Published online Dec 26, 2021. doi: 10.12998/wjcc.v9.i36.11443
Peer-review started: July 22, 2021
First decision: September 1, 2021
Revised: September 9, 2021
Accepted: November 14, 2021
Article in press: November 14, 2021
Published online: December 26, 2021
Processing time: 154 Days and 8.3 Hours
Arteriovenous fistula of the sigmoid sinus is an abnormal connection of arteries with the sigmoid sinus. Endovascular treatments of such lesions are considered safe and with low rates of complications.
A 62-year-old female patient underwent endovascular treatment of an arteriovenous fistula of the right sigmoid sinus on February 7, 2017, but her tinnitus was not cured. She was admitted to the Beijing Tiantan Hospital, Capital Medical University, on March 20, 2017, and her pre-operative diagnosis, by digital subtraction cerebral angiography, was arteriovenous fistula of the sigmoid sinus. She underwent endovascular embolization of the distal occipital artery and posterior auricular artery using Onyx-18. The arteriovenous fistula of the sigmoid sinus was cured, and her tinnitus disappeared, but ischemia of the upper 2/3 of the right auricle occurred without hearing loss. The patient received treatment to improve microcirculation, in addition to fluid supplementation, analgesia, and hyperbaric oxygen, and the swelling due to ischemia in the right auricle did not progress further. The patient reported no tinnitus , and the right auricle had returned to normal 3 years later.
Ischemic complications of vital organs should be considered when performing embolization procedures for arteriovenous fistulas of cerebral sinuses. Compensation of the organs should be evaluated before the operation, and the related treatment regimens should be planned.
Core Tip: A 62-year-old female patient underwent endovascular treatment of an arteriovenous fistula of the right sigmoid sinus, but her tinnitus was not cured. She was admitted to the Beijing Tiantan Hospital, Capital Medical University, on March 20, 2017. She underwent endovascular embolization of the distal occipital artery and posterior auricular artery using Onyx-18. The arteriovenous fistula of the sigmoid sinus was cured, and her symptoms of tinnitus disappeared, but ischemia of the upper 2/3 auricle of the right auricle occurred without hearing loss. Ischemic complications of vital organs should be considered when performing embolization procedures for arteriovenous fistulas of cerebral sinuses.
- Citation: Li W, Zhang SS, Gao XR, Li YX, Ge HJ. Ear ischemia induced by endovascular therapy for arteriovenous fistula of the sigmoid sinus: A case report. World J Clin Cases 2021; 9(36): 11443-11447
- URL: https://www.wjgnet.com/2307-8960/full/v9/i36/11443.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i36.11443
Dural arteriovenous fistulas (DAVFs) refer to the abnormal connections of the internal carotid artery, external carotid artery (ECA), or vertebral artery branches with sinuses of the dura mater, leading to hemodynamic changes in the sinuses and a higher risk of intracerebral hemorrhage[1-4]. Endovascular therapy is an important method for the treatment for DAVFs. There are many vascular anastomoses in vital organs in the head and facial areas, such as eyes, ears, and nose, and endovascular therapy rarely induces ischemic changes in these organs[5-7]. Here we report a patient with auricle ischemia induced by the embolization of an arteriovenous fistula of the sigmoid sinus through the middle meningeal, occipital, and posterior auricular arteries.
A 62-year-old female patient was admitted to the Neurointerventional Department of Beijing Tiantan Hospital, Capital Medical University, on March 20, 2017, due to 41 d of tinnitus symptoms after a partial embolization of an arteriovenous fistula of the sigmoid sinus through the middle meningeal artery (MMA), without any sign of tinnitus improvement.
The patient reported pulsatile tinnitus in the right ear in June 2016, but without hearing loss.
The patient had no history of head trauma, intracranial infection, nasal sinus infection, or cerebral surgery. As her symptoms did not worsen from June 2016 to February 2017, the patient did not receive specific treatments.
She did not report any personal and family history. The patient was admitted to the Zhuhai People’s Hospital on February 7, 2017, due to pulsatile tinnitus in the right ear.
The patient reported pulsatile tinnitus in the right ear without any other abnormal physical examination.
Her laboratory examinations were normal.
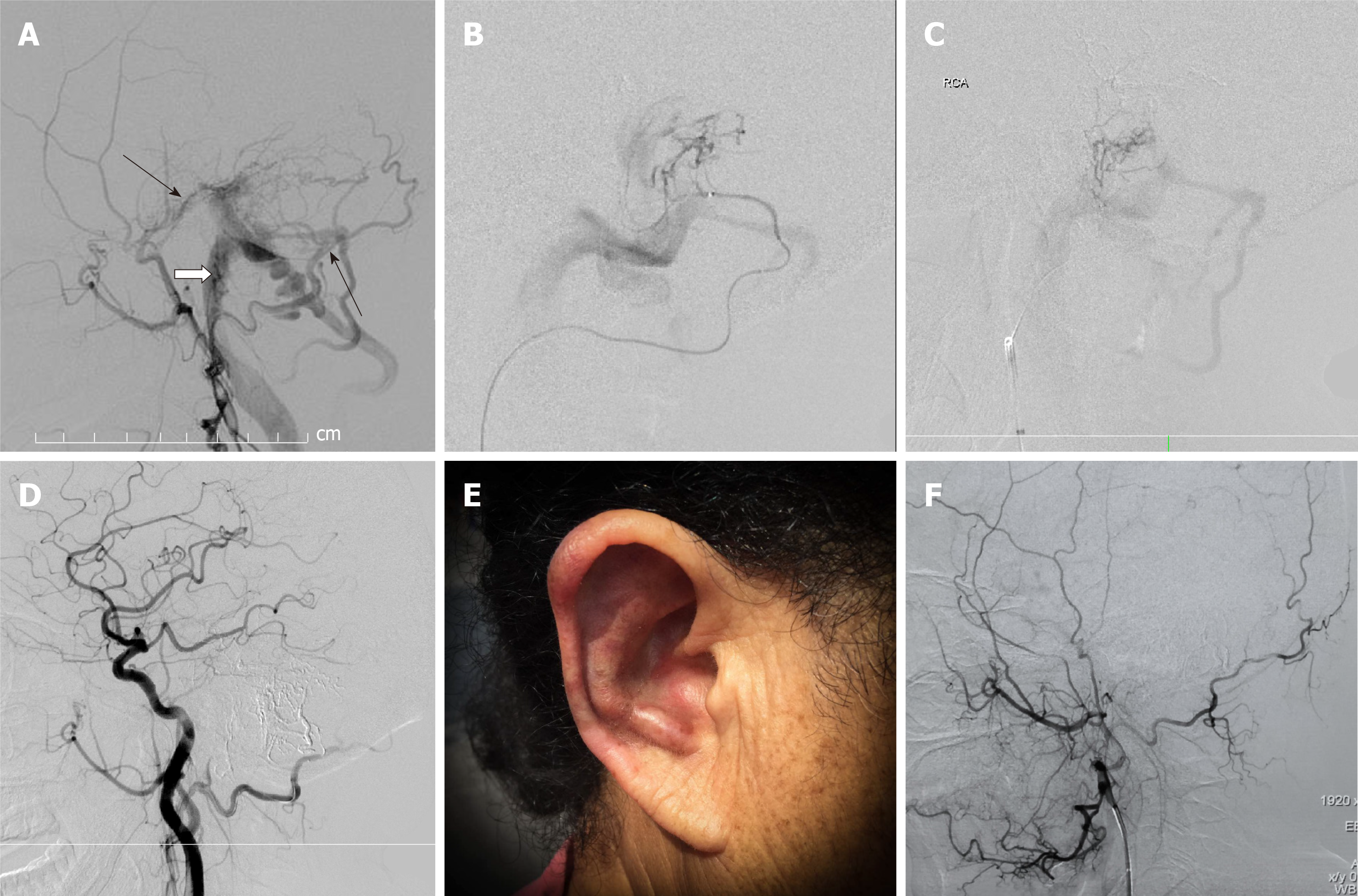
Digital subtraction cerebral angiography (Siemens, Erlangen, Germany) was performed, showing blood flow in the right MMA, right occipital artery (OA), and right posterior auricular artery (PAA) to the right sigmoid sinus, which was classified as Cognard Type-I (Figure 1A). Partial embolization of the arteriovenous fistula of the sigmoid sinus was performed through the MMA at the hospital, but her tinnitus symptoms did not improve after the operation.
Following admission to Beijing Tiantan Hospital, the pre-operative diagnosis, by digital subtraction cerebral angiography, was arteriovenous fistula of the sigmoid sinus. No other treatments were performed before the operation. On March 23, 2017, the patient underwent embolization of the arteriovenous fistula of the sigmoid sinus under general anesthesia. A Marathon micro-catheter (EV3, Plymouth, MN, United States) was inserted into the distal OA to a site close to the fistula, 0.25 mL of dimethyl sulfoxide (DMSO) was injected, and then 0.25 mL of Onyx-18 was injected (Figure 1B). Angiography showed no blood flow from the OA to the sigmoid sinus, but blood flow from the PPA to the sigmoid sinus. A Marathon micro-catheter (EV3, Plymouth, MN, United States) was inserted into the distal PAA to a site close to the fistula, 0.25 mL of DMSO (EV3, Plymouth, MN, United States) was injected, and then 0.25 mL of Onyx-18 was injected (Figure 1C). Angiography showed that the arteriovenous fistula had disappeared after these procedures (Figure 1D). When the patient woke up from anesthesia, her tinnitus symptoms had disappeared. However, she reported pain in the right auricle about 40 min later. Cyanosis and swelling of the upper 2/3 of the right auricle were observed 2 h later, and skin swelling at the occipital area posterior to the ear was also noted (Figure 1E). Hearing in the right ear did not decrease. The patient received treatment to improve microcirculation, in addition to fluid supplementation, analgesia, and hyperbaric oxygen. Swelling of the ischemic right auricle did not progress further. A re-examination using digital subtraction cerebral angiography 3 mo later showed no recurrence of the arteriovenous fistula (Figure 1F), and the cyanosis and swelling in the right auricle had improved. Telephone follow-up 3 years later revealed that the patient had no tinnitus symptoms, and the right auricle had returned to normal.
The final diagnosis of the presented case was arteriovenous fistula of the sigmoid sinus.
The patient underwent endovascular embolization of the distal OA and PAA using Onyx-18 and received treatment to improve microcirculation, in addition to fluid supplementation, analgesia, and hyperbaric oxygen.
The patient reported no tinnitus symptoms, and the right auricle had returned to normal 3 years later.
In the case reported here, tinnitus due to DAVF was effectively managed by embolizing the arteries feeding the DAVF. However, the initial treatment at a local hospital was insufficient as since only one artery was occluded. Embolization of the two other arteries finally resolved the tinnitus, but the patient developed auricle ischemia that required 15 d of management before resolution.
DAVF is a condition caused by the abnormal connection of arteries and veins of the dura mater, mainly at the transverse sinus, sigmoid sinus, and cavernous sinus[8]. The blood supply of a DAVF is mainly from the MMA and meningeal branches of the OA. In addition, the posterior meningeal artery (PMA) and meningo-hypophyseal trunk of the internal carotid artery can also participate in the blood supply in rare cases[9-11]. The PAA, a small branch of the ECA is the major blood supply to the auricle[12]. The PAA originates from an ECA branch above the OA, travels to the space between the parotid gland and belemnoid, and then through the groove between the mastoid process and auricular cartilage[13]. Participation of the PAA in a DAVF is relatively rare but is reported to cause tinnitus[14,15], as in the present case. Although embolization therapy was performed for the MMA and OA, the disease was not cured. Therefore, no other options but the embolization of the PAA was available for this patient.
The arteriovenous fistula disappeared after embolization of the PAA. However, the PAA is responsible for the ear's blood supply, and the blood flow in the auricle is from the PAA and the auricle branch of the superficial temporal artery (STA). The STA is a thick artery but has only limited, fine branches for the auricle's blood supply and mainly provides blood to the upper and lower part and 1/2 of the internal side of the middle part of the anterior auricle. On the other hand, the PAA is finer than the STA and has more and thicker auricle branches that mainly distribute blood to the posterior auricle, the auricle's external margin, and 1/2 of the middle-external part of the anterior auricle. Hence, the PAA is the major blood supply of the posterior auricle, auricular lobule, and 1/2 of the middle-external part of the anterior auricle. There is generally one perforating branch which originates from the lower branch of the PAA that travels through the cartilage of the posterior margin of the external auditory canal to the anterior auricle, and 1-2 marginal branches cross the external margin of the auricle to the anterior auricle, which then comprehensively anastomose with the middle and lower branches of the STA[8]. As there are limited anastomoses at the middle and upper parts of the auricle, over-embolization of the PAA could lead to auricle ischemia symptoms, which has not been previously reported to date. The symptoms in this patient disappeared after treatments. Nevertheless, evaluating the compensations and performing corresponding preventive plans are needed during the embolization of arteries providing blood flow to vital organs in order to prevent serious complications.
We reported a case of DAVF of the sigmoid sinus treated with Onyx-18 embolization of the MMA, OA, and PPA; however, the patient developed auricle ischemia after treatment. When treating DAVF, complications, including occlusion of normal blood vessels, nerve injuries, and intracranial bleeding, should be managed properly. Regarding the blood supply of vital facial organs, especially when the organ's collateral circulation is insufficient, the possible ischemic complications after embolization need to be evaluated thoroughly.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Neurosciences
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ferreira GSA S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Nishijima M, Kuwayama N, Endo S, Takaku A. Clinico-pathological study in patients with transverse-sigmoid sinus dural arteriovenous malformations. J Clin Neurosci. 1998;5 Suppl:42-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Men S, Idiman F, Gulcu A. Reversible cytotoxic edema associated with dural arteriovenous fistula: a case report. Eur J Radiol. 2004;52:1-5. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Caragine LP, Halbach VV, Dowd CF, Ng PP, Higashida RT. Parallel venous channel as the recipient pouch in transverse/sigmoid sinus dural fistulae. Neurosurgery. 2003;53:1261-6; discussion 1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Irie F, Fujimoto S, Uda K, Toyoda K, Hagiwara N, Inoue T, Okada Y. Primary intraventricular hemorrhage from dural arteriovenous fistula. J Neurol Sci. 2003;215:115-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Ertl L, Brückmann H, Kunz M, Crispin A, Fesl G. Endovascular therapy of low- and intermediate-grade intracranial lateral dural arteriovenous fistulas: a detailed analysis of primary success rates, complication rates, and long-term follow-up of different technical approaches. J Neurosurg. 2017;126:360-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Maus V, Drescher F, Goertz L, Weber A, Weber W, Fischer S. Endovascular Treatment of Intracranial Dural Arteriovenous Fistulas: A German Single-Center Experience. Cerebrovasc Dis Extra. 2020;10:84-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Mohr JP, Kejda-Scharler J, Pile-Spellman J. Diagnosis and treatment of arteriovenous malformations. Curr Neurol Neurosci Rep. 2013;13:324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Xu K, Yang X, Li C, Yu J. Current status of endovascular treatment for dural arteriovenous fistula of the transverse-sigmoid sinus: A literature review. Int J Med Sci. 2018;15:1600-1610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Guo Y, Chen H, Chen X, Yu J. Clinical importance of the occipital artery in vascular lesions: A review of the literature. Neuroradiol J. 2019;32:366-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Wang G, Yu J, Hou K, Guo Y. Clinical importance of the posterior meningeal artery: a review of the literature. Neuroradiol J. 2019;32:158-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Yu J, Guo Y, Xu B, Xu K. Clinical importance of the middle meningeal artery: A review of the literature. Int J Med Sci. 2016;13:790-799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | Imanishi N, Nakajima H, Aiso S. Arterial anatomy of the ear. Okajimas Folia Anat Jpn. 1997;73:313-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Standring S. Gray’s Anatomy E-Book: The Anatomical Basis of Clinical Practice. London: Elsevier Health Sciences, 2015: 1519. |
| 14. | Kim S, Byun J, Park M, Lee S. Pulsatile tinnitus with a dural arterio-venous fistula diagnosed by computed tomography-angiography. Korean J Audiol. 2013;17:133-137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Oh SJ, Chon YI, Kong SK, Goh EK. Multiple Dural Arteriovenous Fistulas Presenting as Pulsatile Tinnitus Treated with External Manual Compression. J Audiol Otol. 2017;21:156-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |