Published online Dec 26, 2021. doi: 10.12998/wjcc.v9.i36.11437
Peer-review started: July 15, 2021
First decision: September 28, 2021
Revised: October 8, 2021
Accepted: November 18, 2021
Article in press: November 18, 2021
Published online: December 26, 2021
Processing time: 161 Days and 11.4 Hours
Abdominal pregnancy is a rare type of ectopic pregnancy. We describe here a case of ectopic pregnancy implanted under the surface of the diaphragm, presenting the particular features of imaging findings from ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI).
A 30-year-old woman presented with complaint of intermittent abdominal pain, that had begun 5 d earlier. She had no current or abnormal vaginal bleeding, and her serum human chorionic gonadotropin level (13372.08 IU/L) indicated pregnancy. Vaginal ultrasound showed a mixed echogenic mass in the right ovary. CT (plain) scan showed a curved high density mass beneath the subhepatic space. MRI scan showed a curved mixed signal, with restricted diffusion beneath the subhepatic space. Abdominal ultrasound demonstrated a mixed echogenic mass in the right lobe of the liver near the apex of the diaphragm, with a visible yolk sac and germ cell region with a bud. Subsequent laparoscopy visualized a dark red mass under the right diaphragm, which was resected completely. Histopathological examination of the resected mass confirmed an ectopic pregnancy. The recovery was swift and uneventful, and the patient was discharged to home.
Ectopic pregnancy should be in the differential diagnostic workup (via multiple imaging modalities) of childbearing woman with unexplained abdominal pain.
Core Tip: Diaphragmatic pregnancy is an extremely rare type of ectopic pregnancy and is easily misdiagnosed in practice. Here, we report a 30-year-old woman who experienced 5 d of intermittent abdominal pain, without bleeding, and was diagnosed with ectopic pregnancy implanted under the surface of diaphragm. Inclusion of vaginal and abdominal examinations by various routine imaging modalities (ultrasound, computed tomography and magnetic resonance imaging) will to help improve recognition of the disease and reduce clinical error.
- Citation: Wu QL, Wang XM, Tang D. Ectopic pregnancy implanted under the diaphragm: A rare case report. World J Clin Cases 2021; 9(36): 11437-11442
- URL: https://www.wjgnet.com/2307-8960/full/v9/i36/11437.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i36.11437
Ectopic pregnancy is rare, accounting for only 1.3%-2.4% of all pregnancies[1]. Nearly all ectopic pregnancies (95%) are tubal, with rarer locations of ectopic implantations involving the cervix, ovary and abdominal cavity[2]. We searched the English language literature from 1977 to January 2021 using the MeSH terms “ectopic”, “pregnancy”, and “non-tubal” or “abdominal”, but found only a few reports of ectopic pregnancies implanted under the diaphragm in particular.
Herein, we report a rare case of an ectopic pregnancy implanted under the diaphragm. Findings from ultrasound (US), computed tomography (CT) and magnetic resonance imaging (MRI) were key to the recognition and subsequent treatment of the condition. In the Discussion of this case report, we provide a brief review of the literature on this rare event.
A married, nulliparous, 30-year-old woman presented to our hospital with complaint of intermittent abdominal pain.
The patient reported that the abdominal pain had begun 5 d prior. History-taking revealed normal menstruation and no current or past abnormal vaginal bleeding. The last menstrual period had occurred 13 d before admission.
The patient’s general medical history was unremarkable. Her nulliparous status included neither vaginal nor cesarean delivery. She had no use of an intrauterine device (IUD) and had no history of pelvic inflammatory disease or pelvic surgery.
The patient experienced pressure pain in the upper abdomen.
Serum human chorionic gonadotropin (HCG) concentration was elevated to pregnancy levels (13372.08 IU/L; nonpregnant levels: < 10 mIU/L).
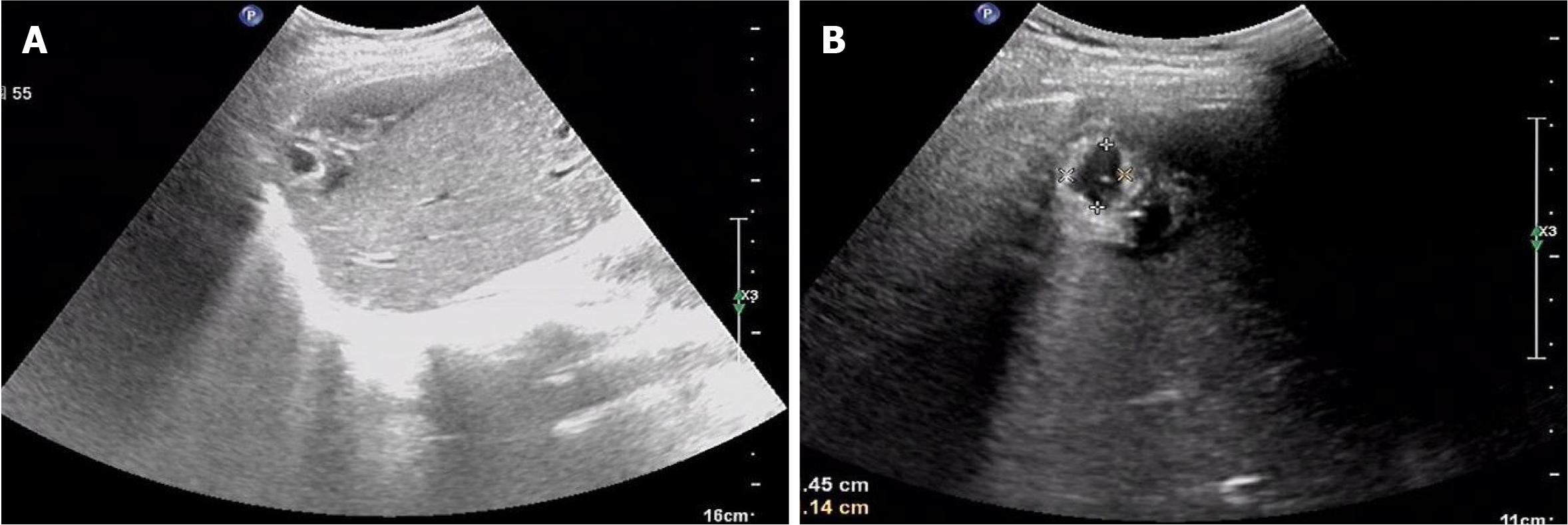
Vaginal US found a mixed echogenic mass in the right ovary. Initially, the finding was considered to represent a corpus luteum, and the possibility of ectopic pregnancy could not be ruled out (Figure 1). In addition, a cystic lesion was found in the right adnexa and pelvic effusion was present.
CT (plain) scan revealed a curved high density mass beneath the subhepatic space, which was interpreted as hemorrhage (Figure 2).
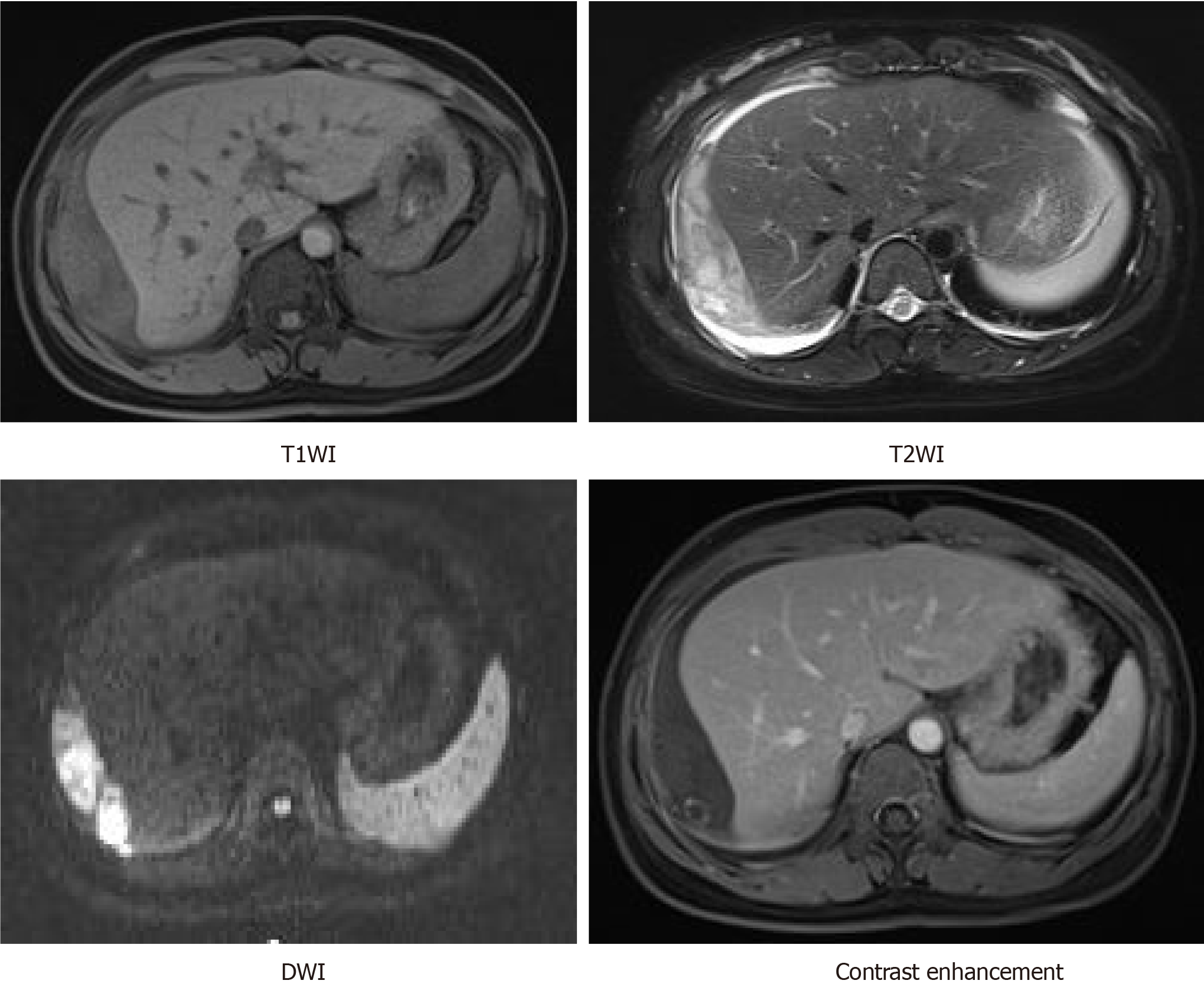
On MRI, a curved mixed signal, mostly low in T1-weighted imaging (WI) and high in T2WI, was observed beneath the subhepatic space. Diffusion-weighted imaging (DWI) showed restricted diffusion. After administration of gadolinium (Gd), a peripheral enhanced nodal was observed within the mixed curved signal (Figure 3). In combination with the HCG laboratory finding, the presence of the nodule could not preclude the possibility of an ectopic gestational sac.
Abdominal US demonstrated a mixed echogenic mass in the right lobe of the liver near the apex of the diaphragm. The mass was approximately 5 cm × 3 cm in size, with a cystic dark area measuring approximately 1.5 cm × 1.1 cm. A yolk sac and germ cell region with a bud of approximately 0.4 cm in length was visible, as was a seemingly primitive heart tube pulsation (Figure 4).
Abdominal ectopic pregnancy.
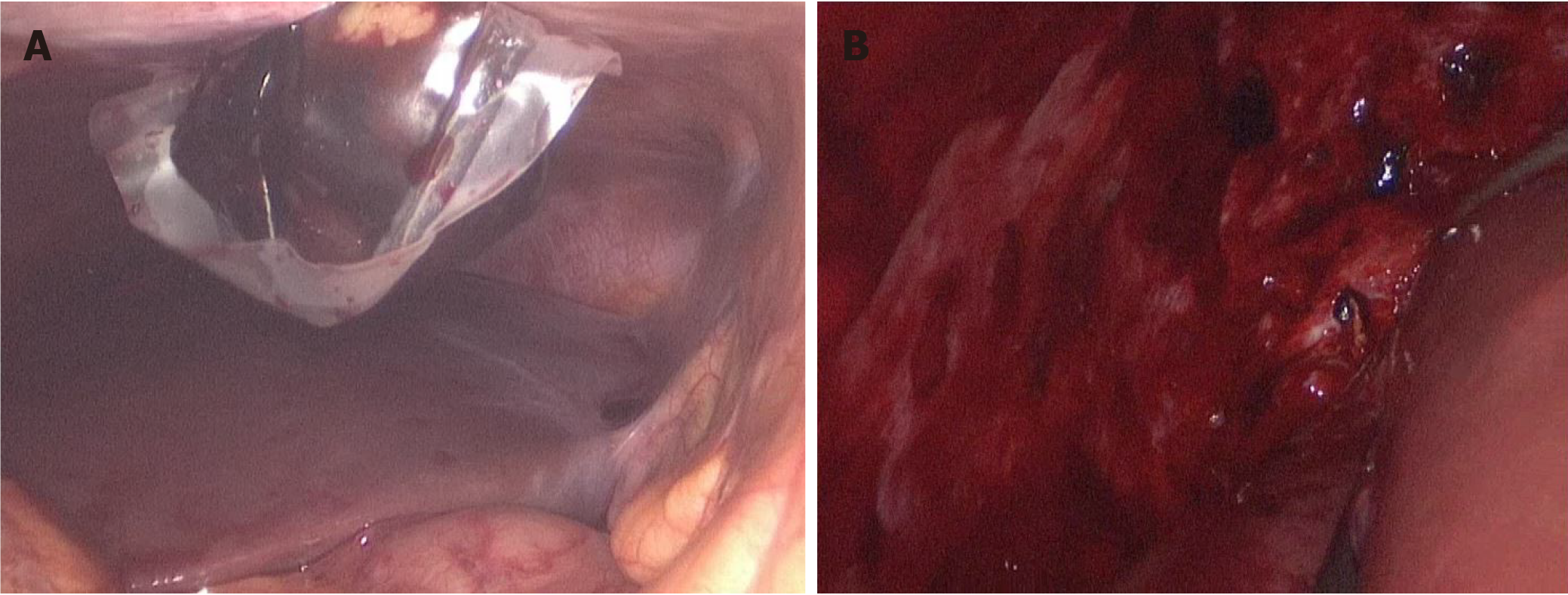
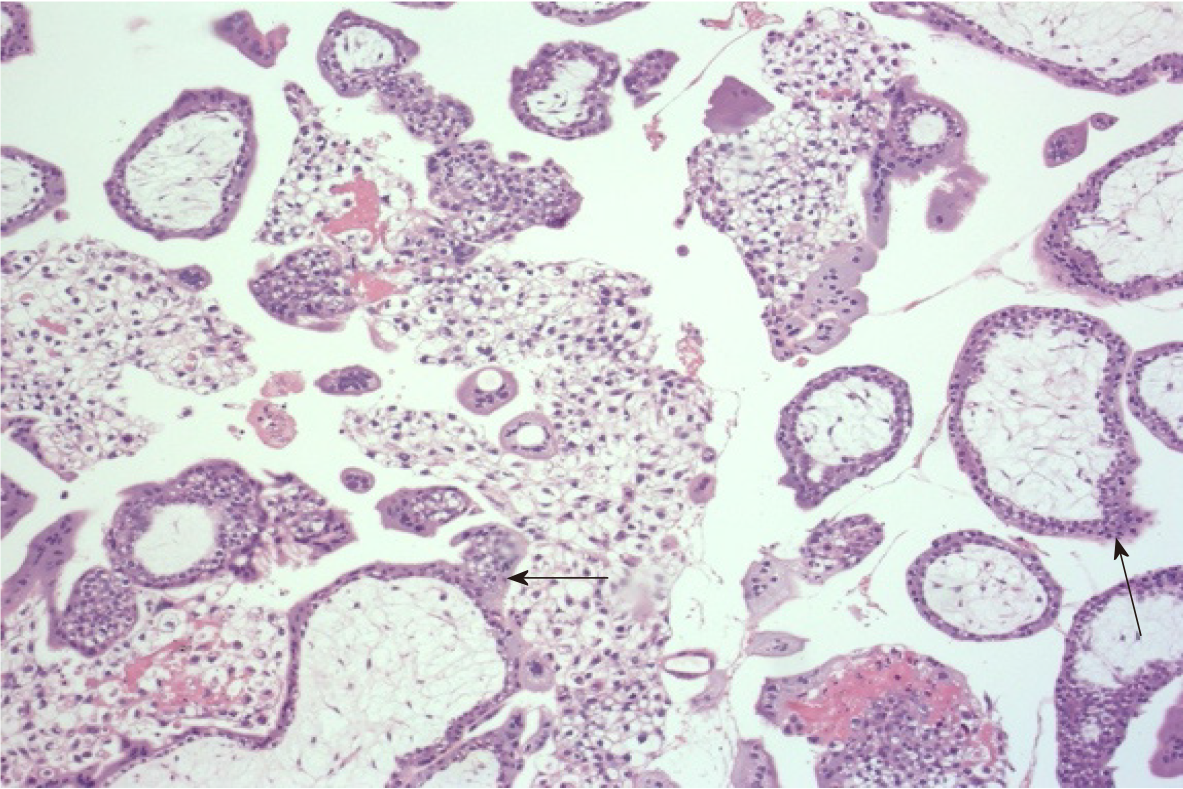
The patient underwent laparoscopic exploration and surgical treatment. A cyst measuring 4 cm in diameter was seen in the right ovary. The uterus, left ovary and bilateral fallopian tubes appeared normal. After removing the blood accumulated in the abdominal cavity, a mass measuring 5 cm × 3 cm, with dark red surface, was apparent under the right diaphragm. The mass was dissected completely (Figure 5). Subsequent histopathological investigation revealed chorionic villi within the mass, with no features of abnormal trophoblastic proliferation, confirming the diagnosis of ectopic pregnancy (Figure 6).
By postoperative day 5, the patient’s HCG level had dropped substantially (to 327.58 IU/L). The patient experienced no vaginal bleeding during the postoperative recovery and was discharged to home.
Less than 1% of ectopic pregnancies are implanted in the abdominal cavity[3,4]. While the underlying mechanism of this abnormal condition remains unclear, some risk factors have been identified, including pelvic inflammatory disease, pelvic surgery history, use of IUD, and previous ectopic pregnancy. Ectopic pregnancy under the diaphragm is extremely rare. The symptoms of abdominal pregnancy are usually non-specific, including abdominal or suprapubic pain, bloody vaginal discharge, and painful fetal movements. Although the beta subgroup of HCG is usually elevated in blood, some (approximately 1%) ectopic pregnancies present undetectable levels of HCG[5]. In this situation, imaging plays a more important role in diagnosis. US can detect fetal heartbeats, to make an accurate diagnosis, but its application is limited by the abdominal fat layer and gases in the intestine[6]. CT and MRI can provide more information about the tissue structure near the gestational sac; specifically, a contrast-enhanced CT and MRI will show ring-shaped intensity in ectopic pregnancy tissues[7,8]. Our patient, described herein, was subject to vaginal and abdominal imaging examinations by US, plain CT, and contrast-enhanced MRI.
In our patient, plain CT scan showed a high density mass beneath the subhepatic space. In the related literature, Qian et al[9] reported on the enhanced-CT finding of nodular lesions at the top of the right hepatic diaphragm. Kuai et al[10] reported a case of ectopic liver pregnancy that showed a mixed density lesion within the right liver lobe under the diaphragm on CT scan. Cai et al[11] reported the plain CT scan finding of a mass in the right hepatic lobe with a slightly low density peripheral region and an oval central portion with lower density, and the enhanced-CT scan finding of a significantly enhanced peripheral portion and nonenhanced center. In our patient, a curved mixed signal was observed beneath the subhepatic space on MRI, being mostly low in T1WI and high in T2WI, and showing restricted diffusion in DWI. After administration of Gd, a peripheral enhanced nodule was observed within the mixed curved signal. Wang et al[12] reported on a round lesion with low signal on T1WI and high signal on T2WI, and irregular mild enhancement in the venous phase. Cai et al[11] also reported on a mass in the right hepatic lobe showing increased glucose metabolism (SUVmax of 5.7) within the peripheral portion on positron emission tomography (PET)-CT scan. Familiarity with the typical and atypical features of the various forms of ectopic pregnancies on US, CT, MRI and PET-CT will certainly help to improve the rate of accurate diagnosis.
The choices of treatment for ectopic pregnancy involve either a conservative nonsurgical approach (typically, methotrexate administration) or surgery. For example, Qian et al[9] reported a successful diaphragmatic ectopic pregnancy intervention using US-guided percutaneous microwave ablation, and Chen et al[13] described a diaphragmatic pregnancy case managed with laparoscopic management. In our case, the diaphragmatic pregnancy had ruptured, necessitating laparoscopic operation.
Diaphragmatic pregnancy is very rare and more challenging to diagnose clinically. In any childbearing-age woman presenting with unexplained abdominal pain and abdominal bleeding, it is important to take a careful history that does not overlook information on menstrual cycle, menopause, vaginal bleeding, abortion, etc. The blood HCG test can clarify the general diagnosis of pregnancy, but imaging examination is necessary to determine if the pregnancy is ectopic. Moreover, a combination of multiple imaging modalities could assist the diagnoses of more difficult cases, such as the rare case described herein.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kato T S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
| 1. | Taran FA, Kagan KO, Hübner M, Hoopmann M, Wallwiener D, Brucker S. The Diagnosis and Treatment of Ectopic Pregnancy. Dtsch Arztebl Int. 2015;112:693-703; quiz 704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Parker VL, Srinivas M. Non-tubal ectopic pregnancy. Arch Gynecol Obstet. 2016;294:19-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 3. | Delabrousse E, Site O, Le Mouel A, Riethmuller D, Kastler B. Intrahepatic pregnancy: sonography and CT findings. AJR Am J Roentgenol. 1999;173:1377-1378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Fylstra DL. Ectopic pregnancy not within the (distal) fallopian tube: etiology, diagnosis, and treatment. Am J Obstet Gynecol. 2012;206:289-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | Wong E, Suat SO. Ectopic pregnancy--a diagnostic challenge in the emergency department. Eur J Emerg Med. 2000;7:189-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Brouard KJ, Howard BR, Dyer RA. Hepatic Pregnancy Suspected at Term and Successful Delivery of a Live Neonate With Placental Attachment to the Right Lobe of the Liver. Obstet Gynecol. 2015;126:207-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Takahashi A, Takahama J, Marugami N, Takewa M, Itoh T, Kitano S, Kichikawa K. Ectopic pregnancy: MRI findings and clinical utility. Abdom Imaging. 2013;38:844-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Harris GJ, Al-Jurf AS, Yuh WT, Abu-Yousef MM. Intrahepatic pregnancy. A unique opportunity for evaluation with sonography, computed tomography, and magnetic resonance imaging. JAMA. 1989;261:902-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Qian H, Tian G, Zheng H, Liang W, Jiang T. Successful management of diaphragmatic ectopic pregnancy using ultrasound-guided percutaneous microwave ablation. J Obstet Gynaecol Res. 2020;46:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Kuai XP, Wang SY, Qiu JM. Ectopic pregnancy implanted in the liver under the diaphragm. Taiwan J Obstet Gynecol. 2013;52:586-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Cai YY, Xiao EH, Shang QL, Xiao LZ. Ectopic pregnancy in the liver incidentally diagnosed by imaging: A case report. Exp Ther Med. 2017;14:373-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Wang CL, Cheng L, Zhang ZQ, Yuan ZD. Imaging diagnosis of hepatic ectopic pregnancy: A report of one case. Intractable Rare Dis Res. 2012;1:40. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Chen L, Liu J, Shu J, Zeng W, Zhao X. Successful laparoscopic management of diaphragmatic pregnancy:a rare case report and brief review of literature. BMC Pregnancy Childbirth. 2019;19:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |