJ, Jeon SR, Rhim SC, Park JH, Roh SW. Surgical Treatment of Lumbar Spinal Discal Cyst: Is It Enough to Remove the Cyst Only without Following Discectomy? Neurol Med Chir (Tokyo). 2019;59:204-212. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Chen S, Suo S, Li C, Wang Y, Li J, Zhang F, Zhang W. Clinical Application of Percutaneous Transforaminal Endoscopic Surgery in Lumbar Discal Cyst. World Neurosurg. 2020;138:e665-e673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Lame A, Kaloshi G, Xhumari A, Vreto G, Petrela M. Insights on the natural history and pathogenesis of multilevel discal cysts. J Clin Neurosci. 2012;19:617-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 21. | Kono K, Nakamura H, Inoue Y, Okamura T, Shakudo M, Yamada R. Intraspinal extradural cysts communicating with adjacent herniated disks: imaging characteristics and possible pathogenesis. AJNR Am J Neuroradiol. 1999;20:1373-1377. [PubMed] |
| 22. | Zekaj E, Franzini A, Bona AR, Servello D. Spontaneous regression of a discal cyst: a physiopathological hypothesis. J Neurosurg Sci. 2020;64:304-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |