Published online Feb 16, 2021. doi: 10.12998/wjcc.v9.i5.1221
Peer-review started: November 21, 2020
First decision: December 3, 2020
Revised: December 13, 2020
Accepted: December 24, 2020
Article in press: December 24, 2020
Published online: February 16, 2021
Processing time: 70 Days and 2.4 Hours
Infective endocarditis (IE) is an uncommon but potentially life-threatening infection, which occasionally develops into acute severe valve insufficiency leading to the onset of heart failure, and necessitates timely intervention. However, the variable and atypical clinical manifestations always make the early detection of IE difficult and challenging.
A 45-year-old female who was previously healthy presented with exertional shortness of breath and paroxysmal nocturnal dyspnea. She also suffered from a significant decrease in exercise capacity, whereas her body temperature was normal. She had severe hypoxemia and hypotension along with a marked aortic valve murmur. Diffuse pulmonary edema and bilateral pleural effusion were observed on both chest X-ray and computed tomography scan. Transthoracic echocardiography was performed immediately and revealed severe regurgitation of the bicuspid aortic valve. Transesophageal echocardiography was further performed and vegetations were detected. In addition to adequate medical therapy and ventilation support, the patient underwent urgent and successful aortic valve replacement. Her symptoms were significantly relieved and the postoperative chest X-ray showed that pulmonary edema was significantly reduced. Histopathology of the resected valve and positive microorganism culture of the surgical specimen provided evidence of definite IE.
IE should be considered in critical patients with refractory heart failure caused by severe bicuspid aortic valve regurgitation.
Core Tip: Infective endocarditis (IE) is a relatively rare disease with diverse clinical manifestations. We present herein, an uncommon case of bicuspid aortic valve endocarditis in a critically ill patient with acute heart failure, which was finally confirmed by histopathology and microorganism culture. Due to normal body temperature and lack of specific transthoracic echocardiography findings, prompt diagnosis of IE is difficult. This case highlights the importance of transesophageal echocardiography for the detection of vegetations, and IE should be considered especially in patients with severe aortic valve regurgitation and resistant heart failure.
- Citation: Hou C, Wang WC, Chen H, Zhang YY, Wang WM. Infective bicuspid aortic valve endocarditis causing acute severe regurgitation and heart failure: A case report. World J Clin Cases 2021; 9(5): 1221-1227
- URL: https://www.wjgnet.com/2307-8960/full/v9/i5/1221.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i5.1221
Acute heart failure (AHF) is a fatal medical condition that may be caused by several precipitants. Identification of these factors and early initiation of appropriate therapy are extremely important[1]. Although the relationship between infective endocarditis (IE) and AHF is known[2], it is easily neglected in seriously ill patients without fever and positive transthoracic echocardiography (TTE) findings. Here, we present a case of AHF with bicuspid aortic valve (BAV) and severe aortic regurgitation attributable to IE. Following urgent surgical replacement of the affected valve, cardiogenic pulmonary edema was markedly improved.
A 45-year-old female presented to our Emergency Department with exertional breathlessness and paroxysmal nocturnal dyspnea.
The patient’s symptoms lasted almost 1 wk after catching a cold. She also complained of fatigue, poor appetite and weight loss. She denied fever, peripheral edema, chest and abdominal pain. Symptoms of petechiae, blindness, stroke, splinter hemorrhage and immunological phenomena were all absent, while exercise capacity was markedly reduced.
The patient was previously healthy, and there was no similar patient in the family history.
The patient had orthopnea and cyanosis. Her systolic blood pressure ranged from 10.67 to 12.00 kPa without tachycardia and signs of hypoperfusion. Pulmonary rales were heard and a marked heart murmur in the diastolic phase was found on auscultation of the aortic valve area.
Arterial blood gas revealed hypoxemia with an oxygenation index of 32.66 kPa. The laboratory tests indicated leukocytosis, anemia, abnormally high C-reactive protein, elevated rheumatoid factor and microscopic hematuria. Cardiac troponins, serum creatinine, blood electrolytes and procalcitonin level were normal. No abnormal findings were found with regard to antinuclear antibodies, anti-double-stranded deoxyribonucleic acid antibody, serum immunoglobulin or complement levels.
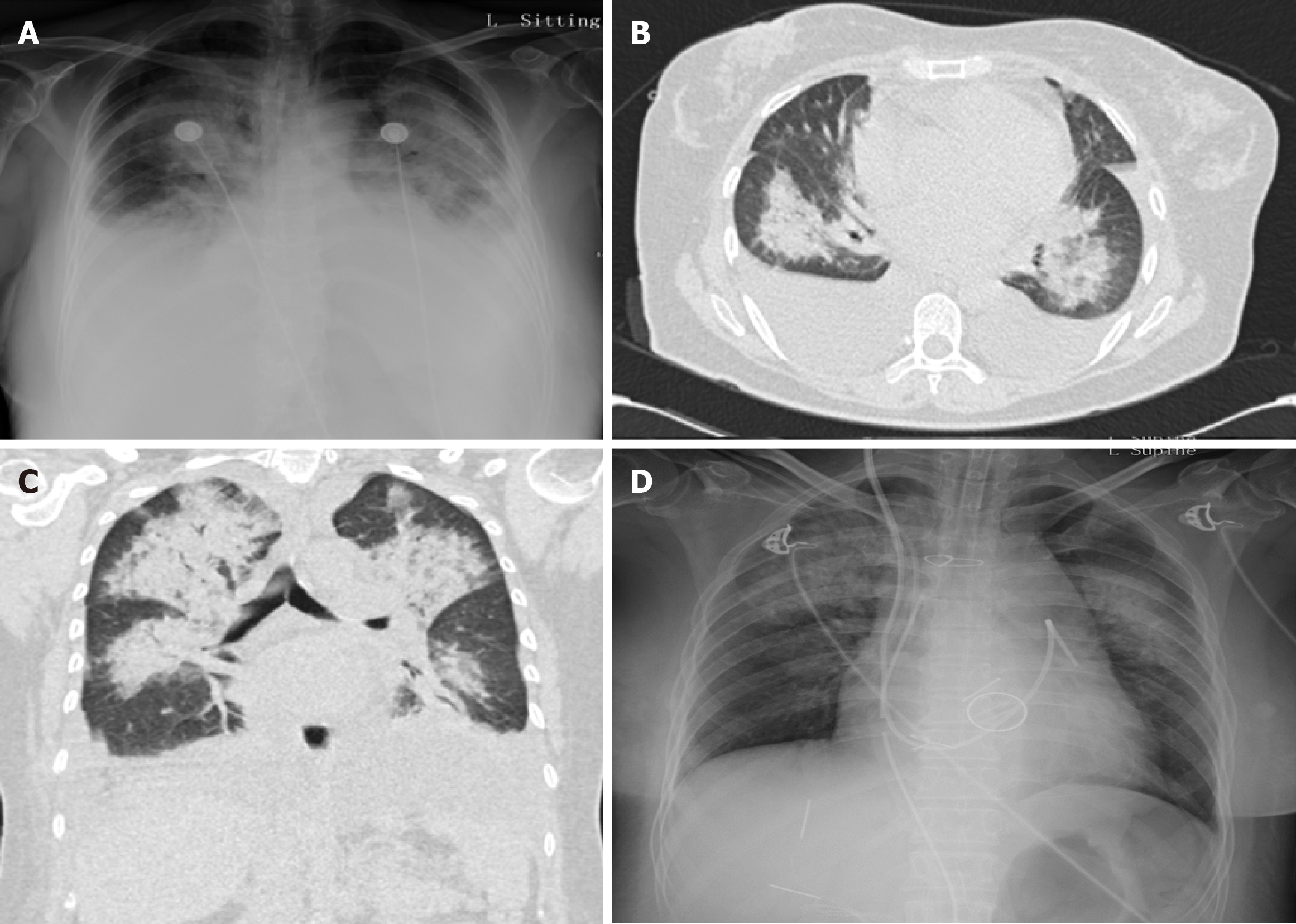
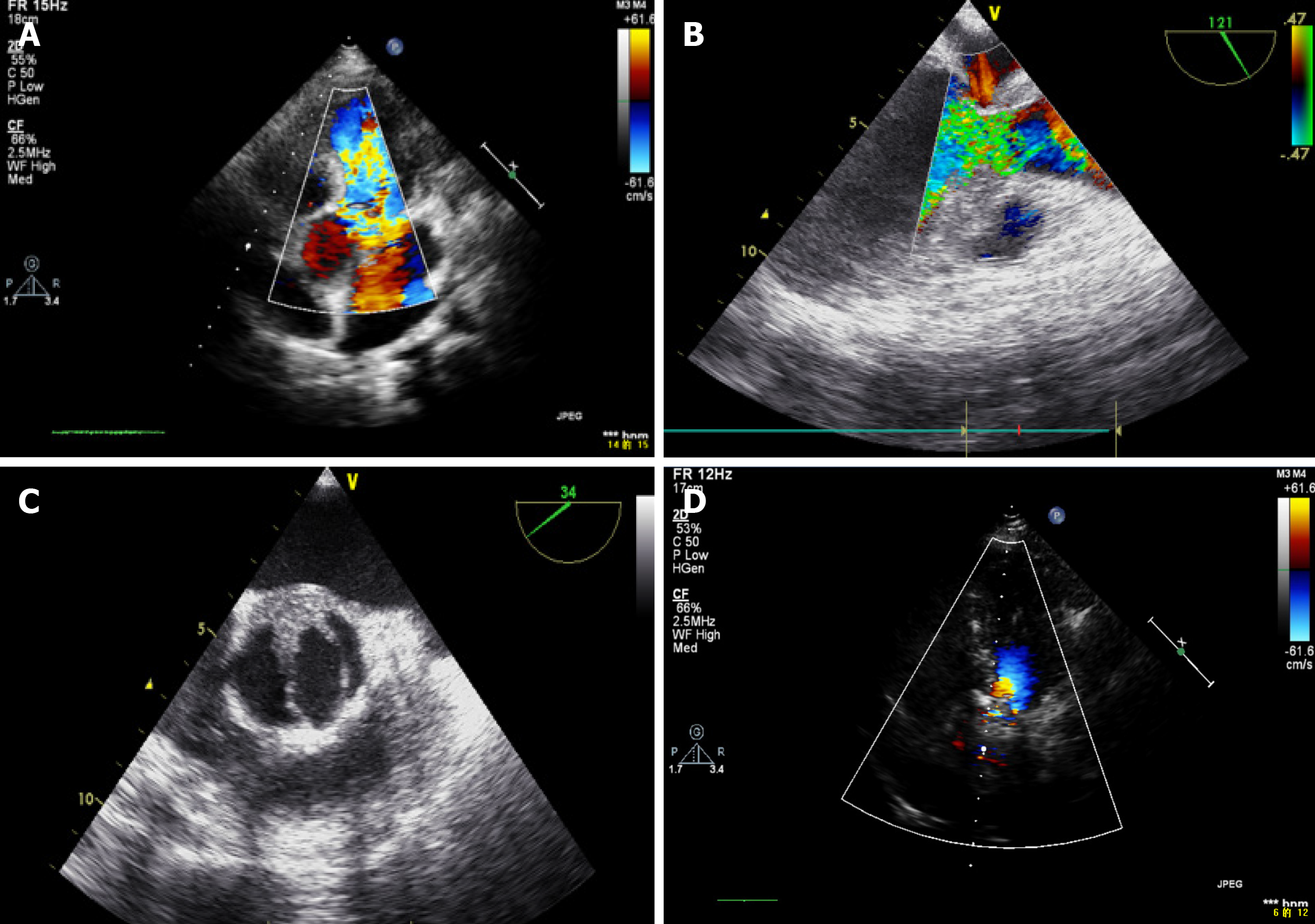
Chest X-ray and computed tomography showed diffuse pulmonary edema and bilateral pleural effusion (Figure 1A-C), which was proven to be transudate by diagnostic thoracentesis. The pulmonary capillary wedge pressure of 2.67 kPa was obtained invasively with a Swan-Ganz catheter. We immediately performed TTE (Table 1) and found severe regurgitation of the BAV (Figure 2A).
| June 26, 2019 | September 16, 2019 | |
| LVEDD | 5.2 cm | 4.4 cm |
| VST | 0.93 cm | 1.1 cm |
| PWT | 0.95 cm | 0.99 cm |
| LVMI | 117.7 g/m2 | 106.1 g/m2 |
| LVEF (Teich method) | 62.8% | 74.5% |
The patient underwent non-invasive positive pressure ventilation to alleviate dyspnea. A loop diuretic was given and adjusted according to the patient’s symptoms and blood pressure level. However, there was no adequate response to therapy and conversely respiratory distress was aggravated. We also performed transesophageal echocardiography (TEE) after cautiously balancing the operational benefit and risk, which clearly showed severe aortic regurgitation and vegetations attached to the BAV (Figure 2B and C).
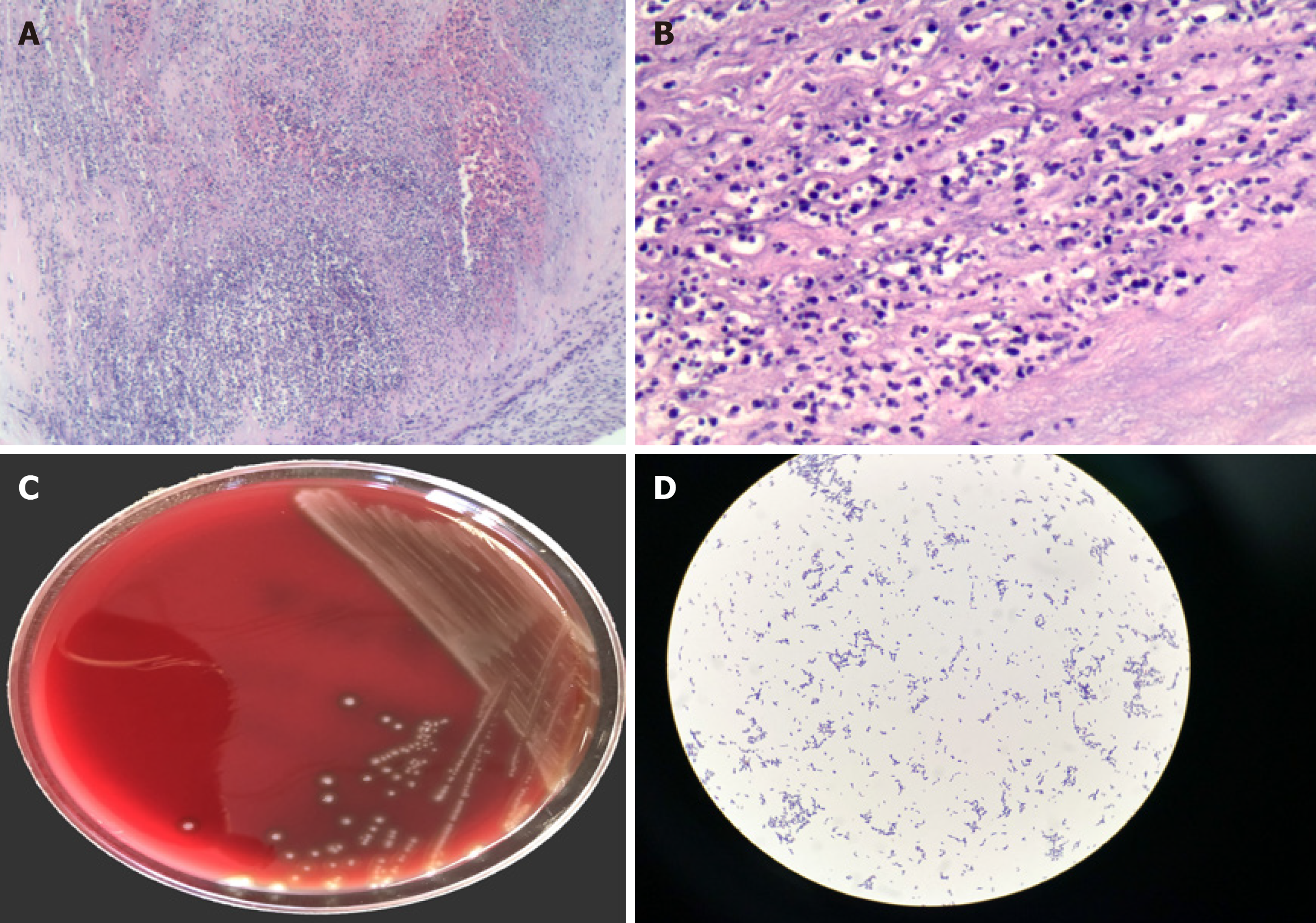
Histopathological examination together with the identification of Streptococcus sanguinis isolated from excised tissue samples confirmed the final diagnosis of IE (Figure 3).
Urgent replacement of the aortic valve using a mechanical prosthesis was successfully performed.
The patient experienced marked symptom relief and the post-procedural chest X-ray revealed that pulmonary edema and pleural effusion had significantly reduced (Figure 1D). Additionally, postoperative follow-up TTE showed normal function of the prosthetic valve (Figure 2D and Table 1).
Excess accumulation of extravascular lung water is manifested as pulmonary edema, which results in the need for mechanical ventilation[3]. In the present case, a pulmonary capillary wedge pressure of 2.67 kPa was measured invasively and suggested the diagnosis of cardiogenic pulmonary edema. Given the absence of previous cardiopulmonary diseases and normal left ventricular ejection fraction without chamber dilation, this patient was considered to have de novo onset of AHF.
It has been observed that heart failure occurs in 42%-60% of native valve endocarditis and is more often present when IE affects the aortic valve[4]. Patients with IE often have multiple comorbidities such as diabetes, cancer, intravenous drug use, degenerative valve disease and a congenital heart defect, and patients with BAV are at risk for IE[5-7]. It has also been reported that acute severe aortic regurgitation is mostly caused by IE[8]. In the present case, the patient developed significant aortic regurgitation, therefore the clinical suspicion of IE was high. Nevertheless, the identification of IE was still easily masked by normal body temperature and non-specific TTE findings as well as lack of typical signs.
The sensitivity of TTE for the detection of vegetations in a native valve is 70%[4]. Thus, initial negative TTE images do not definitely rule out IE, especially in those with a high possibility of IE who should undergo TEE[9]. Three-dimensional TEE has been shown to be useful in improving the diagnosis of this devastating disease[10]. However, due to ventilator-dependence and unstable status, TEE in the present case was risky and posed another challenge in the prompt diagnosis of IE.
Early surgery is indicated in patients with IE who present with valve dysfunction resulting in symptoms or signs of AHF[11,12]. Surgery must be performed emergently when patients have persistent pulmonary edema and cardiogenic shock and if specimens are available, histopathology of the resected valve remains the gold standard in the diagnosis of IE[4,5].
In conclusion, IE should be considered in patients with severe BAV regurgitation and persistent drug-resistant heart failure even in those without fever and typical signs. Although TEE is challenging and highly risky in patients with respiratory distress, it still plays an important role in the detection of vegetations and the diagnosis of IE.
The early identification and rapid diagnosis of IE remain difficult in individual patients, especially those who are critically ill with atypical manifestations. The diagnosis of IE should be considered in patients with acute serious BAV impairment and AHF despite optimal medical therapy.
The authors sincerely thank Yu C, Ma RY and Li SG, Peking University People’s Hospital, for their assistance in providing and interpreting the images in the present case.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yuan XC S-Editor: Fan JR L-Editor: Filipodia P-Editor: Li JH
| 1. | Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10348] [Cited by in RCA: 9323] [Article Influence: 1035.9] [Reference Citation Analysis (3)] |
| 2. | Cahill TJ, Baddour LM, Habib G, Hoen B, Salaun E, Pettersson GB, Schäfers HJ, Prendergast BD. Challenges in Infective Endocarditis. J Am Coll Cardiol. 2017;69:325-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 425] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 3. | Assaad S, Kratzert WB, Shelley B, Friedman MB, Perrino A Jr. Assessment of Pulmonary Edema: Principles and Practice. J Cardiothorac Vasc Anesth. 2018;32:901-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 4. | Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, Dulgheru R, El Khoury G, Erba PA, Iung B, Miro JM, Mulder BJ, Plonska-Gosciniak E, Price S, Roos-Hesselink J, Snygg-Martin U, Thuny F, Tornos Mas P, Vilacosta I, Zamorano JL; ESC Scientific Document Group. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075-3128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2661] [Cited by in RCA: 3335] [Article Influence: 333.5] [Reference Citation Analysis (0)] |
| 5. | Cahill TJ, Prendergast BD. Infective endocarditis. Lancet. 2016;387:882-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 656] [Article Influence: 72.9] [Reference Citation Analysis (0)] |
| 6. | Ward C. Clinical significance of the bicuspid aortic valve. Heart. 2000;83:81-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 547] [Cited by in RCA: 541] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 7. | Braverman AC. The bicuspid aortic valve and associated aortic disease. In: Otto CM, Bonow RO. Valvular heart disase. 4th ed. Philadelpha: Saunders Elsevier; 2013: 179. |
| 8. | Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL; ESC Scientific Document Group. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739-2791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4598] [Cited by in RCA: 4384] [Article Influence: 548.0] [Reference Citation Analysis (0)] |
| 9. | Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Tleyjeh IM, Rybak MJ, Barsic B, Lockhart PB, Gewitz MH, Levison ME, Bolger AF, Steckelberg JM, Baltimore RS, Fink AM, O'Gara P, Taubert KA; American Heart Association Committee on Rheumatic Fever; Endocarditis; and Kawasaki Disease of the Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; Council on Cardiovascular Surgery and Anesthesia; and Stroke Council. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals From the American Heart Association. Circulation. 2015;132:1435-1486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1569] [Cited by in RCA: 2089] [Article Influence: 208.9] [Reference Citation Analysis (1)] |
| 10. | Berdejo J, Shibayama K, Harada K, Tanaka J, Mihara H, Gurudevan SV, Siegel RJ, Shiota T. Evaluation of vegetation size and its relationship with embolism in infective endocarditis: a real-time 3-dimensional transesophageal echocardiography study. Circ Cardiovasc Imaging. 2014;7:149-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 11. | Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD; ACC/AHA Task Force Members. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:2440-2492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1016] [Cited by in RCA: 1075] [Article Influence: 97.7] [Reference Citation Analysis (0)] |
| 12. | Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O'Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;70:252-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1738] [Cited by in RCA: 1881] [Article Influence: 235.1] [Reference Citation Analysis (0)] |