Published online Feb 16, 2021. doi: 10.12998/wjcc.v9.i5.1132
Peer-review started: September 4, 2020
First decision: November 30, 2020
Revised: December 24, 2020
Accepted: January 5, 2021
Article in press: January 5, 2021
Published online: February 16, 2021
Processing time: 148 Days and 2.8 Hours
Although the imaging features of coronavirus disease 2019 (COVID-19) are starting to be well determined, what actually occurs within the bronchi is poorly known. Here, we report the processes and findings of bronchoscopy in a patient with COVID-19 accompanied by respiratory failure.
A 65-year-old male patient was admitted to the Hainan General Hospital on February 3, 2020 for fever and shortness of breath for 13 d that worsened for the last 2 d. The severe acute respiratory syndrome coronavirus 2 nucleic acid test was positive. Routine blood examination on February 28 showed a white blood cell count of 11.02 × 109/L, 86.9% of neutrophils, 6.4% of lymphocytes, absolute lymphocyte count of 0.71 × 109/L, procalcitonin of 2.260 ng/mL, and C-reactive protein of 142.61 mg/L. Oxygen saturation was 46% at baseline and turned to 94% after ventilation. The patient underwent video bronchoscopy. The tracheal cartilage ring was clear, and no deformity was found in the lumen. The trachea and bilateral bronchi were patent, while the mucosa was with slight hyperemia; no neoplasm or ulcer was found. Moderate amounts of white gelatinous secretions were found in the dorsal segment of the left inferior lobe, and the bronchial lumen was patent after sputum aspiration. The right inferior lobe was found with hyperemia and mucosal erosion, with white gelatinous secretion attachment. The patient’s condition did not improve after the application of therapeutic bronchoscopy.
For patients with COVID-19 and respiratory failure, bronchoscopy can be performed under mechanical ventilation to clarify the airway conditions. Protection should be worn during the process. Considering the risk of infection, it is not necessary to perform bronchoscopy in the mild to moderate COVID-19 patients.
Core Tip: A 65-year-old male patient was admitted to the Hainan General Hospital on February 3, 2020 for fever and shortness of breath for 13 d that worsened for the last 2 d. The severe acute respiratory syndrome coronavirus 2 nucleic acid test was positive. Routine blood examination on February 28 showed a white blood cell count of 11.02 × 109/L, 86.9% of neutrophils, 6.4% of lymphocytes, absolute lymphocyte count of 0.71 × 109/L, procalcitonin of 2.260 ng/mL, and C-reactive protein of 142.61 mg/L. Oxygen saturation was 46% at baseline and turned to 94% after ventilation.
- Citation: Chen QY, He YS, Liu K, Cao J, Chen YX. Bronchoscopy for diagnosis of COVID-19 with respiratory failure: A case report. World J Clin Cases 2021; 9(5): 1132-1138
- URL: https://www.wjgnet.com/2307-8960/full/v9/i5/1132.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i5.1132
Coronavirus disease 2019 (COVID-19) is a global pandemic acute respiratory disease that first appeared in Wuhan (Hubei, China) in December 2019[1,2]. The pandemic spread rapidly to nearly all countries around the world, with 3917366 confirmed cases and 274361 deaths as of May 10, 2020[3]. On January 7, 2020, genomic sequencing of the pathogens isolated from the airway samples of patients was firstly conducted by Chinese investigators, and the findings demonstrated that the epidemic was caused by a novel coronavirus[4]. The virus was named severe acute respiratory syndrome coronavirus 2 by the International Committee on Taxonomy of Viruses[5].
The disease is mainly transmitted by respiratory droplets and close contacts and is transmitted from humans to humans[6]. The common signs of COVID-19 include fever, cough, and shortness of breath[2]. The severity of the COVID-19 could be classified as mild, regular, severe, and critical[7]. There is no specific antiviral treatment for COVID-19, but supportive care may help relieve symptoms and should include support of vital organ functions in severe cases[2]. Severe and critical cases require oxygen support and mechanical ventilation[2]. Death is usually due to respiratory failure, but emerging evidence indicates that inflammation, thromboembolism, and multi-organ failure could be involved[1,2,8].
Although the imaging features of COVID-19 are starting to be well determined[9-11], what actually occurs within the bronchi is poorly known. Bronchoscopy adds important information in this regard but carries a high risk of aerosol spread of the virus, so its use must be carefully evaluated before use in emergency and necessary situations such as unexplained increase in airway pressure or lung collapse[12,13]. Here, we report the processes and findings of bronchoscopy in one patient with COVID-19 accompanied by respiratory failure. In addition, the related literature is reviewed to provide evidence in helping understand the advantages and disadvantages of bronchoscopy in such cases, as well as improving the bronchoscopy in COVID-19 patients.
A 65-year-old male patient was admitted to the Hainan General Hospital on February 3, 2020 for fever and shortness of breath for 13 d that worsened for the last 2 d. The patient is from Wuhan, Hubei, traveled to Haikou by plane on January 21, 2020, and then drove to Danzhou, Hainan using a rented car.
The fever appeared 13 d before the admission, with the highest body temperature being 38.0 °C, which was accompanied by chilling, shortness of breath, headache, and weakness. No cough, expectoration, chest distress, or chest pain was reported. The severe acute respiratory syndrome coronavirus 2 nucleic acid test was initially performed at the Danzhou People’s Hospital and was positive. Due to the shortness of breath worsening, the patient was transferred to the Hainan General Hospital.
The patient had a 20-year history of hypertension and was treated with oral metoprolol 23.75 mg/d. The patient underwent minimally invasive surgery for atrial fibrillation 2 years before at Wuhan Union Hospital.
The patient was born and raised in Wuhan without family history of genetic disease, psychosis, and tumor.
Physical examination showed that the body temperature was 36.0 °C, pulse was 110 beats/min, respiration was 30 breaths/min, blood pressure was 179/99 mmHg, and blood oxygen saturation was 46%.
Tracheal intubation was conducted immediately after hospitalization, and mechanical ventilation was used. The mechanical ventilator settings were assisted ventilation, synchronized intermittent mandatory ventilation (SIMV) mode, FiO2 50%, ventricular tachycardia (VT) 480 mL, respiratory rate (f) 20 times/min, polystyrene (PS) 12
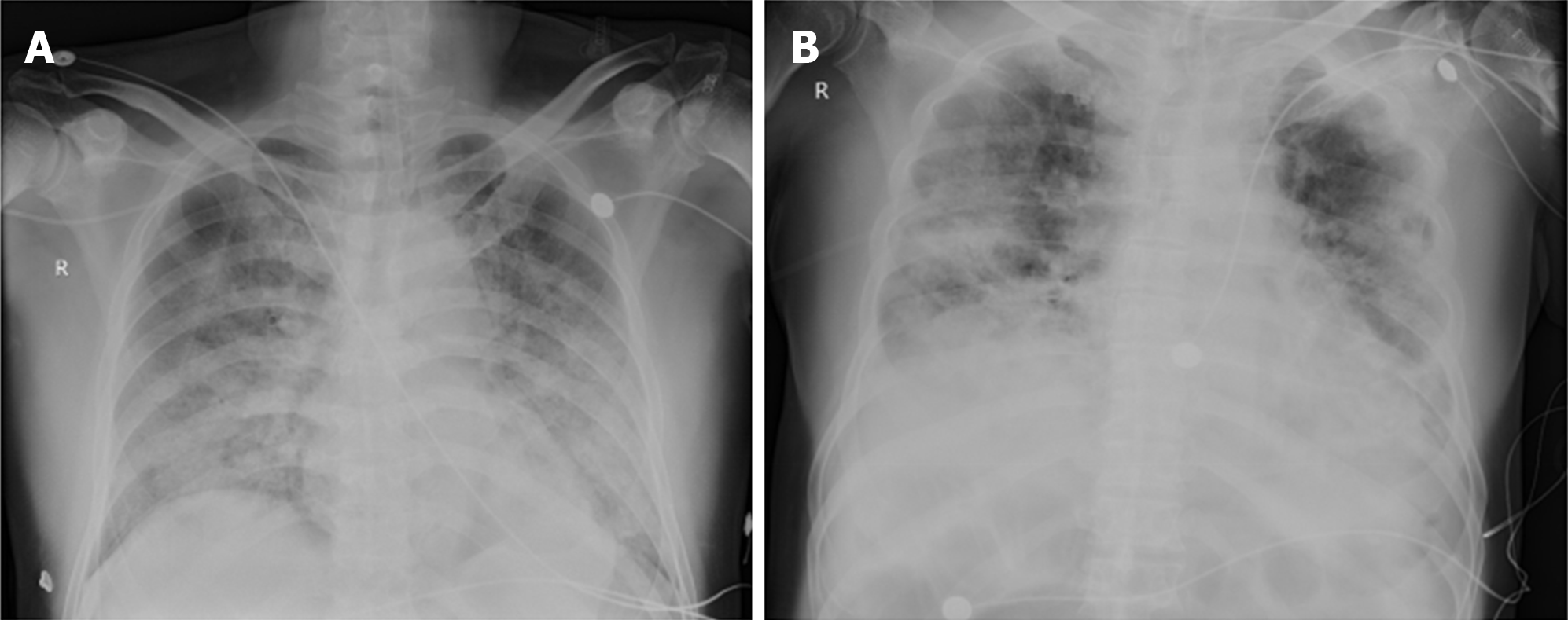
Chest imaging was completed (Figure 1). For patients with pulmonary exudation, bronchoscopy can be used to observe the condition of airway secretions and to remove them. During the hospitalization, the patient changed from type I to type II respiratory failure, and there was insufficient ventilation. Therefore, bronchoscopy was carried out to determine the cause of airway problems and observe for lesions. The patient underwent video bronchoscopy [QG-3490 (4.8-2.2); Zhuhai seesheen Medical Technology Co., Ltd., Zhuhai, China]. The one-piece protective suit and full-face respiratory protective device were worn according to the level-3 protection standards for infectious diseases before entering the negative-pressure ward. Intravenous injection of midazolam (3 mg) was performed at 5 min before bronchoscopy, and propofol (30 µg/min/kg) and remifentanil (0.1 µg/min/kg) were used for sedation and analgesia. The richmond agitation-sedation scale score of the patient was maintained at -4 points. The mechanical ventilator was set to the SIMV mode, with FiO2 100%, VT 480 mL, f 20 times/min, PS 12 cmH2O, and PEEP 5 cmH2O. Sterilized paraffin oil was applied to the surface of the bronchoscope, which was inserted through the working access of the universal joint that was connected to the tracheal catheter.
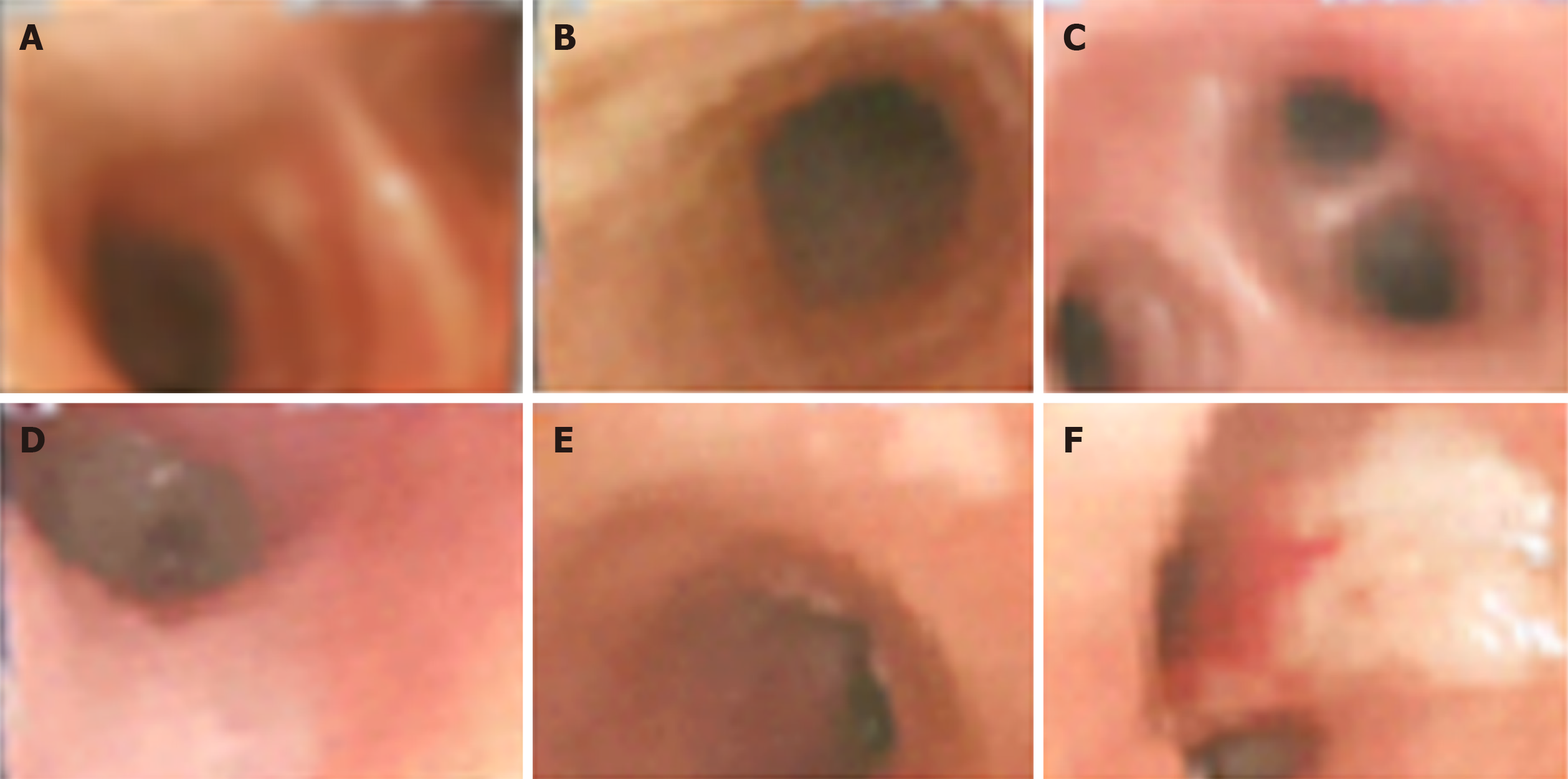
The tracheal cartilage ring was clear, and no deformity was found in the lumen. The trachea and bilateral bronchi were patent, while the mucosa was with slight hyperemia; no neoplasm or ulcer was found. Moderate amounts of white gelatinous secretions were found in the dorsal segment of the left inferior lobe, and the bronchial lumen was patent after sputum aspiration. The right inferior lobe was found with hyperemia and mucosal erosion, with white gelatinous secretion attachment (Figure 2).
The patient received intravenous injection of midazolam (3 mg) 5 min before video bronchoscopy [QG- 3490 (4.8-2.2); Zhuhai Seesheen Medical Technology Co., Ltd., Zhuhai, China] to determine the cause of airway problems and observe for lesions. Propofol (30 µg/min/kg) and remifentanil (0.1 µg/min/kg) were used for sedation and analgesia. The richmond agitation-sedation scale score of the patient was maintained at -4 points. The mechanical ventilator was set to the SIMV mode, with FiO2 100%, VT 480 mL, f 20 times/min, PS 12 cmH2O, and PEEP 5 cmH2O. Sterilized paraffin oil was applied to the surface of the bronchoscope, which was inserted through the working access of the universal joint that was connected to the tracheal catheter.
The patient’s condition did not improve after the application of therapeutic bronchoscopy.
The condition of the patient deteriorated, prompting hospitalization, and he was in a critical condition because of respiratory failure on admission. This deterioration could be due to his advanced age, delayed hospitalization, and the existence of comorbidities such as hypertension. Of course, the natural history of COVID-19 is still poorly understood, and additional aggravation factors could have been missed. Angiotensin-converting enzyme inhibitors were not used by the patient, and the disease severity was not significantly associated with anti-hypertensive drugs such as angiotensin-converting enzyme inhibitors[14].
During COVID-19, the pulmonary exudation in this patient was evident. During disease progression, the blood oxygen saturation decreased to dramatic levels, and PCO2 increased, indicated poor ventilation. The patient was diagnosed with critical COVID-19 accompanied with type II respiratory failure that required mechanical ventilation. For pneumonia patients with ventilation and gas-exchange dysfunctions, bronchoscopy might help clarify the airway conditions, identify the hidden pulmonary lesions, and remove airway secretions, which could improve ventilation to some extent[15]. Bronchoscopy in this patient showed no secretions in the trachea and bilateral bronchi, while the mucosa was with slight hyperemia. Moderate amounts of white gelatinous secretions were found in the dorsal segment of the left inferior lobe. These findings were generally in agreement with the autopsy findings of COVID-19 patients[16]. The findings also suggested that the airway secretions were from the respiratory bronchiole, namely, the small terminal airways, alveolar ducts, alveolar sacs, and alveoli, which have ventilation and gas-exchange functions. These structures have no goblet cells with high mucosa-secretion functions and are where COVID-19 seems to occur[17]. These findings could explain the low blood oxygen saturation and increased PCO2 in the patient.
The patient was with ventilator-associated pneumonia in addition to viral pneumonia. Tracheal intubation and tracheotomy provide conditions favoring the bacteria breeding, damages of the respiratory mucosal barrier, and reduction of immunity. Ventilator-associated pneumonia is the most common complication of mechanical ventilation[18]. After the occurrence of ventilator-associated pneumonia, diagnostic bronchoscopy could shorten antibiotic treatment and hospital stay[19]. Nevertheless, in this case, the application of therapeutic bronchoscopy achieved no evident benefits.
Nevertheless, the bronchoscopy clarified the airway conditions of the patients with critical COVID-19 accompanied by type II respiratory failure. In addition, bronchoscopy could directly visualize the lesion and accurately and completely remove the airway secretions, but the damage was relatively mild. Therefore, bronchoscopy could avoid the aimlessness of routine sputum suction and increase ventilation efficiency[20]. A bronchoscopic examination might be necessary for critical COVID-19 patients accompanied by respiratory failure. In order to ensure the safety of patients, the ventilator should not be stopped during the procedures, and the oxygen concentration should be increased at the same time to ensure the oxygen supply during the procedures. Nevertheless, it has to be noted that some societies issued guidelines about the use of bronchoscopy in the context of COVID-19[12,21-23], but none address specifically the case of diagnostic and therapeutic bronchoscopy in patients with COVID, mainly because of the lack of data[24].
It is important to note that bronchoscopy is not recommended in patients with mild COVID-19[12,13]. COVID-19 is transmitted through respiratory droplets and close contacts[7]. The bronchoscopy physician could come in contact with the respiratory secretions, and bronchoscopy might induce aerosol spread, and thus the risk is extremely high. It has been suggested that bronchoscopy in patients with COVID-19 should be strictly kept for emergency and necessary situations[12,13]. In this case, bronchoscopy was performed because the patient’s pCO2 was still elevated under invasive mechanical ventilation, that is, type II respiratory failure. Because this patient has already undergone invasive mechanical ventilation, bronchoscopy was easier to perform. Therefore, in similar cases protection is very important, not only for the physicians and personnel but also to prevent the spread of the virus to unaffected patients[25]. The following items could be considered. First, level-3 protection standards for infectious diseases should be used by the operators, and a full-face respiratory protective device should be worn. Second, before the examination, the patients should receive sedatives and analgesics, which could ease the nervousness, reduce cough, and decrease the spraying of droplets, thus protecting the operators and increasing the safety and comfort of the procedures. Third, the bronchoscope was inserted through the working access of the universal joint connected to the tracheal catheter, and paraffin oil was applied to the surface of the bronchoscope, which could increase the smoothness of the procedures and also help isolate the airway and external environment. Finally, the skillfulness of the operators and a gentle and swift operation could shorten the time of procedures in the trachea as possible.
For mild to moderate COVID-19 patients, there is no need for bronchoscopy, while for patients with respiratory failure and high amounts of exudative lesions in the lung, bronchoscopy examinations can be necessary under respiratory assistance by the ventilator. Nevertheless, the operators are at high risk of infection when performing bronchoscopic diagnosis and treatment for COVID-19 patients. In addition, the airway secretions in such patients might be limited. Therefore, frequent examinations in such patients are not necessary, and bronchial lavage could be performed according to the amount of airway secretions.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shorrab AA S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30122] [Article Influence: 6024.4] [Reference Citation Analysis (3)] |
| 2. | Chen J, Liu L, Su S, Fu WG, Lei SJ, Zheng SL. Meta analysis of the effect of accelerated rehabilitation nursing on the rebatilitation of patients undergoing pancreaticoduodenectomy. Hushi Jinxiu Zazhi. 2019;34:685-689. |
| 3. | World Health Organization. Coronavirus disease (COVID-19). Situation Report - 111. May 10, 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200510covid-19-sitrep-111.pdf?sfvrsn=1896976f_2. Accessed May 11, 2020. |
| 4. | Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18987] [Cited by in RCA: 17647] [Article Influence: 3529.4] [Reference Citation Analysis (0)] |
| 5. | Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 based on current evidence. J Med Virol. 2020;92:548-551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 514] [Cited by in RCA: 559] [Article Influence: 111.8] [Reference Citation Analysis (0)] |
| 6. | Phan LT, Nguyen TV, Luong QC, Nguyen TV, Nguyen HT, Le HQ, Nguyen TT, Cao TM, Pham QD. Importation and Human-to-Human Transmission of a Novel Coronavirus in Vietnam. N Engl J Med. 2020;382:872-874. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 758] [Cited by in RCA: 695] [Article Influence: 139.0] [Reference Citation Analysis (0)] |
| 7. | General Office of the National Health Commission of the People’s Republic of China. Diagnosis and treatment plan of novel coronavirus pneumonia (Trial version 7). Issued 2020-03-03. |
| 8. | Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14113] [Cited by in RCA: 14767] [Article Influence: 2953.4] [Reference Citation Analysis (0)] |
| 9. | Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32-E40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3614] [Cited by in RCA: 3285] [Article Influence: 657.0] [Reference Citation Analysis (0)] |
| 10. | Zhu J, Zhong Z, Li H, Ji P, Pang J, Li B, Zhang J. CT imaging features of 4121 patients with COVID-19: A meta-analysis. J Med Virol. 2020;92:891-902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 11. | Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol. 2020;215:87-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 769] [Cited by in RCA: 860] [Article Influence: 172.0] [Reference Citation Analysis (0)] |
| 12. | Wahidi MM, Lamb C, Murgu S, Musani A, Shojaee S, Sachdeva A, Maldonado F, Mahmood K, Kinsey M, Sethi S, Mahajan A, Majid A, Keyes C, Alraiyes AH, Sung A, Hsia D, Eapen G. American Association for Bronchology and Interventional Pulmonology (AABIP) Statement on the Use of Bronchoscopy and Respiratory Specimen Collection in Patients With Suspected or Confirmed COVID-19 Infection. J Bronchology Interv Pulmonol. 2020;27:e52-e54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 163] [Article Influence: 32.6] [Reference Citation Analysis (0)] |
| 13. | Wahidi MM, Shojaee S, Lamb CR, Ost D, Maldonado F, Eapen G, Caroff DA, Stevens MP, Ouellette DR, Lilly C, Gardner DD, Glisinski K, Pennington K, Alalawi R. The Use of Bronchoscopy During the Coronavirus Disease 2019 Pandemic: CHEST/AABIP Guideline and Expert Panel Report. Chest. 2020;158:1268-1281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 138] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 14. | Peng YD, Meng K, Guan HQ, Leng L, Zhu RR, Wang BY, He MA, Cheng LX, Huang K, Zeng QT. [Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV]. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:450-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 221] [Reference Citation Analysis (0)] |
| 15. | British Thoracic Society Bronchoscopy Guidelines Committee, a Subcommittee of Standards of Care Committee of British Thoracic Society. British Thoracic Society guidelines on diagnostic flexible bronchoscopy. Thorax. 2001;56 Suppl 1:i1-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 151] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 16. | Liu Q, Wang RS, Gu GQ. General anatomy report of novel coronavirus pneumonia death corpse. Fayixue Zazhi. 2020;36:1-3. |
| 17. | Feng B, Chen ZX, Jin LW, Zheng ZH. Feng QX. Concerns about the Pharmacotherapeutics of COVID-19 Based on the Essence of "Sputum Emboli". Jinri Yaoxue. 2020;04:220-224. |
| 18. | Koenig SM, Truwit JD. Ventilator-associated pneumonia: diagnosis, treatment, and prevention. Clin Microbiol Rev. 2006;19:637-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 285] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 19. | Guidry CA, Mallicote MU, Petroze RT, Hranjec T, Rosenberger LH, Davies SW, Sawyer RG. Influence of bronchoscopy on the diagnosis of and outcomes from ventilator-associated pneumonia. Surg Infect (Larchmt). 2014;15:527-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Han Q, Chen C, Hu HQ, Shen J, Yang G, Chen B, Xia L. Effect evaluation on use of bedside fiber bronchoscope in treating stroke-associated pneumonia. Top Stroke Rehabil. 2018;25:459-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Group of Interventional Respiratory Medicine, Chinese Thoracic Society. [Expert consensus for bronchoscopy during the epidemic of 2019 Novel Coronavirus infection (Trial version)]. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:E006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 22. | Darwiche K, Ross B, Gesierich W, Petermann C, Huebner RH, Grah C, Gompelmann D, Hetzel J, Holland A, Eisenmann S, Stanzel F, Kempa A, Conrad K, Eberhardt R. [Recommendations for Performing Bronchoscopy in Times of the COVID-19 Pandemic]. Pneumologie. 2020;74:260-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Cordovilla R, Álvarez S, Llanos L, Nuñez Ares A, Cases Viedma E, Díaz-Pérez D, Flandes J. SEPAR and AEER consensus recommendations on the Use of Bronchoscopy and Airway Sampling in Patients with Suspected or Confirmed COVID-19 Infection. Arch Bronconeumol. 2020;56 Suppl 2:19-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 24. | Lentz RJ, Colt H. Summarizing societal guidelines regarding bronchoscopy during the COVID-19 pandemic. Respirology. 2020;25:574-577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 25. | Luo F, Darwiche K, Singh S, Torrego A, Steinfort DP, Gasparini S, Liu D, Zhang W, Fernandez-Bussy S, Herth FJF, Shah PL. Performing Bronchoscopy in Times of the COVID-19 Pandemic: Practice Statement from an International Expert Panel. Respiration. 2020;99:417-422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |