Published online Feb 6, 2021. doi: 10.12998/wjcc.v9.i4.927
Peer-review started: October 4, 2020
First decision: November 8, 2020
Revised: November 10, 2020
Accepted: December 17, 2020
Article in press: December 17, 2020
Published online: February 6, 2021
Processing time: 112 Days and 11.1 Hours
Brucella infections in the shoulder joint are uncommon, and few have been reported in the literature.
A 26-year-old male was admitted to our hospital with complaint of recurrent pain and limited movement of the right shoulder. The patient reported the pain to have first occurred as an isolated event 6 mo previously and to have reoccurred 5 mo later, when it was accompanied by limited movement of the shoulder. Findings from physical examination and magnetic resonance imaging (referred to as MRI) suggested the diagnosis of subacromial bursitis, and diagnostic paracentesis and arthroscopic debridement were performed. Surprisingly, synovial fluid culture detected brucella, and the finding was confirmed by mass spectrometry of a colony sample. The diagnosis was corrected to brucellosis of the shoulder joint, and antibiotic drug treatment (oral rifampicin and doxycycline) was administrated for 6 wk. The 4-mo postoperative follow-up examination (MRI) yielded normal findings. The 2-year follow-up showed no signs of recurrence.
This rare case of brucellosis infection in shoulder highlights the importance of increasing awareness to help avoid misdiagnosis.
Core Tip: We report our first encounter of a case of brucellosis in the shoulder joint, which was initially misdiagnosed as subacromial bursitis. A 26-year-old male was admitted with recurrent pain and limited movement of the right shoulder. The pain reportedly occurred first 6 mo previously and reoccurred 5 mo later, accompanied by limited movement of the shoulder. Diagnostic paracentesis and arthroscopic debridement were performed. Surprisingly, brucella growth was detected from the synovial fluid and confirmed by colony sample analysis using mass spectrometry. This case report is intended to increase awareness for brucellosis and help avoid future misdiagnoses by orthopedists and physicians.
- Citation: Wang FS, Shahzad K, Zhang WG, Li J, Tian K. Atypical presentation of shoulder brucellosis misdiagnosed as subacromial bursitis: A case report . World J Clin Cases 2021; 9(4): 927-934
- URL: https://www.wjgnet.com/2307-8960/full/v9/i4/927.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i4.927
Brucellosis, a highly contagious zoonosis caused by ingestion of unpasteurized milk or undercooked meat from infected animals, remains an important public health concern worldwide but especially in developing countries[1]. The disease is transmitted to humans through close contact with domestic animals, in addition to the libation of raw dairy products and infected meat from livestock. The annual nationwide incidence of brucellosis in China is reported to range from 0.00 to 1395.84 per 100000, with the mean time from onset of symptoms to treatment being 36.97 d[2,3]. Brucellosis is a systemic infection that can involve any organ or system of the body, and features an usually long incubation period of 1-4 wk[4,5]. Brucellosis itself results in joint pain, limitation of range of motion, limited mobility, and joint effusion; unfortunately, this non-specific clinical profile overlaps with other diseases, leading to misdiagnosis and mis- or delayed treatment. Moreover, the lack of epidemiological history and slow growth rate of Brucella spp. in blood cultures, and presence of asymptomatic as well as chronic infections with atypical symptoms further hinder the ability to achieve a correct diagnosis in a timely manner[6].
Herein, we report a case of brucellosis in a young adult male. The infection presented a long incubation period (6 mo) and lacked diagnostic evidence for infectious disease until after surgical intervention. Ultimately, we considered this case a chronic infection with atypical symptoms, which highlights the difficulties for differential diagnosis of such. This is also our first encounter with a case of brucella infection in the shoulder joint, representing a rare form of brucellosis.
A 26-year-old patient was admitted to our hospital with complaint of recurrent pain and limited movement of the right shoulder.
The patient reported the symptom of pain to have first appeared 6 mo previously and that it self-resolved within 2 wk (without treatment). The patient also reported that the pain reoccurred 1 mo before admission, and described the pain as involving the anterolateral aspect of the shoulder, being accompanied by limited movement of the shoulder joint. In addition, he cited having developed mild cold symptoms 2 wk before admission. He denied any experiences of fever, weight loss, or night sweats.
The patient had unremarkable history of past illness.
The patient had unremarkable personal and familial medical history, including psycho-social history.
Diffuse swelling was found at the lateral side of the shoulder, with subacromial tenderness (+). Visible flexion limitation was noted, with active flexion to 80° and passive flexion to 110°. Abduction and external rotation of the shoulder joint was normal, while internal rotation was limited because of the pain. The patient was classified as Hawkins test (+), Neer’s test (+), Jobe test (-), lift-off test (-), and strength test of the rotator cuff (-). Throughout the physical examination, the patient's body temperature fluctuated within normal range. There were no signs of significant superficial lymphadenopathy.
The patient showed elevated C-reactive protein (CRP) (15.8 mg/L; normal range: 0-8 mg/L). Considering the normal body temperature and no systemic symptoms, the elevated CRP was considered to be related to the transient cold-like symptoms experienced at the 2 wk before admission.
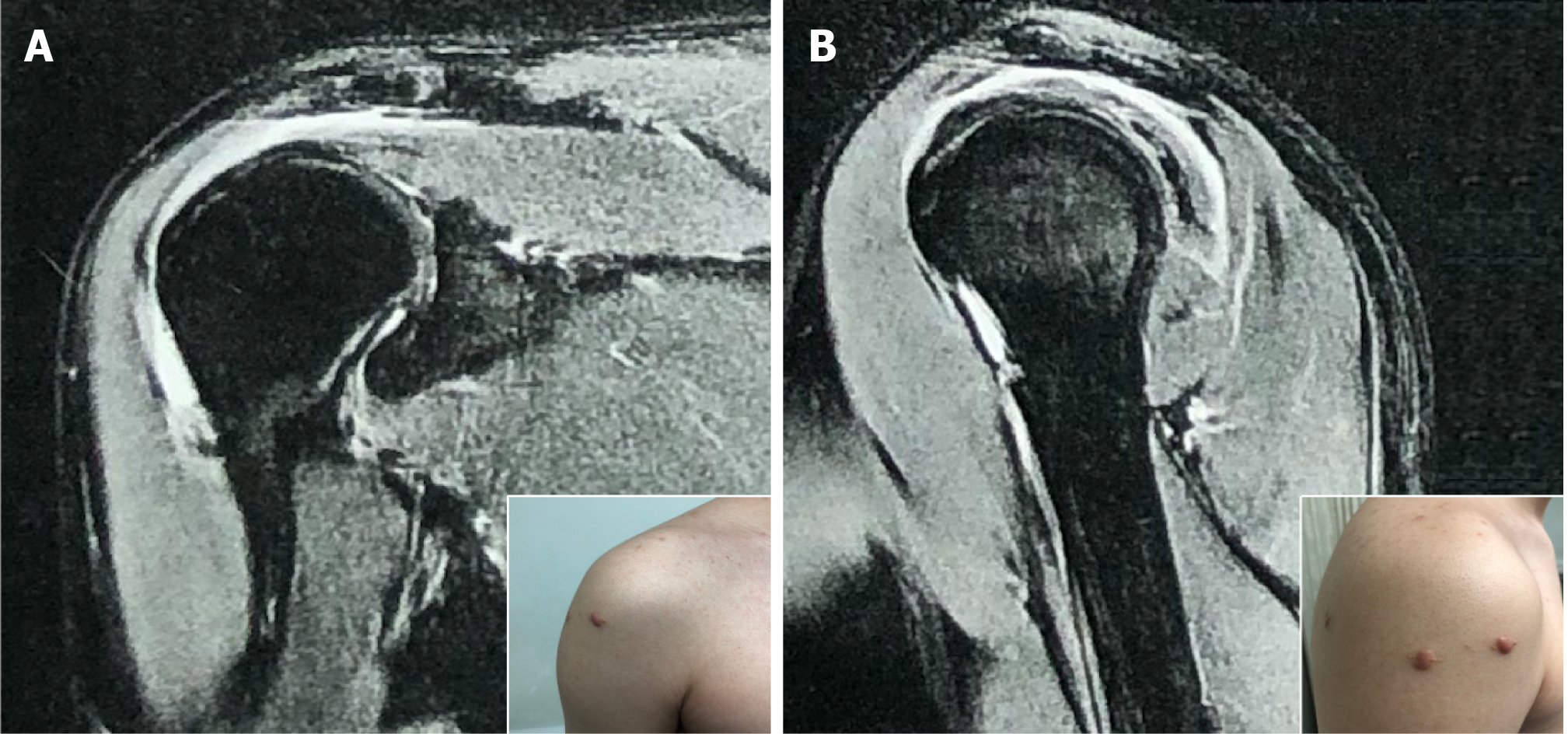
There were no positive findings matching the diffuse swelling of the shoulder observed on X-ray (Figure 1A). Magnetic resonance imaging (MRI) revealed subacromial space (subacromial bursa) effusion with high signal intensity in the coronal T2-weighted images (Figure 1B).
The diagnosis of subacromial bursitis was made according to the findings from physical examination and MRI examination.
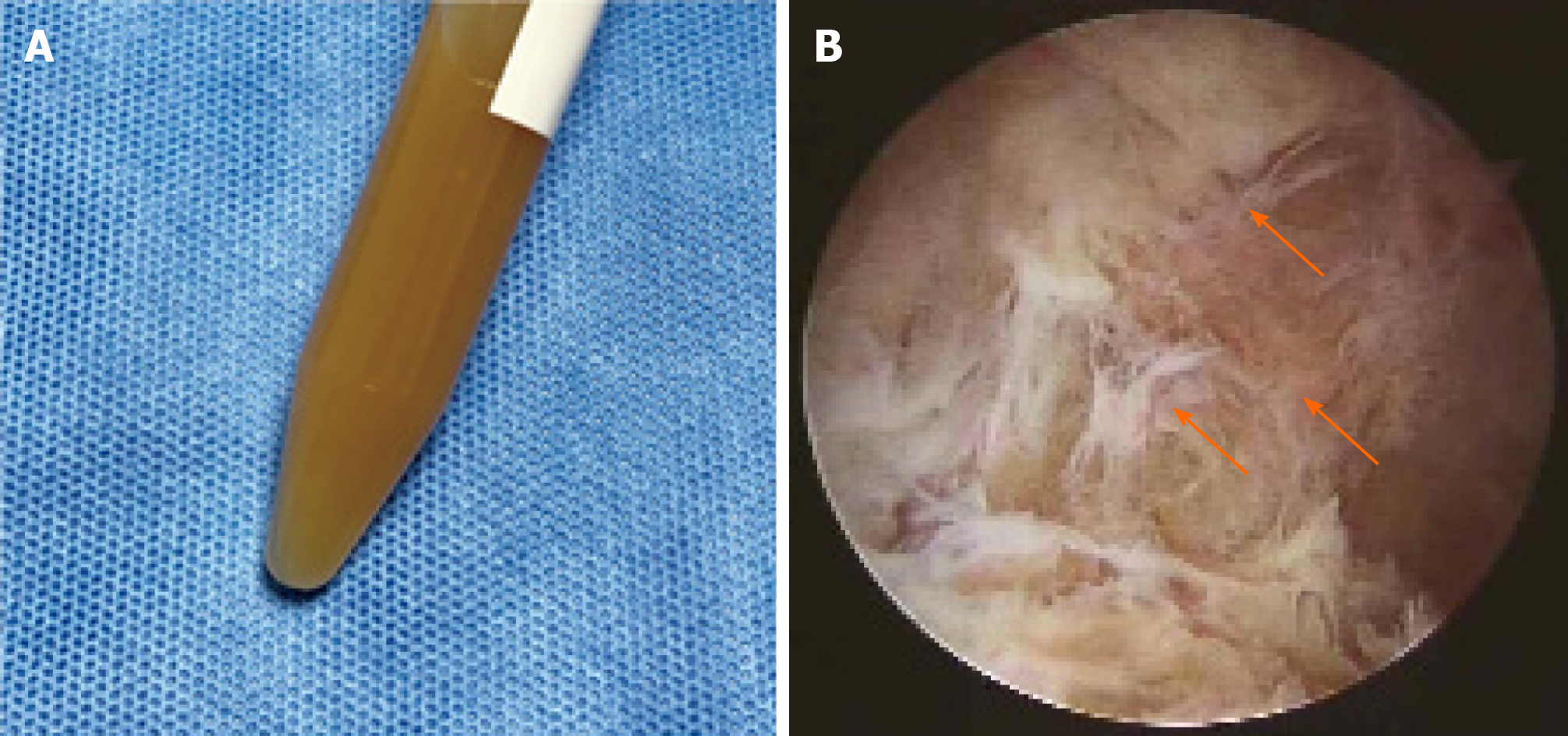
The patient underwent diagnostic paracentesis followed by arthroscopy, and a 15-mL synovial fluid sample was obtained, which appeared as a purulent and turbid fluid (Figure 2A). Microscopic examination and bacterial culture were performed on the sample to rule-out or confirm infection. Considering the possibility of infectious diseases according to the appearance of the extracted effusion from a subacromial bursa, shoulder joint arthroscopic inspection was first performed in an attempt to avoid contamination[7].
The shape of the long head of the biceps tendon and rotator cuff seemed normal under arthroscopic observation, with no sign of hyperplasia around the glenoid labrum or degenerative change of articular cartilage. The subacromial bursa was checked subsequently, using an arthroscope, and hyperemic synovium with fibrinoid necrotic tissue deposition was observed (Figure 2B). After synovial tissue showing severe hyperemic change was collected for histological analysis, arthroscopic debridement was performed.
Surprisingly, culture of the synovial fluid sample produced brucella growth, indicating brucellosis. The diagnosis was confirmed by subsequent mass spectrometry of the culture colonies and positive brucella antibody blood test. The postoperative histopathology report showed fibrous tissue hyperplasia with localized purulent inflammation changes and neutrophil infiltration (Figure 1C).
While tracking the source of infection, it was noted that the patient had consumed raw beef in a rural area 6 mo before the onset of symptoms, which further confirmed our diagnosis.
Brucella infection in the shoulder joint.
The patient’s shoulder pain was significantly relieved following the debridement procedure, without analgesic treatment[7]. However, to address the infection, a 6-wk course of rifampicin (0.75 g qd) combined with doxycycline (0.1 g bid) was initiated.
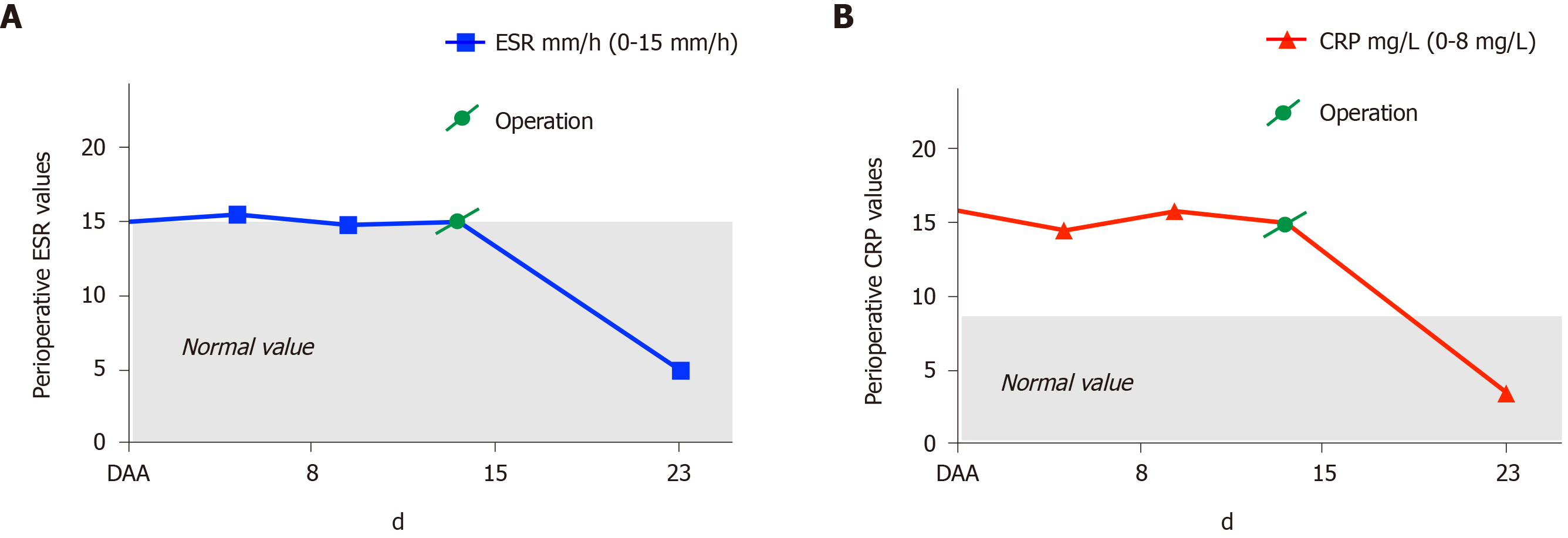
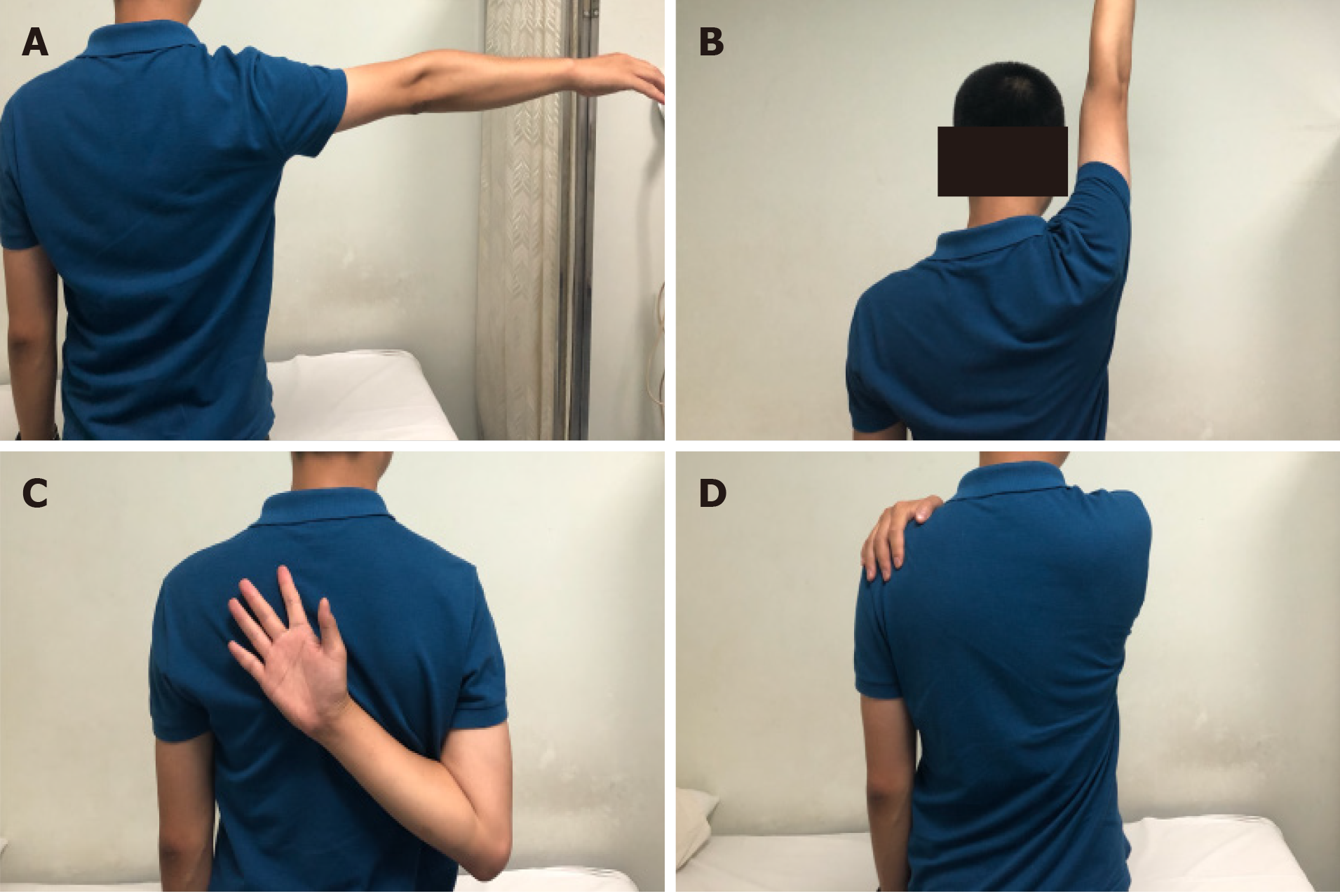
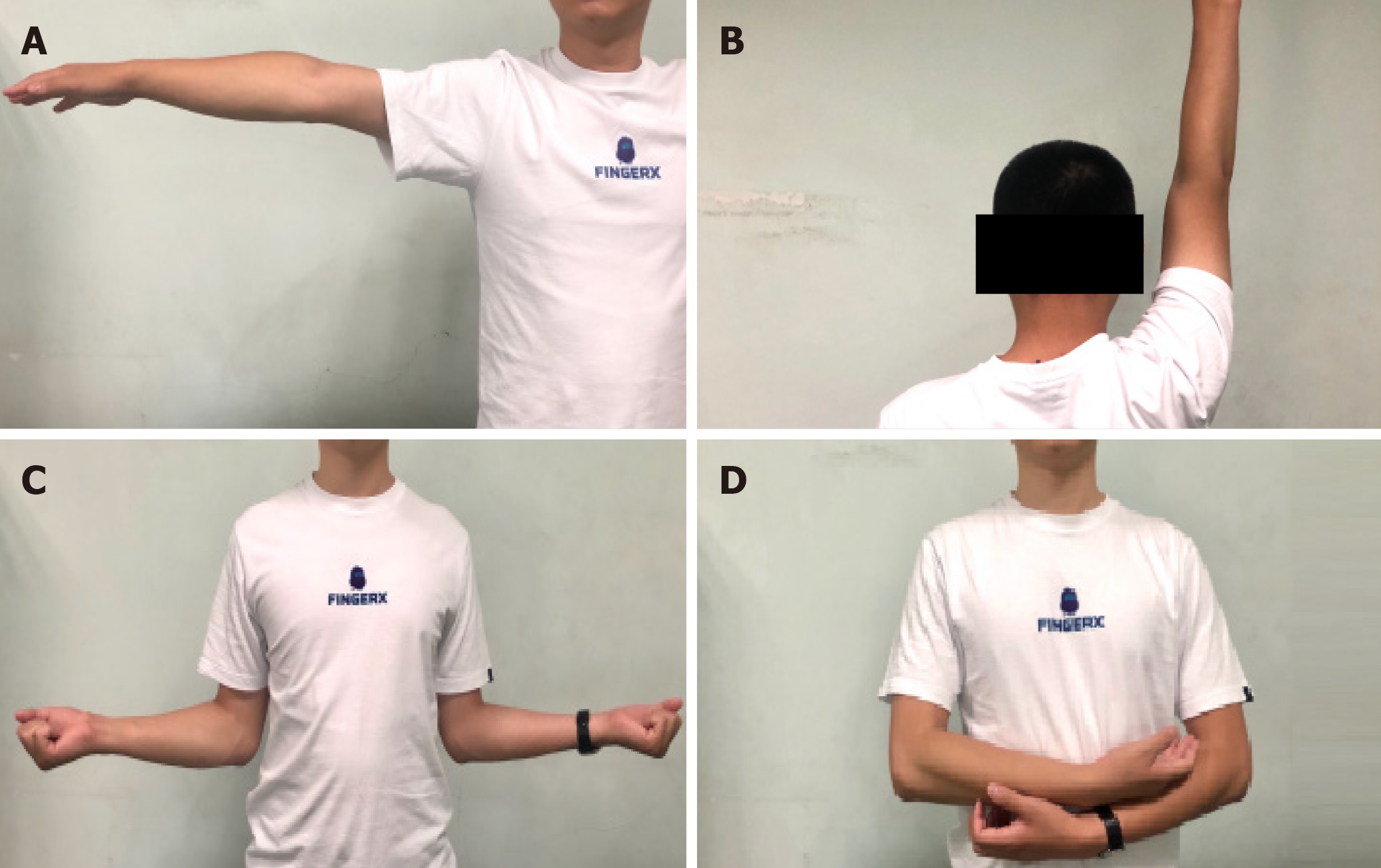
The patient’s CRP and erythrocyte sedimentation rate declined to normal values within 1 wk postoperative (Figure 3). Interestingly, body temperature stayed normal throughout the course of clinical care. Follow-up evaluation by MRI was performed 4 mo after the surgery and showed the effusion of the subacromial bursa to be significantly reduced (Figure 4). Physiotherapy had been carried out at 48 h postoperatively, and the patient’s incisions were completely healed during follow-up (Figure 4). The range of motion of the right shoulder improved gradually and become completely normal at 4-mo postoperative (Figure 5). No recurrence of symptoms occurred during the 2-year follow-up (Figure 6).
The case we report here serves as a reminder that chronic infection caused by Brucella spp. should be included among the considerations for differential diagnoses upon appearance of joint symptoms and dysfunction. These cases usually do not manifest symptoms typical of systemic infection, making them easy to miss or misdiagnose. Diagnostic paracentesis and debridement are the most efficient methods for differential etiological diagnosis of joint diseases and hold the additional benefit of allowing for control of any infectious lesions. In our case, function of the shoulder joint recovered well within 4 mo after the surgery and remained (without recurrence) throughout the 2 years of follow-up.
Brucellosis is a zoonotic infection caused by Brucella spp., an intracellular Gram-negative coccobacilli. Human infections can be transmitted through fluids of infected animals, for example via the consumption of unpasteurized dairy products or from aerosols of infected individuals[8,9]. Brucellosis can cause either an acute febrile illness, after a usual incubation period of 1-4 wk but ranging up to 6 mo, or a chronic infection, which can occur without focus and can affect any organ system[10,11]. The musculoskeletal system and spine are the most common sites of infection, however, and in general there is a wide spectrum of clinical manifestations that may last from several days up to several years[6]. Acute brucellosis presents flu-like symptoms, including fever, night sweats, muscle pain, fatigue and headache[12]. Clinical studies have reported that fever is the most common feature of brucellosis, and more than 30% of patients with brucellosis have positive findings during physical examination of hepatomegaly and splenomegaly. In addition, osteoarticular manifestations can occur, including sacroiliitis and spondylitis, which account for over half of the focal complications. Sixteen percent of patients with brucellosis also have pulmonary complications, including pleural effusions and pneumonias[13]. With non-specific constitutional symptoms, 10% of patients have accompanying symptoms of lymphadenopathy and genitourinary complications, such as orchiepididymitis and glomerulonephritis. Due to these complicated and varying clinical presentations[14,15], brucellosis is easily misdiagnosed as other diseases, with the result of inadequate therapy and prolonged illness that may lead to a high rate of disability.
The comprehensive diagnosis of brucellosis arthritis is mainly based on epidemiological history, clinical symptoms, serology and imaging findings. A final diagnosis of brucellosis requires etiological detection of the Brucella organisms from blood, synovial fluid, or tissue samples. However, the sensitivity of blood and synovial fluid culture varies, with positive cultures ranging from 15%-70%[16]. In addition, a large number of patients present with normal white blood count. This variable clinical profile acts as a reminder for clinicians that, although brucellosis is an infectious disease, it can exist with a normal white blood cell count, and it should not be ruled-out easily at the time of initial diagnosis. A previous study of clinical manifestations and pathogenesis of human brucellosis in China suggested that contact with infected animals (79.4%) and consumption of unsterile animal products (11.5%) are the main causes of brucellosis in non-endemic areas[17]. In our case, the patient had a history of consuming undercooked meat, which is an important clue and supported the diagnosis of brucellosis; although, 6 mo seems a particularly long incubation period for Brucella infection. Symptoms of the patient in our case were not typical; CRP was the only infection/inflammation marker found to be increased prior to surgery, with no significant restriction in joint activity.
Treatment of human brucellosis should involve antibiotics that can penetrate macrophages and act in an acidic intracellular environment[12]. There is also a general need for a combination drug treatment, since all monotherapies are characterized by unacceptably high relapse rates. Previous studies have recommended two regimens, both using doxycycline for a period of 6 wk, in combination with either streptomycin for 2-3 wk or rifampin for 6 wk.
Despite the advances in diagnostic technology, brucellosis remains under-diagnosed and under-reported, especially in developing countries. This case was our first encounter with a brucellosis infection in the subacromial bursa and reminds us to consider the possibility of infectious diseases in differential diagnosis for patients with diffuse swelling of the shoulder. It is necessary for clinicians to consider and recognize brucellosis in patients with atypical clinical manifestations or contact history. We hope that the case we report here will increase awareness for brucellosis and help avoid future misdiagnosis by orthopedists and physicians.
The author would like to thank Dr. Hong Wei, Dr. Nan Jiang, Dr. Yu-Shan Wei and Dr. Jing-Song Wang for their help during the follow-up of the patient.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: China Association of Bone and Joint Disease, Youth commissioners.
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aribas BK S-Editor: Liu M L-Editor: Filipodia P-Editor: Li JH
| 1. | He J, Zhang Q. Hip osteoarticular complication due to delay in diagnosis and treatment of brucellar hip arthritis: two cases report. BMC Infect Dis. 2019;19:412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Ke Y, Zhen Q, Wang Y, Yuan X, Li W, Lu Y, Qiu Y, Yu Y, Huang L, Chen Z. Window of treatment initiation for human brucellosis, implications for treatment efficacy, and prevention of chronic infection. Clin Infect Dis. 2013;56:1350-1352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Wang Y, Zhang W, Ke Y, Zhen Q, Yuan X, Zou W, Li S, Sun Y, Wang Z, Wang D, Cui B, Song H, Huang L, Chen Z. Human brucellosis, a heterogeneously distributed, delayed, and misdiagnosed disease in china. Clin Infect Dis. 2013;56:750-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Young EJ. Brucellosis: current epidemiology, diagnosis, and management. Curr Clin Top Infect Dis. 1995;15:115-128. [PubMed] |
| 5. | Warrender WJ, Syed UAM, Hammoud S, Emper W, Ciccotti MG, Abboud JA, Freedman KB. Pain Management After Outpatient Shoulder Arthroscopy: A Systematic Review of Randomized Controlled Trials. Am J Sports Med. 2017;45:1676-1686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 90] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 6. | Franco MP, Mulder M, Gilman RH, Smits HL. Human brucellosis. Lancet Infect Dis. 2007;7:775-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 606] [Cited by in RCA: 711] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 7. | Lu Y, Zhang Q, Zhu Y, Jiang C. Is radiofrequency treatment effective for shoulder impingement syndrome? J Shoulder Elbow Surg. 2013;22:1488-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Dean AS, Crump L, Greter H, Hattendorf J, Schelling E, Zinsstag J. Clinical manifestations of human brucellosis: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2012;6:e1929. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 350] [Cited by in RCA: 310] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 9. | Pappas G. The changing Brucella ecology: novel reservoirs, new threats. Int J Antimicrob Agents. 2010;36 Suppl 1:S8-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 136] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 10. | Rubach MP, Halliday JE, Cleaveland S, Crump JA. Brucellosis in low-income and middle-income countries. Curr Opin Infect Dis. 2013;26:404-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 149] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 11. | Lewis JM, Folb J, Kalra S, Squire SB, Taegtmeyer M, Beeching NJ. Brucella melitensis prosthetic joint infection in a traveller returning to the UK from Thailand: Case report and review of the literature. Travel Med Infect Dis. 2016;14:444-450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Pappas G, Akritidis N, Bosilkovski M, Tsianos E. Brucellosis. N Engl J Med. 2005;352:2325-2336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 878] [Cited by in RCA: 880] [Article Influence: 44.0] [Reference Citation Analysis (0)] |
| 13. | Kerem E, Diav O, Navon P, Branski D. Pleural fluid characteristics in pulmonary brucellosis. Thorax. 1994;49:89-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Buzgan T, Karahocagil MK, Irmak H, Baran AI, Karsen H, Evirgen O, Akdeniz H. Clinical manifestations and complications in 1028 cases of brucellosis: a retrospective evaluation and review of the literature. Int J Infect Dis. 2010;14:e469-e478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 321] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 15. | Ebrahimpour S, Bayani M, Moulana Z, Hasanjani Roushan MR. Skeletal complications of brucellosis: A study of 464 cases in Babol, Iran. Caspian J Intern Med. 2017;8:44-48. [PubMed] |
| 16. | Memish Z, Mah MW, Al Mahmoud S, Al Shaalan M, Khan MY. Brucella bacteraemia: clinical and laboratory observations in 160 patients. J Infect. 2000;40:59-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 140] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 17. | Zheng R, Xie S, Lu X, Sun L, Zhou Y, Zhang Y, Wang K. A Systematic Review and Meta-Analysis of Epidemiology and Clinical Manifestations of Human Brucellosis in China. Biomed Res Int. 2018;2018:5712920. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 123] [Article Influence: 17.6] [Reference Citation Analysis (0)] |