Published online Feb 6, 2021. doi: 10.12998/wjcc.v9.i4.960
Peer-review started: October 26, 2020
First decision: November 20, 2020
Revised: December 2, 2020
Accepted: December 16, 2020
Article in press: December 16, 2020
Published online: February 6, 2021
Processing time: 90 Days and 20 Hours
In this case, platelet-rich fibrin (PRF) was added to guided tissue regeneration as a biomaterial in proper order for immediate planting in aesthetic area with periapical infection.
With the history of endodontic failure in maxillary central incisor, a 34-year-old female patient required the extraction of maxillary anterior residual root and immediate implantation. Cone beam computed tomography and clinical observation were used to assess the regeneration of soft and bone tissue. Before operation, cone beam computed tomography showed the anterior residual root had serious periapical periodontitis with insufficient labial bone in the aesthetic zone. The patient underwent immediate implant placement and reconstruction of the bone substitution by modified guided bone regeneration. The barrier was a three-layer structure of PRF-collagen membrane-PRF that covered the mixture of PRF and Bio-Oss to promote both osteogenesis and soft tissue healing. At 6 mo postoperatively, the definitive crown was placed after accomplished finial impression. One-year follow-up showed a satisfactory aesthetic effect with no obvious absorption of the labial bone and soft tissue.
The use of PRF in combination with guided bone regeneration can serve as a reliable and simple adjuvant for immediate implanting in infected socket and result in a stable osteogenic effect with good aesthetic outcome.
Core Tip: In spite of the high-risk of immediate implantation in infected areas, there is a unique advantage. In this case report, the process of tooth extraction, implant placement and platelet-rich fibrin have been combined in one appointment, which significantly shortened the course of treatment the patient required. Furthermore, the existence of the platelet-rich fibrin was adopted to alleviate the inflammatory reaction and promote tissue recovery.
- Citation: Fang J, Xin XR, Li W, Wang HC, Lv HX, Zhou YM. Immediate implant placement in combination with platelet rich-fibrin into extraction sites with periapical infection in the esthetic zone: A case report and review of literature. World J Clin Cases 2021; 9(4): 960-969
- URL: https://www.wjgnet.com/2307-8960/full/v9/i4/960.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i4.960
The predictability of immediate implant placements of anterior teeth has been significantly demonstrated. Immediate implants of single tooth usually result in preserving soft and hard tissue as well as shortening course of treatment and satisfying esthetics[1,2]. Recently, there is some controversy regarding placement of an immediate implant into extraction sites with periapical infection[3]. Traditionally, the lesion of periapical inflammation was forbidden to be replaced directly with intraosseous implants because of the increasing failure risk of osseointegration[4]. One of the main causes of implant failure is the contamination with bacteria during the initial healing period[5]. Research has shown that the failure rates of implants were significantly increased after immediate implanting with chronic periapical disease[6].
A further cause for concern, immediate implantation is often accompanied by tissue defects. Bone grafts and barrier membranes are usually necessary to correct the bone and soft defects surrounding the implants. In the immediate implant in aesthetic area, enough labial bone and soft tissue are the key factor to achieve stable and satisfactory results[2]. Moreover, one of the main challenges confronting the surgery of immediate implantation is wound closure with inadequate soft tissue, which may greatly affected the implants’ aesthetics of gingival formation in the aesthetic area[7]. Therefore, appropriate protocols in clinic are necessary to use for immediate implant placement at periapical infected sites.
Platelet-rich fibrin (PRF), a second-generation platelet concentrate, has played an important role in tissue regeneration. PRF is prepared from the patient’s own blood, which could reduce or eliminating the possible adverse reactions[8]. The three-dimensional mesh architecture of PRF could release the growth factors slowly and accelerate the healing of both soft and hard tissues[8,9]. The application of PRF could not only benefit the construction of osteogenic environment but also repair the regeneration of soft tissue in the treatment of immediate implant placement[10,11]. In addition, various kinds of leukocytes in PRF (especially granulocytes and lymphocytes) also present a noticeable impact on antimicrobial and immuno-modulatory effects, which could reduce the inflammatory response of wound healing and prevent the infected risk of chronic periodontitis[12-15].
In this case report, we demonstrate the clinical effectiveness of PRF for multiple procedures in immediate implantation with periapical infection in esthetic zone. The labial bone mass of patient’s anterior maxilla was defected, caused by chronic periapical periodontitis. The high aesthetic requirement and urgency time increased the difficulty of implant treatment. Immediate implantation in combination with PRF was adopted to alleviate the inflammatory reaction and promote the tissue recovery. During the surgery, PRF was added in proper sequence as an important biomaterial for both bone and soft tissue regeneration.
A 34-year-old, healthy female patient was consulted at the Department of Dental Implantology with the residual root of the right maxillary central incisor.
The patient suffered from the fracture in endodontic failure of the right maxillary central incisor (No. 11). The crown of right lateral incisor was fell off after root canal therapy.
The patient has no significant systemic complaint and medical history.
The patient has no personal and family history.
The physical examination was normal.
The hematology test was normal.
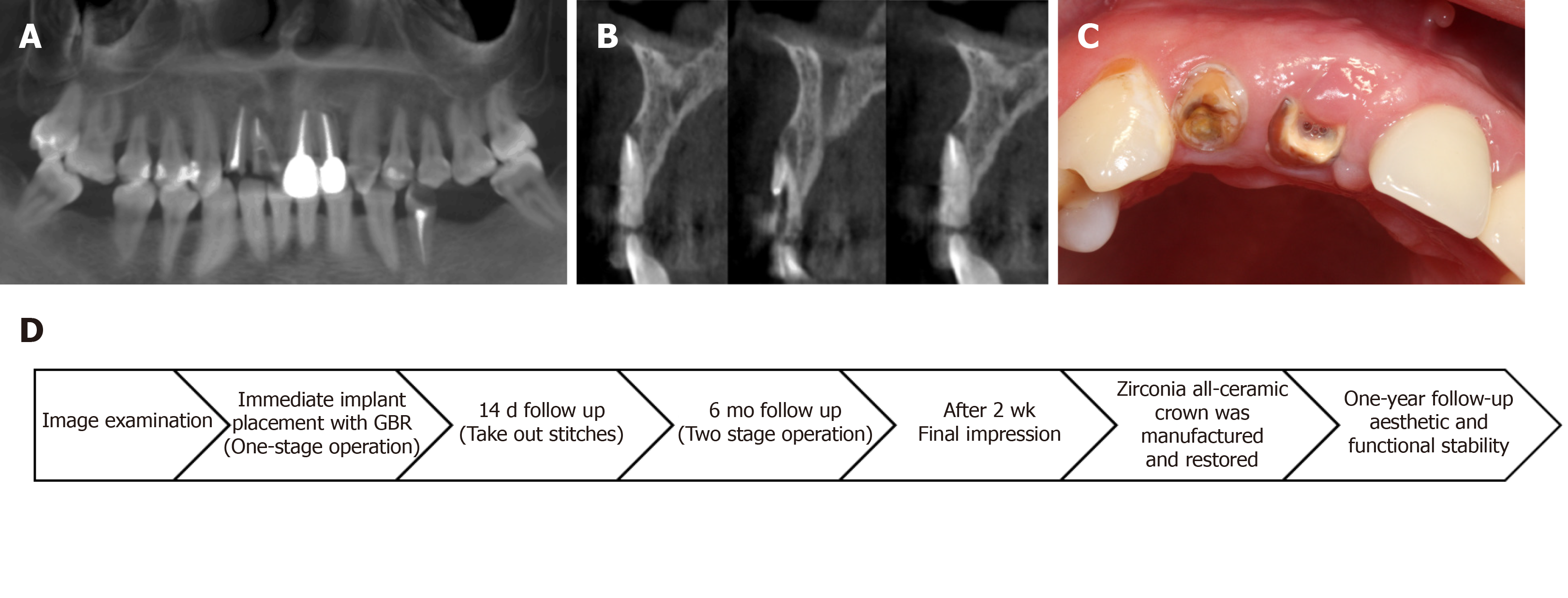
Cone beam computed tomography (CBCT) demonstrated that the root tip of No. 11 was filled with a low-density shadow, and the labial bone plate was deficient (Figure 1A). There was severe labial bone loss with a mean bone weight less than 3.5 mm (Figure 1B).
The right maxillary central incisor was root fracture with chronic inflammation. The keratinized gingival width of No. 11 was adequate. The patient’s gingival biotype was thick- and fan-shaped (Figure 1C).
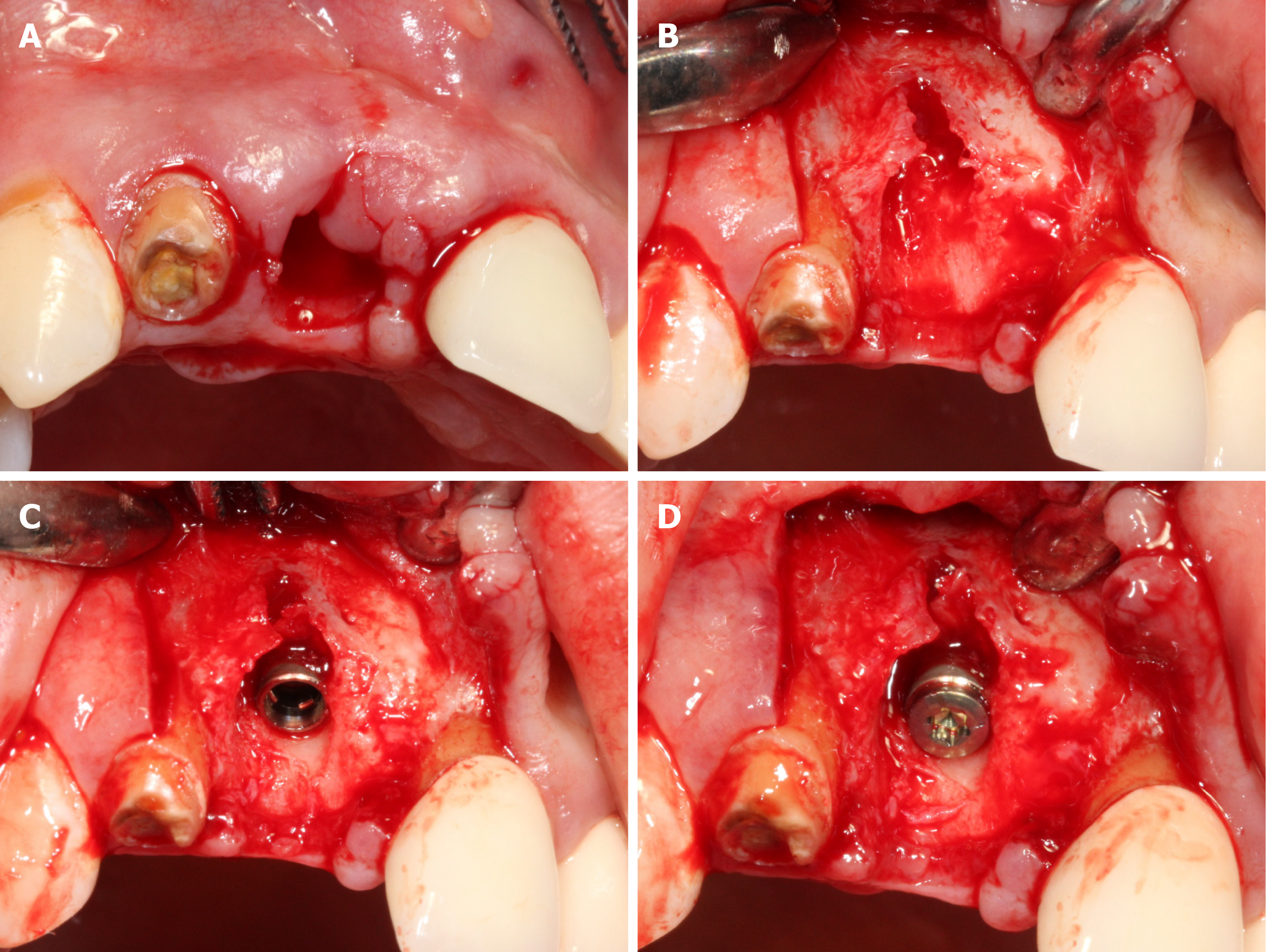
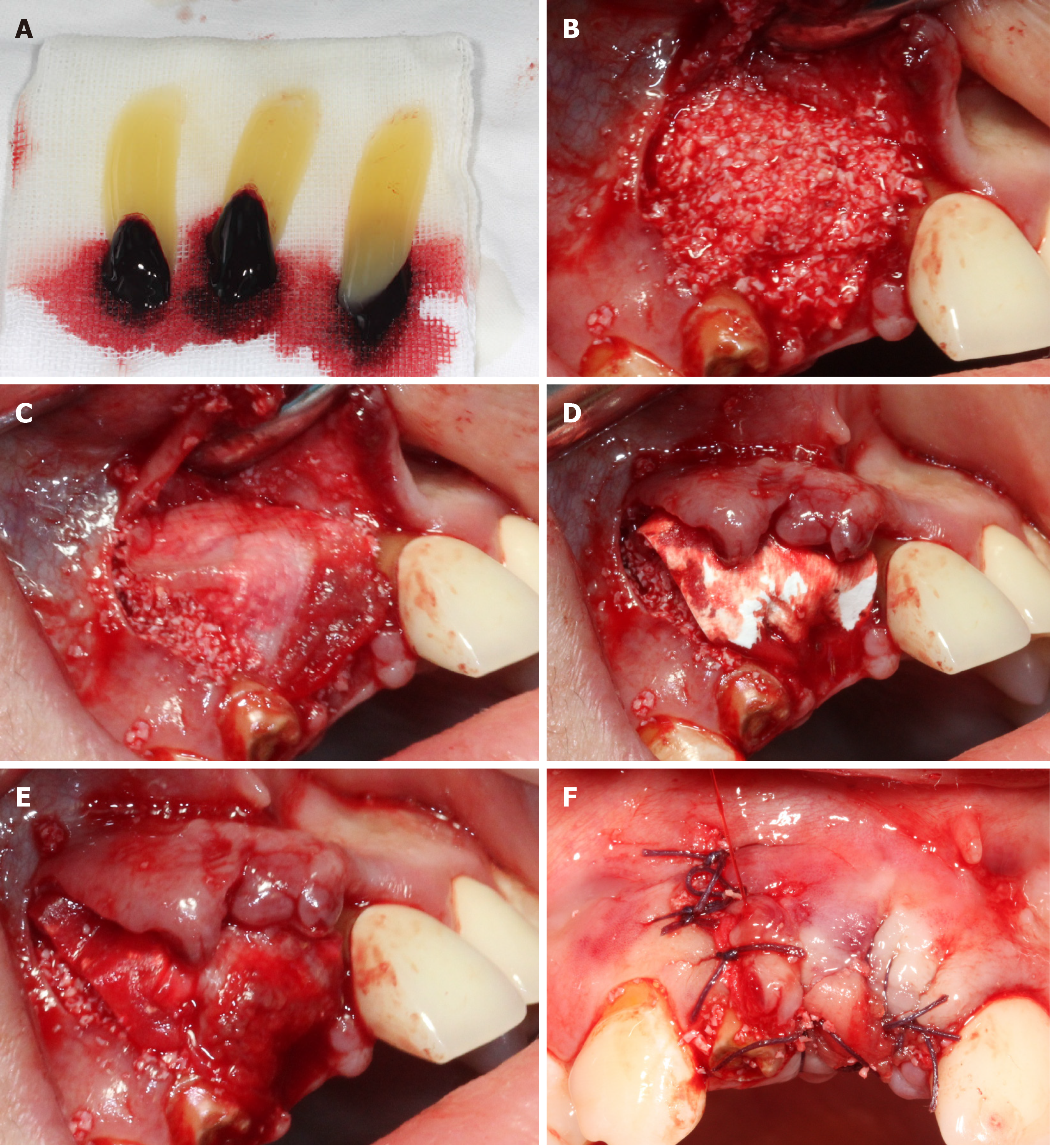
All relevant aspects of the operative risk and complications were communicated with the patient and a prophylactic dose of 1 g amoxicillin was taken orally before the surgery. After local anesthesia by Articaine Hydrochloride, minimally invasive extraction was used to replace the residual root of No. 11 (Figure 2A). The full thickness flap was elevated and the granulation tissue in the alveolar socket was debrided clearly. Severe loss of buccal bone was observed after proper irrigation (Figure 2B). A bone level implant (3.3 mm × 12 mm, SLA®, Straumann AG, Basel, Switzerland) was installed in the alveolar socket, following a healing screw placement (Figure 2C and D). Before the operation, PRF was extracted from whole blood and immediately centrifuged at the speed of 3000 rpm for 10 min (Figure 3A). One of the PRF clots was separated from the red blood clot and mixed with 0.25 g spongious bone substitute (Bio-Oss®, Geistlich AG, Wolhusen, Switzerland). The other PRFs were gently pressed into membranes using sterile gauze. The mixture was filled into the marginal gap between the buccal plate and implant. One piece of PRF membranes was used as barrier (Figure 3B and C) on the mixture. Then, a bioabsorbable collagen membrane (Bio-Gide®, Geistlich AG, Wolhusen, Switzerland) (Figure 3D) was covered on them with another piece of PRF membrane overlap on the top (Figure 3E). Tension-free suture was performed in the operative area (Figure 3F). Antibiotic prophylaxis of postoperative protocol was received for 3 d, rinsing with 0.12% chlorhexidine solution for 7 d.
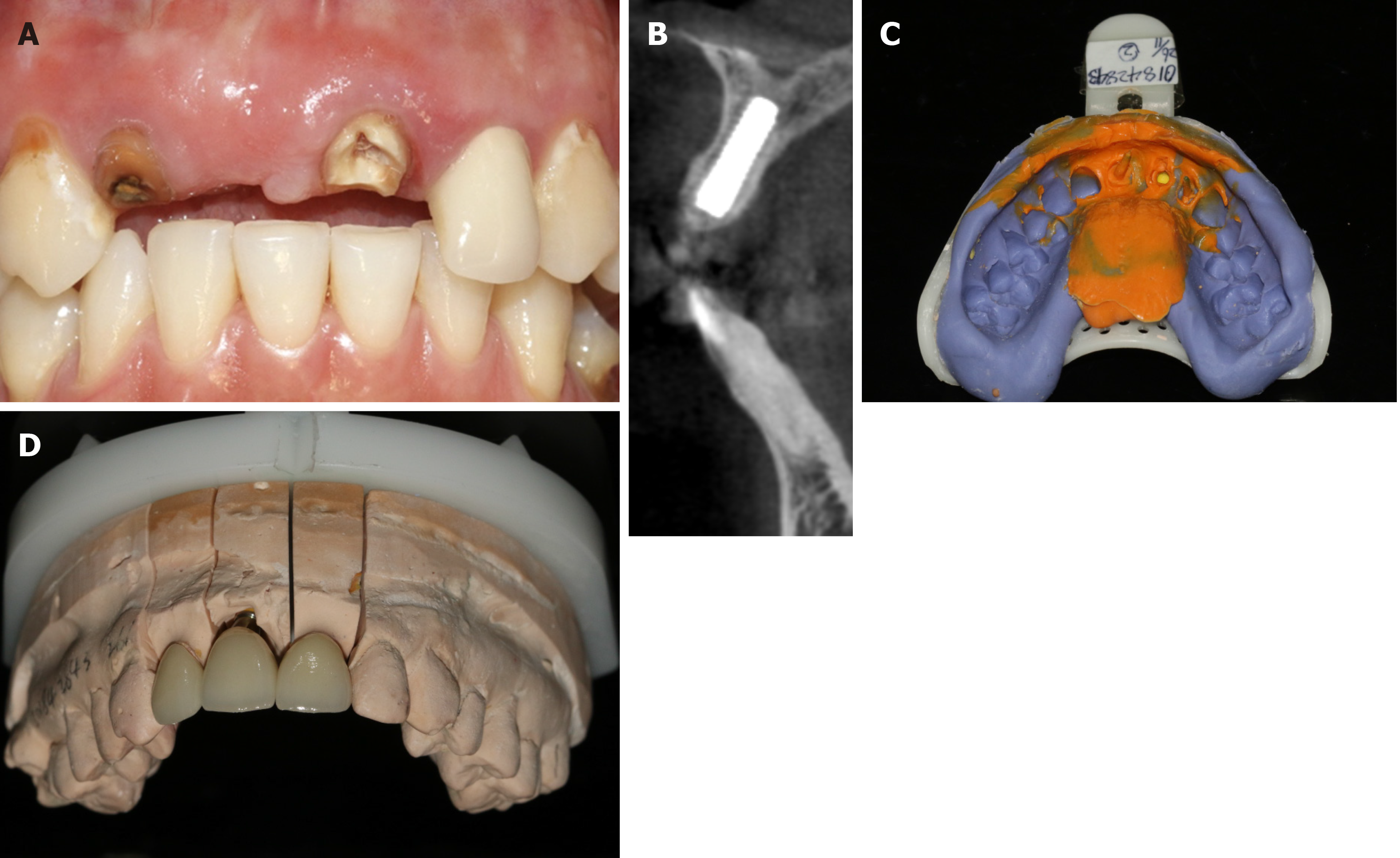
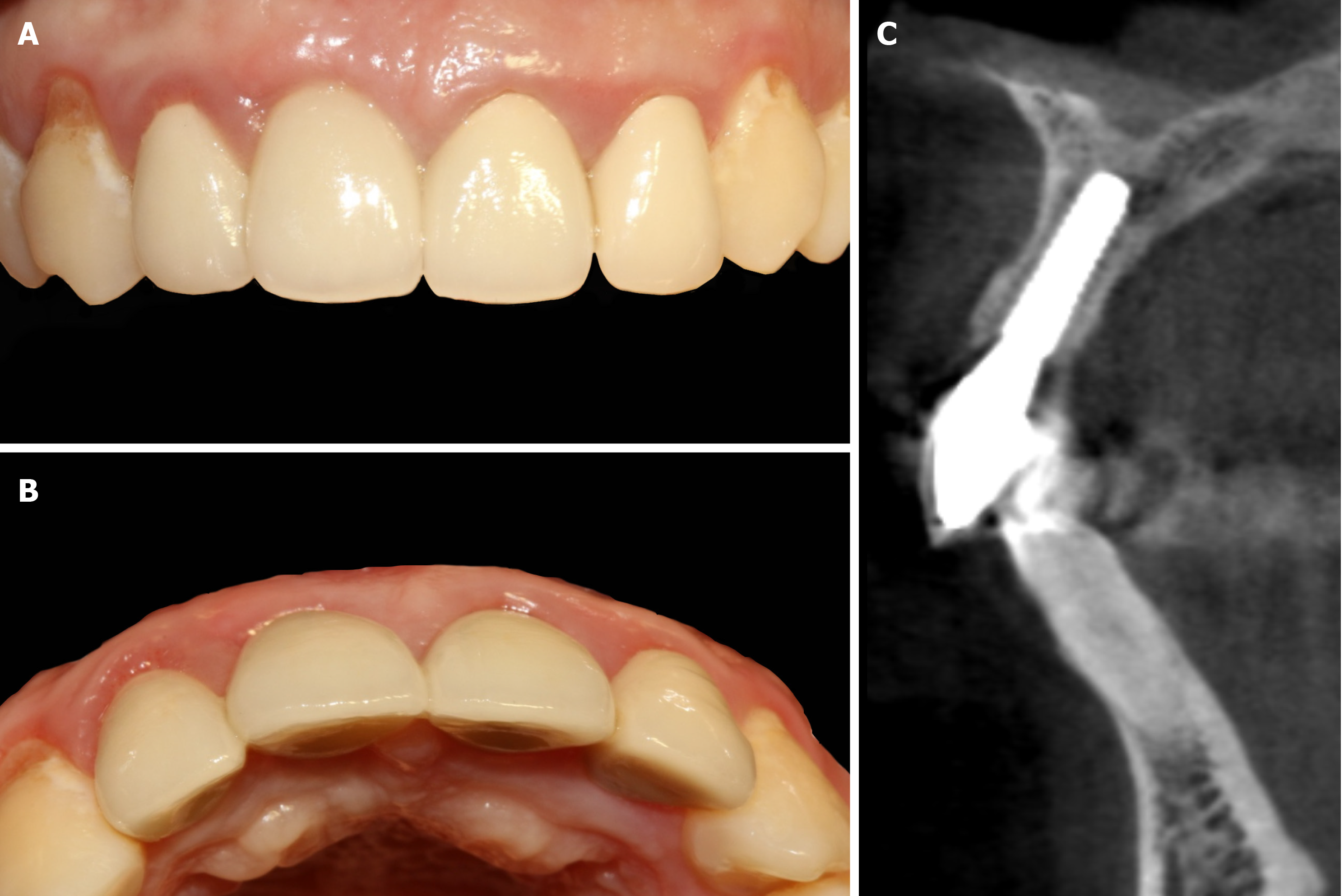
There were no complications during the postsurgical healing period. The 6-mo follow-up showed well-rounded shape of gingiva (Figure 4A). CBCT scanning revealed that the incremental thickness of labial bone was more than 2 mm (Figure 4B). Two-stage operation was taken to replace the cover screw by healing abutment. Because the restored crown fell off 2 wk ago, No. 21 had to be restored simultaneously with the implant. After impression (Figure 4C and D), definitive all-ceramic crowns were manufactured and restored for both implant and adjacent teeth with patient’s high satisfaction (Figure 5A, B and D). Periapical radiograph confirmed that the implant was well-integrated while the crowns of the adjacent teeth were good condition (Figure 5C). Follow-up after 1 year, the hard and soft tissue was still healthy and stable (Figure 6A and B). Moreover, CBCT showed that the labial and palatal side of alveolar bone around the implant were completely favorable without obvious absorption (Figure 6C).
Periapical lesion caused by frustrated root canal therapy or root fracture is common clinically, which frequently leads to the severe resorption of alveolar bone and to the increasing risk of esthetic restoration[5,6]. Recent studies have shown that the survival rates of immediate implantation at infected sites is similar as the areas without infection[16,17]. However, some research also demonstrated that the contaminated tissue of infected alveoli should be removed completely in immediate implantation[18]. There was no significant difference in the final success rate between the infected-group and the non-infected group, but the bone-to-implant contact and the rate of initial bone bonding in infected areas were obviously decreased[19]. Especially in the situation of immediate implantation at maxillary anterior region, enough width of labial bone is absolutely necessary for the aesthetic requirement[20,21]. The alveolar ridge would be atrophic as well as the recession of soft tissue after tooth extraction[22]. This evidence suggests that the correct disposal of dentoalveolar infections in the clinic and the exact option of implanting location along with proper considerations of tissue augmentation can greatly increase the successful rates of immediate implant placement in the esthetic zone[2,18]. In addition, the effective technique such as guided bone regeneration was frequently used in immediate implantation to repair the bone defect and to obtain the ideal effects of finial restoration in clinic. In order to maintain the space for bone regeneration, enough artificial bone dust should be filled into the defect region. But the lack of cancellous bone with insufficient blood supply and the exposure of collagen membrane in guided bone regeneration might directly lead to the ultimate failure of osseointegration[23,24]. Thus, the adequate blood supply and soft tissue covering bone substitute should be the key factor of immediate implantation, which also directly affects the final aesthetic effect.
In recent years, concentrated platelets have been used in wound healing because of their high growth factor content[25]. PRF is a typical platelet concentrate consisting of an autologous leukocyte-platelet-rich fibrin matrix, which has three-dimensional structure filling with cytokines, platelets and stem cells within[26]. These cytokines have significant defense capacities against infections. The large amount of white blood cells has played an important role in anti-inflammatory and anti-bacterial action during the process of immune regulation and angiogenesis[27]. The local and continuous releasing growth factors of PRF could stimulate the vascularization of damaged tissues, presenting synergetic effects on healing processes[13]. The presence of inflammatory retrocontrol cytokines could also participate in the inflammatory regulation on implanting sites[28]. In addition, the slow blood activation process of PRF would increase the secretion of the inflammatory or cicatricial interleukins at injured site, which means that the PRF was an immune node able to stimulate defense mechanisms[29]. Clinical studies demonstrate that the PRF could be used in periapical surgery[30], chronic periodontitis[31], osseous regeneration after cystic enucleation[32] and other surgical applications for infected wound[33] to reduce the inflammation and accelerate the tissue regeneration. In addition, the combination of PRF and bone substitutes used in immediate implantation presents an excellent promotion of osteogenesis and remarkable acceleration of bone healing under inflammatory conditions[34]. Compared with the collagen membrane, PRF has better and faster healing with fewer postoperative complications for grafting of oral soft tissue defects[35,36]. Therefore, in this case, PRF was mixed with the bone substitute to reduce the inflammatory response in extraction socket, preventing the interference with bone regeneration and accelerating the early bone healing. The mixture of Bio-Oss and PRF were filled into the bone defect to repair the hard tissue. The PRF functioned to improve the blood circulation and shaping and stimulate the regeneration of bone tissues. At the same time, the gradual release of cytokines in PRF played an important role in the self-regulation of inflammation and infection, which could reduce the inflammatory response, prevent the interference of bone regeneration and accelerate early bone healing.
Furthermore, the innovation approaches of PRF and collagen membranes have been used simultaneously as a sandwich-like bio-membrane to improve the regeneration of soft tissue. The PRF on the surface of Bio-Oss was designated to facilitate the osseointegration and provide the profitable space for cell proliferation and migration[37,38]. The PRF placed over the collagen membrane served as a protective barrier to promote the remodeling of soft tissue, while minimizing the risk exposure of internal membrane and lessening the scar formation of soft tissues[35]. As shown in this case, CBCT and clinical assessment have both represented the great osseointegration and satisfactory contour of gingival in the aesthetic area. The three-layer membrane structure has not only provided a better mechanical property for maintaining stable space but also presented good biological functions for accelerating tissue regeneration and infection prevention.
In spite of the high-risk of the immediate implantation in infected areas, there is also a unique advantage. The process of tooth extraction, implant placement and PRF have been combined in one appointment, which has significantly shortened the course of treatment that patients require. In this case, PRF was used as an important healing biomaterial for immediate implantation of anterior teeth with periapical inflammation, which is considered a safe, reliable and economical material to improve the efficiency of tissue repair. By the simple improvement of traditional guided bone regeneration, the bone augmentation, aesthetic effect and psychological effects have been well satisfied by clinician and patient. Therefore, immediate implantation in infected sockets with PRF is an alternative method to optimize treatment and to improve esthetics. It can be recommended for tissue regeneration of inflammatory sites. Despite successful results in this case report, more superb surgical skills and longer follow-up are still necessary to be confirmed.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Nobel Bloccare Dental Academy Member; International College of Dentists Member; International College of Prosthodontists Member; FDI Member.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Velikova TV S-Editor: Zhang L L-Editor: Filipodia P-Editor: Xing YX
| 1. | Evans CD, Chen ST. Esthetic outcomes of immediate implant placements. Clin Oral Implants Res. 2008;19:73-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 132] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 2. | Wheeler SL. Implant complications in the esthetic zone. J Oral Maxillofac Surg. 2007;65:93-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Marcaccini AM, Novaes AB Jr, Souza SL, Taba M Jr, Grisi MF. Immediate placement of implants into periodontally infected sites in dogs. Part 2: A fluorescence microscopy study. Int J Oral Maxillofac Implants. 2003;18:812-819. [PubMed] |
| 4. | Zhao D, Wu Y, Xu C, Zhang F. Immediate dental implant placement into infected vs. non-infected sockets: a meta-analysis. Clin Oral Implants Res. 2016;27:1290-1296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Hita-Iglesias C, Sánchez-Sánchez FJ, Montero J, Galindo-Moreno P, Mesa F, Martínez-Lara I, Sánchez-Fernández E. Immediate Implants Placed in Fresh Sockets Associated with Periapical Pathology: A Split-Mouth Design and Survival Evaluation after 1-Year Follow-Up. Clin Implant Dent Relat Res. 2016;18:1075-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Deng F, Zhang H, Zhang H, Shao H, He Q, Zhang P. A comparison of clinical outcomes for implants placed in fresh extraction sockets versus healed sites in periodontally compromised patients: a 1-year follow-up report. Int J Oral Maxillofac Implants. 2010;25:1036-1040. [PubMed] |
| 7. | Misch CE. Endosteal implants for posterior single tooth replacement: alternatives, indications, contraindications, and limitations. J Oral Implantol. 1999;25:80-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Boora P, Rathee M, Bhoria M. Effect of Platelet Rich Fibrin (PRF) on Peri-implant Soft Tissue and Crestal Bone in One-Stage Implant Placement: A Randomized Controlled Trial. J Clin Diagn Res. 2015;9:ZC18-ZC21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Luo WJ, Zhao JH, Ma SS, Sun QY, Guo TQ, Zhou YM. Biological composition and function of platelet-rich fibrin. Int J Stomatol. 2014;41:448-454. [DOI] [Full Text] |
| 10. | Jang ES, Park JW, Kweon H, Lee KG, Kang SW, Baek DH, Choi JY, Kim SG. Restoration of peri-implant defects in immediate implant installations by Choukroun platelet-rich fibrin and silk fibroin powder combination graft. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:831-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Brouwers JEIG, Buis S, Haumann R, de Groot PPG, de Laat B, Remijn JA. Successful soft and hard tissue augmentation with platelet-rich fibrin in combination with bovine bone space maintainer in a delayed implant placement protocol in the esthetic zone: A case report. Clin Case Rep. 2019;7:1185-1190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Everts PA, Devilee RJ, Brown Mahoney C, van Erp A, Oosterbos CJ, Stellenboom M, Knape JT, van Zundert A. Exogenous application of platelet-leukocyte gel during open subacromial decompression contributes to improved patient outcome. A prospective randomized double-blind study. Eur Surg Res. 2008;40:203-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 167] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 13. | Bielecki T, Dohan Ehrenfest DM, Everts PA, Wiczkowski A. The role of leukocytes from L-PRP/L-PRF in wound healing and immune defense: new perspectives. Curr Pharm Biotechnol. 2012;13:1153-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 127] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 14. | Martande SS, Kumari M, Pradeep AR, Singh SP, Suke DK, Guruprasad CN. Platelet-Rich Fibrin Combined With 1.2% Atorvastatin for Treatment of Intrabony Defects in Chronic Periodontitis: A Randomized Controlled Clinical Trial. J Periodontol. 2016;87:1039-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Pradeep AR, Nagpal K, Karvekar S, Patnaik K, Naik SB, Guruprasad CN. Platelet-rich fibrin with 1% metformin for the treatment of intrabony defects in chronic periodontitis: a randomized controlled clinical trial. J Periodontol. 2015;86:729-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 16. | Lindeboom JA, Tjiook Y, Kroon FH. Immediate placement of implants in periapical infected sites: a prospective randomized study in 50 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:705-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 158] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 17. | Yi JY, Kim JH, Han DH. Immediate implant placement into extraction sites with periapical lesions in the esthetic zone: a case report. J Korean Acad Prosthodont. 2012;50:191-197. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Casap N, Zeltser C, Wexler A, Tarazi E, Zeltser R. Immediate placement of dental implants into debrided infected dentoalveolar sockets. J Oral Maxillofac Surg. 2007;65:384-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 19. | Chang SW, Shin SY, Hong JR, Yang SM, Yoo HM, Park DS, Oh TS, Kye SB. Immediate implant placement into infected and noninfected extraction sockets: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, Steigmann M, Rebaudi A, Palti A, Pikos MA, Schwartz-Arad D, Choukroun J, Gutierrez-Perez JL, Marenzi G, Valavanis DK. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008;17:5-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 517] [Cited by in RCA: 598] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 21. | Mestas G, Alarcón M, Chambrone L. Long-Term Survival Rates of Titanium Implants Placed in Expanded Alveolar Ridges Using Split Crest Procedures: A Systematic Review. Int J Oral Maxillofac Implants. 2016;31:591-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Hansson S, Halldin A. Alveolar ridge resorption after tooth extraction: A consequence of a fundamental principle of bone physiology. J Dent Biomech. 2012;3:1758736012456543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 101] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 23. | Halmos J, Korman V, Bálek F, Benuska J, Mentel J. [Reparative osteogenesis in interrupted blood supply]. Cesk Stomatol. 1967;67:174-177. [PubMed] |
| 24. | Garcia J, Dodge A, Luepke P, Wang HL, Kapila Y, Lin GH. Effect of membrane exposure on guided bone regeneration: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29:328-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 115] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 25. | Durmuşlar MC, Balli U, Dede FÖ, Misir AF, Bariş E, Kürkçü M, Kahraman SA. Histological Evaluation of the Effect of Concentrated Growth Factor on Bone Healing. J Craniofac Surg. 2016;27:1494-1497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 26. | Cortese A, Pantaleo G, Amato M, Howard CM, Pedicini L, Claudio PP. Platelet-Rich Fibrin (PRF) in Implants Dentistry in Combination with New Bone Regenerative Flapless Technique: Evolution of the Technique and Final Results. Open Med (Wars). 2017;12:24-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Herrera-Vizcaíno C, Dohle E, Al-Maawi S, Booms P, Sader R, Kirkpatrick CJ, Choukroun J, Ghanaati S. Platelet-rich fibrin secretome induces three dimensional angiogenic activation in vitro. Eur Cell Mater. 2019;37:250-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 28. | Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e45-e50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 544] [Cited by in RCA: 686] [Article Influence: 36.1] [Reference Citation Analysis (0)] |
| 29. | Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part III: leucocyte activation: a new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e51-e55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 481] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 30. | E D, Kumar A, Tewari RK, Mishra SK, Iftekhar H. Management of large preiapical lesion with the combination of second generation platelet extract and hydroxyapatite bone graft: a report of three cases. J Clin Diagn Res. 2015;9:ZD24-ZD27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Sharma A, Pradeep AR. Treatment of 3-wall intrabony defects in patients with chronic periodontitis with autologous platelet-rich fibrin: a randomized controlled clinical trial. J Periodontol. 2011;82:1705-1712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 117] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 32. | Dar M, Hakim T, Shah A, Najar L, Yaqoob G, Lanker F. Use of autologous platelet-rich fibrin in osseous regeneration after cystic enucleation: A clinical study. J Oral Biol Craniofac Res. 2016;6:S29-S32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 33. | Yamakawa S, Hayashida K. Advances in surgical applications of growth factors for wound healing. Burns Trauma. 2019;7:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 164] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 34. | Del Fabbro M, Boggian C, Taschieri S. Immediate implant placement into fresh extraction sites with chronic periapical pathologic features combined with plasma rich in growth factors: preliminary results of single-cohort study. J Oral Maxillofac Surg. 2009;67:2476-2484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 35. | Mahajan M, Gupta MK, Bande C, Meshram V. Comparative Evaluation of Healing Pattern After Surgical Excision of Oral Mucosal Lesions by Using Platelet-Rich Fibrin (PRF) Membrane and Collagen Membrane as Grafting Materials-A Randomized Clinical Trial. J Oral Maxillofac Surg 2018; 76: 1469.e1-1469. e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 36. | Miron RJ, Fujioka-Kobayashi M, Bishara M, Zhang Y, Hernandez M, Choukroun J. Platelet-Rich Fibrin and Soft Tissue Wound Healing: A Systematic Review. Tissue Eng Part B Rev. 2017;23:83-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 270] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 37. | Hafez W, Seif S, Shawky H, Hakam MM. Platelet rich fibrin as a membrane for coverage of immediate implants: Case-series study on eight patients. Tanta Dental J. 2015;12:203-210. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 38. | Zhou T, Yang HW, Tian ZW, Wang Y, Tang XS, Hu JZ. Effect of Choukroun Platelet-Rich Fibrin Combined With Autologous Micro-Morselized Bone on the Repair of Mandibular Defects in Rabbits. J Oral Maxillofac Surg. 2018;76:221-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |