Published online Feb 16, 2021. doi: 10.12998/wjcc.v9.i5.1168
Peer-review started: October 20, 2020
First decision: November 24, 2020
Revised: November 28, 2020
Accepted: December 11, 2020
Article in press: December 11, 2020
Published online: February 16, 2021
Processing time: 101 Days and 18.8 Hours
Cases of obturator nerve impingement (ONI) caused by osteophytes resulting from bone hyperplasia on the sacroiliac articular surface have never been reported. This paper presents such a case in a patient in whom severe lower limb pain was caused by osteophyte compression of the sacroiliac joint on the obturator nerve.
A 65-year-old Asian man presented with severe pain and numbness in his left lower limb, which became aggravated during walking and showed intermittent claudication. The physical examination revealed that the muscle strength of the left lower limb had decreased and that the passive knee flexion test result was positive. Computed tomography (CT) and 3D reconstruction showed a large osteophyte located in the anterior lower part of the left sacroiliac joint. The results of electrophysiological examination showed peripheral neuropathy. A CT-guided obturator nerve block significantly reduced the severity of pain in this patient. According to the above findings, ONI caused by the osteophyte in the sacroiliac joint was diagnosed. This patient underwent an operation to remove the bone spur and symptomatic treatment. After therapy, the patient's pain and numbness were significantly relieved. The last follow-up was performed 6 mo after the operation, and the patient recovered well without other complications, returned to work, and resumed his normal lifestyle.
Osteophytes of the sacroiliac joint can cause ONI, which leads to symptoms including severe radiative pain in the lower limb in patients. The diagnosis and differentiation of this disease should attract the attention of clinicians. Surgical excision of osteophytes should be considered when conservative treatment is not effective.
Core Tip: Obturator nerve impingement is a peripheral neurogenic disease. It has a low incidence, but symptoms such as pain will affect the work and life of patients. Since the nerve runs deep and belongs to the peripheral nerve, the exact diagnosis is challenging. We present a very rare case of severe pain and numbness in the left lower extremity due to obturator nerve compression by an osteophyte of the sacroiliac joint. Our report could help clinicians diagnose and treat this disease better. Meanwhile, it provides a new idea for unexplained lower limb pain.
- Citation: Cai MD, Zhang HF, Fan YG, Su XJ, Xia L. Obturator nerve impingement caused by an osteophyte in the sacroiliac joint: A case report. World J Clin Cases 2021; 9(5): 1168-1174
- URL: https://www.wjgnet.com/2307-8960/full/v9/i5/1168.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i5.1168
The obturator nerve is composed of the anterior branches of the 2nd to 4th lumbar nerves in the anterior thigh. After the obturator nerve exits the medial edge of the psoas muscle, it enters the small pelvis toward the thigh and is divided into the anterior and posterior branches. The muscle branches of that nerve innervate the obturator externus and the adductor muscles of the thigh, while the cutaneous branches are distributed on the skin on the inner side of the thigh. In addition, some branches of the obturator nerve reach the hip and knee joints. Obturator nerve injury often causes pain and numbness in the inner thigh and front of the knee and joint movement disorders[1]. Some nerves, including the obturator nerve, need to pass through the surface of the sacroiliac joint during walking. As individuals age, because of bone hyperplasia, this joint can produce osteophytes that entrap the nerve traveling from it. Previous studies have reported cases of sciatica caused by osteophytes behind the sacroiliac joint[2]. However, cases of obturator neuralgia caused by osteophytes in the front of the same joint have not been reported before.
The diagnosis of this disease may be challenging due to its low prevalence. At present, obturator nerve impingement (ONI) is mainly diagnosed on the basis of the clinical manifestations and imaging findings, and the diagnosis is confirmed by determining whether a local nerve block is effective in treating the case[3]. Of course, the effects of other diseases need to be ruled out. We herein present a rare case of pain and numbness in the left lower extremity due to compression of the obturator nerve by an osteophyte in the anterior inferior sacroiliac joint. The diagnostic and treatment processes for this case are explained in detail as well.
A 65-year-old man presented with a 14-d history of numbness and pain in the left lower limb, which became aggravated after physical activity.
The patient had a 2-wk history of numbness and pain in his left lower limb when carrying heavy loads, which became aggravated during walking and showed intermittent claudication. The numbness and pain were mainly located on the medial aspect of the thigh and extended to the left knee. The patient could not sleep supinely due to the pain. He had previously visited a local hospital and received symptomatic treatment with painkillers for 2 wk. The pain, however, was still severe, and the patient’s quality of life was severely affected. For further diagnosis and treatment, this patient came to our hospital. The initial diagnosis was "left lower extremity pain of unknown origin with dyskinesia". The patient had a good general condition since onset.
The patient could not sleep supinely due to the pain. He had previously visited a local hospital and received symptomatic treatment with painkillers for 2 wk. The pain, however, was still severe, and the patient’s quality of life was severely affected.
The patient had no family history of genetic disease.
The physical examination revealed numbness and pain in his left groin and inner thigh, as well as tenderness on the medial side of the left knee joint. The visual analog scale (VAS) pain score was 7 (severe pain). The patient walked with an abnormal pattern and posture: He bent his back and put his left hand on his left thigh. The passive knee flexion test result was positive. This patient had a normal muscle tone, and the level of muscle strength was grade V in the right lower limb and IV in the left lower limb. The knee and Achilles tendon reflexes were normal, and the Babinski sign was negative on both sides.
No obvious abnormalities were found in laboratory examinations.
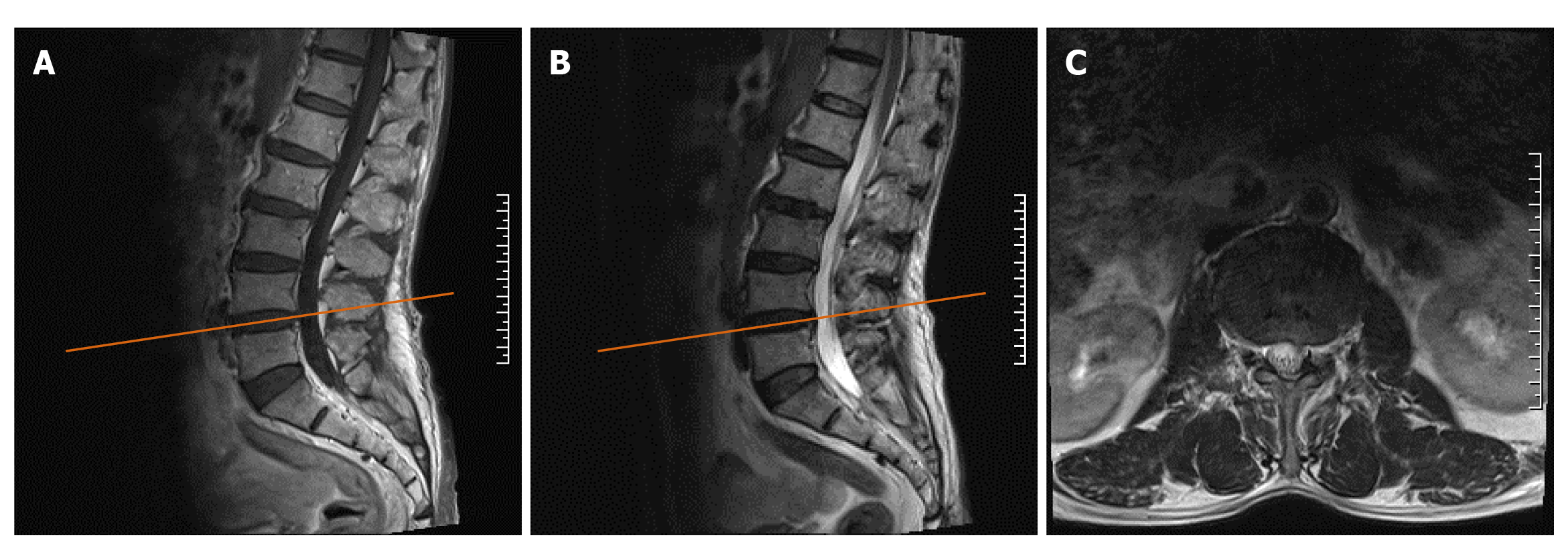
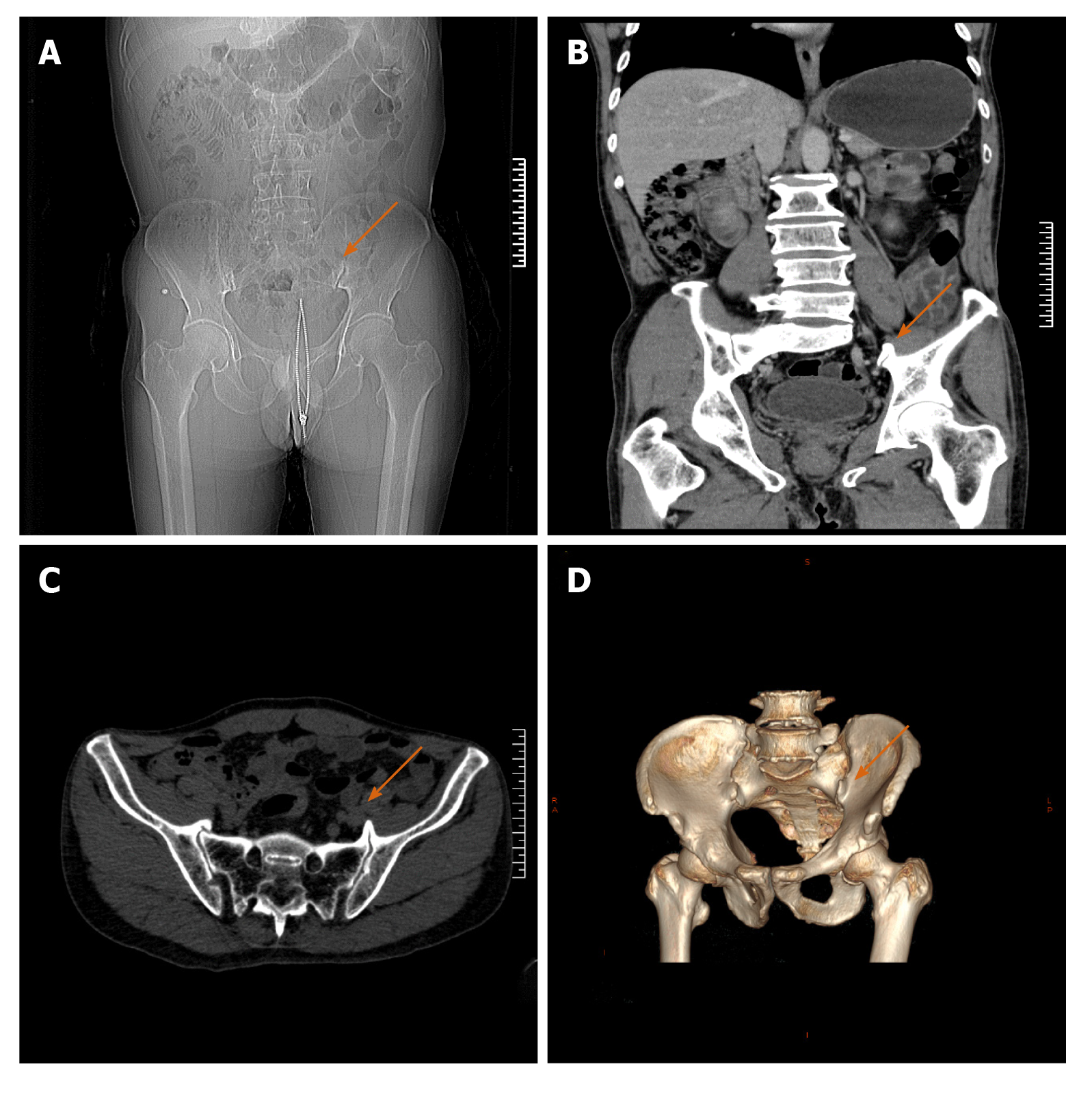
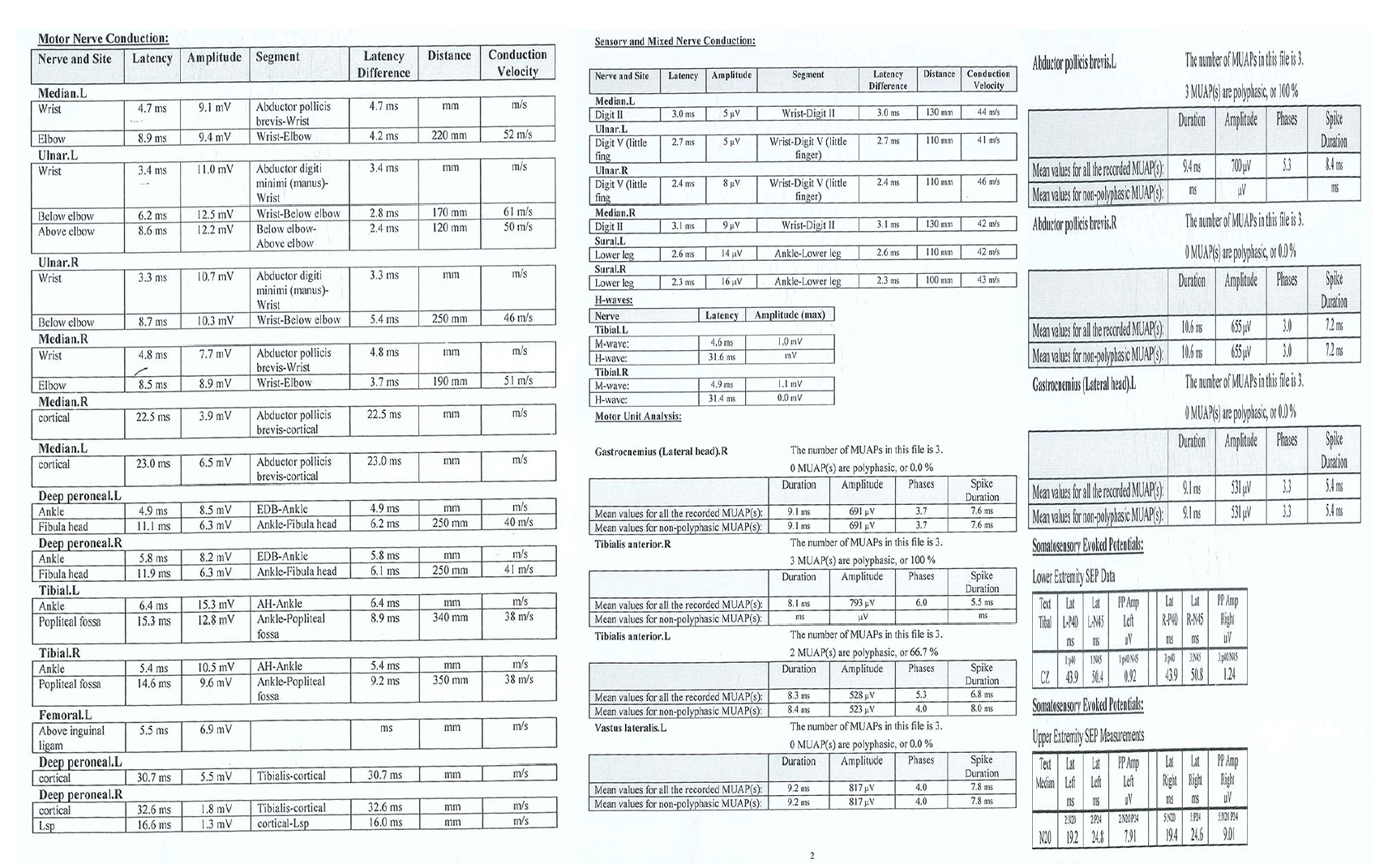
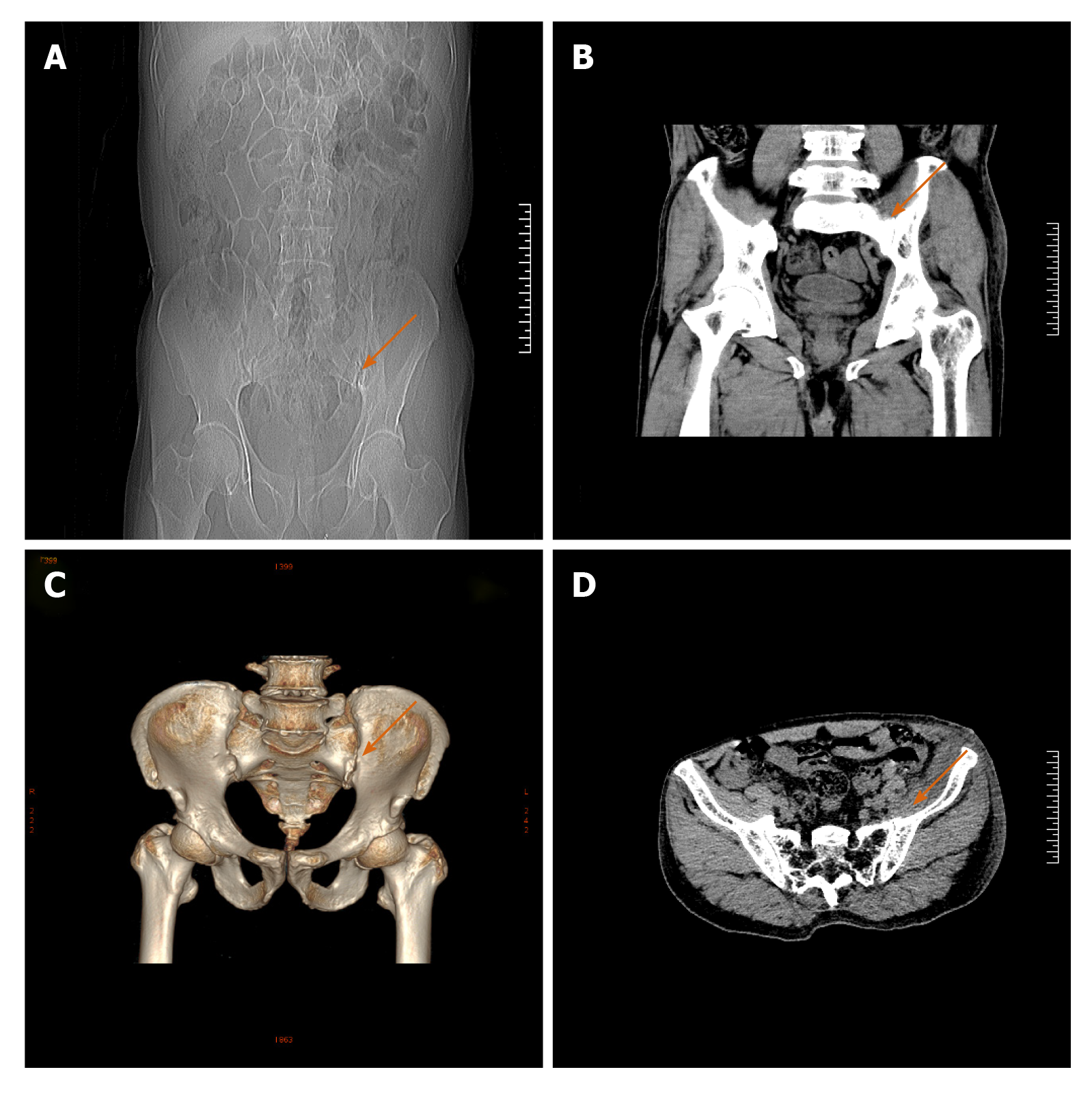
The plain X-ray scans of the two knees and right hip showed no obvious abnormalities except mild hyperosteogeny. The plain and dynamic enhanced magnetic resonance imaging scans showed slight disc bulging at the L4-L5 level (Figure 1A-C). The pelvic computed tomography (CT) scan plus 3D reconstruction revealed bilateral sacroiliac joint osteophyte formation (Figure 2A-D), and the left osteophyte was larger (arrow). The electromyography and nerve conduction velocity studies showed partial peripheral nerve damage in both lower extremities (Figure 3A-C).
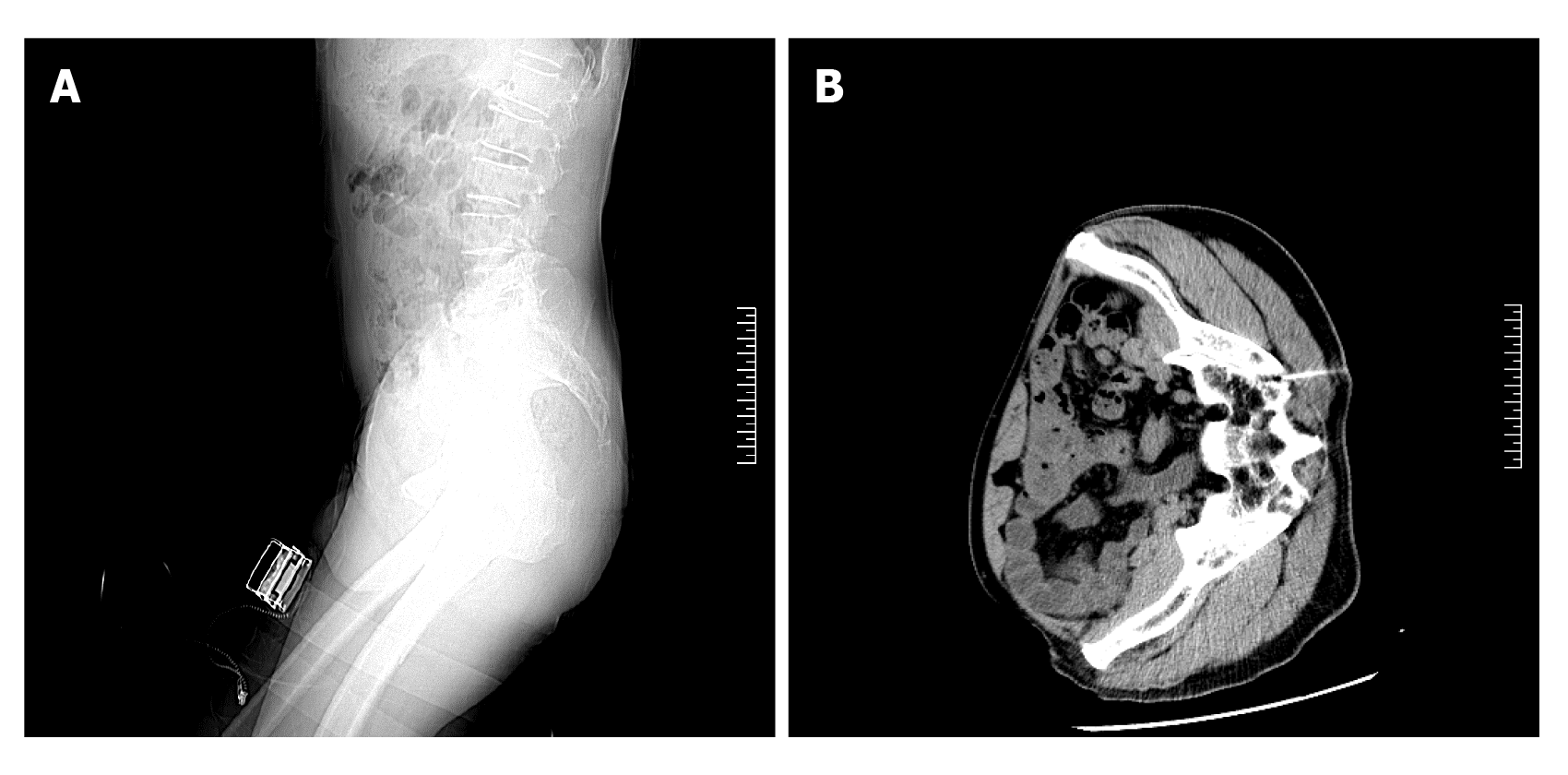
A CT-guided diagnostic obturator nerve local block was performed at the site of the left sacroiliac joint osteophyte[4,5] (Figure 4A and B). Immediately after surgery, the patient felt that the pain had significantly reduced, and the passive knee flexion test result became negative. In addition, intermittent claudication disappeared. However, the pain recurred the next day after the local block and could not be relieved after conservative therapy for a week.
The final diagnosis was ONI caused by an osteophyte in the sacroiliac joint with mild lumbar disc herniation.
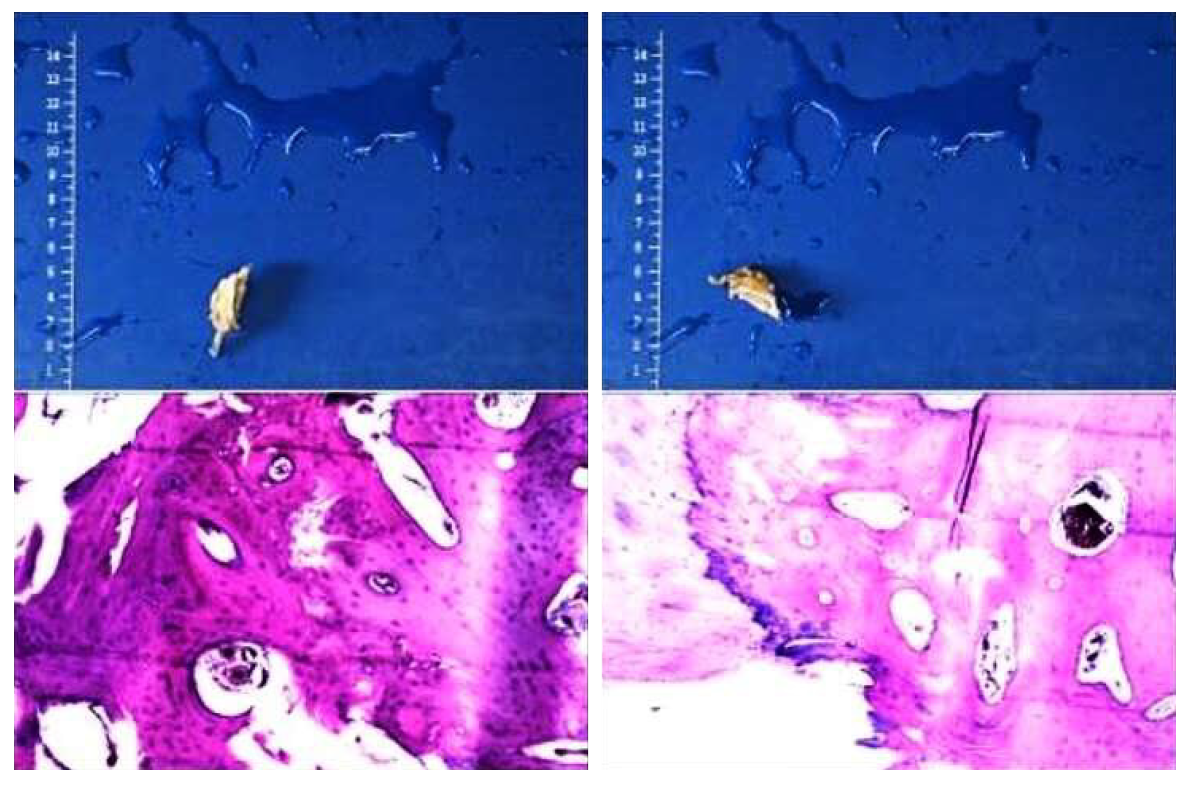
The patient was treated by surgery via an anterior approach to remove the osteophyte in the sacroiliac joint. A hard bone spur (2.5 cm × 2.2 cm × 1.3 cm) was found, which seemed to protrude from the anterior side of the left sacroiliac joint, and the patient had poor mobility. The hyperplastic component was excised along the base of the joint by using an osteotome, and wound healing was promoted with bone wax. Then, the specimen was sent for a routine pathological examination.
After the operation, the patient reported that the pain was significantly relieved (VAS 1), and he could sleep supinely and walk normally again without using analgesics. A CT scan after the surgery revealed that the left sacroiliac joint osteophyte was completely removed (Figure 5A and D). The pathological results showed that there was mature bone and cartilage tissue, which were consistent with benign lesions (Figure 6). At the 6-mo postoperative follow-up, the patient had returned to his normal lifestyle.
ONI is relatively rare but can severely affect a patient’s ability to work and quality of life. It is a peripheral neurogenic disease. Because the nerve lies protected deep within the pelvis and medial thigh, ONI is infrequent but may arise from direct trauma due to pelvic fractures, particularly those that affect the sacroiliac joint. Total hip arthroplasty, pelvic operations, and femoral artery procedures, as well as compression caused by tumors or metastatic diseases, have also been implicated[6-8]. However, as far as we know, cases of this disease caused by osteophytes have not been reported. At present, this disease is mainly diagnosed on the basis of physical examination and imaging findings, and the diagnosis is confirmed by determining whether nerve block treatment is an effective treatment. Regarding sacroiliac joint degeneration and osteophytes, studies have shown that osteophytes are more common in men than in women and particularly common on the anterior surface of the joint[9]. Kumar et al[2] have previously reported cases of sciatica caused by sacroiliac joint osteophytes. It can be seen that the formation of osteophytes on the sacroiliac joint surface can lead to neurological symptoms, which can be confirmed by auxiliary examinations combined with nerve blocks. If conservative treatment cannot relieve the pain or improve the patient’s ability to work or quality of life, surgical treatment should be considered.
ONI caused by bone spurs is rather uncommon. We report a rare case that may be important for further research on this disease. Therefore, when patients have unexplained radiating pain in the lower extremities and other causes can be ruled out, this rare disease should be considered.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aota Y S-Editor: Huang P L-Editor: Wang TQ P-Editor: Wang LYT
| 1. | Bowley MP, Doughty CT. Entrapment Neuropathies of the Lower Extremity. Med Clin North Am. 2019;103:371-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 2. | Kumar B, Sriram KG, George C. Osteophyte at the sacroiliac joint as a cause of sciatica: a report of four cases. J Orthop Surg (Hong Kong). 2002;10:73-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Tipton JS. Obturator neuropathy. Curr Rev Musculoskelet Med. 2008;1:234-237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | House CV, Ali KE, Bradshaw C, Connell DA. CT-guided obturator nerve block via the posterior approach. Skeletal Radiol. 2006;35:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Heywang-Köbrunner SH, Amaya B, Okoniewski M, Pickuth D, Spielmann RP. CT-guided obturator nerve block for diagnosis and treatment of painful conditions of the hip. Eur Radiol. 2001;11:1047-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 41] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Sorenson EJ, Chen JJ, Daube JR. Obturator neuropathy: causes and outcome. Muscle Nerve. 2002;25:605-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 55] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Kleiner JB, Thorne RP. Obturator neuropathy caused by an aneurysm of the hypogastric artery. A case report. J Bone Joint Surg Am. 1989;71:1408-1409. [PubMed] |
| 8. | Rogers LR, Borkowski GP, Albers JW, Levin KH, Barohn RJ, Mitsumoto H. Obturator mononeuropathy caused by pelvic cancer: six cases. Neurology. 1993;43:1489-1492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Shibata Y, Shirai Y, Miyamoto M. The aging process in the sacroiliac joint: helical computed tomography analysis. J Orthop Sci. 2002;7:12-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |