Published online Dec 26, 2021. doi: 10.12998/wjcc.v9.i36.11425
Peer-review started: June 26, 2021
First decision: September 1, 2021
Revised: September 6, 2021
Accepted: November 14, 2021
Article in press: November 14, 2021
Published online: December 26, 2021
Processing time: 180 Days and 5.2 Hours
Root canal retreatment is common after root canal therapy in clinical situations. Especially, completing the retreatment of variant root canals can be challenging. This is particularly true for the molars located at the end of the dental arch. However, advancements in digital dental diagnosis and treatment techniques can solve these problems. Here, we describe a case of a maxillary second molar with a variant distobuccal root canal treated via a novel “inlay-guided endodontics” technique based on improved computer-generated programs.
A 63-year-old man complained of a defect in the maxillary left second molar. The tooth, diagnosed with post-treatment endodontic disease, was initially treated by conventional methods, which were ineffective. Our “inlay-guided endodontics” technique was subsequently adopted, with the establishment of a precise integrated three-dimensional (3D) plate model of cone-beam computed tomography data and a digital impression of the dentition. An optimal root canal approach was generated for the “virtual file” in the 3D model. The plate data were imported into a 3D printer and printed. With the help of the guide plate, the file was accurately placed into the cervical third of the distal root canal. The root canal and prosthodontic treatments successfully proceeded subsequently.
Our newly developed inlay guide plates may facilitate individualized and minimally invasive root canal treatment.
Core Tip: Operating the maxillary second molar is challenging due to the limited clinical space. “Guided orthodontics” has not been used to identify variant root canals of molars. We developed “inlay-guided endodontics” to improve on “guided endodontics”. Our guide plates may enable individualized, minimally invasive root canal treatment.
- Citation: Yan YQ, Wang HL, Liu Y, Zheng TJ, Tang YP, Liu R. Three-dimensional inlay-guided endodontics applied in variant root canals: A case report and review of literature. World J Clin Cases 2021; 9(36): 11425-11436
- URL: https://www.wjgnet.com/2307-8960/full/v9/i36/11425.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i36.11425
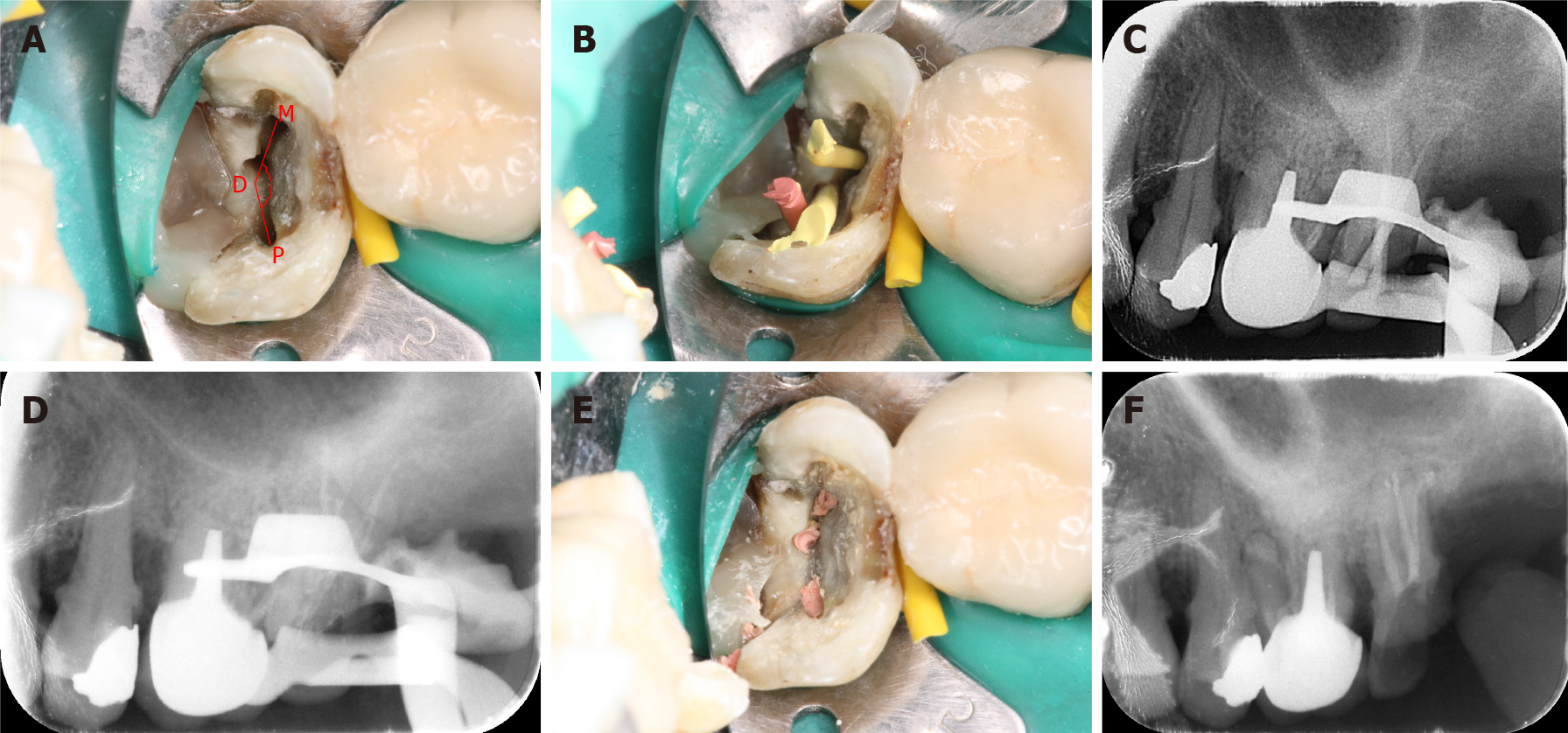
Root canal therapy is performed following a diagnosis of irreversible pulpitis or apical periodontitis. Despite inconsistencies in the literature, most previous studies have reported optimistic potential outcomes of root canal therapy, with the prevention or cure of apical periodontitis in over 80% of treated teeth[1-4]. However, many cases after root canal therapy require root canal retreatment[5], and the incidence of untreated root canals in these retreated cases is as high as 42%[3,6]. Furthermore, reports describing the retreatment of variant root canals are relatively scarce. Completing the retreatment of variant root canals can be challenging and is associated with a high technical failure rate and poor prognosis. This is particularly true for the maxillary second molar located at the end of the dental arch. The restricted clinical space and poor visual field increase operational difficulty. Additionally, variations in root canal anatomy can make the root canal orifice difficult to locate[7-10]. The roots of the maxillary second molar usually have small bifurcation angles, and the distal roots are often displaced medially or palatally, resulting in the fusion of roots[11]. A previous study that focused on the location of the root canal orifice of maxillary second molars showed that the PDM angle formed by the mesiobuccal (M), distobuccal (D), and palatal (P) root canal orifices was within 90°-140° in the majority of cases (92.8%) and ranged from 140° to 180° in only 2.49% of cases in which the angle was difficult to locate[12].
Advancements in digital dental diagnosis and treatment techniques can provide solutions to these problems[13-15]. Cone-beam computed tomography (CBCT) and three-dimensional (3D) printing technology yield high-definition 3D visualization data and facilitate precise navigation for dental treatment, allowing the use of 3D guide plates in stomatology. However, guide plates based on dental digital navigation technology have been mostly used in implant and oral surgery[16-18] and have not been effectively and widely used in endodontic treatment. If the new concept of “guided endodontics” can be effectively implemented in the field of root canal therapy, it may yield breakthroughs in the treatment of variant and challenging root canals. “Guided endodontics” refers to the process of integrating CBCT data and digital impression registration obtained by oral scanning technology with the help of special software. The implementation of this concept allows the fabrication of virtual files and virtual planning of an optimal root canal access, after which a 3D printer can produce the root canal guide plate[19]. This guide plate can guide root canal instruments to accurately identify variant root canal orifices, guiding smooth entry into the orifice and enabling complete root canal preparation.
Several pioneering studies have compared the guided endodontics technique with conventional methods using models[20-22]. Some recent clinical case reports presented the successful application of “guided endodontics” in clinical practice, including cavity preparation and root canal location in incisors with pulp canal calcification[19,21], and the removal of fiber-reinforced posts[23]. However, to our knowledge, no study has reported using this novel method to identify variant root canals of the posterior teeth, and all previous studies used only overlay guide plates. Moreover, many technical aspects have not been optimized in this novel method, including: (1) The stability of the root canal guide plate and sufficient clinical space for accessing the posterior teeth; (2) The protocol for automatic matching and precise integration of CBCT and oral scanning data; and (3) Accurate positioning and verification of virtual navigation channels. These are important factors, and their lack of optimization limits the effective use of “guided endodontics” in clinical practice. Therefore, we improved computer algorithms obtained from related fields to solve these problems in the development of digital root canal guides, and we developed the “inlay-guided endodontics” technology for retreating the residual crown of maxillary second molars with a variant distobuccal root canal orifice, which finally yielded the desired effect.
This paper presents a case of a novel “inlay-guided endodontics” technique applied in the retreatment of a maxillary second molar with a variant distobuccal root canal in a 63-year-old man.
A 63-year-old male patient presented to the department of stomatology of our hospital with a chief complaint of a defect in the maxillary left second molar, which had lasted for 8 mo.
Eight months earlier, the restoration fell out and the patient experienced occasional discomfort during eating. Therefore, he visited the clinic for further diagnosis and treatment.
Two years earlier, he was diagnosed with pulpitis of the maxillary left second molar and the tooth was subjected to root canal therapy.
Not mentioned.
After a clinical examination, a lesion was seen covering two-thirds of the distal occlusal surface of the maxillary left second molar, with exposure of the pulp chamber and secondary caries. The molar was tender to percussion but was not loose and did not respond to thermal tests.
There were no laboratory examinations.
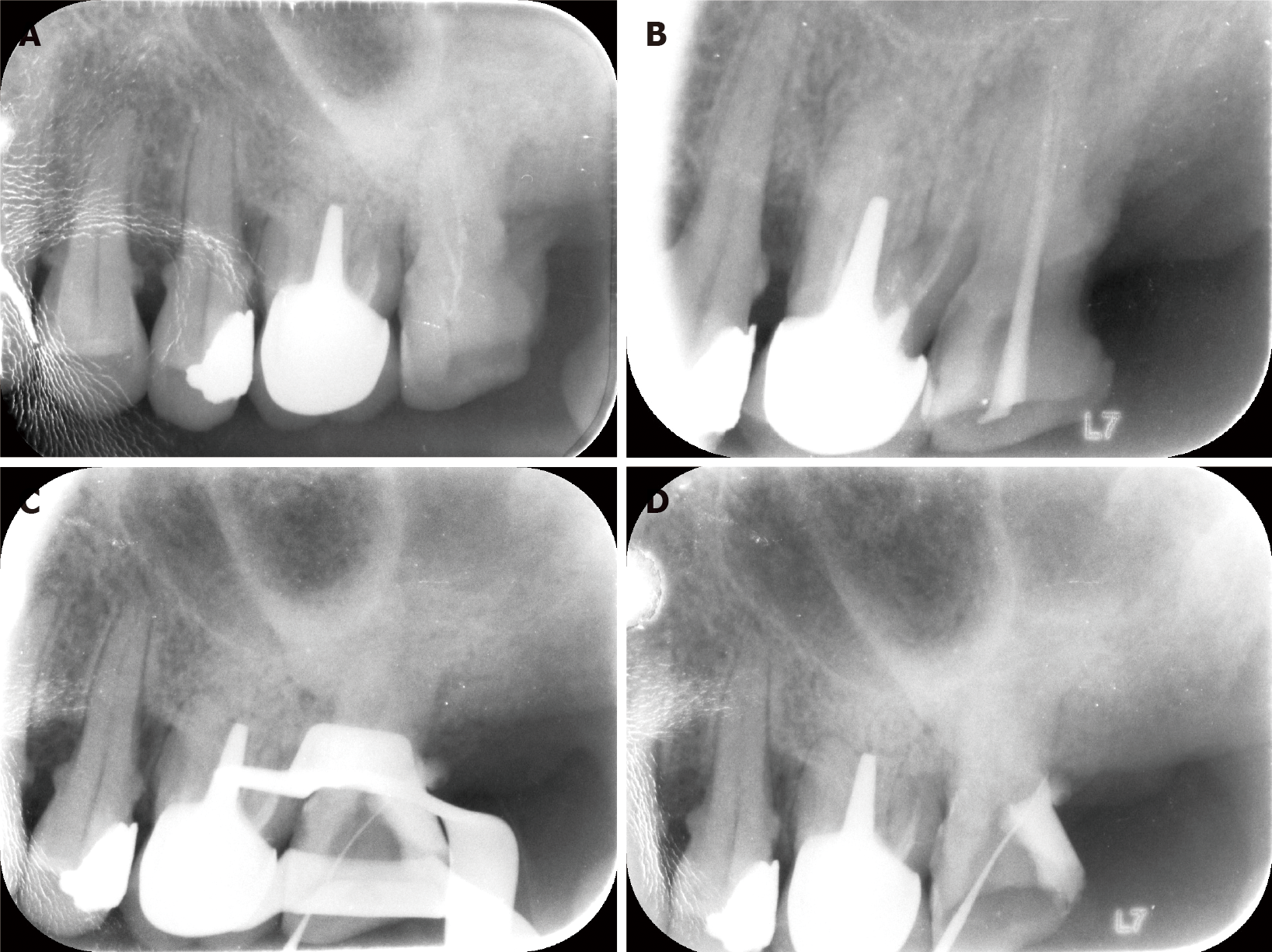
Radiological examinations showed hyperintensity in the mesial and palatal roots of the tooth, which were insufficiently filled, while the distobuccal root canal was empty. The tooth also showed mild radiologic signs of apical periodontitis, and the periodontal ligament space had widened (Figure 1A).
Therefore, the patient was diagnosed with post-treatment endodontic disease (chronic apical periodontitis, insufficient root canal filling, and root canal omission) involving the maxillary left second molar.
The clinical process of this study was approved by the ethics committee of our institution. The intervention on the patient complies with the requirements of the Declaration of Helsinki.
Retreatment of the mesial and palatal roots was completed successfully using conventional methods; however, the distal root could not be detected, even with a dental operating microscope. Moreover, the search for the distobuccal root resulted in a small perforation in the pulp chamber (Figure 1B-D). Therefore, we attempted treatment based on “guided endodontics.”
The patient's maxillary teeth were scanned via CBCT (New Tom, Verona, Italy). The patient was asked to open his mouth slightly to ensure that the occlusal surfaces of the upper and lower jaws were separated[24]. Because the patient's adjacent teeth had porcelain fused to a metal crown, as well as metal fillings, CBCT yielded noise-affected images and metal artifacts. Therefore, the traditional Retinex algorithm was improved with “image logarithmic domain operations.” The Retinex algorithm uses Retinex filtering to enhance bright regions of the image by combining color constancy with local contrast enhancement. We used this algorithm to enhance the CBCT images to allow better positioning of the tooth channel. To achieve this, image logarithmic domain operations were used to obtain the logarithm of each pixel value in each CBCT image. Segmented images were then obtained to differentiate the edges of teeth. In addition, the data were “normalized,” and the “weighted vectors” were removed; these vectors were used to cover image edges to remove the effect of noise in the CBCT images. Finally, the data were inverse-transformed to the real number domain to clarify the target root canal image. This domain contained all real numbers except 0, since division by 0 is undefined, (x-3) cannot be 0, and x cannot be 3. In such cases, we easily transformed all irrational number-related image pixels to real numbers to create the K-D tree.
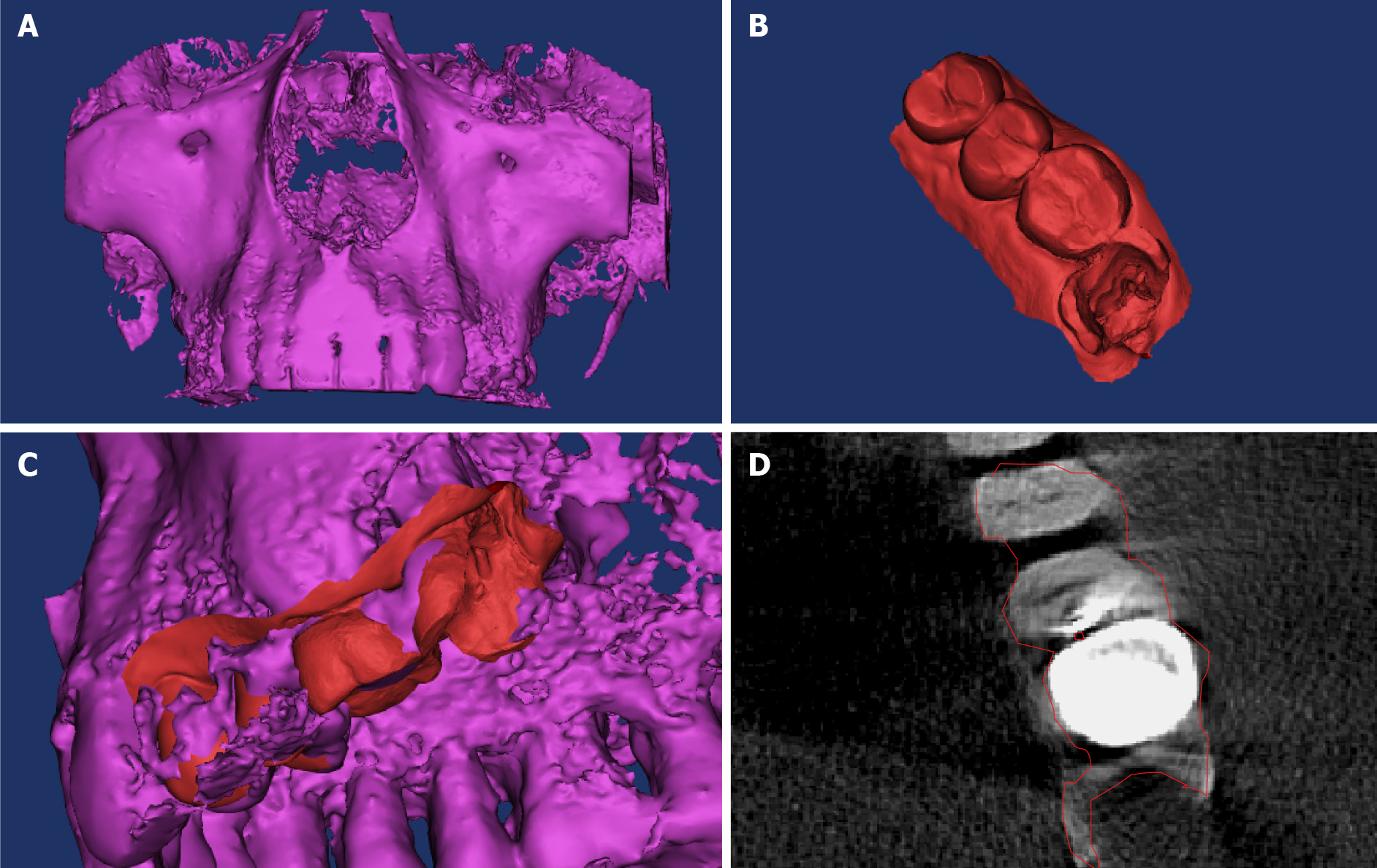
The data were saved in DICOM format by the 3D software (NNT version 5.6, Verona) for CBCT[25]. Subsequently, these DICOM data were imported into medical image processing software (Mimics 19.0; Materialise, Belgium) for processing. Finally, a 3D model of dental hard tissue with enamel, dentin, and partial alveolar bone was established, and the root canal morphology was assessed (Figure 2A).
A maxillary dentition impression was made using a 3D scanner (3Shape D750 Optical Scanner; 3Shape, Denmark)[26]. The STL files were exported, and the digital model of the work part was edited using reverse engineering software (Geomagic Studio 10; Geomagic, United States) (Figure 2B). Subsequently, the edited maxillary digital dentition impression of the work part and CBCT data were imported into the 3D visualization tool “Open Graphics Library,” wherein the two datasets were transformed into a digital grid using an “isosurface grid.” An isosurface grid is a 3D analog of an isoline and is a surface grid representing the points of a constant value connected by a normal face. In this case, we used an isosurface grid to transform CBCT images into a 3D mesh. The “transformation matrix” was produced by identifying the same feature points of two mathematical models and calculating the distance and axial difference between these feature points. Finally, automatic integration of CBCT data and the digital impression of the dentition was objectively and precisely achieved (Figure 2C and D)[27-29].
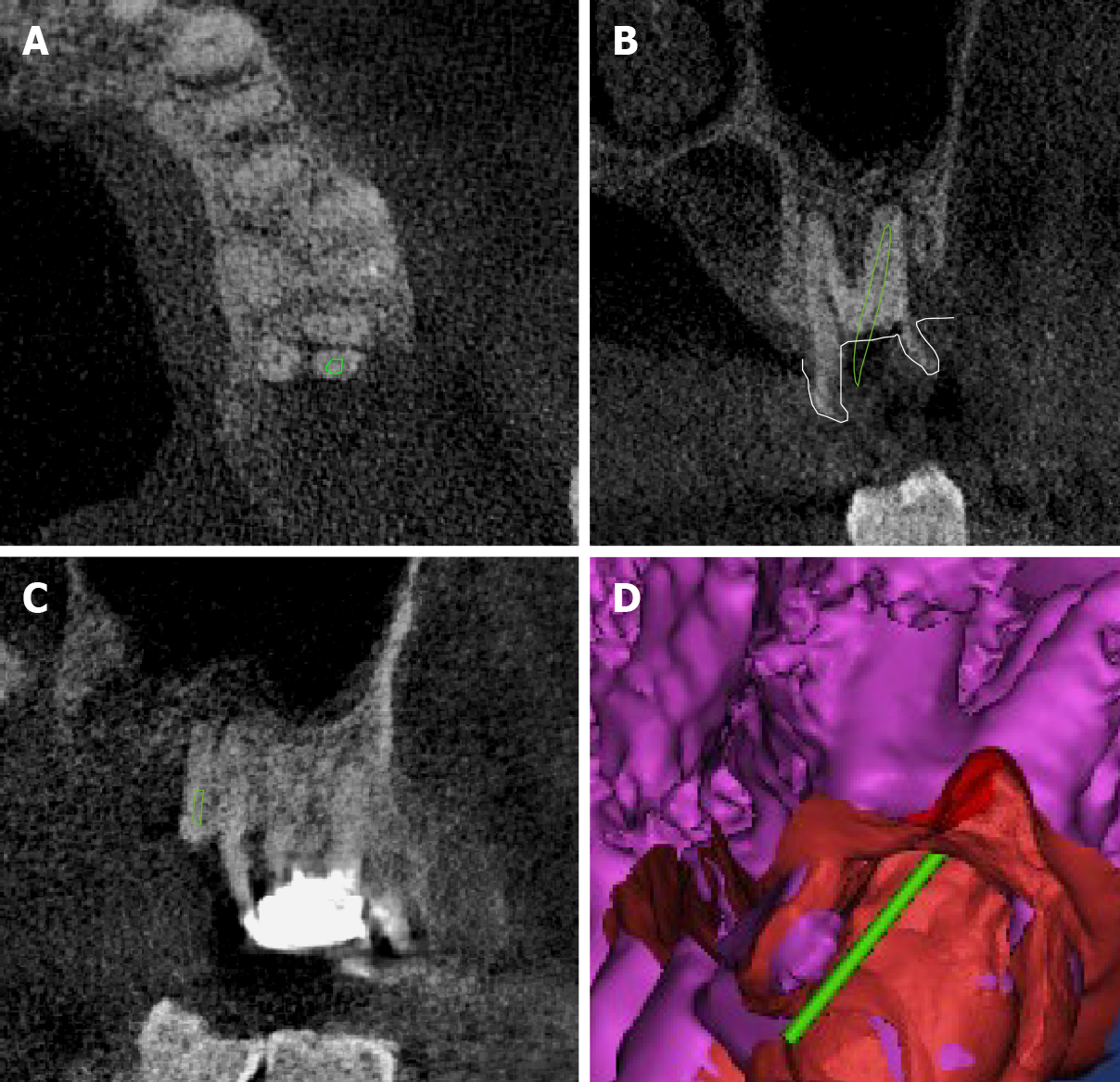
The point clouds (collections of data points that define the shape of some real or created physical system) of the virtual root canal file were located in sagittal, occlusal, and mesiodistal planes based on the transformation matrix in “Open Graphics Library” and then placed in the ideal location. To accurately navigate nickel-titanium instruments, the diameter of the virtual root canal file was set to 0.6 mm (Figure 3A-C). Subsequently, based on the difference in pixel values between the root and alveolar bone, we used the region growth method and Open Source Computer Vision Library (OPENCV) to separate the root edge and remove the surrounding alveolar bone. For the region growth method, the region growth algorithm was used to separate the goal mesh or model based on differences between the maximum and minimum pixel values within the region. This method tends to act as an edge detection algorithm. OPENCV is an open source computer vision and machine learning software library built to provide a common infrastructure for computer vision applications and accelerate the use of machine perception in commercial products. We used OPENCV to separate the edges of the roots of the teeth. Next, a K-dimensional (K-D) tree and the Poisson equation were adopted to smoothen the root of the teeth and obtain the real root shape (Figure 3D). A K-D tree is a binary search tree wherein data in each node is a K-dimensional point in space. In short, it is a space-partitioning data structure for organizing points in a K-dimensional space. The Poisson equation is a partial differential equation of the elliptic type with broad utility in mechanical engineering and theoretical physics. A K-D tree can be used, for instance, to describe the potential field caused by a given charge or mass density distribution. When the potential field is known, the gravitational or electrostatic field can be calculated. The purpose of root separation in this study was to check whether the virtual root canal file was in the target root canal in 3D space and to avoid errors. By far, this is the first study to report such an approach for removing the surrounding alveolar bone of the root.
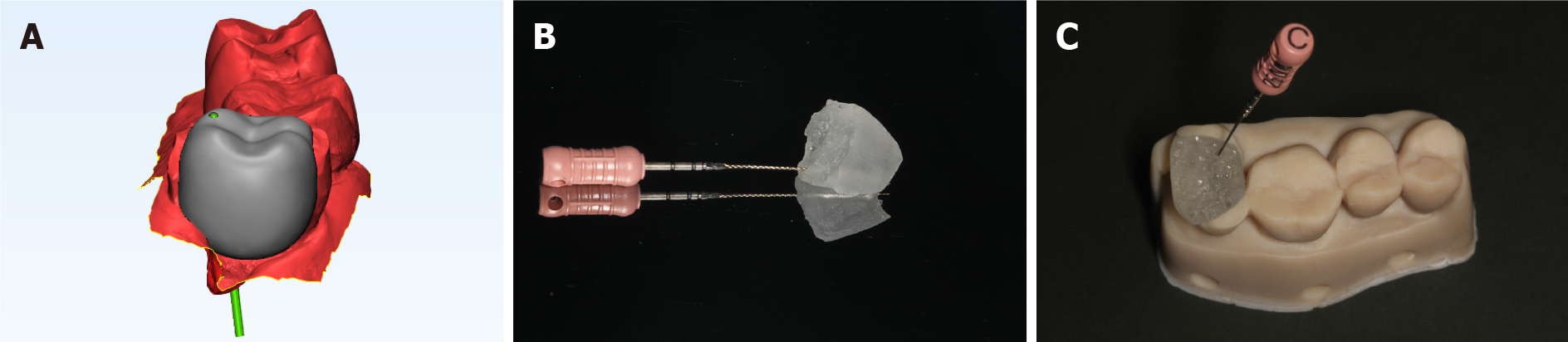
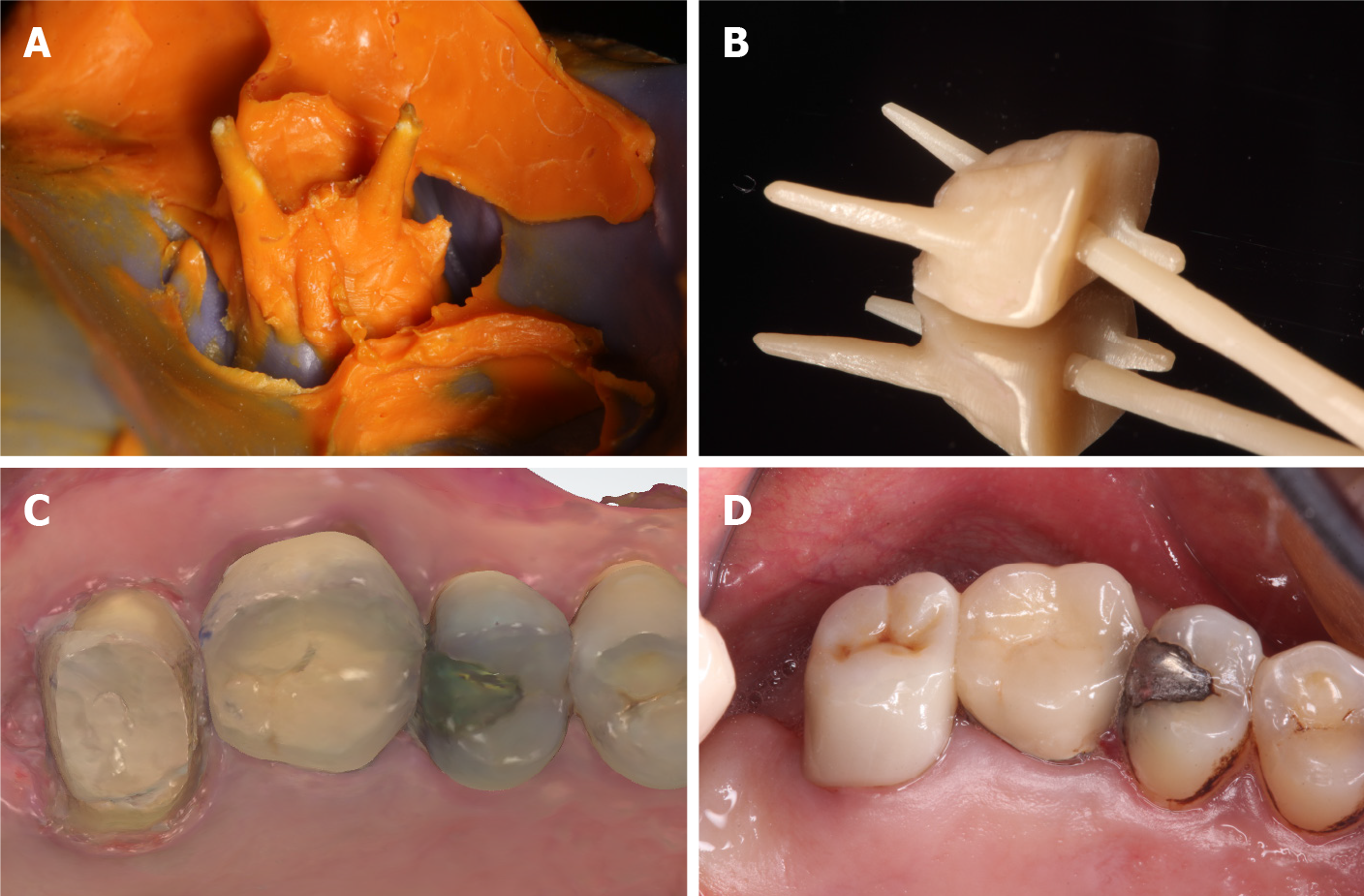
The dehiscent crown was filled by the regional growth method based on the standard crown shape. Boolean operations (Boolean operators are simple words such as AND, OR, NOT, or AND NOT) were used as conjunctions to combine or exclude keywords in a search, resulting in more focused and productive results. We used this approach to create the inlay of the target tooth and generate the “inlay-like guide plate” in the finite element analysis software (3-Matic 11.0; Materialise, Belgium). Based on the virtual 3D file design, a 0.6-mm-diameter navigation channel was generated on the axis of the inlay-like guide plate (Figure 4A). Subsequently, the generated plate data (in STL format) were imported into the 3D printer (Micro Plus Advantage; EnvisionTEC, Germany), with a precision of 50 µm.
Polylactic acid (True White PLA Large Spool; MakerBot, United States) was used as the printing material for the pedestal, and E-Guide Tint (E-Guide Tint; EnvisionTEC, Germany) was used for the guide plate (Figure 4B and C)[29,30].
The correct fit of the guide plate was checked when it was placed into the maxillary left second molar. After the guide plate was fully in place, the flow resin temporarily bonded the edges, and the entrance of the instrument on the surface of the guide plate was marked with gentian violet (Figure 5A). With the guidance of the plate, a 21-mm C-pilot file (10#) accurately entered the cervical third of the distal root canal (Figure 5B). Radiography was used to confirm the instrument’s entry into the root canal (Figure 5C). Subsequently, the working length of the distobuccal root canal was measured using a 16.5-mm Raypex 6 (VDW, Germany), and, using hand instruments, the distobuccal root canal was prepared and shaped up to the stainless steel K-file size 15. A root canal motor and nickel-titanium rotary instruments (M two; VDW, Germany) were used to prepare the root canal to 25#. EDTA gel was applied to lubricate the canal walls during the preparation process, and the root canals were irrigated. Next, ultrasonic root canal washing was performed with 1% NaClO. Subsequently, the PDM angle was measured and found to be 154.5°, indicating that it was in the minority group, as mentioned earlier. Therefore, it might have been difficult to locate, and root canal omission would have easily occurred if conventional methods had been employed.
After the completion of the preliminary rotary preparation of the distobuccal root canal, the guide plate was removed. The distal wall of the coronal lesion was restored with a resin (3M/ESPE, United States). Under rubber dam isolation, the remaining root canals were prepared with standard endodontic treatment procedures using K files and nickel–titanium rotary instruments. At 1 wk after intracanal treatment with VITAPAX, the tooth was clinically asymptomatic, with no visible erythema or fistula. The intracanal medicine was removed and the canals were cleaned by ultrasonic washing. Finally, the root canals were obturated with hot gutta-percha and the AH-plus root canal sealer. Vertical pressure was applied using the VDW system (Figure 6).
During the treatment, we kept close communication about the patient’s tension and anxiety as well as humanistic caring.
The tooth remained asymptomatic 1 wk after root filling and the patient reported no systemic symptoms. Then it was subsequently restored with an all-ceramic post-core and an all-ceramic crown (Sinold, Germany) (Figure 7)[31].
At the 2-year follow-up after treatment, the tooth remained asymptomatic. The crown showed a satisfactory marginal fit. Moreover, there was no mobility or sensitivity to percussion, with no gingival edema or erythema (Figure 8). A radiograph showed adequately filled canals with no low-density area in the apical region (Figure 9).
This is the first study to describe root canal retreatment of a maxillary second molar using an “inlay-guided plate.” The treatment process proceeded without adverse effects such as excessive tooth tissue removal or perforation, and the procedure yielded successful outcomes.
In this case, preoperative radiographs showed that the mesial and palatal roots of the maxillary left second molar had not been successfully filled, while the distal root was untreated. This implied the presence of a variant distal root. Additionally, failure to detect the root canal using a dental operating microscope confirmed that the distal root orifice was heterotopic. Moreover, the search procedure resulted in a small perforation in the pulp floor of the tooth. After this attempt, we doubted the possibility of further exploration of the remaining part of the pulp floor to identify the orifice of the variant root canal since it could lead to more defects in the hard tissue of the pulp floor and even loss of the tooth, violating the principles of preservation dentistry[32,33].
Under this circumstance, applying 3D digital dental technology by multidisciplinary joint diagnosis and treatment yielded unique advantages[28]. Based on the precise integration of CBCT data and digital impression, the virtual file was used to plan the surgical path, and the precise root canal guide plate was produced by a 3D printer[27,29,30]. Thus, identifying heterotopic root canal orifices and following the direction with the guidance of a guide plate will save chair time, increase efficiency, and reduce risks.
To date, some studies have used overlay root canal guide plates in the treatment of calcified single root canals of the anterior teeth[19-21]. However, these guide plates have limitations. The operation space for root canal therapy is not guaranteed due to the limited posterior space and the thickness of the overlay guide plates. Moreover, the stability of the overlay root canal guide plate is relatively poor. If the thickness and width of the plate are increased to improve its stability, the improved plate will further reduce the operation space. Moreover, the overlay guide plate can only navigate the outer part of the crown, not the whole process. Since nickel-titanium instruments are quite flexible, they may bend when they encounter resistance without the guide path, and the working length may be difficult to reach.
In this case, the inlay root canal guide plate was creatively designed and produced. The dental crown defect of the retreated teeth provided enough space for the design and use of the embedded guide plate. The inlay was only used to complete the crown without occupying additional space. Therefore, it provided sufficient operational space for root canal therapy of the posterior teeth, especially for the treatment of the maxillary second molar. Further, because the inlay guide plate was embedded in the inner part of the tooth, it guaranteed retention and stability. Furthermore, the inlay guide plate can guide nickel-titanium root canal instruments into the root canal for the whole guide path. Consequently, the inlay guide plate technique, which is a novel approach, could make root canal treatment more precise, individualized, yet minimally invasive. Thus, we can effectively preserve the remaining tooth tissues, particularly the pulp floor, and reduce the risk of root canal penetration.
The implementation of inlay guide plates relies on close communication and cooperation between dentists and computer professionals. Because the diameter of any root canal is very small, accuracy is required in the production process. Based on the high resolution and precision of CBCT imaging, precise integration with oral scanning data is essential to establish an accurate virtual path design and location. Some innovative computing processes were introduced into the design and fabrication of guide plates to address these requirements. These improved the clarity of CBCT scans, completed the precise integration of digital dentition impression and CBCT scans, and enabled precise positioning of the virtual file in the target root canal. The position was reviewed by digitally separating the root image. Finally, with the guidance of the inlay plate, the root canal, which could not be located previously, was accurately located.
However, because the amount of radiation and the cost of the procedure may increase with the use of CBCT, intraoral scanning, digital simulation, and guide plate production, the entire process has been described as time-consuming[34]. Although a small field of view is adequate for this purpose and updated CBCT devices can produce a limited radiation dose of only 5 µSv, the procedure still involves a large range of radiation doses produced by different devices. Therefore, every CBCT scan has to be justified. However, the chair time is reduced, and the success rate of treatment to preserve the root is significantly increased. Thus, the cost seems acceptable, and the radiation dose can be controlled.
The restoration of the all-ceramic post-core crown was completed in time after the root canal was filled. With the successful completion of root canal therapy, timely crown closure is of great importance to prevent root canal re-infection[31]. Despite the successful application of an inlay-guided location device and the timely integral crown-root restoration in this case, more cases and long-term follow-up are required to establish this protocol. Additionally, the inlay guide plate that we designed could only be used to locate and enter roots with a straight canal or the upper straight portion of a curved root canal, not curved root canals. This aspect requires further exploration and might be a source of future breakthroughs. Thus, “inlay-guided endodontics” may provide a useful adjunct technique for handling difficult cases of root canal retreatment in the future.
Using the inlay guide plate, root canal retreatment of the maxillary second molar was efficiently completed without adverse effects. Thus, the inlay guide plate, which was developed using a computerized technique, may facilitate more precise, individualized, yet minimally invasive root canal treatment. However, more cases and further research are required to establish this method.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Velázquez-Saornil J S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Yan JP
| 1. | Del Fabbro M, Corbella S, Sequeira-Byron P, Tsesis I, Rosen E, Lolato A, Taschieri S. Endodontic procedures for retreatment of periapical lesions. Cochrane Database Syst Rev. 2016;10:CD005511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Sinha N, Singh B, Langaliya A, Mirdha N, Huda I, Jain A. Cone beam computed topographic evaluation and endodontic management of a rare mandibular first molar with four distal canals. Case Rep Dent. 2014;2014:306943. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Swartz DB, Skidmore AE, Griffin JA Jr. Twenty years of endodontic success and failure. J Endod. 1983;9:198-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 158] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Monguilhott Crozeta B, Damião de Sousa-Neto M, Bianchi Leoni G, Francisco Mazzi-Chaves J, Terezinha Corrêa Silva-Sousa Y, Baratto-Filho F. A micro-computed tomography assessment of the efficacy of rotary and reciprocating techniques for filling material removal in root canal retreatment. Clin Oral Investig. 2016;20:2235-2240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Hoen MM, Pink FE. Contemporary endodontic retreatments: an analysis based on clinical treatment findings. J Endod. 2002;28:834-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 104] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Nimigean V, Nimigean VR, Sălăvăstru DI. A rare variant of internal anatomy of a third mandibular molar: a case report. Rom J Morphol Embryol. 2011;52:691-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Ashraf H, Dianat O, Hajrezai R, Paymanpour P, Azadnia S. Endodontic treatment of a double-rooted maxillary second molar with four canals: a case report. Iran Endod J. 2014;9:304-306. [PubMed] |
| 8. | Lin YH, Lin HN, Chen CC, Chen MS. Evaluation of the root and canal systems of maxillary molars in Taiwanese patients: A cone beam computed tomography study. Biomed J. 2017;40:232-238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Alamri HM, Mirza MB, Riyahi AM, Alharbi F, Aljarbou F. Root canal morphology of maxillary second molars in a Saudi sub-population: A cone beam computed tomography study. Saudi Dent J. 2020;32:250-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Maggiore C, Gallottini L, Resi JP. Mandibular first and second molar. The variability of roots and root canal system. Minerva Stomatol. 1998;47:409-416. [PubMed] |
| 11. | Han X, Yang H, Li G, Yang L, Tian C, Wang Y. A study of the distobuccal root canal orifice of the maxillary second molars in Chinese individuals evaluated by cone-beam computed tomography. J Appl Oral Sci. 2012;20:563-567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Wesemann C, Muallah J, Mah J, Bumann A. Accuracy and efficiency of full-arch digitalization and 3D printing: A comparison between desktop model scanners, an intraoral scanner, a CBCT model scan, and stereolithographic 3D printing. Quintessence Int. 2017;48:41-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 29] [Reference Citation Analysis (0)] |
| 13. | Eliášová H, Dostálová T. 3D Multislice and Cone-beam Computed Tomography Systems for Dental Identification. Prague Med Rep. 2017;118:14-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Alghazzawi TF. Advancements in CAD/CAM technology: Options for practical implementation. J Prosthodont Res. 2016;60:72-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 308] [Article Influence: 34.2] [Reference Citation Analysis (0)] |
| 15. | Colombo M, Mangano C, Mijiritsky E, Krebs M, Hauschild U, Fortin T. Clinical applications and effectiveness of guided implant surgery: a critical review based on randomized controlled trials. BMC Oral Health. 2017;17:150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 108] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 16. | Vercruyssen M, Laleman I, Jacobs R, Quirynen M. Computer-supported implant planning and guided surgery: a narrative review. Clin Oral Implants Res. 2015;26 Suppl 11:69-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 121] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 17. | Greenberg AM. Digital technologies for dental implant treatment planning and guided surgery. Oral Maxillofac Surg Clin North Am. 2015;27:319-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Krastl G, Zehnder MS, Connert T, Weiger R, Kühl S. Guided Endodontics: a novel treatment approach for teeth with pulp canal calcification and apical pathology. Dent Traumatol. 2016;32:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 143] [Article Influence: 14.3] [Reference Citation Analysis (1)] |
| 19. | Zehnder MS, Connert T, Weiger R, Krastl G, Kühl S. Guided endodontics: accuracy of a novel method for guided access cavity preparation and root canal location. Int Endod J. 2016;49:966-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 164] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 20. | Connert T, Zehnder MS, Amato M, Weiger R, Kühl S, Krastl G. Microguided Endodontics: a method to achieve minimally invasive access cavity preparation and root canal location in mandibular incisors using a novel computer-guided technique. Int Endod J. 2018;51:247-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 21. | Connert T, Krug R, Eggmann F, Emsermann I, ElAyouti A, Weiger R, Kühl S, Krastl G. Guided Endodontics versus Conventional Access Cavity Preparation: A Comparative Study on Substance Loss Using 3-dimensional-printed Teeth. J Endod. 2019;45:327-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 22. | Perez C, Finelle G, Couvrechel C. Optimisation of a guided endodontics protocol for removal of fibre-reinforced posts. Aust Endod J. 2020;46:107-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 23. | Ordinola-Zapata R, Bramante CM, Versiani MA, Moldauer BI, Topham G, Gutmann JL, Nuñez A, Duarte MA, Abella F. Comparative accuracy of the Clearing Technique, CBCT and Micro-CT methods in studying the mesial root canal configuration of mandibular first molars. Int Endod J. 2017;50:90-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 103] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 24. | Zhao YJ, Wang SW, Liu Y, Wang Y. [A method for rapid extracting three-dimensional root model of vivo tooth from cone beam computed tomography data based on the anatomical characteristics of periodontal ligament]. Beijing Da Xue Xue Bao Yi Xue Ban. 2017;49:54-59. [PubMed] |
| 25. | Nagao M, Sohmura T, Kinuta S, Kojima T, Wakabayashi K, Nakamura T, Takahashi J. Integration of 3-D shapes of dentition and facial morphology using a high-speed laser scanner. Int J Prosthodont. 2001;14:497-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Rangel FA, Maal TJJ, de Koning MJJ, Bronkhorst EM, Bergé SJ, Kuijpers-Jagtman AM. Integration of digital dental casts in cone beam computed tomography scans-a clinical validation study. Clin Oral Investig. 2018;22:1215-1222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | van der Meer WJ, Vissink A, Ng YL, Gulabivala K. 3D Computer aided treatment planning in endodontics. J Dent. 2016;45:67-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 28. | Zhang HR, Yin LF, Liu YL, Yan LY, Wang N, Liu G, An XL, Liu B. [Fabrication and accuracy research on 3D printing dental model based on cone beam computed tomography digital modeling]. Hua Xi Kou Qiang Yi Xue Za Zhi. 2018;36:156-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 29. | Chen H, Zhao T, Wang Y, Sun YC. [Computer aided design and 3-dimensional printing for the production of custom trays of maxillary edentulous jaws based on 3-dimensional scan of primary impression]. Beijing Da Xue Xue Bao Yi Xue Ban. 2016;48:900-904. [PubMed] |
| 30. | Pedro FM, Marques A, Pereira TM, Bandeca MC, Lima S, Kuga MC, Tonetto MR, Semenoff-Segundo A, Borges AH. Status of Endodontic Treatment and the Correlations to the Quality of Root Canal Filling and Coronal Restoration. J Contemp Dent Pract. 2016;17:830-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 31. | Jiang HW. [Theory and practice of minimally invasive endodontics]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2016;51:460-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Rayapudi J, Usha C. Knowledge, attitude and skills of dental practitioners of Puducherry on minimally invasive dentistry concepts: A questionnaire survey. J Conserv Dent. 2018;21:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 33. | Cohenca N, Shemesh H. Clinical applications of cone beam computed tomography in endodontics: A comprehensive review. Quintessence Int. 2015;46:657-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 34. | Ludlow JB, Timothy R, Walker C, Hunter R, Benavides E, Samuelson DB, Scheske MJ. Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol. 2015;44:20140197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 300] [Article Influence: 30.0] [Reference Citation Analysis (0)] |