Published online Feb 6, 2021. doi: 10.12998/wjcc.v9.i4.951
Peer-review started: October 22, 2020
First decision: November 20, 2020
Revised: November 25, 2020
Accepted: December 11, 2020
Article in press: December 11, 2020
Published online: February 6, 2021
Processing time: 94 Days and 23 Hours
Pheochromocytoma is a rare catecholamines-secreting tumor arising from chromaffin cells in the adrenal medulla. It classically presents with paroxysmal hypertension, headaches, palpitations, sweating, and metabolic disorders. Atypical presentations such as acute myocardial infarction, heart failure, cardiomyopathy, stroke, and transient erythrocytosis have been infrequently documented.
We describe the case of a 72-year-old man diagnosed with pheochromocytoma presenting with non-ST segment elevation myocardial infarction, heart failure, and transient erythrocytosis with nonobstructed coronary arteries. This was his second heart attack. The patient was previously diagnosed with myocardial infarction, and an immense mass was found on the left adrenal gland 3 years prior. Based on clinical and laboratory findings, a diagnosis of pheochromocytoma was confirmed. His coronary angiogram showed nonobstructed coronary arteries except for a myocardial bridge in the left anterior descending branch. This was a form of type-2 myocardial infarction. The myocardial cell lesions were caused by sudden secretion of catecholamines by the pheochromocytoma. Even more atypically, his hemoglobin level was obviously elevated at admission, but after a few days of treatment with an alpha-adrenergic receptor blocker, it dropped to normal levels without additional treatment.
Pheochromocytoma may be a cause of acute myocardial infarction, heart failure, and transient erythrocytosis.
Core Tip: Pheochromocytomas release massive amounts of catecholamines that can cause life-threatening cardiovascular complications, including cardiac arrhythmia, ST and non-ST segment elevation myocardial infarction, heart failure, and hypertensive urgency. For acute myocardial infarction with unexplained erratic blood pressure, headaches, palpitations, and sweating, pheochromocytoma should be considered a differential diagnosis. Pheochromocytoma is a non-atherosclerotic cause of myocardial infarction. The myocardial cell lesions may be caused by tachycardia, coronary artery spasm, or cardiomyopathy, which are related to excess catecholamines. Pheochromocy-toma with erythrocytosis is rarely reported. Elevated hematocrit contributes to increased blood viscosity and thus, to higher risk of coronary heart disease.
- Citation: Shi F, Sun LX, Long S, Zhang Y. Pheochromocytoma as a cause of repeated acute myocardial infarctions, heart failure, and transient erythrocytosis: A case report and review of the literature. World J Clin Cases 2021; 9(4): 951-959
- URL: https://www.wjgnet.com/2307-8960/full/v9/i4/951.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i4.951
Pheochromocytoma is a neuroendocrine tumor of the adrenal medulla. The prevalence of pheochromocytoma is estimated at between 1:4500 and 1:1700 in the general population[1]. Severe cardiovascular complications including ventricular tachycardia, ST and non-ST segment elevation myocardial infarction (NSTEMI), heart failure, stress cardiomyopathy, and hypertensive urgency can occur in 19.3% of pheochromocytoma patients[2,3]. It classically presents with paroxysmal hypertension, headaches, palpitations, sweating, and metabolic disorders[4-7]. Plasma and urinary catecholamine and 24-hurine vanillylmandelic acid measurements can be helpful to aid its diagnosis in addition to computed tomography scans or other imaging examinations. In this study, we present a case with acute myocardial infarction, heart failure, and transient erythrocytosis secondary to pheochromocytoma.
A 72-year-old Chinese man presented to the Emergency Department of our hospital with retrosternal chest pain. The pain lasted approximately half an hour and was associated with palpitations, sweating, dizziness, nausea, and difficulty breathing.
In the prior 3 years, the patient experienced intermittent retrosternal pain with palpitations, sweating, fatigue, and dizziness lasting from a few minutes to an hour. The patient’s symptoms relapsed 3 d before admission in a resting state. He was previously diagnosed with NSTEMI, and an immense mass was found on his left adrenal gland 3 years prior. Since then, he was treated with aspirin, statin, and nitrate for an extended time, but there was no obvious effect. At the same time, progressive weight loss was observed (approximately 5 kg within the prior 6 mo, 16 kg in total since NSTEMI diagnosis).
The patient had a history of paroxysmal hypertension for 3 years. Because of the large fluctuation of blood pressure (from 11.9/7.3 kPa to 30.6/18.6 kPa), taking medicine was burdensome to him. He was treated with oral nifedipine intermittently (nifedipine was taken when blood pressure higher than 18.6/13.3 kPa).
He had been smoking approximately 10 cigarettes a day for 30 years. There was no significant family history to note.
During the patient’s hospital stay, his blood pressure showed erratic fluctuations from 27.1/17.0 kPa to 11.8/7.4 kPa and heart rates from 79 to 138 beats per minute associated with the symptoms described previously. His body weight was 54 kg and height was 170 cm (BMI 18.7 kg/m2). The physical examination revealed mild bilateral basilar crackles, with no jugular venous distention and normal heart sounds. He had tenderness beneath the xiphoid process, and there was no peripheral pedal edema.
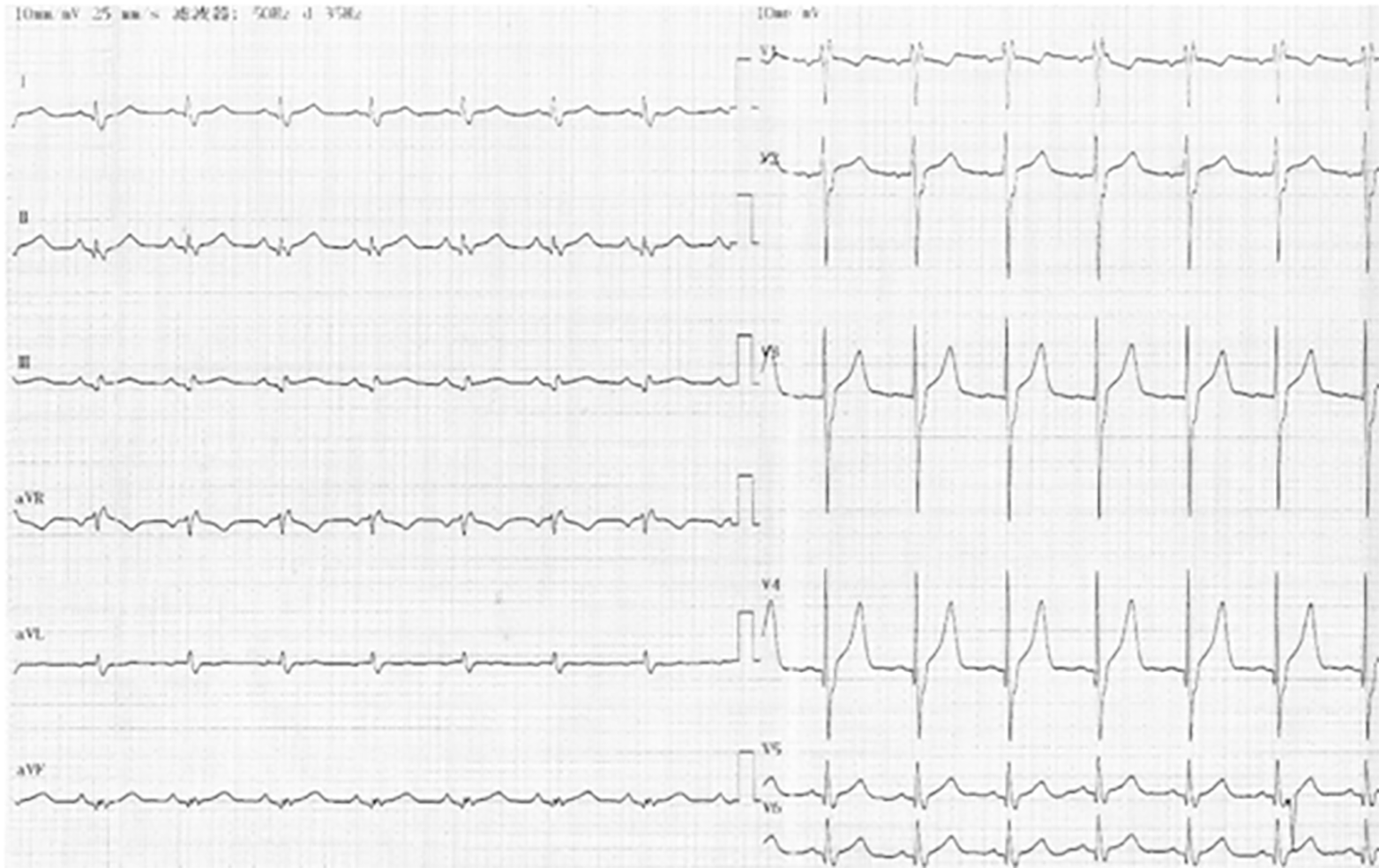
The patient was diagnosed with NSTEMI because troponin I was abnormal (0.75 ng/mL and 0.89 ng/mL, normal reference < 0.4 ng/mL). Electrocardiogram showed sinus tachycardia, incomplete right bundle branch block, and no significant change in ST segment or T wave (Figure 1). Brain natriuretic peptide (BNP), a biomarker of heart failure, was significantly increased (2980 pg/mL, normal reference < 100 pg/mL). An unusual blood test was also found. The levels of the patient’s hemoglobin increased remarkably (203 g/L and 194 g/L, normal reference 130-175 g/L). These episodic symptoms, the erratic blood pressure pattern, and the volume of the mass on adrenal gland raised the suspicion of pheochromocytoma. Plasma and urinary catecholamines were elevated more than 10-fold compared to the reference range (Table 1). The value of 24-h urine vanillylmandelic acid was also extremely high (86.2 mg/24 h and 69.5 mg/24 h, normal reference 0-12 mg/24 h).
| Catecholamines | Plasma urine | Reference range |
| Free normetanephrine (NMN) | 8590 pg/mL | < 145 pg/mL |
| Free metanephrine (MN) | 1260 pg/mL | < 62 pg/mL |
| Free (NMN + MN) | 9850 pg/mL | < 207 pg/mL |
| Normetanephrine (NMN) | 6440 μg/24h | 109-393 μg/24h |
| Metanephrine (MN) | 1920 μg/24h | 39-143 μg/24h |
| (NMN + MN) | 8360 μg/24h | 148-536 μg/24h |
| Free norepinephrine (NE) | 7000 μg/24h | 0-90 μg/24h |
| Free epinephrine (E) | 676 μg/24h | 0-20 μg/24h |
| Free dopamine (DA) | 557 μg/24h | 0-600 μg/24h |
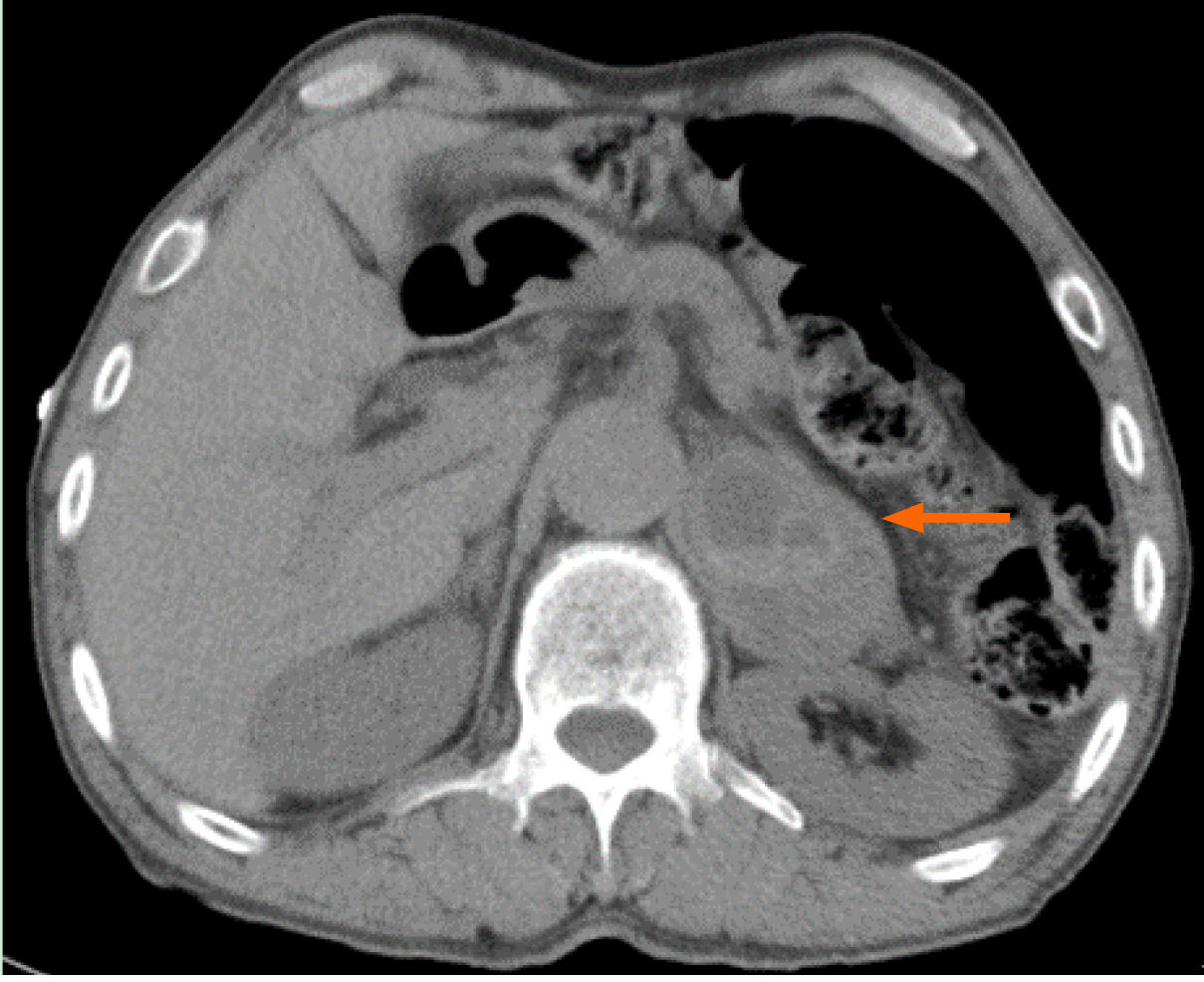
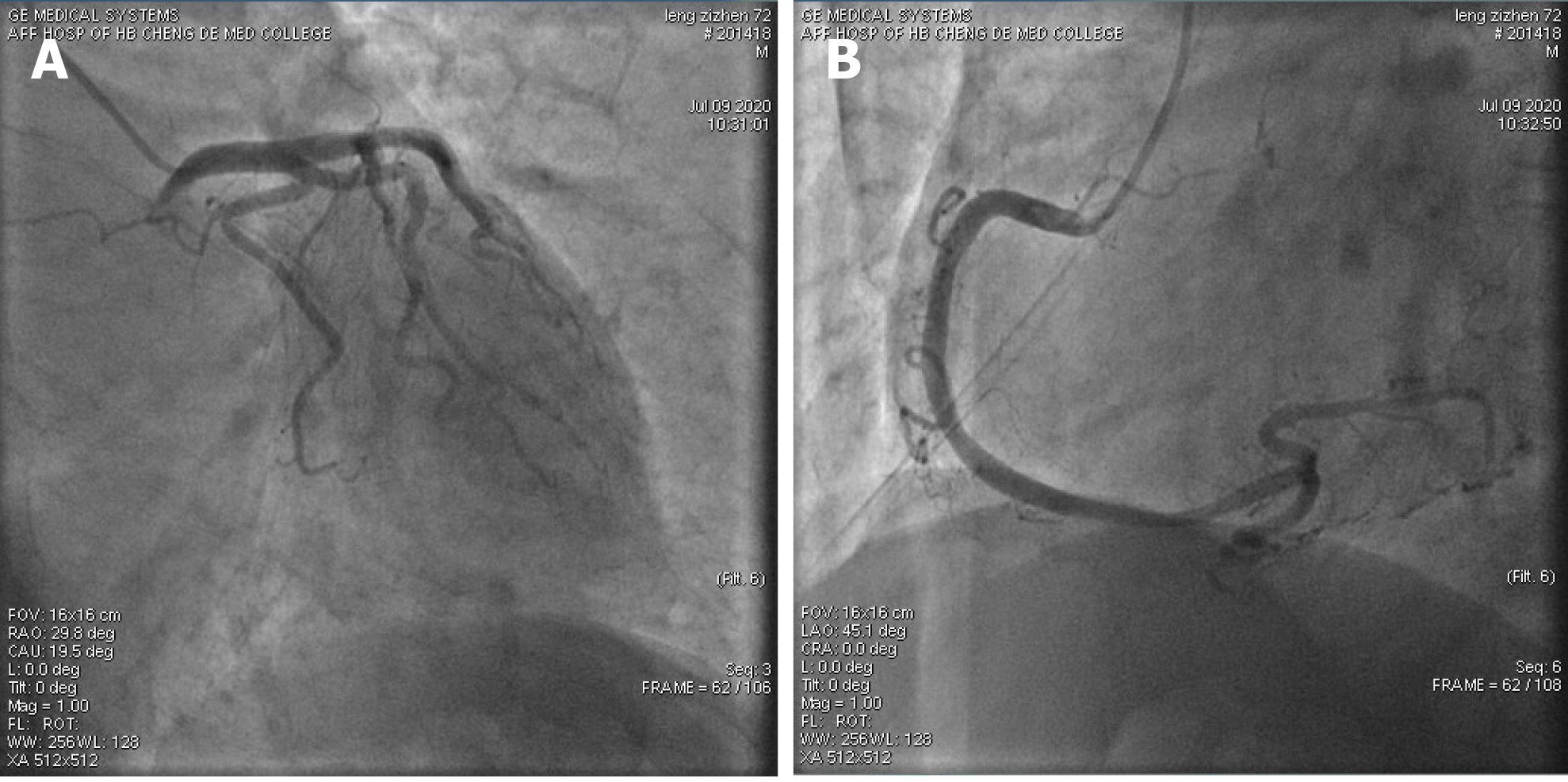
Computed tomography and Doppler ultrasound showed a well-defined, rounded mass in the left adrenal gland, measuring 46.4 mm × 53.5 mm × 56.0 mm (Figure 2), which was consistent with the diagnosis of pheochromocytoma. The left ventricular ejection fraction (LVEF) was measured by cardiac Doppler ultrasound and was only 41%. Additionally, a regional wall motion defect was observed. The patient’s biomarker of acute myocardial infarction was mildly elevated, and there were no new Q waves or changes in ST segment. We suspected that there was no obstruction in his coronary arteries. After a loading dose of aspirin and clopidogrel, coronary angiography was performed and revealed no occlusion in coronary arteries except a myocardial bridge in the left anterior descending branch (Figure 3).
The final diagnosis was pheochromocytoma with secondary acute myocardial infarction and heart failure.
The patient was medically stabilized with an alpha-adrenergic receptor blocker (terazosin, 4 mg per day). Dyspnea was relieved by diuretics (furosemide, 20 mg per day and spironolactone, 20 mg per day). He refused to have a left adrenalectomy.
After 10 d of medication, the patient’s symptoms improved. The biomarkers of myocardial injury returned to normal, and BNP decreased to 1070 pg/mL. Interestingly, his hemoglobin level also dropped to normal (137 g/L) without additional treatment. At the 1-mo follow-up, he had no complaints and his BNP decreased to 385 pg/mL and LVEF returned to normal (52%).
Pheochromocytoma with life-threatening cardiovascular complications is rare and atypical. In our case, the patient was diagnosed with pheochromocytoma presenting with repeated acute myocardial infarctions and heart failure. The coronary angiogram showed nonobstructed coronary arteries. We noted that most of such patients had few significant coronary atherosclerosis in past reports[8-10]. Most reports suggested that cardiomyopathy, severe coronary vasospasm, myocarditis, and tachycardia caused by excessive release of catecholamines result in elevated cardiac troponin and reduced left ventricular systolic function[11,12]. This case illustrates pheochromocytoma as one of the differential diagnoses for myocardial infarction with nonobstructed coronary arteries, especially in patients with unexplained erratic blood pressure and symptoms suggestive of pheochromocytoma.
In this case, the patient’s biomarker of acute myocardial infarction was mildly elevated, which was not consistent with the severity of heart failure. Pheochromocy-toma can lead to different cardiomyopathies, including Takotsubo cardiomyopathies and catecholamine cardiomyopathies[13,14].
Takotsubo cardiomyopathy, also called stress cardiomyopathy or apical ballooning syndrome, may lead to transient left ventricular systolic dysfunction and mimic ST segment elevation myocardial infarction[15-17]. The left ventriculography and echocardiography can show a ballooning pattern that is most apparent in the anterior wall and apical septum rather than the basal part of the left ventricle[18]. The abnormal motion of the myocardium would normalizes within a few days to several weeks[19-21]. In this case, the patient was diagnosed with NSTEMI with nonobstructed coronary arteries and segmental left ventricular wall motion abnormalities (no ballooning pattern, and LVEF was only 41%). This is a form of catecholamine cardiomyopathy. The two types of cardiomyopathies may be explained by the same pathophysiological mechanism of catecholamine oversecretion which induces microvascular dysfunction, epicardial spasm, and direct effects on cardiac myocytes[22]. Acute pulmonary edema is more frequent in catecholamine cardiomyopathy. Left ventricular mass index, relative wall thickness, and elevated blood pressure are more prominent in catecholamine cardiomyopathy compared to Takotsubo cardiomyopathy[23]. Patients with Takotsubo cardiomyopathy exhibit better recovery of left ventricular ejection fraction. The reported in-hospital mortality rate of pheochromocytoma-induced cardiomyopathy is relatively low (2.5%)[24]. Early diagnosis of both conditions is crucial for improving prognosis[25].
Pheochromocytoma with erythrocytosis is rarely reported. This atypical syndrome may result from somatic mutations in hypoxia-inducible factor 2A (HIF-2A) and germline mutations in prolyl hydroxylases 1 and 2 (PHD1 and PHD2), which have been identified to function as regulators of erythropoietin and its receptor[26-29]. A new report provides evidence of an association between a somatic iron regulatory protein (IRP1) mutation and pheochromocytoma with secondary erythrocytosis[30]. IRP1 is a principal regulator of translational derepression of HIF-2A mRNA in iron-deficient cells, which facilitates HIF-2A mRNA accumulation and increased stimulation of erythropoietin expression[31,32]. These findings explain the transient exacerbation of secondary polycythemia in patients with erythropoietin-secreting pheochromocy-toma[33]. Elevated hematocrit contributes to increased blood viscosity and platelet adhesion[34,35]. Increased blood viscosity promotes blood clot formation and increased platelet activation at the vessel wall and thus, presents a higher risk of coronary heart disease[36].
Many different treatment options are used to control the effects of catecholamine hypersecretion including blockades (such as alpha blockers, calcium channel blockers, beta blockers, and tyrosine hydroxylase inhibitors), surgical resection, radiofrequency ablation, and radiotherapy[37]. Alpha blockers and surgical resection are the primary approach for managing patients with pheochromocytoma. Phenoxybenzamine is a long-lasting and noncompetitive inhibitor that is commonly used in perioperative management. Other alpha blockers such as doxazosin, terazosin, and prazosin can be used when phenoxybenzamine is not available or when a patient's hypertension is not severe enough to warrant the use of a long-acting alpha blocker. Calcium channel blockers can also be used for additional blood pressure control. These include nifedipine, amlodipine, and verapamil. In patients with tachycardia, arrhythmias, or angina, beta blockers such as propranolol, atenolol, or metoprolol are indicated. Beta blockers should never be used in the absence of an efficient α-blockade because loss of β-adrenoceptor-mediated vasodilatation can lead to hypertensive crises and even cardiac arrest[38,39]. Surgical resection, especially laparoscopic surgery, has been successfully performed in patients with pheochromocytoma with outcomes similar to open surgery[40,41] (Table 2).
| Date | Events |
| May 18, 2017 | Retrosternal pain, palpitations, sweating, dizziness |
| May 20, 2017 | Acute myocardial infarction |
| An immense mass on the adrenal gland | |
| Paroxysmal hypertension | |
| June 29, 2020 | Acute myocardial infarction |
| Heart failure | |
| Erythrocytosis | |
| July 3, 2020 | Pheochromocytoma was confirmed |
| July 9, 2020 | Coronary angiogram showed nonobstructed coronary arteries |
| July 10, 2020 | Hemoglobin level dropped to normal |
| August 15, 2020 | At follow-up, no complaints, laboratory examinations improved |
Excessive release of catecholamines in pheochromocytoma results in elevated cardiac troponin, reduced left ventricular systolic function, and transient erythrocytosis with most lesions returning to normal within days to weeks. In patients with unexplained erratic blood pressure control and myocardial infarction with normal coronary arteries, pheochromocytoma should be considered a differential diagnosis.
The authors thank the patient and his family for their participation.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Holmes J, Shetty K S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Kantorovich V, Pacak K. Pheochromocytoma and paraganglioma. Prog Brain Res. 2010;182:343-373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Menke-van der Houven van Oordt CW, Twickler TB, van Asperdt FG, Ackermans P, Timmers HJ, Hermus AR. Pheochromocytoma mimicking an acute myocardial infarction. Neth Heart J. 2007;15:248-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Melson E, Amir S, Shepherd L, Kauser S, Freestone B, Kempegowda P. Myocardial Infarction with non-obstructed coronaries - atypical presentation of pheochromocytoma. Endocrinol Diabetes Metab Case Rep. 2019;2019:EDM190089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Lenders JW, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet. 2005;366:665-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1154] [Cited by in RCA: 1138] [Article Influence: 56.9] [Reference Citation Analysis (0)] |
| 5. | Falhammar H, Kjellman M, Calissendorff J. Initial clinical presentation and spectrum of pheochromocytoma: a study of 94 cases from a single center. Endocr Connect. 2018;7:186-192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 81] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 6. | Amar L, Servais A, Gimenez-Roqueplo AP, Zinzindohoue F, Chatellier G, Plouin PF. Year of diagnosis, features at presentation, and risk of recurrence in patients with pheochromocytoma or secreting paraganglioma. J Clin Endocrinol Metab. 2005;90:2110-2116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 257] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 7. | Gruber LM, Hartman RP, Thompson GB, McKenzie TJ, Lyden ML, Dy BM, Young WF, Bancos I. Pheochromocytoma Characteristics and Behavior Differ Depending on Method of Discovery. J Clin Endocrinol Metab. 2019;104:1386-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 103] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 8. | Imam T, Finny P, Choo-Kang A, Khan R. Phaeochromocytoma presenting as an acute coronary syndrome. BMJ Case Rep. 2016;2016:bcr2016214737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Yang TH, Tsai WC. Recurrence and metastasis of pheochromocytoma mimic acute ST-segment elevation myocardial infarction: a case report. Am J Emerg Med 2015; 33: 311.e3-311. e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Y-Hassan S, Falhammar H. Cardiovascular Manifestations and Complications of Pheochromocytomas and Paragangliomas. J Clin Med. 2020;9:2435. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 11. | Sethi P, Chang GV, Gowda SN, Elnair R, Fenner R, Lamfers R. Recurrent Catecholamine-Induced Cardiomyopathy and Hypertensive Emergencies: A presentation of Pheochromocytoma and Related Concerns. S D Med. 2020;73:78-80. [PubMed] |
| 12. | Diaz B, Elkbuli A, Ehrhardt JD Jr, McKenney M, Boneva D, Hai S. Pheochromocytoma-related cardiomyopathy presenting as broken heart syndrome: Case report and literature review. Int J Surg Case Rep. 2019;55:7-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Santos JRU, Brofferio A, Viana B, Pacak K. Catecholamine-Induced Cardiomyopathy in Pheochromocytoma: How to Manage a Rare Complication in a Rare Disease? Horm Metab Res. 2019;51:458-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 61] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 14. | Batisse-Lignier M, Pereira B, Motreff P, Pierrard R, Burnot C, Vorilhon C, Maqdasy S, Roche B, Desbiez F, Clerfond G, Citron B, Lusson JR, Tauveron I, Eschalier R. Acute and Chronic Pheochromocytoma-Induced Cardiomyopathies: Different Prognoses? Medicine (Baltimore). 2015;94:e2198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Y-Hassan S, De Palma R. Contemporary review on the pathogenesis of takotsubo syndrome: The heart shedding tears: Norepinephrine churn and foam at the cardiac sympathetic nerve terminals. Int J Cardiol. 2017;228:528-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 16. | Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, Cammann VL, Crea F, Galiuto L, Desmet W, Yoshida T, Manfredini R, Eitel I, Kosuge M, Nef HM, Deshmukh A, Lerman A, Bossone E, Citro R, Ueyama T, Corrado D, Kurisu S, Ruschitzka F, Winchester D, Lyon AR, Omerovic E, Bax JJ, Meimoun P, Tarantini G, Rihal C, Y-Hassan S, Migliore F, Horowitz JD, Shimokawa H, Lüscher TF, Templin C. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Eur Heart J. 2018;39:2032-2046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 641] [Cited by in RCA: 1020] [Article Influence: 170.0] [Reference Citation Analysis (0)] |
| 17. | Khalighi K, Farooq MU, Aung TT, Oo S. Takotsubo Cardiomyopathy: A Long Term Follow-up Shows Benefit with Risk Factor Reduction. J Cardiovasc Dev Dis. 2015;2:273-281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Dawson DK. Acute stress-induced (takotsubo) cardiomyopathy. Heart. 2018;104:96-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 74] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 19. | Komamura K, Fukui M, Iwasaku T, Hirotani S, Masuyama T. Takotsubo cardiomyopathy: Pathophysiology, diagnosis and treatment. World J Cardiol. 2014;6:602-609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 171] [Article Influence: 15.5] [Reference Citation Analysis (3)] |
| 20. | Amin HZ, Amin LZ, Pradipta A. Takotsubo Cardiomyopathy: A Brief Review. J Med Life. 2020;13:3-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 84] [Reference Citation Analysis (0)] |
| 21. | Banerjee S. Inverted Takotsubo cardiomyopathy: A rare entity often missed! Indian Heart J. 2016;68 Suppl 1:S8-S9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Champion S. Takotsubo Cardiomyopathy related to Pheochromocytoma or Other Etiology Should Be Considered as Similar. Korean Circ J. 2015;45:535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Choi SY, Cho KI, Han YJ, You GI, Kim JH, Heo JH, Kim HS, Cha TJ, Lee JW. Impact of Pheochromocytoma on Left Ventricular Hypertrophy and QTc Prolongation: Comparison with Takotsubo Cardiomyopathy. Korean Circ J. 2014;44:89-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Y-Hassan S. Clinical Features and Outcome of Pheochromocytoma-Induced Takotsubo Syndrome: Analysis of 80 Published Cases. Am J Cardiol. 2016;117:1836-1844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 25. | Y-Hassan S, Falhammar H. Pheochromocytoma- and paraganglioma-triggered Takotsubo syndrome. Endocrine. 2019;65:483-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 26. | Pang Y, Gupta G, Jha A, Yue X, Wang H, Huynh TT, Li A, Li L, Baker E, Chew E, Feelders RA, Korpershoek E, Zhuang Z, Yang C, Pacak K. Nonmosaic somatic HIF2A mutations associated with late onset polycythemia-paraganglioma syndrome: Newly recognized subclass of polycythemia-paraganglioma syndrome. Cancer. 2019;125:1258-1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 27. | Därr R, Nambuba J, Del Rivero J, Janssen I, Merino M, Todorovic M, Balint B, Jochmanova I, Prchal JT, Lechan RM, Tischler AS, Popovic V, Miljic D, Adams KT, Prall FR, Ling A, Golomb MR, Ferguson M, Nilubol N, Chen CC, Chew E, Taïeb D, Stratakis CA, Fojo T, Yang C, Kebebew E, Zhuang Z, Pacak K. Novel insights into the polycythemia-paraganglioma-somatostatinoma syndrome. Endocr Relat Cancer. 2016;23:899-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 28. | Percy MJ, Beer PA, Campbell G, Dekker AW, Green AR, Oscier D, Rainey MG, van Wijk R, Wood M, Lappin TR, McMullin MF, Lee FS. Novel exon 12 mutations in the HIF2A gene associated with erythrocytosis. Blood. 2008;111:5400-5402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 98] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 29. | Gardie B, Percy MJ, Hoogewijs D, Chowdhury R, Bento C, Arsenault PR, Richard S, Almeida H, Ewing J, Lambert F, McMullin MF, Schofield CJ, Lee FS. The role of PHD2 mutations in the pathogenesis of erythrocytosis. Hypoxia (Auckl). 2014;2:71-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 30. | Pang Y, Gupta G, Yang C, Wang H, Huynh TT, Abdullaev Z, Pack SD, Percy MJ, Lappin TRJ, Zhuang Z, Pacak K. A novel splicing site IRP1 somatic mutation in a patient with pheochromocytoma and JAK2V617F positive polycythemia vera: a case report. BMC Cancer. 2018;18:286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Wilkinson N, Pantopoulos K. IRP1 regulates erythropoiesis and systemic iron homeostasis by controlling HIF2α mRNA translation. Blood. 2013;122:1658-1668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 105] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 32. | Meyron-Holtz EG, Ghosh MC, Rouault TA. Mammalian tissue oxygen levels modulate iron-regulatory protein activities in vivo. Science. 2004;306:2087-2090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 200] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 33. | Haase VH. Regulation of erythropoiesis by hypoxia-inducible factors. Blood Rev. 2013;27:41-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 520] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 34. | McMullin MF. Idiopathic erythrocytosis: a disappearing entity. Hematology Am Soc Hematol Educ Program. 2009;629-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Gori T. Viscosity, platelet activation, and hematocrit: progress in understanding their relationship with clinical and subclinical vascular disease. Clin Hemorheol Microcirc. 2011;49:37-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Griesshammer M, Kiladjian JJ, Besses C. Thromboembolic events in polycythemia vera. Ann Hematol. 2019;98:1071-1082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 82] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 37. | Martucci VL, Pacak K. Pheochromocytoma and paraganglioma: diagnosis, genetics, management, and treatment. Curr Probl Cancer. 2014;38:7-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 119] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 38. | Mazza A, Armigliato M, Marzola MC, Schiavon L, Montemurro D, Vescovo G, Zuin M, Chondrogiannis S, Ravenni R, Opocher G, Colletti PM, Rubello D. Anti-hypertensive treatment in pheochromocytoma and paraganglioma: current management and therapeutic features. Endocrine. 2014;45:469-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 39. | Pacak K. Preoperative management of the pheochromocytoma patient. J Clin Endocrinol Metab. 2007;92:4069-4079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 340] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 40. | Lowery AJ, Walsh S, McDermott EW, Prichard RS. Molecular and therapeutic advances in the diagnosis and management of malignant pheochromocytomas and paragangliomas. Oncologist. 2013;18:391-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 41. | Gumbs AA, Gagner M. Laparoscopic adrenalectomy. Best Pract Res Clin Endocrinol Metab. 2006;20:483-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 124] [Article Influence: 6.5] [Reference Citation Analysis (0)] |