Published online Feb 16, 2021. doi: 10.12998/wjcc.v9.i5.1048
Peer-review started: July 24, 2020
First decision: September 14, 2020
Revised: October 1, 2020
Accepted: January 6, 2021
Article in press: January 6, 2021
Published online: February 16, 2021
Processing time: 189 Days and 15.7 Hours
Gastrointestinal bleeding (GIB) is a major concern in patients hospitalized with acute coronary syndrome (ACS) due to the common use of both antiplatelet medications and anticoagulants. Studies evaluating the safety of gastrointestinal endoscopy (GIE) in ACS patients with GIB are limited by their relatively small size, and the focus has generally been on upper GIB and esophago-gastroduod-enoscopy (EGD) only.
To evaluate the safety profile and the hospitalization outcomes of undergoing GIE in patients with ACS and concomitant GIB using the national database for hospitalized patients in the United States.
The Nationwide Inpatient Sample database was queried to identify patients hospitalized with ACS and GIB during the same admission between 2005 and 2014. The International Classification of Diseases Code, 9th Revision Clinical Modification was utilized for patient identification. Patients were further classified into two groups based on undergoing endoscopic procedures (EGD, small intestinal endoscopy, colonoscopy, or flexible sigmoidoscopy). Both groups were compared regarding demographic information, outcomes, and comorbi-dities. Multivariate analysis was conducted to identify factors associated with mortality and prolonged length of stay. Chi-square test was used to compare categorical variables, while Student’s t-test was used to compare continuous variables. All analyses were performed using SAS 9.4 (Cary, NC, United States).
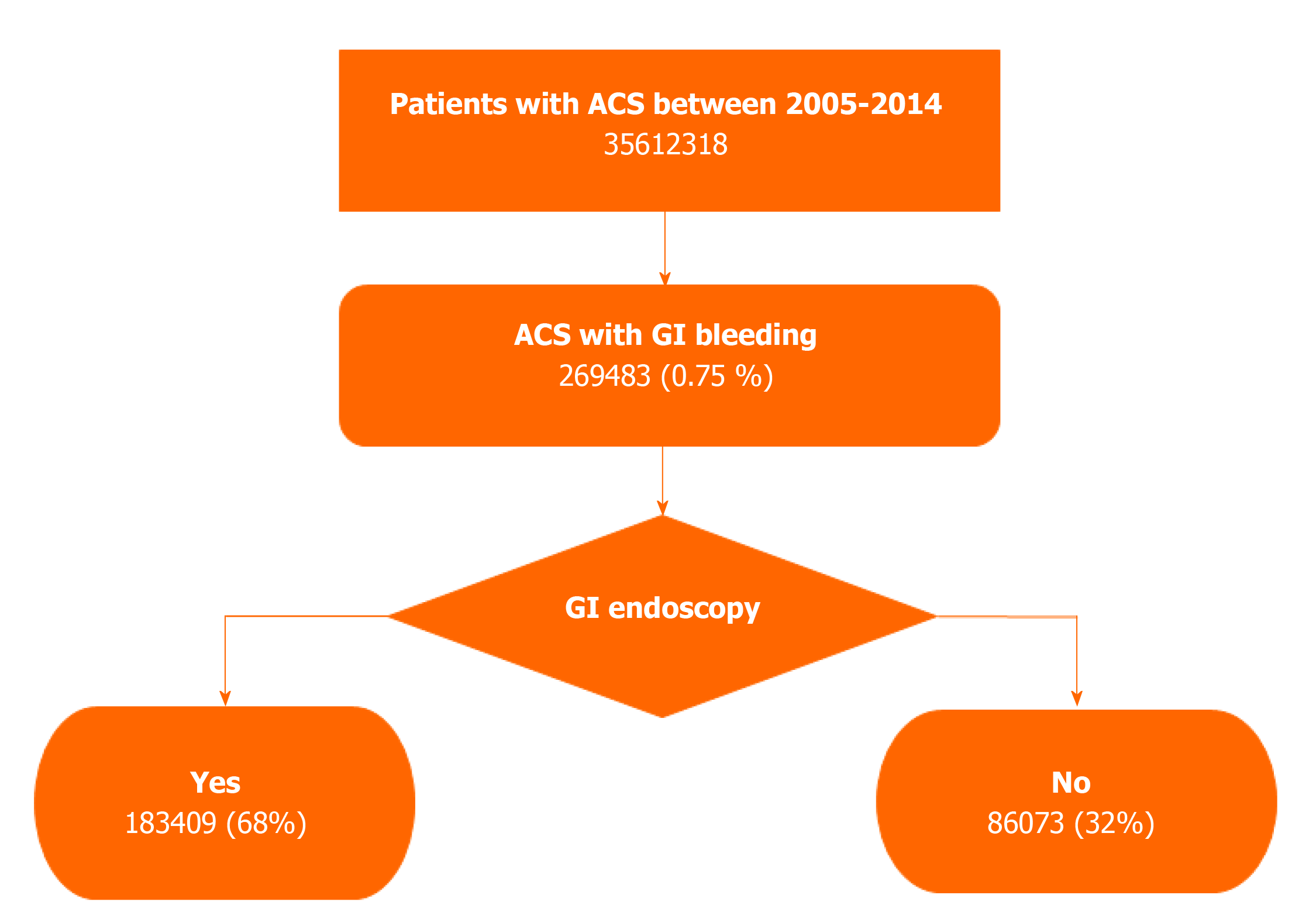
A total of 35612318 patients with ACS were identified between January 2005 and December 2014. 269483 (0.75%) of the patients diagnosed with ACS developed concomitant GIB during the same admission. At least one endoscopic procedure was performed in 68% of the patients admitted with both ACS and GIB. Patients who underwent GIE during the index hospitalization with ACS and GIB had lower mortality (3.8%) compared to the group not undergoing endoscopy (8.6 %, P < 0.001). A shorter length of stay (LOS) was observed in patients who underwent GIE (mean 6.59 ± 7.81 d) compared to the group not undergoing endoscopy (mean 7.84 ± 9.73 d, P < 0.001). Multivariate analysis showed that performing GIE was associated with lower mortality (odds ratio: 0.58, P < 0.001) and shorter LOS (-0.36 factor, P < 0.001).
Performing GIE during the index hospitalization of patients with ACS and GIB was correlated with a better mortality rate and a shorter LOS. Approximately two-thirds of patients with both ACS and GIB undergo GIE during the same hospitalization.
Core Tip: Less than 1% of hospitalized patients have concomitant acute coronary syndrome (ACS) and gastrointestinal bleeding (GIB). However, the combination of these two conditions is reported to be associated with increased morbidity and mortality. Studies evaluating the safety and hospitalization outcomes of gastrointestinal endoscopy (GIE) in patients with ACS and GIB are limited and conflicting. This analysis was designed to evaluate GIE safety and efficacy in patients with ACS and GIB. This study concluded that GIE in patients hospitalized with ACS and GIB is both safe and associated with lower mortality as well as a shorter hospital stay.
- Citation: Elkafrawy AA, Ahmed M, Alomari M, Elkaryoni A, Kennedy KF, Clarkston WK, Campbell DR. Safety of gastrointestinal endoscopy in patients with acute coronary syndrome and concomitant gastrointestinal bleeding. World J Clin Cases 2021; 9(5): 1048-1057
- URL: https://www.wjgnet.com/2307-8960/full/v9/i5/1048.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i5.1048
Gastrointestinal bleeding (GIB) is associated with increased morbidity and mortality[1]. The annual incidence of upper GIB in the United States is estimated to be 65 per 100000 individuals[2], and between 0.7% and 3% of patients with acute coronary syndrome (ACS) develop GIB[3-6]. GIB in patients with ACS is associated with a higher 30-d mortality rate (9.6%) as compared to ACS patients without GIB (1.4%)[3]. Studies evaluating the safety of gastrointestinal endoscopy (GIE) in ACS patients with GIB are limited by their relatively small size, and the focus has generally been on upper GIB and esophagogastroduodenoscopy (EGD) only. The current study aims to evaluate the safety and outcomes of undergoing GIE (EGD, enteroscopy, colonoscopy, or flexible sigmoidoscopy) in patients with concomitant ACS and acute GIB (upper and lower GIB) using the Nationwide Inpatient Sample (NIS) database.
In patients with GIB, it may be difficult to determine whether the source is in the upper or lower GI tract. Emergent EGD is frequently the initial diagnostic study used to evaluate patients with GIB[7]. However, its safety and utility, in the setting of ACS, present a common management dilemma[8]. Patients with ACS are at a higher risk of arrhythmias, heart failure, further ischemic events, and death. The stress of undergoing endoscopic procedures with procedural sedation can theoretically precipitate cardiac complications and increase procedural risk[9-12].
Antiplatelet therapy, dual antiplatelet therapy, anticoagulation therapy, and mechanical revascularization are well-established treatment modalities for ACS. However, these strategies are associated with an increased risk of precipitating gastrointestinal hemorrhage[13,14]. These therapies, especially when used together or when used in patients with comorbidities (e.g., prior peptic ulcer disease, renal failure, etc.) may precipitate GIB[15,16].
Endoscopic studies of the upper and/or lower GI tract are frequently required to: (1) Identify the anatomic site of bleeding; (2) Identify the lesion; and (3) Intervene to control bleeding[17].
The dilemma endoscopists often face is determining how safe an endoscopic procedure is in a patient with ACS. The current study was designed to evaluate on a large scale the safety and outcomes associated with the performance of endoscopic procedures during the same hospitalization with ACS and concomitant GIB.
Patients older than 18 years of age with the diagnosis of ACS and GIB (upper and/or lower GIB) during the same index admission were included in the study. ACS was defined as acute myocardial infarction, subendocardial infarction, and acute coronary occlusion without infarction. Patients with chronic ischemic heart disease without an ACS associated diagnosis, peptic ulcer without hemorrhage, acute duodenal ulcer without hemorrhage, gastric ulcer without hemorrhage, and esophageal varices without bleeding were excluded.
The study population was identified from the Healthcare Cost and Utilization Project databases (HCUP). The Agency for Healthcare Research and Quality sponsors the HCUP databases. The NIS database is the largest HCUP database, and it contains unweighted data from over seven million hospital admission each year. The data represent a 20% random sample of participating hospital discharges from 46 states. The NIS database is de-identified and available to the public. Thus, it is not considered human subject research and is exempted from review by the institutional review board. To assure a meaningful study cohort, the investigators agreed upon a minimum study cohort of 250000 admissions. International Classification of Diseases (ICD)-9 codes were transitioned to ICD-10 codes in the last quarter of 2015. To assure consistency and data integrity, the study was designed only to include ICD-9 codes. Therefore, the study population and variables of interest (Table 1) between January 2005 and December 2014 were evaluated as in subsequent years, ICD-10 codes were used to populate the NIS database.
| Total (n = 269483) | Patients underwent endoscopy | Patients without endoscopy | P value | |
| Mean age at admission | 72.32 ± 11.72 | 72.82 ± 11.41 | 71.27 ± 12.29 | < 0.001 |
| Males | 178111 (66.1) | 120040 (65.4) | 58070 (67.5) | < 0.001 |
| Females | 91372 (33.9) | 63369 (34.6) | 28003 (32.5) | |
| Race | < 0.001 | |||
| Caucasian | 185713 (79.1) | 127623 (79.5) | 58089 (78.1) | |
| African American | 17453 (7.4) | 11555 (7.2) | 5898 (7.9) | |
| Hispanic | 16362 (7.0) | 10710 (6.7) | 5652 (7.6) | |
| Other | 15338 (6.5) | 10639 (6.6) | 5652 (7.6) | |
| Mortality | 14448 (5.4) | 7027 (3.8) | 7421 (8.6) | < 0.001 |
| Length of stay | 6.99 ± 8.49 | 6.59 ± 7.81 | 7.84 ± 9.73 | < 0.001 |
| Primary expected payer | < 0.001 | |||
| Medicare | 198925 (73.9) | 137580 (75.1) | 61344 (71.4) | |
| Medicaid | 12590 (4.7) | 7864 (4.3) | 4726 (5.5) | |
| Private | 45991 (17.1) | 30558 (16.7) | 15433 (18.0) | |
| Self-pay | 6407 (2.4) | 3900 (2.1) | 2507 (2.9) | |
| No charge | 578 (0.2) | 318 (0.2) | 261 (0.3) | |
| Other | 4642 (1.7) | 2971 (1.6) | 1672 (1.9) | |
| Location/teaching status of hospital | < 0.001 | |||
| Rural | 26040 (9.7) | 19100 (10.5) | 6939 (8.1) | |
| Urban nonteaching | 119321 (44.5) | 82796 (45.4) | 6939 (8.1) | |
| Urban teaching | 122779 (45.8) | 80650 (44.2) | 42129 (49.2) | |
| Region of hospital | 0.022 | |||
| Northeast | 49463 (18.4) | 34252 (18.7) | 15212 (17.7) | |
| Midwest | 64974 (24.1) | 44079 (24.0) | 20895 (24.3) | |
| South | 100860 (37.4) | 68653 (37.4) | 20895 (24.3) | |
| West | 100860 (37.4) | 68653 (37.4) | 17759 (20.6) | |
| Shock | 24171 (9) | 13172 (7.2) | 10999 (12.8) | < 0.001 |
| Mechanical ventilation | 24705 (9.2) | 12736 (9.2) | 11969 (13.9) | < 0.001 |
| Blood transfusion | 145939 (54.2) | 102484 (55.9) | 43455 (50.5) | < 0.001 |
Patients undergoing single or multiple endoscopic procedures (esophago-gastro-duodenoscopy, small intestinal endoscopy, colonoscopy, or flexible sigmoidoscopy) were compared to those not undergoing endoscopic procedures in the same hospital encounter. Demographic data, including age, gender, race, payer status, geographic region, hospital size, and academic affiliation were evaluated. Mortality, length of stay (LOS), blood transfusion requirement, shock, mechanical ventilation, and commonly associated comorbidities were compared between both groups. Commonly associated comorbidities obtained from the NIS database were defined by the Agency for Healthcare Research and Quality and included thirty categories of comorbidity[18] (Supplementary Table 1). Analyses of mortality and LOS in ACS patients with GIB were further adjusted for comorbidities. All ICD-9 CM and ICD-9 PCS codes are detailed in Appendix-1, Supplementary material.
Continuous variables were described using mean ± SD, while categorical variables were described using proportion (percentage). Chi-square test was used to compare categorical variables, while Student’s t-test was used to compare continuous variables. Multivariate analysis was done using logistic regression models to decrease bias and adjust for possible confounding factors. Statistical analysis was performed by a biomedical statistician. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, United States).
A total of 35612318 patients with ACS were identified between January 2005 and December 2014, and 269483 (0.75%) of the patients with ACS developed GIB during the same index admission. At least one GIE procedure was performed in 183248 (68%) patients with concomitant GIB and ACS, and outcomes in these patients were compared to the 86235 patients who did not undergo any endoscopic procedures (Figure 1). Males comprised 66.1% of the study population, while females comprised 33.9%. The mean age of the study population was 72.3 years, 79.1% were Caucasian, 7.4% African American, and 7.0% were Hispanic.
In the study cohort, undergoing GIE procedure was associated with reduced mortality (3.8%) in comparison to (8.6 %) in the group not having an endoscopic procedure (95%CI: -5.2, -4.4), (P < 0.001). Hospital length of stay (LOS) was shorter in patients who underwent gastrointestinal endoscopic procedures (mean 6.59 ± 7.81 d) in comparison to the group who did not undergo endoscopy (mean 7.84 ± 9.73 d) (95%CI: -1.42, -1.10), (P < 0.001). Shock was present in 7.2% of patients undergoing GIE compared to 12.8% in patients not undergoing endoscopy (95%CI: -6.1, -5.1), (P < 0.001) while 6.9% of patients were mechanically ventilated from the first group as compared to 13.9% in the group not undergoing endoscopy (95%CI: -7.5, -6.5), (P < 0.001). 55.9 % of patients who underwent GIE received blood transfusions in comparison to 50.5% of patients not undergoing endoscopic procedures (95%CI: 4.5, 6.3) (P < 0.001). Refer to Table 1 for comparison between both groups. Other compared comorbidities are detailed in Supplementary Table 1.
Multivariate logistic regression models were used to predict factors associated with increased mortality and LOS. GIE was associated with less mortality; odds ratio (OR) of 0.58 (95%CI: 0.53-0.63) (P < 0.0001). Coagulopathy, shock, and mechanical ventilation were associated with higher mortality, OR of 1.76, 3.03, and 9.16, respectively (P < 0.0001). Regarding LOS, performing endoscopy was associated with a shorter LOS by -0.36 factor (beta weight) (95%CI: -0.56, -0.16) (P < 0.001). Congestive heart failure, shock, and mechanical ventilation were associated with prolonged LOS by 1.57, 3.16, 8.48 factor, respectively (beta weight). Refer to Tables 2 and 3 for all variables included in the logistic regression models.
| Odds ratio, 95%CI | P value | |
| GIE | 0.58 (0.53, 0.63) | < 0.0001 |
| Age | 1.03 (1.03, 1.03) | < 0.0001 |
| Female | 0.99 (0.9, 1.08) | 0.7729 |
| Race (Caucasian) | 0.9 (0.83, 0.99) | 0.0225 |
| DM | 0.71 (0.64, 0.79) | < 0.0001 |
| CHF | 1.13 (1.02, 1.26) | 0.0186 |
| Coagulopathy | 1.76 (1.57, 1.98) | < 0.0001 |
| Anemia | 0.85 (0.76, 0.96) | 0.0069 |
| Liver disease | 1.75 (1.51, 2.02) | < 0.0001 |
| Renal failure | 1.32 (1.2, 1.44) | < 0.0001 |
| Diagnosis of cancer | 1.76 (1.41, 2.19) | < 0.0001 |
| Shock | 3.03 (2.72, 3.38) | < 0.0001 |
| Mechanical ventilation | 9.16 (8.33, 10.07) | < 0.0001 |
| Blood transfusion | 0.9 (0.82, 0.99) | 0.0314 |
| Tobacco smoking | 0.71 (0.63, 0.8) | < 0.0001 |
| Alcohol abuse | 1.19 (1.01, 1.41) | 0.0400 |
| Label | Beta weight, 95%CI for LOS | P value |
| GIE | -0.36 (-0.56, -0.16) | < 0.001 |
| Age | -0.01 (-0.02, 0) | 0.0059 |
| Sex (female) | 0.34 (0.2, 0.48) | < 0.0001 |
| Race (Caucasian) | -0.47 (-0.62, -0.32) | < 0.0001 |
| DM | -0.8 (-0.95, -0.66) | < 0.0001 |
| CHF | 1.57 (1.35, 1.8) | < 0.0001 |
| Coagulopathy | 1.39 (1.04, 1.74) | < 0.0001 |
| Anemia | 0.07 (-0.11, 0.26) | 0.4333 |
| Liver disease | 0.28 (-0.05, 0.61) | 0.0945 |
| Renal failure | 1.41 (1.24, 1.59) | < 0.0001 |
| Diagnosis of cancer | 0.56 (0.08, 1.04) | 0.0228 |
| Shock | 3.16 (2.73, 3.59) | < 0.0001 |
| Mechanical ventilation | 8.48 (7.96, 9) | < 0.0001 |
| Blood transfusion | -0.69 (-0.9, -0.49) | < 0.0001 |
| Tobacco smoking | -1.58 (-1.77, -1.38) | < 0.0001 |
| Alcohol abuse | -0.77 (-1.08, -0.47) | < 0.0001 |
Similar to previous studies, the results of this analysis found that 0.75% of patients admitted during a ten-year period with ACS develop GIB. Previous studies estimated the prevalence of GIB in ACS patients between 0.7% and 3%[3-5]. Performing GIE (EGD, small intestinal endoscopy, colonoscopy, or flexible sigmoidoscopy) in patients with ACS and GIB was associated with significantly lower mortality and a shorter hospitalization stay in comparison to the group not undergoing endoscopic procedure. The selection of endoscopic procedures depended on the clinical impression of the gastroenterologist. Since patients with hematochezia may be experiencing brisk upper GIB or lower GI hemorrhage, some patients required evaluation with more than one endoscopic procedure. For that reason, all types of endoscopic procedures commonly used in the management of GIB were included in this study without stratification. One of the challenges in this study was to determine whether the patients who did not undergo GIE were at excessive risk for an endoscopic procedure or whether they developed complications (shock, respiratory failure, etc.) as a result of not having had an endoscopic procedure performed. A temporal relationship between performing endoscopy, presence of shock, mechanical ventilation, and other comorbid confounding factors could not be evaluated in this database. However, the association between performing GIE and better outcomes was statistically significant in the logistic regression models in the presence of these comorbidities.
GIB complicating ACS is a complex clinical scenario with sparse data to direct evidence-based guidelines on proper management. A recent study reported that the use of antiplatelet therapy, malignancy, renal impairment, heart failure, previous peptic ulcer disease, and abnormal activated partial thromboplastin time were predictors of GIB following ACS[19]. Pioppo et al[20] concluded that non-variceal upper GIB in hospitalized patients with ACS was correlated with higher mortality, a longer length of stay, and increased hospitalization charges. Several studies have evaluated the safety of upper endoscopy shortly after ACS (usually within 30 d) and concluded it could be safely performed[21-24]. The current study assessed the safety of endoscopic procedures during the same admission as ACS, and those admissions averaged approximately eight days. Al-Ebrahim et al[25] reported complications occurred in 25% of patients undergoing endoscopy. However, mortality was not reported in that study, and only a small number of patients met the inclusion criteria. Lim et al[21] evaluated major and minor complications following performing EGD within 30 d of ACS. They found no major complication, while minor complications occurred in 31% of the patients.
Another study concluded that undergoing upper GIE before cardiac catheterization was associated with a lower death rate when done for overt upper GIB[24]. Addition-ally, Modi et al[26] found that colonoscopy performed in the same admission for patients with STEMI and concomitant GIB was associated with lower mortality as compared with no intervention.
A meta-analysis by Cena et al[27] evaluated the safety and benefits of performing GIE after myocardial infarction. It demonstrated that endoscopic procedures are safe and beneficial in stable patients with GIB after recent MI and should be performed without delay. A more recent meta-analysis found higher rates of cardiac complications following endoscopy in ACS patients[28]. However, that study included endoscopic retrograde cholangiopancreatography and endoscopic ultrasound, which may have increased the rates of complications.
Several predictors of GIB in patients with ACS have been identified, including; older age, diabetes, hypertension, previous peptic ulcer disease, and dual antiplatelet therapy[3,5,29]. In the study reported herein, the presence of coagulopathy, chronic heart failure, liver disease, renal failure, shock, and mechanical ventilation are associated with increased mortality.
A recently published study concluded that performing endoscopy in ACS patients was associated with better outcomes. However, it was not limited to the patients with GI hemorrhage and included other indications for performing endoscopy[30]. The current analysis highlights the safety and superior outcomes of undergoing gastrointestinal endoscopic procedures in the specific setting of ACS and GIB.
Like all retrospective database studies, the usual concerns apply (selection bias, confounding, reliability of data, etc.). The diagnoses of diseases, comorbidities, outcomes, and procedures were identified using ICD-9 CM and ICD-9 PCS codes. Coding accuracy and missing data are potential sources of bias. The inability to review the individual medical records to validate the data may have led to inaccuracies. The temporal relationship between the performance of endoscopic procedures and confounding comorbidities could not be evaluated. However, the logistic regression models allowed for evaluation for comorbidities and minimization of possible confounding factors. Despite these limitations, the large sample size (269483 patients with concomitant ACS and GIB), wide geographic representation, variable size, and type of hospital (community vs. academic) enhance the generalizability of the findings.
This large retrospective analysis found that over a ten year period, 0.75% of patients admitted with ACS developed significant GIB. An endoscopic procedure was performed during the same hospitalization in the majority of the 269483 patients experiencing ACS and gastrointestinal hemorrhage. Patients with ACS who underwent GIE had lower mortality (3.8%) compared to patients who did not undergo endoscopic procedures (8.6%). Undergoing GIE in these patients during the same hospitalization was not only safe but was also correlated to lower mortality and a shorter hospital stay. The study confirms GIE can be safely performed in the majority of patients with ACS and concomitant GIB. The analysis highlights the need for future prospective controlled studies to determine the optimal time for intervention in patients with concomitant ACS and GIB and whether different modalities of endoscopy are equally safe. However, it’s unlikely such a study will ever be completed given the requisite enrollment numbers combined with current and other studies demonstrating the safety and superior outcomes with the same hospitalization endoscopy.
Gastrointestinal bleeding (GIB) in patients with acute coronary syndrome (ACS) is reported to be associated with increased morbidity and mortality.
Large scale studies investigating the safety profile and hospitalization outcomes of undergoing gastrointestinal endoscopic (GIE) procedure in hospitalized patients with ACS and GIB are limited and conflicting.
This large scale study assesses the safety and utility of performing GIE in hospitalized patients with concomitant ACS and GIB.
The Nationwide Inpatient Sample database was queried to identify patients hospitalized with ACS and GIB during the same admission between 2005 and 2014 using ICD-9 codes. The study cohort was further categorized into two groups based on undergoing GIE. Outcomes of interest were compared between both groups. Multivariate analysis was conducted to predict factors associated with increased mortality and prolonged length of stay.
Patients with both ACS and GIB during the same admission who underwent GIE had a lower mortality rate (3.8%) in comparison to the group without endoscopy (8.6 %). Patients who underwent GIE had a shorter hospital stay (mean 6.59 ± 7.81 d) contrasted to those not undergoing endoscopic procedure (mean 7.84 ± 9.73 d). Multivariate regression analysis showed that undergoing GIE in this cohort was an independent predictor of lower mortality and shorter hospital stay.
Undergoing GIE in patients presenting with ACS and GIB during the same index admission was associated with lower mortality as well as a shorter hospital stay.
Future prospective studies are needed to evaluate the optimal time for intervention in patients with concomitant ACS and GIB and whether different modalities of endoscopy and endoscopic interventions are equally safe.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: American Association for the Study of Liver Diseases, No. 239694; and American College of Gastroenterology, No. 51583.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen YD, Guo JS, Ju SQ, Karayiannakis AJ, Wang K S-Editor: Zhang H L-Editor: A P-Editor: Xing YX
| 1. | Kim JS, Kim BW, Kim DH, Park CH, Lee H, Joo MK, Jung DH, Chung JW, Choi HS, Baik GH, Lee JH, Song KY, Hur S. Guidelines for Nonvariceal Upper Gastrointestinal Bleeding. Gut Liver. 2020;14:560-570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Wuerth BA, Rockey DC. Changing Epidemiology of Upper Gastrointestinal Hemorrhage in the Last Decade: A Nationwide Analysis. Dig Dis Sci. 2018;63:1286-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 172] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 3. | Nikolsky E, Stone GW, Kirtane AJ, Dangas GD, Lansky AJ, McLaurin B, Lincoff AM, Feit F, Moses JW, Fahy M, Manoukian SV, White HD, Ohman EM, Bertrand ME, Cox DA, Mehran R. Gastrointestinal bleeding in patients with acute coronary syndromes: incidence, predictors, and clinical implications: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. J Am Coll Cardiol. 2009;54:1293-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 156] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 4. | Collins RT 2nd, Doshi P, Onukwube J, Fram RY, Robbins JM. Risk Factors for Increased Hospital Resource Utilization and In-Hospital Mortality in Adults With Single Ventricle Congenital Heart Disease. Am J Cardiol. 2016;118:453-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Al-Mallah M, Bazari RN, Jankowski M, Hudson MP. Predictors and outcomes associated with gastrointestinal bleeding in patients with acute coronary syndromes. J Thromb Thrombolysis. 2007;23:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Gaglia MA Jr, Torguson R, Gonzalez MA, Ben-Dor I, Maluenda G, Collins SD, Syed AI, Delhaye C, Wakabayashi K, Belle L, Mahmoudi M, Hanna N, Xue Z, Kaneshige K, Suddath WO, Kent KM, Satler LF, Pichard AD, Waksman R. Correlates and consequences of gastrointestinal bleeding complicating percutaneous coronary intervention. Am J Cardiol. 2010;106:1069-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Cader MZ, Di Pietro M. Acute Upper GIB: Good Night, Sleep Tight, Endoscopy Can Wait until Morning Light. Gastroenterology. 2020;159:1990-1991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Mehran R, Pocock S, Nikolsky E, Dangas GD, Clayton T, Claessen BE, Caixeta A, Feit F, Manoukian SV, White H, Bertrand M, Ohman EM, Parise H, Lansky AJ, Lincoff AM, Stone GW. Impact of bleeding on mortality after percutaneous coronary intervention results from a patient-level pooled analysis of the REPLACE-2 (randomized evaluation of PCI linking angiomax to reduced clinical events), ACUITY (acute catheterization and urgent intervention triage strategy), and HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trials. JACC Cardiovasc Interv. 2011;4:654-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 315] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 9. | Gangi S, Saidi F, Patel K, Johnstone B, Jaeger J, Shine D. Cardiovascular complications after GIE: occurrence and risks in a large hospital system. Gastrointest Endosc. 2004;60:679-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Kounis NG, Zavras GM, Papadaki PJ, Kouni SN, Batsolaki M, Gouvelou-Deligianni GV, Markoglou C, Goudevenos JA, Mallioris CN, Kokkinis C, Kalokairinou K, Grapsas N, Kounis GN, Koutsojannis CM. Electrocardiographic changes in elderly patients during endoscopic retrograde cholangiopancreatography. Can J Gastroenterol. 2003;17:539-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | McAlpine JK, Martin BJ, Devine BL. Cardiac arrhythmias associated with upper gastrointestinal endoscopy in elderly subjects. Scott Med J. 1990;35:102-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Yazawa K, Adachi W, Koide N, Watanabe H, Koike S, Hanazaki K. Changes in cardiopulmonary parameters during upper gastrointestinal endoscopy in patients with heart disease: towards safer endoscopy. Endoscopy. 2000;32:287-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Huang KW, Luo JC, Leu HB, Huang CC, Hou MC, Chen TS, Lu CL, Lin HC, Lee FY, Chang FY. Risk factors for upper gastrointestinal bleeding in coronary artery disease patients receiving both aspirin and clopidogrel. J Chin Med Assoc. 2013;76:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Abraham NS, Yang EH, Noseworthy PA, Inselman J, Yao X, Herrin J, Sangaralingham LR, Ngufor C, Shah ND. Fewer gastrointestinal bleeds with ticagrelor and prasugrel compared with clopidogrel in patients with acute coronary syndrome following percutaneous coronary intervention. Aliment Pharmacol Ther. 2020;52:646-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Wallace MC, Rankin J, Forbes GM. Acute gastrointestinal bleeding after percutaneous coronary intervention. Expert Rev Gastroenterol Hepatol. 2012;6:211-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Abraham NS, Hlatky MA, Antman EM, Bhatt DL, Bjorkman DJ, Clark CB, Furberg CD, Johnson DA, Kahi CJ, Laine L, Mahaffey KW, Quigley EM, Scheiman J, Sperling LS, Tomaselli GF; ACCF/ACG/AHA. ACCF/ACG/AHA 2010 expert consensus document on the concomitant use of proton pump inhibitors and thienopyridines: a focused update of the ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. Am J Gastroenterol. 2010;105:2533-2549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 134] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 17. | Strate LL, Gralnek IM. ACG Clinical Guideline: Management of Patients With Acute Lower Gastrointestinal Bleeding. Am J Gastroenterol. 2016;111:755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 18. | Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6456] [Cited by in RCA: 7798] [Article Influence: 288.8] [Reference Citation Analysis (0)] |
| 19. | Zheng W, Zhang YJ, Liu R, Zhao XD, Ai H. Prediction of gastrointestinal bleeding events in patients with acute coronary syndrome undergoing percutaneous coronary intervention: An observational cohort study (STROBE compliant). Medicine (Baltimore). 2020;99:e21312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Pioppo L, Bhurwal A, Reja D, Tawadros A, Mutneja H, Goel A, Patel A. Incidence of Non-variceal Upper Gastrointestinal Bleeding Worsens Outcomes with Acute Coronary Syndrome: Result of a National Cohort. Dig Dis Sci. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Lim RG, Cobell WJ, Theivanayagam S, Kilgore TW, Matteson ML, Puli SR, Bechtold ML. Endoscopy after acute myocardial infarction: an evaluation of safety. South Med J. 2013;106:545-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Mumtaz K, Ismail FW, Jafri W, Abid S, Hamid S, Shah H, Dhakam S. Safety and utility of oesophago-gastro-duodenoscopy in acute myocardial infarction. Eur J Gastroenterol Hepatol. 2008;20:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Lin S, Konstance R, Jollis J, Fisher DA. The utility of upper endoscopy in patients with concomitant upper gastrointestinal bleeding and acute myocardial infarction. Dig Dis Sci. 2006;51:2377-2383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Yachimski P, Hur C. Upper endoscopy in patients with acute myocardial infarction and upper gastrointestinal bleeding: results of a decision analysis. Dig Dis Sci. 2009;54:701-711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Al-Ebrahim F, Khan KJ, Alhazzani W, Alnemer A, Alzahrani A, Marshall J, Armstrong D. Safety of esophagogastroduodenoscopy within 30 days of myocardial infarction: a retrospective cohort study from a Canadian tertiary centre. Can J Gastroenterol. 2012;26:151-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Modi RM, Li F, Mumtaz K, Hinton A, Lilly SM, Hussan H, Levine E, Zhang C, Conwell DL, Krishna SG, Stanich PP. Colonoscopy in Patients With Postmyocardial Infarction Gastrointestinal Bleeding: A Nationwide Analysis. J Clin Gastroenterol. 2019;53:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Cena M, Gomez J, Alyousef T, Trohman RG, Pierko K, Agarwal R. Safety of endoscopic procedures after acute myocardial infarction: a systematic review. Cardiol J. 2012;19:447-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Dorreen A, Moosavi S, Martel M, Barkun AN. Safety of Digestive Endoscopy following Acute Coronary Syndrome: A Systematic Review. Can J Gastroenterol Hepatol. 2016;2016:9564529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | Shalev A, Zahger D, Novack V, Etzion O, Shimony A, Gilutz H, Cafri C, Ilia R, Fich A. Incidence, predictors and outcome of upper gastrointestinal bleeding in patients with acute coronary syndromes. Int J Cardiol. 2012;157:386-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 30. | Hoffman GR, Stein DJ, Moore MB, Feuerstein JD. Safety of Endoscopy for Hospitalized Patients With Acute Myocardial Infarction: A National Analysis. Am J Gastroenterol. 2020;115:376-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |