Published online Feb 6, 2021. doi: 10.12998/wjcc.v9.i4.904
Peer-review started: September 16, 2020
First decision: November 13, 2020
Revised: December 1, 2020
Accepted: December 10, 2020
Article in press: December 10, 2020
Published online: February 6, 2021
Processing time: 131 Days and 1.4 Hours
Acute pancreatitis (AP) is a common critical disease of the digestive system that is often associated with multiple complications. Vascular complications are relatively rare and are one of the causes of death. AP complicated with pulmonary embolism (PE) is even rarer, and there are no reports of AP complicated with PE in elderly patients.
We describe a rare case of AP complicated with PE and review the literature. A 68-year-old woman was diagnosed with AP due to widespread abdominal pain. During the course of treatment, the patient had shortness of breath and progressively worsening dyspnea without chest pain or hemoptysis with a progressive increase in D-dimer and fibrin degradation product. Respiratory failure and right heart failure occurred, and refractory hypoxemia remained after mechanical ventilation. Plain chest computed tomography revealed a small amount of left pleural effusion and external pressure atelectasis in the lower lobe of the left lung but no findings that could lead to refractory hypoxemia. Color Doppler ultrasound indicated pulmonary hypertension and extensive venous thrombosis in the lower extremities. Chest computed tomography angiography finally suggested pulmonary thromboembolism. The patient’s dyspnea symptoms disappeared after anticoagulation treatment.
During the diagnosis and treatment of AP, it is necessary to dynamically monitor D-dimer and consider PE.
Core Tip: Acute pancreatitis complicated with pulmonary embolism (PE) is very rare, and the mortality rate is extremely high if not detected in time. PE often coexists with other complications that can affect respiratory function and is easily missed and misdiagnosed. This report describes the first case of acute pancreatitis complicated by PE in an elderly patient. Clinicians should be reminded that it is important to dynamically monitor blood coagulation indicators such as D-dimer during the diagnosis and treatment of acute pancreatitis and to be alert to the occurrence of deep vein thrombosis and PE to reduce missed diagnosis and misdiagnosis.
- Citation: Fu XL, Liu FK, Li MD, Wu CX. Acute pancreatitis with pulmonary embolism: A case report. World J Clin Cases 2021; 9(4): 904-911
- URL: https://www.wjgnet.com/2307-8960/full/v9/i4/904.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i4.904
Acute pancreatitis (AP) is an acute inflammatory process characterized by pancreatic edema, hemorrhage, and necrosis caused by the self-digestion of pancreatic tissue due to various etiologies, which can trigger a systemic inflammatory response[1]. Pulmonary thromboembolism (PTE) is the most common type of pulmonary embolism (PE), accounting for approximately 80% of PE[2]. The thrombus causing PTE mainly stems from deep vein thrombosis (DVT)[2]. Venous thrombosis is a rare complication of AP[3]. The most common sites are the splenic vein (70%), portal vein, and superior mesenteric vein, and thrombosis in other blood vessels is rare[4]. AP complicated by PTE is rarely reported. It is currently believed to be mainly caused by systemic inflammation and blood hypercoagulability. The case fatality rate of undiagnosed patients with PE is as high as 20%-30%, while the case fatality rate of PE patients who are diagnosed and treated in time can be reduced to 2%-8%[5]. Therefore, physicians need to be highly vigilant with respect to the occurrence of this disease. To our knowledge, only six young and middle-aged patients with AP and PE have been reported in the English literature, and there are no reports of this complication in elderly patients. Here we describe the first case of AP complicated with PE in an elderly patient and review the relevant English literature.
A 68-year-old woman was admitted to the hospital with a chief complaint of persistent pain throughout the abdomen for 3 d.
The patient suffered from persistent pain throughout the abdomen for 3 d, especially in the upper and middle abdomen, accompanied by vomiting and diarrhea without fever, shortness of breath, edema, pain in the lower extremities, and other discomfort. She was diagnosed with AP in a local hospital. The patient gradually developed shortness of breath and difficulty in breathing during treatment of AP.
The patient had a history of hypertension for more than 10 years and diabetes for more than 6 years.
The patient denied a history of smoking, tuberculosis, and alcohol or drug use. No family members had similar diseases.
On admission (day 4 of onset), the patient’s vital signs were recorded as follows: blood pressure was 189/108 mmHg, respiratory rate was 21 breaths/min, pulse rate was 117 bpm, and SPO2 was 93%, with epigastric tenderness on deep palpation. Slightly rapid breathing and lower lung breath sounds were observed, and a small amount of wet rales were heard. The entire abdomen was tender with no rebound pain and no edema in either lower limb.
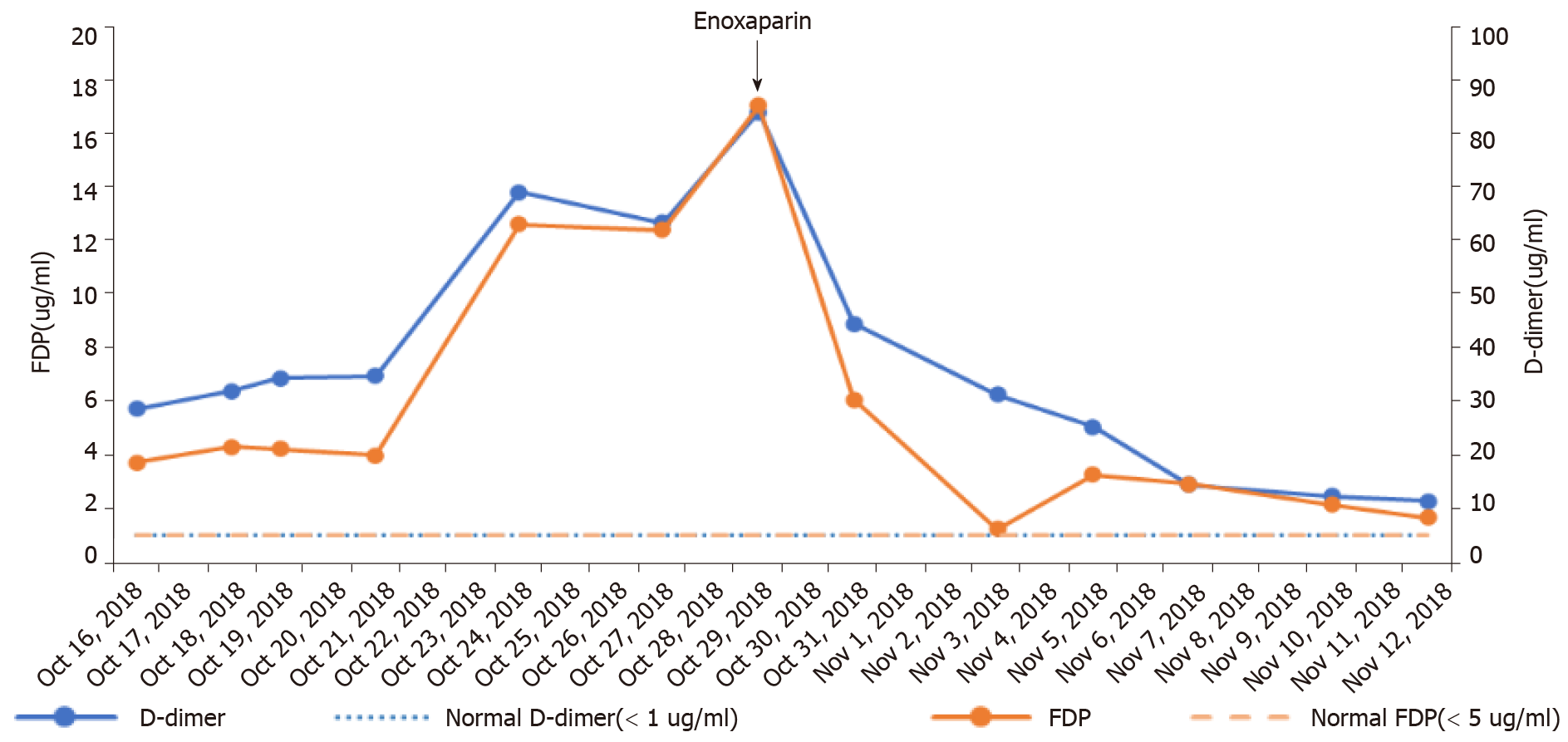
After admission (day 4 of onset), plasma amylase and lipase were elevated to 956 U/L and 796 U/L, respectively. Blood lipids were normal. The levels of D-dimer and fibrin degradation product (FDP) were 5.73 mg/L and 18.7 mg/L, respectively. The white blood cell count and neutrophil ratio were 22.95 × 109/L and 87.1%, respectively, and high-sensitivity C-reactive protein was 233.06 mg/L. After treatment, D-dimer and FDP levels gradually increased (Figure 1). On the 16th d of onset, B-type natriuretic peptide was 983.6 pg/mL, and high-sensitivity troponin T was 0.159 μg/L. Both D-dimer and FDP increased to 12.69 mg/L and 62.06 mg/L, respectively. Enoxaparin was administered for anticoagulation. The patient’s dyspnea gradually eased, D-dimer and FDP levels gradually decreased, and blood pressure returned to normal.
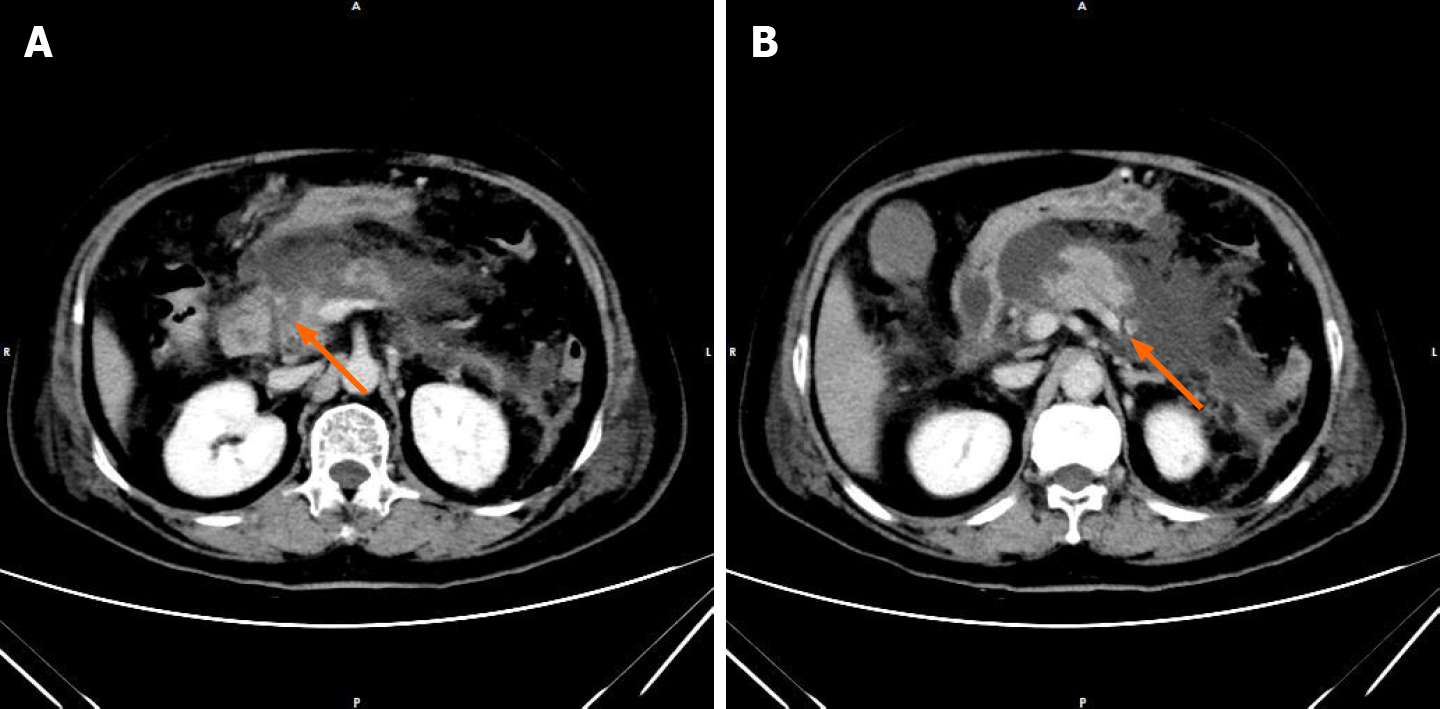
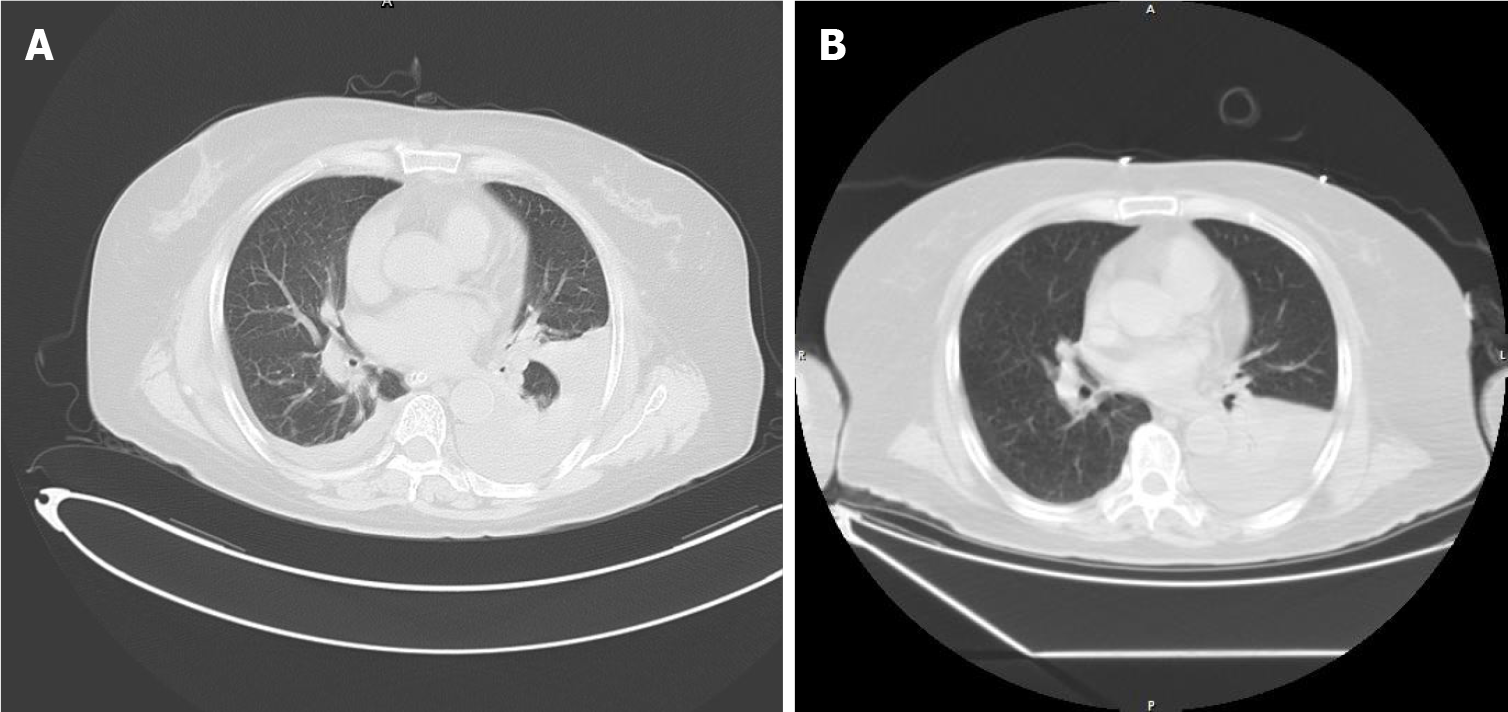
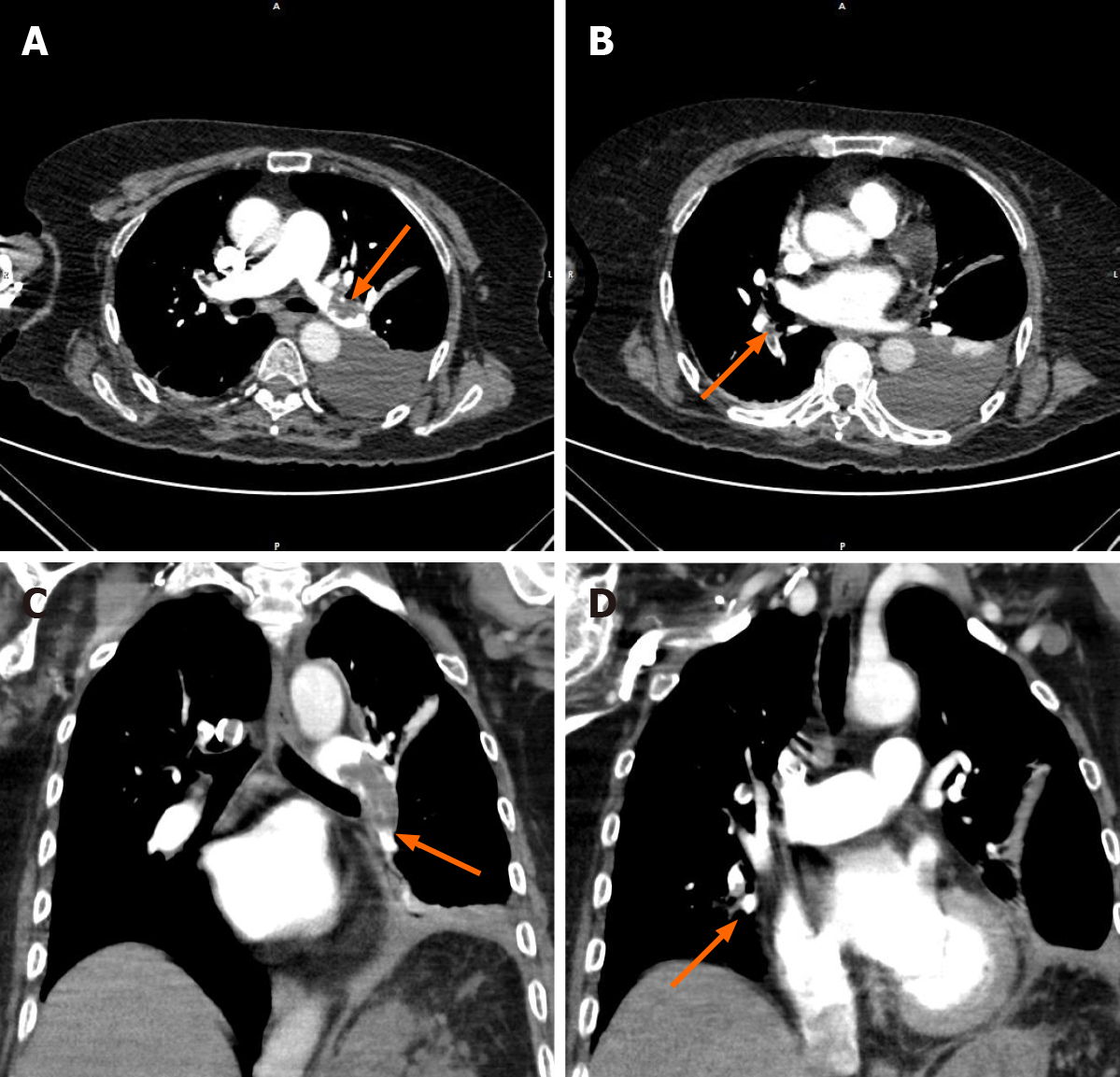
After admission (day 4 of onset), an abdominal computed tomography (CT) scan revealed severe necrosis of the head and body of the pancreas (Figure 2). Abdominal color Doppler ultrasound showed silt-like deposits in the gallbladder and fluid in the gallbladder. The patient was diagnosed with acute necrotizing pancreatitis. Chest CT (Figure 3) on the 5th d after admission showed a small amount of inflammation in both lungs and a small amount of pleural effusion on both sides. After treatment, re-examination by the chest CT scan showed that pleural effusion had gradually reduced, but the patient developed progressively worsening dyspnea. On the 16th d of onset, the patient developed extreme dyspnea and respiratory failure and was treated with mechanical ventilation with tracheal intubation. Her electrocardiogram showed no myocardial infarction or atrial fibrillation. Heart color Doppler ultrasound indicated pulmonary hypertension (pulmonary artery systolic pressure was approximately 30 mmHg), and ejection fraction was 60%. Chest CT revealed a small amount of pleural effusion on the left side with atelectasis of the left lower lobe. Color Doppler ultrasound of the lower limbs showed thrombosis in the common femoral vein and bilateral posterior tibial veins on the right, and thrombosis in the saphenous vein on the left. On the 24th d of onset, chest CT angiography (Figure 4) showed PE in the left main pulmonary artery and multiple branches of the left and right pulmonary arteries.
The patient was eventually diagnosed with acute necrotizing pancreatitis, PE, lung infection, acute respiratory failure, acute right heart failure, venous thrombosis of the lower extremities, hypertension, and type 2 diabetes.
The patient received the following treatments: Inhibition of pancreatic secretion, anti-infective agents, mechanical ventilation, blood pressure stabilization, anticoagulation, and parenteral nutrition. The patient was positive for fecal occult blood, and the possibility of gastrointestinal bleeding was considered. Thus, thrombolysis was not given, and she received only enoxaparin and warfarin for anticoagulation.
After treatment, dyspnea gradually improved, and hemodynamics returned to normal. Laboratory values showed a downward trend, pleural effusion decreased significantly, and abdominal pain and edema of both lower limbs resolved. The patient was followed up for 3 mo and showed no discomfort such as shortness of breath or dyspnea during this period.
Any factors that can cause venous blood flow stasis, vascular endothelial damage, and blood hypercoagulability can lead to venous thrombosis[6]. Estimates derived from epidemiological data show that the rate of incidental PE in the course of symptomatic deep vein thrombosis is between 35.0% and 66.0%[7]. It was found that 81.7% of patients with acute PE had lower-extremity deep vein thrombosis[7]. AP complicated by PE is very rare, and the pathogenesis is still unclear. The underlying mechanism is currently believed to be as follows[8-10]: The cyst connected to the pancreatic duct penetrates into the blood vessel and releases pancreatic juice, which damages the vascular endothelium. This causes the release of procoagulant substances and the activation of platelets, causing the blood to be in a hypercoagulable state. Systemic inflammatory response syndrome is often present during AP. Various inflammatory mediators can damage the vascular endothelium, which consequently trigger the endothelium-dependent acetylcholine relaxation reaction. Blood hypercoagulability is also considered to be the result of liver dysfunction, hypertrypsinemia, and cachexia. However, one study reported that the main causes of AP complicated by venous thrombosis were cell infiltration, edema, and inflammation of the venous endothelium rather than blood hypercoagulability[11]. In addition, patients may also have a variety of risk factors for venous thrombosis.
Our patient was an elderly woman who was diagnosed with acute necrotizing pancreatitis and severe pancreatitis with severe pancreatic necrosis and accumulation of peripancreatic fluid but no pseudocyst. The patient had no previous thrombotic diseases or lower limb venous thrombosis-related symptoms, and no history of blood disease, recent surgery, or trauma. Examinations revealed normal blood lipids, normal platelet count and red blood cell count, normal fibrinogen, and no evidence of atrial fibrillation on electrocardiogram. Predisposing factors for venous thrombosis include possible hypercoagulability of blood, systemic inflammatory response syndrome, administration of drugs that damage the vascular intima (such as long-term parenteral nutrition), long-term bed rest (16 d in bed), older age, high blood pressure, and type 2 diabetes. In addition, studies have shown that patients with severe acute necrotizing pancreatitis are more prone to venous thrombotic complications[12]. We hypothesize that PTE and the formation of venous thrombosis in the lower extremities are caused by the combination of severe systemic response syndrome, vascular damage, and possible hypercoagulability of blood caused by pancreatic juice entering the blood vessels and the patient’s own various venous thrombosis factors.
The clinical manifestations of PE mainly depend on the size and number of emboli, the rate of embolism, location of the embolism, and the patient’s cardiopulmonary function. The manifestations are varied and include shortness of breath, dyspnea, chest pain, syncope, cough, hemoptysis and other symptoms. Lack of specificity and small thromboses have no obvious symptoms and are easily missed or mis-diagnosed[13]. This patient showed shortness of breath in the early stage without chest pain and hemoptysis. We believed that the shortness of breath was caused by pleural effusion, lung infection, and atelectasis. During the course of the disease, the patient gradually developed progressively worsening dyspnea, and progressively increased D-dimer and FDP levels. Chest CT scan did not reveal manifestations of acute respiratory distress syndrome, extensive lung consolidation and infection, or large pleural effusion, which did not explain the cause of the patient’s respiratory failure. Therefore, we suspected that the patient may have PTE. Patients with AP often have pleural effusion and abdominal effusion, pulmonary effusion or infection, and even acute respiratory distress syndrome, leading to shortness of breath and dyspnea. The patient’s dyspnea may be caused by a single complication or a combination of multiple complications. In addition, because AP with PE is rare, it is easily missed or misdiagnosed.
When PTE is suspected, the risk of venous thrombosis should be assessed, and the detection of related coagulation indicators such as D-dimer, pulmonary artery pressure assessment, and pulmonary angiography should be completed to make the diagnosis as soon as possible[14,15]. D-dimer is a specific degradation product produced by plasmin hydrolysis of cross-linked fibrin. D-dimer increases in thrombotic diseases, infections, trauma, surgery, tumors, etc. The diagnostic sensitivity for acute PTE is 92%-100%, which makes it an important indicator to exclude the possibility of acute PTE[16]. FPD, fibrinogen, and other indicators can also be used to detect the formation of thrombus. In the present case, only D-dimer and FPD increased during the course of the disease, and there were no significant changes in other coagulation-related indicators. In addition, troponin, brain natriuretic peptide, or N-terminal prohormone of brain natriuretic peptide, and electrocardiography are also important auxiliary examination methods for acute PE. Once the diagnosis of PTE is confirmed, anticoagulant therapy should be started as soon as possible, and thrombolytic therapy should be performed if necessary.
As AP complicated by PE is extremely rare, we collected and compiled six cases of AP complicated by PE reported in the English literature (Table 1). These patients were all young, aged 21 to 38 years, and the male/female ratio was 1:1. We present the first elderly patient diagnosed with AP complicated by PE. Five of these six patients had shortness of breath and dyspnea. Our patient also had shortness of breath and dyspnea as the main manifestations. Three patients had venous thrombosis in other areas, while our patient had extensive venous thrombosis in the lower extremities during hospitalization. Only two cases had symptoms of venous embolism in the lower extremities manifested as edema. Our patient had symmetrical edema of both lower extremities, which may have been caused by hypoproteinemia and right heart failure, and the possibility of venous thrombosis in the lower extremities cannot be excluded. D-dimer level was more than 500 μg/L in these patients. In our case, her D-dimer level exceeded 1000 μg/L. It can be seen that in patients with AP and PE, shortness of breath or dyspnea is the main symptom, which may or may not be accompanied by thrombosis in other parts of the body. In addition, a significant increase in D-dimer has important implications for venous thrombosis and PE. Therefore, it is essential to monitor the changes in D-dimer levels.
| Ref. | Year | Age/sex | Clinical symptoms | Predisposing factors | External pulmonary vein thrombosis | Imaging performance | D-dimer | Outcome |
| Deiss et al[17] | 2014 | 28/F | Abdominal pain, nausea, vomiting, abdominal distension | NA | NA | Multiple pulmonary emboli in bilateral lower lobes, a right-sided pleural effusion, and lower lobe consolidation, ascites | NA | Cure |
| Deiss et al[17] | 2014 | 32/M | Abdominal pain, nausea, vomiting, nonbloody diarrhea, abdominal distension, dyspnea, hemoptysis, fever | NA | NA | Bilateral pulmonary emboli, pleural effusions, and ascites | NA | Cure |
| Deiss et al[17] | 2014 | 21/F | Chest tightness, shortness of breath, mid-back and abdominal soreness | Medical history of craniotomy 1 wk prior, oral contraceptives | NA | Pulmonary embolism in the right lower lobe | 911 µg/L | Cure |
| Herath et al[18] | 2016 | 38/M | Upper abdominal pain, bloating, vomiting, edema of both ankles | No | DVT | Pulmonary embolism of the right lower lobe, pulmonary artery, and segmental branches of the left pulmonary artery. Pseudocyst of pancreatic head compressed inferior vena cava. Gross ascites and minimal pleural effusion | 1430 µg/L | Cure |
| Zhang et al[19] | 2012 | 38/F | Abdominal pain, vomiting, cough and expectoration with a little blood, progressive dyspnea | NA | No celiac and pelvic vein thrombosis or proximal leg deep venous thrombosis | Pulmonary embolism (both down pulmonary arteries, left pulmonary artery, and branch of right pulmonary artery). Bilateral pleural effusion, lung infection and pulmonary hypertension | More than 500 µg/L | Cure |
| Goenka et al[20] | 1994 | 35/M | Upper abdominal pain, fever, shortness of breath, dyspnea, pain, and swelling of right calf | NA | Inferior vena cava thrombosis | Pulmonary embolism, pancreatic necrosis | NA | Cure |
| Our case | 2020 | 68/F | Abdominal pain, shortness of breath, dyspnea, symmetrical edema of both lower limbs | Hypertension, type 2 diabetes | DVT and superficial vein thrombosis | The left main pulmonary artery and multiple branches of the left and right pulmonary arteries. Low to moderate pleural effusion, lung infection, abdominal effusion, pancreatic necrosis | 16820 µg/L | Cure |
AP complicated with PE is very rare, and the associated mortality rate is extremely high. This case is a reminder for clinicians that in patients with AP, it is necessary to dynamically monitor D-dimer and other coagulation function indices. Clinicians should be aware of the occurrence of PE in order to reduce missed diagnosis and misdiagnosis.
This case report was supported by ward doctors in terms of data acquisition, analysis and interpretation. We would like to thank the patient for permitting disclosure of her medical history.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Inal V, Slomiany BL S-Editor: Huang P L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Crockett S, Falck-Ytter Y, Wani S, Gardner TB. Acute Pancreatitis Guideline. Gastroenterology. 2018;154:1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (2)] |
| 2. | Di Nisio M, van Es N, Büller HR. Deep vein thrombosis and pulmonary embolism. Lancet. 2016;388:3060-3073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 411] [Cited by in RCA: 582] [Article Influence: 64.7] [Reference Citation Analysis (0)] |
| 4. | Patel R, Choksi D, Chaubal A, Pipaliya N, Ingle M, Sawant P. Renal Vein and Inferior Vena Cava Thrombosis: A Rare Extrasplanchnic Complication of Acute Pancreatitis. ACG Case Rep J. 2016;3:e172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 5. | Anderson FA Jr, Wheeler HB, Goldberg RJ, Hosmer DW, Patwardhan NA, Jovanovic B, Forcier A, Dalen JE. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med. 1991;151:933-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 229] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 6. | Wolberg AS, Rosendaal FR, Weitz JI, Jaffer IH, Agnelli G, Baglin T, Mackman N. Venous thrombosis. Nat Rev Dis Primers. 2015;1:15006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 244] [Article Influence: 24.4] [Reference Citation Analysis (1)] |
| 7. | Goldhaber SZ, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012;379:1835-1846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 607] [Cited by in RCA: 686] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 8. | Piercy KT, Ayerdi J, Geary RL, Hansen KJ, Edwards MS. Acute pancreatitis: A complication associated with rheolytic mechanical thrombectomy of deep venous thrombosis. J Vasc Surg. 2006;44:1110-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Camargo EA, Delbin MA, Ferreira T, Landucci EC, Antunes E, Zanesco A. Influence of acute pancreatitis on the in vitro responsiveness of rat mesenteric and pulmonary arteries. BMC Gastroenterol. 2008;8:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Lungarella G, Gardi C, de Santi MM, Luzi P. Pulmonary vascular injury in pancreatitis: evidence for a major role played by pancreatic elastase. Exp Mol Pathol. 1985;42:44-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 11. | Easler J, Muddana V, Furlan A, Dasyam A, Vipperla K, Slivka A, Whitcomb DC, Papachristou GI, Yadav D. Portosplenomesenteric venous thrombosis in patients with acute pancreatitis is associated with pancreatic necrosis and usually has a benign course. Clin Gastroenterol Hepatol. 2014;12:854-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 90] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 12. | Roch AM, Maatman TK, Carr RA, Colgate CL, Ceppa EP, House MG, Lopes J, Nakeeb A, Schmidt CM, Zyromski NJ. Venous Thromboembolism in Necrotizing Pancreatitis: an Underappreciated Risk. J Gastrointest Surg. 2019;23:2430-2438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Le Gal G, Righini M, Mottier D. [Clinical diagnosis of pulmonary embolism: a real challenge]. Rev Med Interne. 2007;28:394-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Raja AS, Greenberg JO, Qaseem A, Denberg TD, Fitterman N, Schuur JD; Clinical Guidelines Committee of the American College of Physicians. Evaluation of Patients With Suspected Acute Pulmonary Embolism: Best Practice Advice From the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med. 2015;163:701-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 214] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 15. | Rivera-Lebron B, McDaniel M, Ahrar K, Alrifai A, Dudzinski DM, Fanola C, Blais D, Janicke D, Melamed R, Mohrien K, Rozycki E, Ross CB, Klein AJ, Rali P, Teman NR, Yarboro L, Ichinose E, Sharma AM, Bartos JA, Elder M, Keeling B, Palevsky H, Naydenov S, Sen P, Amoroso N, Rodriguez-Lopez JM, Davis GA, Rosovsky R, Rosenfield K, Kabrhel C, Horowitz J, Giri JS, Tapson V, Channick R; PERT Consortium. Diagnosis, Treatment and Follow Up of Acute Pulmonary Embolism: Consensus Practice from the PERT Consortium. Clin Appl Thromb Hemost. 2019;25:1076029619853037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 188] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 16. | Patel H, Sun H, Hussain AN, Vakde T. Advances in the Diagnosis of Venous Thromboembolism: A Literature Review. Diagnostics (Basel). 2020;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 17. | Deiss R, Young P, Yeh J, Reicher S. Pulmonary embolism and acute pancreatitis: case series and review. Turk J Gastroenterol. 2014;25:575-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Herath HM, Kulatunga A. Acute pancreatitis complicated with deep vein thrombosis and pulmonary embolism: a case report. J Med Case Rep. 2016;10:182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 19. | Zhang Q, Zhang QX, Tan XP, Wang WZ, He CH, Xu L, Huang XX. Pulmonary embolism with acute pancreatitis: a case report and literature review. World J Gastroenterol. 2012;18:583-586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 20. | Goenka MK, Kochhar R, Gulati M, Singh G, Khanna SK, Mehta SK. Acute pancreatitis complicated by pulmonary thromboembolism secondary to inferior vena caval thrombosis. J Clin Gastroenterol. 1994;19:85-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |