Published online Feb 26, 2021. doi: 10.12998/wjcc.v9.i6.1353
Peer-review started: August 10, 2020
First decision: November 14, 2020
Revised: December 3, 2020
Accepted: December 16, 2020
Article in press: December 16, 2020
Published online: February 26, 2021
Processing time: 180 Days and 4.7 Hours
Epithelioid hemangioendothelioma (EHE) is an uncommon low-grade aggressive vascular tumor. It can occur in almost all locations, but is rarely encountered in bone.
We report a 23-year-old man who presented with left hip pain with no obvious cause. X-ray revealed bone destruction in the left femoral neck with sclerosis at the edges of the lesions. Magnetic resonance imaging (MRI) showed bone destruction in the medullary cavity of the left femoral head and neck. 18F-deoxyglucose-positron emission tomography/computed tomography (PET/CT) imaging showed bone destruction in the left ischium, acetabulum, and left femoral head neck, accompanied by increased radioactive uptake; the maximum standard uptake value was 4.2. Histopathologic examination revealed spindle-shaped mesenchymal tissue hyperplasia with scattered epithelioid cells. The patient underwent left femoral head replacement surgery. No signs of recurrence were observed as of the 18-mo follow-up.
The definitive diagnosis of femoral EHE can be established aided by the MRI and PET/CT findings.
Core Tip: Epithelioid hemangioendothelioma (EHE) is an uncommon low-grade aggressive vascular tumor that rarely occurs in bone. We report a case of femoral EHE which was diagnosed based on magnetic resonance imaging and positron emission tomography/computed tomography findings; the diagnosis was later confirmed by pathological and immunohistochemical examination. Left femoral head replacement was performed. No signs of recurrence were observed as of the 18-mo follow-up.
- Citation: Zhao HG, Zhang KW, Hou S, Dai YY, Xu SB. Femoral epithelioid hemangioendothelioma detected with magnetic resonance imaging and positron emission tomography/computed tomography: A case report. World J Clin Cases 2021; 9(6): 1353-1358
- URL: https://www.wjgnet.com/2307-8960/full/v9/i6/1353.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i6.1353
Epithelioid hemangioendothelioma (EHE), also called histiocytoid hemangioma or angiolymphoid hyperplasia with eosinophilia, is an uncommon vascular tumor with low-to-moderate malignant potential[1]. According to previous reports, EHE exhibits an intermediate biological behavior between angiosarcoma and hemangioma. The reported recurrence rate is approximately 11% and metastasis occurs in 2.7% of patients[2-4].
Primary bone EHE occurs mainly in the long bones of the lower limbs and accounts for < 1% of malignant bone lesions. Approximately 50% of patients with primary bone EHE have multiple lesions[1,5]. Femoral presentation is even rarer, which renders it liable to be misdiagnosed, both on imaging and histopathological examination. Indeed, the imaging findings of these rare vascular tumors closely mimic those of metastatic carcinoma[6] .
To the best of our knowledge, few studies have described the 18F fluorodeo-xyglucose (FDG) positron emission tomography (PET) or PET/computed tomography (CT) findings of bone EHE[7-9]. We report a patient with femoral EHE, which was detected based on magnetic resonance imaging (MRI) and PET/CT findings; the diagnosis was later confirmed by pathological and immunohistochemical results.
In January 2018, a 23-year-old man presented with left hip pain with no obvious cause. The pain was not linked to physical activities such as walking. The pain was not relieved after rest and showed no response to treatment.
Routine blood investigations, tumor markers, and erythrocyte sedimentation rate were within the normal reference range.
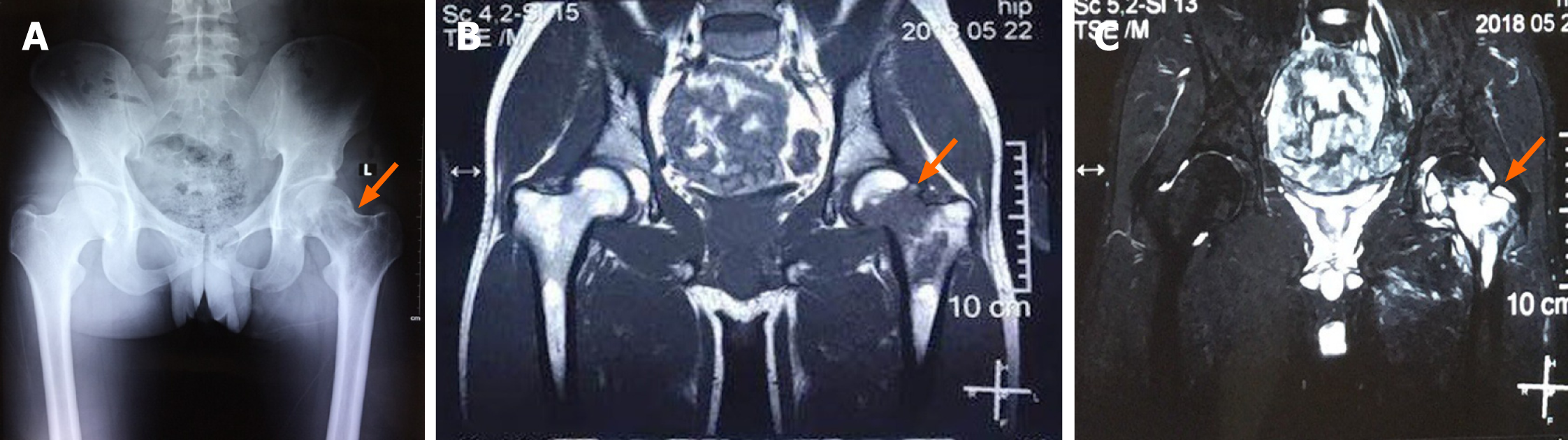
X-ray plain film showed bone destruction in the left femoral neck with peri-lesional sclerosis (Figure 1A). MRI examination of the pelvis showed bone destruction in the medullary cavity of the left femoral head and neck. The lesions showed low signal on T1-sequence and high signal on T2 sequence (Figure 1B and C). Therefore, the preliminary diagnosis was malignant space occupying lesions.
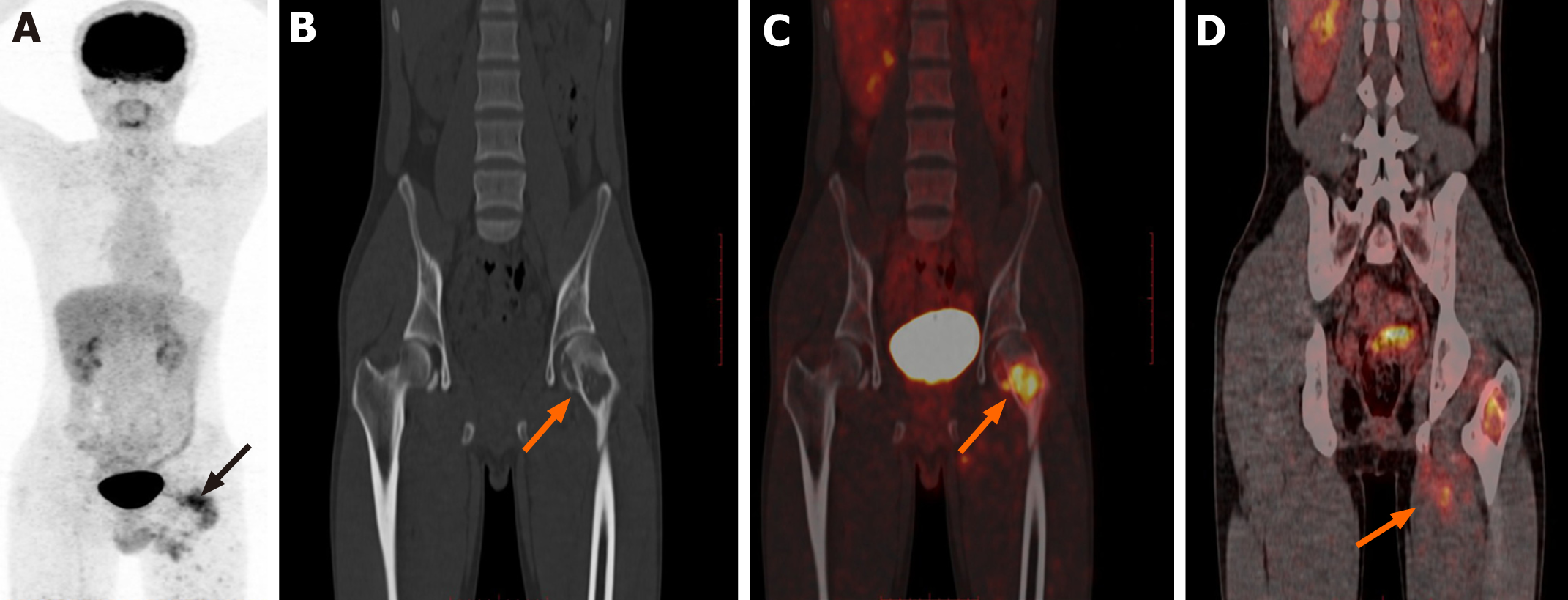
In February 2018, 18F-FDG PET/CT imaging from the head to trunk was performed. The results showed bone destruction in the left ischium, left acetabulum, and left femoral head neck, accompanied by increased radioactive uptake (Figure 2); the maximum standard uptake value (SUVmax) was 4.2. Soft tissue swelling was observed around the upper part of the left femur, which was accompanied by increased radioactive uptake (SUVmax: 3.5). CT examination revealed osteoblastic destruction in the left femoral head and neck, with hardened lesion edges; there was swelling of adjacent soft tissue, which showed slightly lower density than the surrounding muscle tissue with an unclear boundary (Figure 2B). As there were no abnormalities in other organs, a diagnosis of primary low-grade malignant bone lesion was suspected.
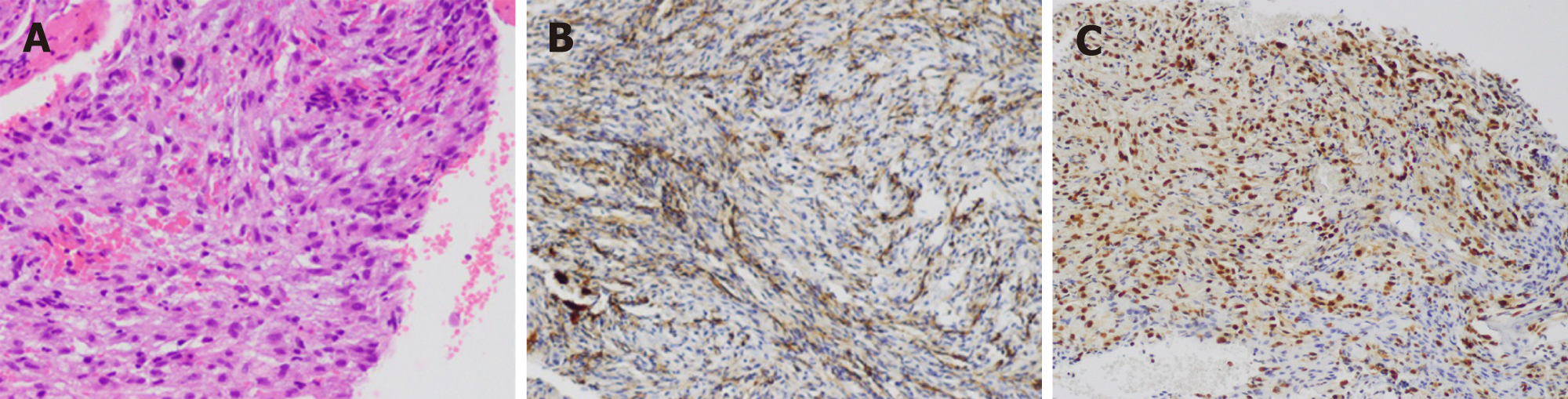
The left femur was subsequently punctured. Histopathological examination revealed spindle-shaped mesenchymal tissue hyperplasia with scattered epithelioid cells (Figure 3). Immunohistochemical staining results showed smooth muscle actin (-), desmin (-), actin (-), S-100 (-), CD68 (focal+), CD31 (+), CD34 (-), cytokeratin (+), proliferating cell nuclear antigen Ki67 (+5%), anaplastic lymphoma kinase (-), vimentin (+), and ERG (+). Based on these findings, a diagnosis of bone EHE was established.
Left femoral head replacement was performed.
No signs of recurrence were observed as of the 18-mo follow-up.
Bone EHE can occur in both men and women. It typically occurs in the 20-50 years age group, while patients aged 50-65 years may rarely be affected[10]. It is classified as a low-to-moderate malignant tumor by the World Health Organization (2013), with an associated mortality rate of about 20%. Lesions may occur in any part of the bone tissue, mostly in long tubular bones[11]. It is mainly described in the lower extremity bones, followed by the pelvis, and ribs[11]; 50%-64% of patients have multifocal lesions[1]. Lesions may involve multiple bones or may be confined to a single bone[11]. Aggregation of multifocal lesions at a single anatomical site should raise suspicion of bone EHE. In our patient, the imaging manifestations were consistent with this characteristic. Bone destruction lesions were mainly concentrated in the proximal region of the left femur.
The classical radiographic manifestation of bone EHE is that of a well demarcated lytic lesion located in the bone cortex and medullary cavity; smaller lesions are usually well-defined, while larger lesions are ill-defined and permeative. Soap bubble appearance with expansion of bone has been described[10]. A "palisade-like" bone crest can be seen in some lesions, which indicates that the lesions may originate from blood vessels in bone. Some lesions may also exhibit mild sclerosis and periosteal reaction. There are no specific MRI manifestations of bone EHE; it usually shows intraosseous lesions with slightly long T1 and long T2 signals[12]. The lesions exhibit high signal intensity and apparent lobulation in T2-weighted images; on contrast-enhanced MRI, the lesions show homogenous contrast-enhancement with irregular borders. Regional involvement and multi-center distribution are important imaging manifestations of bone EHE; this may be related to the mode of venous return from long bones. Long bone veins flow back to the central venous sinus of bone marrow first, and then out of bone via veins accompanying the nutrient artery, epiphyseal artery, and metaphyseal artery[13].
In general, bone EHE shows slight to moderate uptake of 18F-FDG on 18F-FDG PET/CT. Treglia et al[14] reported a 38-year-old man with multiple soft tissue and bone EHE in the left lower extremity; the diagnosis was established by pathological examination of some 18F-FDG high uptake lesions. Song[15] reported a 45-year-old man with T2-4 vertebral body EHE, The T2 vertebra was compressed by a soft tissue mass invading the paravertebral region and spinal canal (SUVmax: 5.7). Slight to medium uptake of 18F-FDG uptake in bone EHE helps exclude the possibility of metastatic cancer. Although the imaging findings are non-specific, it may help differentiate from metastatic tumor, osteosarcoma, Langerhans cell histiocytosis, lymphomas, myeloma, giant cell tumor, and angiosarcoma. An expansive osteolytic lesion with no periosteal reaction, distinctive sclerotic margin, and soap-bubble matrix are the most commonly reported findings[16]. Lesions with ill-defined margins and marked loss of trabeculae are regarded as more aggressive[1,2]. In our study, a young patient presented with multiple bone destruction lesions at the junction of the left femoral head and head and neck and left ischium. Gross bone ridges were seen at the edges of the lesions, which indicated a high possibility of angiogenic lesions. Moreover, there was swelling of the peripheral soft tissues due to bone destruction accompanied by increased radioactive uptake. This suggested that the lesions had involved the surrounding muscles. However, in contrast to primary malignant lesions of muscles, there was no muscle mass. We initially suspected a primary malignant bone lesion. However, the MRI and 18F-FDG PET/CT findings pointed more towards bone EHE. Finally, the diagnosis of bone EHE was confirmed based on the pathological and immunohistochemical results.
Bone EHE is an uncommon primary vascular bone lesion which typically occurs in the long bones. Femoral presentation is extremely rare and very few patients have been described due to the non-specific imaging findings. In the present case, a diagnosis of femoral EHE was established aided by the MRI and PET/CT findings. The possibility of bone EHE should be considered in cases of bone destructive lesions characterized by regional involvement, multi-center distribution, and a slight to medium increase in metabolism on 18F-FDG PET/CT systemic scan. Simultaneously, the relatively slight to medium metabolism shown by FDG also indicates the low-grade malignant characteristics of the disease. As of the 18-mo follow-up, the patient showed no signs of recurrence on imaging examination.
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee SS S-Editor: Zhang H L-Editor: Webster JR P-Editor: Zhang YL
| 1. | Rosenberg A, Agulnik M. Epithelioid Hemangioendothelioma: Update on Diagnosis and Treatment. Curr Treat Options Oncol. 2018;19:19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 107] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 2. | Neves N, Lima-Rodrigues F, Ribeiro-Silva M, Cacho-Rodrigues P, Eloy C, Paiva ME, Pinto R. Epithelioid hemangioendothelioma presenting as a vertebral fracture. Acta Reumatol Port. 2010;35:370-374. [PubMed] |
| 3. | Verbeke SL, Bovée JV. Primary vascular tumors of bone: a spectrum of entities? Int J Clin Exp Pathol. 2011;4:541-551. [PubMed] |
| 4. | Balansay BE, Zhang X, Loftus PD, Aparicio Valenzuela J, Zambrano E, Lee AM. Diagnosing Epithelioid Hemangioendothelioma With Pericardial Involvement. Ann Thorac Surg. 2018;106:e173-e175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Kerry G, Marx O, Kraus D, Vogel M, Kaiser A, Ruedinger C, Steiner HH. Multifocal epithelioid hemangioendothelioma derived from the spine region: case report and literature review. Case Rep Oncol. 2012;5:91-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Brennan JW, Midha R, Ang LC, Perez-Ordonez B. Epithelioid hemangioendothelioma of the spine presenting as cervical myelopathy: case report. Neurosurgery. 2001;48:1166-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Hubaut MA, Jaillard A, Eloy C, Petyt G. 18F-FDG PET and Bone Scintigraphy of Epithelioid Hemangioendothelioma. Clin Nucl Med. 2019;44:127-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Zhao H, Han J, Qin L, Zhang C. Primary Left Tibial Epithelioid Hemangioendotheliomas With Multiple Metastases Revealed by FDG PET/CT Imaging. Clin Nucl Med. 2016;41:872-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Rao M, Chen Y, Huang Z, Zhu Y, Xiao X. FDG PET/CT Findings of Multifocal Epithelioid Hemangioendotheliomas of the Bones. Clin Nucl Med. 2015;40:821-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Albakr A, Schell M, Drew B, Cenic A. Epithelioid hemangioendothelioma of the spine: case report and review of the literature. J Spine Surg. 2017;3:250-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Gómez-Arellano LI, Ferrari-Carballo T, Domínguez-Malagón HR. Multicentric epithelioid hemangioendothelioma of bone. Report of a case with radiologic-pathologic correlation. Ann Diagn Pathol. 2012;16:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Munier O, Muckensturm B, Fesneau M, Wachter T. [Epithelioid hemangioendothelioma of the spine: A case report]. Cancer Radiother. 2017;21:222-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Yang H, Wang J, Song L, Zou H. Intraosseous epithelioid haemangioendothelioma of the mandible: A case report and literature review. Medicine (Baltimore). 2019;98:e16572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Treglia G, Ceriani L, Paone G, Rusca T, Bongiovanni M, Giovanella L. Multifocal epithelioid hemangioendothelioma of the lower limbs detected by 18F-FDG PET/MRI. Clin Nucl Med. 2014;39:e402-e404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Song L, Han S, Jiang L, Zhang W. F18-fluorodeoxyglucose positron emission tomography/computed tomography in the evaluation of vertebral vascular tumors. Clin Imaging. 2020;65:24-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Chen Y, Khanna A, Chen JQ, Zhang HZ, Caraway NP, Katz RL. Cytologic features, immunocytochemical findings, and DNA ploidy in four rare cases of epithelioid hemangioendothelioma involving effusions. Cytojournal. 2018;15:13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |