Published online Dec 26, 2021. doi: 10.12998/wjcc.v9.i36.11355
Peer-review started: April 27, 2021
First decision: June 5, 2021
Revised: June 6, 2021
Accepted: August 16, 2021
Article in press: August 16, 2021
Published online: December 26, 2021
Processing time: 240 Days and 11 Hours
An incarcerated hernia is a common cause of acute abdominal pain. There are various types of incarcerated hernias, including incarcerated hernias of the appendix. These hernias are often complicated by appendiceal inflammation, necrosis, and suppuration, which affect the outcome of surgical repair. A De Garengeot hernia is a femoral hernia that contains the appendix. This type of hernia has a low incidence. When a De Garengeot hernia is clinically suspected, emergency surgical treatment should be performed as soon as possible.
A 59-year-old man was admitted to the hospital with a painful right inguinal mass that had suddenly developed 6 hours earlier. Physical examination revealed a 4 cm × 2 cm palpable mass in the right groin. The mass was hard and could not be reduced due to tenderness. It did not descend into the scrotum. B-ultrasound revealed an incarcerated hernia. During surgery, the hernia was found to contain the appendix, which exhibited distal avascular necrosis. A De Garengeot hernia was diagnosed according to the classification criteria of this type of inguinal hernia. Laparoscopic reduction of the incarcerated hernia, appendectomy, and small-incision femoral hernia repair were performed in the emergency department, and cefuroxime was administered as anti-infection therapy for 2 d postoperatively. After treatment, the patient had no abdominal pain or infection and was discharged on postoperative day 4. He had no recurrence of the inguinal hernia after 16 months of follow-up.
De Garengeot hernias have a low incidence and are difficult to diagnose. Laparoscopy is useful for their diagnosis and treatment.
Core Tip: Clinicians should be aware of the fact that a De Garengeot hernia has a low incidence and is difficult to diagnose in the early stages. When a De Garengeot hernia is clinically suspected, B-ultrasound or computed tomography and emergency surgical treatment should be performed as soon as possible. Laparoscopy is useful for the diagnosis and treatment of De Garengeot hernias and is thus worthy of clinical application.
- Citation: Yao MQ, Yi BH, Yang Y, Weng XQ, Fan JX, Jiang YP. De Garengeot hernia with avascular necrosis of the appendix: A case report. World J Clin Cases 2021; 9(36): 11355-11361
- URL: https://www.wjgnet.com/2307-8960/full/v9/i36/11355.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i36.11355
Clinically, incarcerated hernias include an incarcerated hernia of part of the intestinal wall (Richter hernia), a small intestinal diverticulum-containing incarcerated hernia (Littre hernia), a retrograde loop incarcerated hernia (Maydl hernia), and an incarcerated hernia of the appendix[1]. A De Garengeot hernia contains the appendix, which is often complicated by inflammation, necrosis, and suppuration, affecting the outcome of surgical repair[2]. De Garengeot hernias have a low incidence that tends to be consistent with the incidence pattern of femoral hernias, and they are more common in older women[3]. We admitted a patient with an incarcerated hernia on December 10, 2019, who was diagnosed intraoperatively with a De Garengeot hernia and avascular necrosis of the appendix.
A 59-year-old man was admitted to hospital with a painful right groin mass that had suddenly developed 6 h earlier.
The pain was located in the inguinal region, and the mass did not descend into the scrotum. The patient reported nausea and vomiting, but he had no fever, diarrhea, hematochezia, or associated dysuria.
The patient had a 10-year history of hypertension that was controlled with valsartan at 40 mg once daily.
He had smoked approximately 10 cigarettes daily for 20 years and did not drink. The patient’s family history was negative.
On admission, the patient showed normal consciousness and had evidence of acute illness, a flat and soft abdomen, and mild tenderness in the right lower abdomen with no rebound pain. A hard 4 cm × 2 cm mass was palpable in the right groin, and it was unable to be reduced due to tenderness. The mass did not descend into the scrotum, and the skin in the groin area showed no obvious redness or swelling.
Examination after admission showed a white blood cell count of 4.6 × 109/L (75.4% neutrophils), red blood cell count of 5.29 × 1012/L, platelet count of 153.0 × 109/L, and C-reactive protein concentration of 25.2 mg/L. The prothrombin time was 10.9 s, activated partial thromboplastin time was 32.5 s, and international normalized ratio was 1.01. The blood urea nitrogen concentration was 9.2 mmol/L, the serum creatinine concentration was 84 µmol/L, and the alanine aminotransferase concentration was 39 U/L.
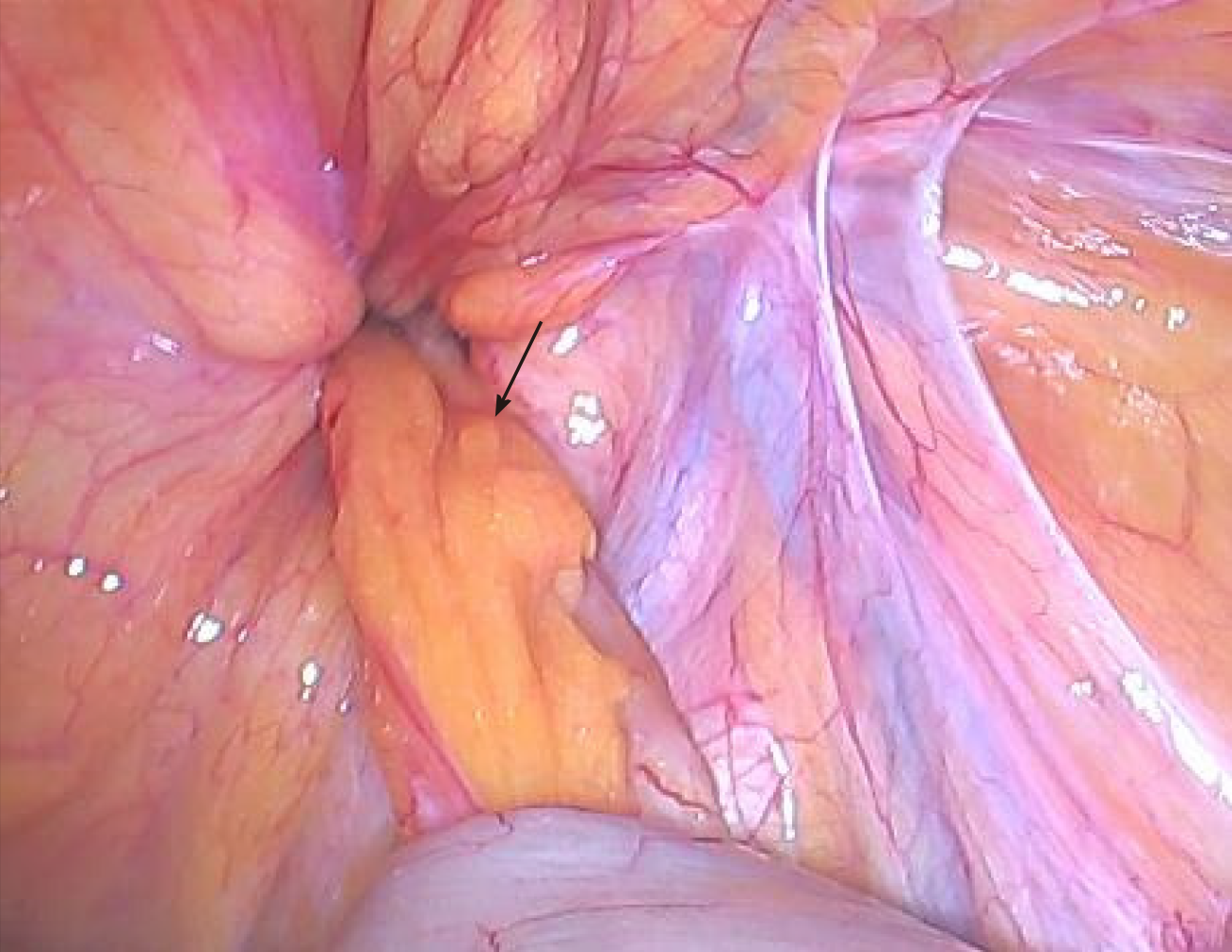
Inguinal B-ultrasound showed involvement of the right inguinal canal with no obvious reduction after pressurization with probes. Color Doppler flow imaging indicated no change in blood flow, and scanning of the left groin area showed no obvious abnormalities (Figure 1).
The appendix was herniated into the femoral ring, leading to a definitive diagnosis of a De Garengeot hernia.
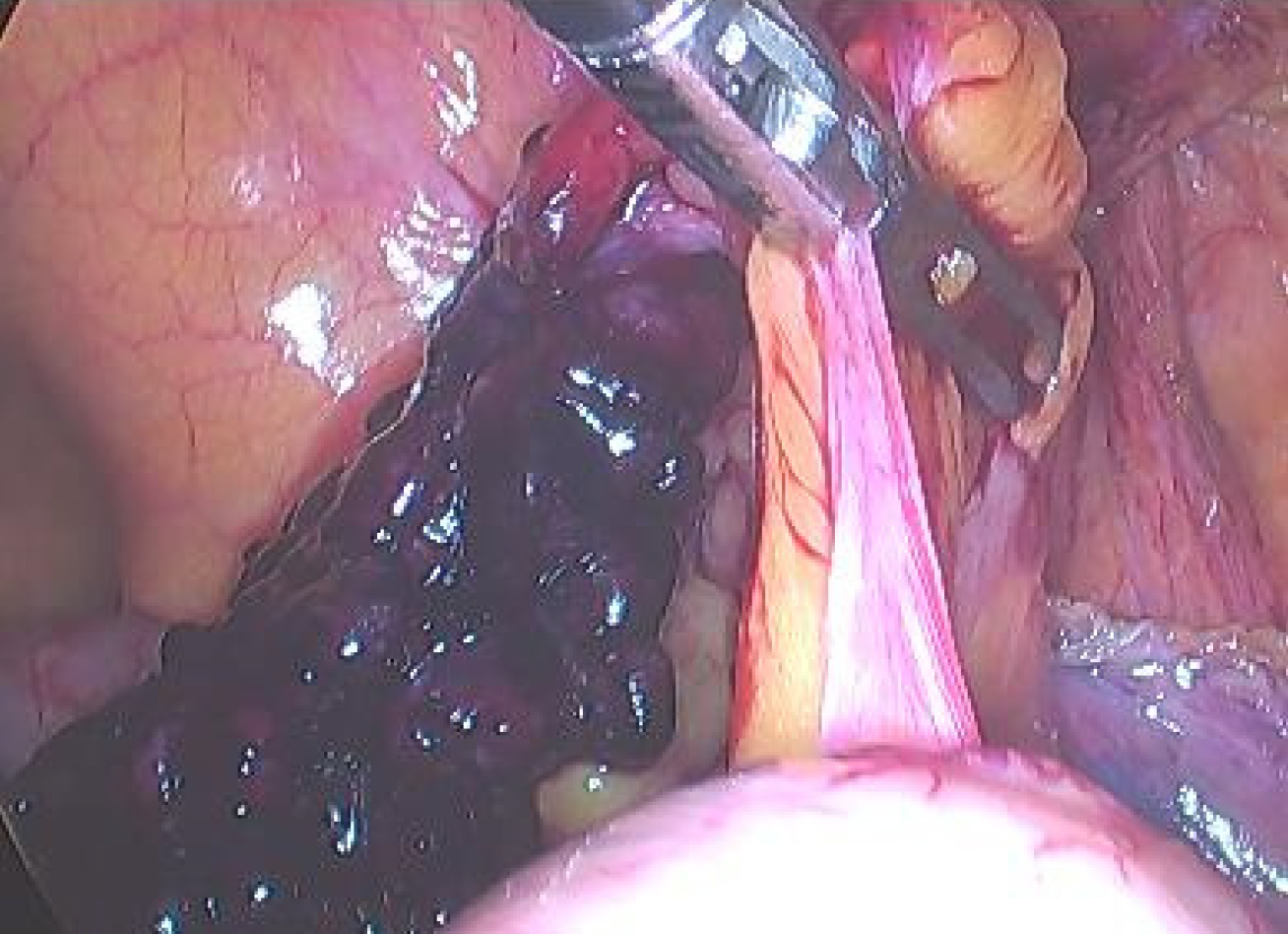
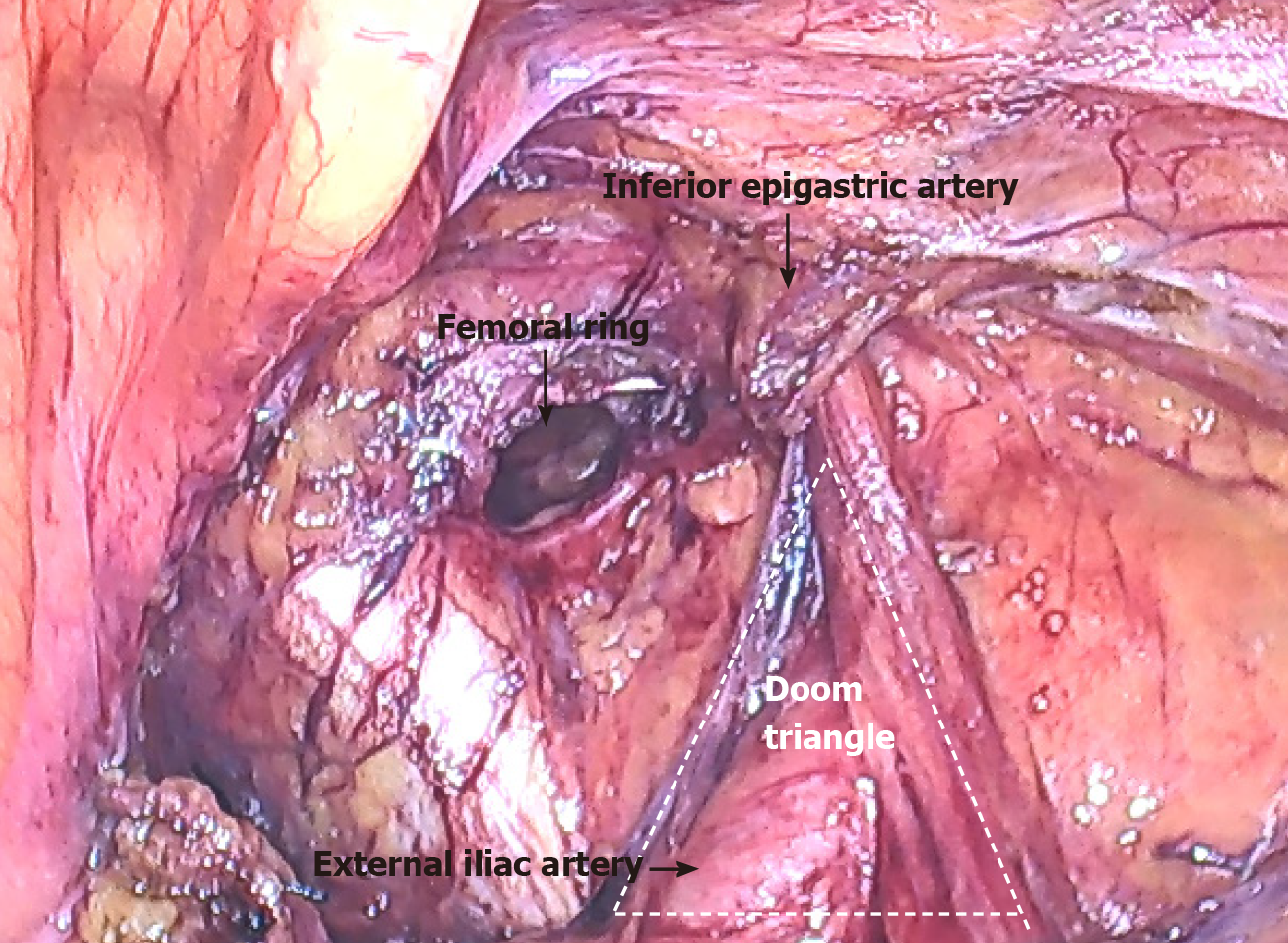
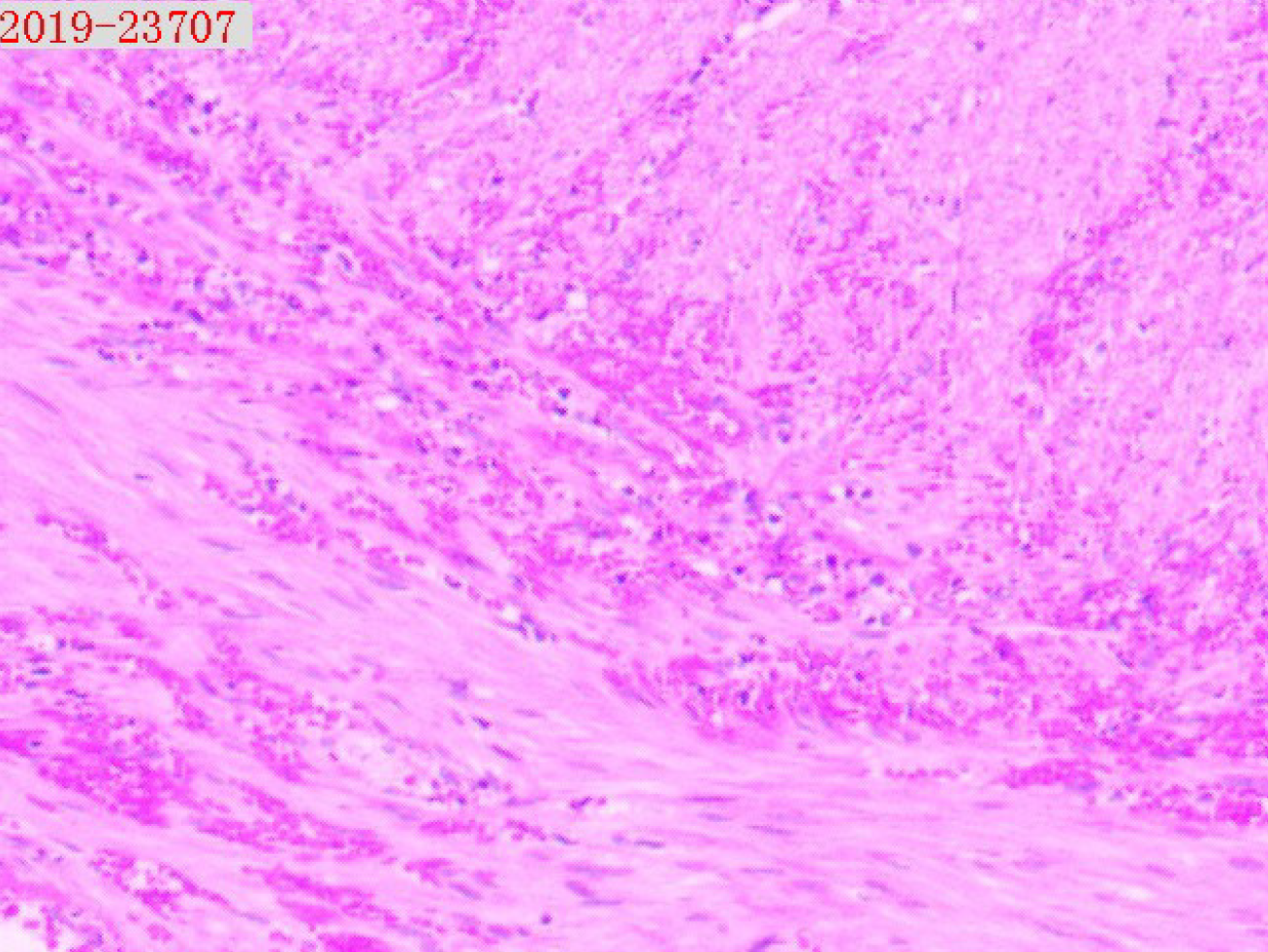
A right-sided incarcerated hernia was considered, and laparoscopic exploration was performed under general anesthesia in the emergency department. During surgery, the appendix and its mesangium were found to be herniated into the femoral ring. The 3-cm most proximal segment of the appendix was in the abdominal cavity, and its color was normal (Figure 2). The proximal appendix was pulled and assisted manual reduction was attempted, but the hernia could not be reduced. The 2-cm section of peritoneum above the femoral ring was cut in an arc to detach the preperitoneal space and thus expose the iliopubic tract (Figure 3). After cutting part of the iliopubic tract using an electric hook to loosen the hernia ring and return the appendix, we found that the distal appendix and its mesangium were dark in color and demonstrated avascular necrosis (Figure 4). After reduction, the femoral ring was clear (Figure 5). The necrotic appendix was removed by laparoscopic surgery, and the roots were ligated using double silk sutures. Considering that patch placement after surgery had a high risk of serious complications such as patch infection, a small incision was made in the right groin to suture the internal oblique muscle and syndesmosis to the pectineal ligament. The right femoral hernia was then repaired using the McVay method. The postoperative pathology report showed that a large number of neutrophils had infiltrated the wall of the appendix and mesangial fat, and hemorrhagic necrosis was also observed in the mesangium (Figure 6).
The surgical course was smooth, and cefuroxime was administered as anti-infection therapy for 2 d after surgery. The patient was discharged 4 d after surgery without complications such as wound infection. He had no recurrence of the inguinal hernia after 16 mo of follow-up.
Incarcerated hernias of the groin and strangulated hernias require timely emergency surgery. Delays in diagnosis and surgery greatly increase the possibility of intestinal necrosis, which markedly increases the incidence of postoperative complications and mortality[4]. Amyand hernias have a low incidence, accounting for less than 1% of all inguinal hernias. Amyand hernias with complications, such as inflammation, perforation, or abscess formation, are even rarer, with an incidence of approximately 0.1%[5]. De Garengeot hernias are much rarer than Amyand hernias, with a reported incidence of 0.5% to 5.0% of all femoral hernias[6]. Due to the narrow femoral ring, a De Garengeot hernia has a much higher risk of strangulation than an Amyand hernia[7]. De Garengeot hernias are difficult to diagnose before surgery; thus, they are easily misdiagnosed and may be missed clinically. The mechanism underlying the development of a De Garengeot hernia is compression of the neck of the hernia ring, which causes extraluminal obstruction. Muscle contraction or any other cause of a sudden increase in intra-abdominal pressure may cause compression of the appendix, and its blood supply may be subsequently interrupted or significantly reduced, leading to inflammation and bacterial overgrowth[8]. Whether appendectomy should be performed in patients with a healthy appendix and whether patch repair should be adopted after appendectomy remain controversial. Laparoscopic exploration enables visual observation of the abdominal cavity and hernia, and can be used to diagnose a De Garengeot hernia, assess the condition of the appendix, and choose the subsequent treatment regimen (appendectomy, femoral hernia repair, or transabdominal preperitoneal prosthetic and laparoscopic appendectomy)[9]. The choice of the most appropriate surgical method depends on whether the appendix is inflamed and, if so, the severity of inflammation (Table 1). If the appendix is not inflamed, laparoscopic patch repair is recommended. If appendicitis is observed but peritonitis is not, and if tissue conditions permit, laparoscopic appendectomy and patch repair can be performed[10]. When inflammation of the appendix is severe, patch repair may have an infection rate as high as 50%[11]; therefore, this form of repair is not recommended. Due to avascular necrosis of the appendix, patch repair may complicate infection. Thus, the patient in the present case underwent appendectomy and hernia repair using the conventional McVay method. The patient was discharged from the hospital 4 d after surgery. One week after surgery, he returned to hospital for suture removal, and no evidence of incisional infection was present.
| Appendiceal inflammation | Interventions |
| No inflammation | Return the appendix and perform laparoscopic patch repair |
| Non-severe inflammation | Laparoscopic appendectomy and patch repair |
| Severe inflammation with perforation or abscess formation | Laparoscopic appendectomy and mesh-free repair |
Clinicians should be aware of the fact that De Garengeot hernias have a low incidence and are difficult to diagnose in the early stages. When a De Garengeot hernia is suspected, surgery should be performed as soon as possible. Laparoscopy is useful for the diagnosis and treatment of De Garengeot hernias and is therefore worthy of clinical application.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ferreira GSA, Strainiene S S-Editor: Wu YXJ L-Editor: Webster JR P-Editor: Wang LYT
| 1. |
China Hernia Society, Guideline for diagnosis and treatment of adult groin hernia (2018 edition).
|
| 2. | Chen XP, Wang JP, Zhao JZ. Surgery. Peking: People's Sanitary Publishing Pub, 2018: 371-374. |
| 3. | Granvall SA. de Garengeot hernia: a unique surgical finding. JAAPA. 2014;27:39-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Zhu L, Tang WH, Tang JX. Emergency surgery of groin incarcerated hernia and strangulated hernia in adults. Guoji Waikexue Zazhi. 2016;43:712-715. [DOI] [Full Text] |
| 5. | Michalinos A, Moris D, Vernadakis S. Amyand's hernia: a review. Am J Surg. 2014;207:989-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 6. | Talini C, Oliveira LO, Araújo AC, Netto FA, Westphalen AP. De Garengeot hernia: Case report and review. Int J Surg Case Rep. 2015;8C:35-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Sharma D, Katsnelson J, Nwachuku E, Kolff J. The De Garengeot hernia: A case report of an unusual presentation of appendicitis. Int J Surg Case Rep. 2020;76:46-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Sharma H, Jha PK, Shekhawat NS, Memon B, Memon MA. De Garengeot hernia: an analysis of our experience. Hernia. 2007;11:235-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Shiihara M, Kato T, Kaneko Y, Yoshitoshi K, Ota T. de Garengeot hernia with appendicitis treated by two-way-approach surgery: a case report. J Surg Case Rep. 2017;2017:rjx140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Dai WG, Chen JH, Yu HL, Chen CQ. right-sided De Garengeot's hernia with gangrenous appendicitis: a case report. Zhongguo Shiyong Waike Zazhi. 2018;38:1084-1085. [DOI] [Full Text] |
| 11. | Holmes K, Guinn JE. Amyand hernia repair with mesh and appendectomy. Surg Case Rep. 2019;5:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |