Published online Dec 26, 2021. doi: 10.12998/wjcc.v9.i36.11311
Peer-review started: June 28, 2021
First decision: July 26, 2021
Revised: July 27, 2021
Accepted: November 5, 2021
Article in press: November 5, 2021
Published online: December 26, 2021
Processing time: 178 Days and 6.3 Hours
Acute otitis media (AOM) is a common disease that is more prevalent in children. Most studies concerning AOM-associated sudden sensorineural hearing loss are case reports and retrospective in nature, hence the etiology of AOM-associated sudden hearing loss has not been fully established.
To analyze audiological characteristics of AOM-associated sudden hearing loss and evaluate efficacy of combined tympanostomy tube placement (TTP) and intratympanic methylprednisolone.
Eight adult patients who were diagnosed with AOM-associated sudden hearing loss and ineffectively treated by conventional medical therapy were enrolled in this study. Basic data were collected, and pure tone audiometry was performed to assess the audiological characteristics. Combination therapy with TTP and intratympanic methylprednisolone injection was given to the patients.
Mixed or sensorineural hearing loss was observed at high frequencies (2–4 kHz). All the cases in this study were cured after TTP and intratympanic methylprednisolone. After treatment, the average hearing threshold at affected frequencies was significantly lower than those in the pretreatment group (P < 0.05) and was similar to that in the healthy ears (P > 0.05).
AOM rarely induces sudden sensorineural hearing loss. Combination therapy with TTP and intratympanic methylprednisolone injection may be effective after failure of conventional medical treatment.
Core Tip: Acute otitis media (AOM)-associated sudden sensorineural hearing loss is a rare otological condition and the mechanism and treatment methods have not been defined. This study described the audiological features of the patients with AOM-associated sudden hearing loss and evaluated the clinical efficacy of tympanostomy tube placement and intratympanic methylprednisolone injection after failure of conventional medical therapy.
- Citation: Cao X, Yi HJ. Audiological characteristics and exploratory treatment of a rare condition of acute-otitis-media-associated sudden sensorineural hearing loss. World J Clin Cases 2021; 9(36): 11311-11319
- URL: https://www.wjgnet.com/2307-8960/full/v9/i36/11311.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i36.11311
Acute otitis media (AOM) is a common disease that is more prevalent in children, affecting > 80% of children before the age of 3 years[1]. Globally, there are > 709 million new cases reported every year[2,3]. AOM is mainly caused by acute viral infection of the upper respiratory tract, which alters eustachian tube function and exposes the middle ear to bacterial infiltration[4]. There may be a conductive hearing loss if the patient also has tympanic effusion, and the degree of hearing loss can vary from negligible to 60 dB[5-8]. In the clinic, antibiotics and early myringotomy are the only two treatment options currently available for AOM patients[9]. Sudden sen
Most studies concerning AOM-associated sudden sensorineural hearing loss are case reports and retrospective in nature[12-14], hence, the etiology of AOM-associated sudden hearing loss has not been fully established. One of the hypotheses is that effusion in the middle ear causes vibration limitation and hypoxia of two windows, which leads to bone conduction hearing loss[15]. Another hypothesis for the sudden deafness is that the toxins released by infection enter the inner ear through the round window membrane (RWM)[16]. Since absorbing the effusion in the middle ear does not completely restore sensorineural hearing loss, the latter hypothesis currently seems more acceptable. Even though AOM-associated sudden hearing loss is a rare otological disorder, if not treated on time, it might cause permanent hearing loss. Therefore, it is important that the disorder is diagnosed early and treated immediately. This study described the audiological features of patients with AOM-associated sudden hearing loss and evaluated the clinical efficacy of tympanostomy tube placement (TTP) and intratympanic methylprednisolone injection after failure of conventional medical therapy.
Patients with AOM-associated sudden hearing loss who visited the Department of Otolaryngology of Beijing Tsinghua Changgung Hospital between October 1, 2018 and June 1, 2020 were enrolled for this retrospective study. Written consent was signed by all the subjects, and this study was approved by the Human Research Ethics Committee of Beijing Tsinghua Changgung Hospital.
The patients were chosen based on following criteria: (1) Age 18–70 years; (2) AOM was diagnosed based on clinical symptoms, pneumatic otoscopy, pure-tone au
Exclusion criteria were as follows: (1) Current administration of oral or topical antibiotics for the affected ear; (2) Steroid treatment within 10 d before enrollment; (3) Previous perforation in the affected ear; (4) Allergic to cefuroxime axetil, cefdinir or moxifloxacin; and (5) Grommet (ventilation tube) i in the affected ear.
All patients underwent myringotomy under local anesthesia, a ventilation tube was placed, and intratympanic injection of methylprednisolone (approximate 0.4 mL, 40 mg/mL) was given once every 3–4 d. The surgical procedures were performed by an experienced physician. The injection was given at most four times and PTA was performed 2 d after the last treatment or when hearing improvement was reported by the subjects.
Pure-tone test: It was conducted by using audiometry (TDH-39P Telephonics headset; Clinical Audiometer AC40, Interacoustics Company, Assens, Denmark, and the B-71 bone vibrator) in a sound-insulated cabin. The frequency-specific threshold was determined as the lowest sound intensity that the patient could hear at the specific frequency. The air conduction thresholds at 0.25, 0.5, 1, 2 and 4 kHz were determined.
Measurement of bone conduction thresholds: A B-71 bone vibrator was placed on the mastoid protrusion of the temporal bone of the subjects. The BC threshold values were determined at 0.25, 0.5, 1, 2 and 4 kHz.
Air–bone gap: The air–bone gap (ABG) was calculated as the difference between the pure-tone bone conduction and air conduction thresholds.
Average hearing at affected frequencies: When the bone conduction threshold was ≥ 20 dB over two or more consecutive frequencies, these frequencies were determined as affected frequencies. An average hearing at the affected frequencies was determined as the average hearing threshold at the corresponding frequencies.
An improvement of ≥ 15 dB of the average hearing threshold at the affected frequencies after treatment was identified as effective, whereas an improvement of < 15 dB was identified as ineffective. A cure was defined as restoring the average hearing threshold at the affected frequencies to the normal hearing levels or the contralateral hearing levels after treatment.
The data were evaluated by using SPSS version 26.0 (Chicago, IL, United States). The data were expressed as mean ± SD. The changes in the hearing threshold values before and after treatment were analyzed by nonparametric test, and the difference was considered statistically significant if P was < 0.05.
Eight patients who met the inclusion criteria were included in the study (Table 1), with an average age of 51.1 ± 13.60 years. All of them were affected in one ear with different degrees of bone conduction hearing loss.
| Case No. | Side of the affected ear | Gender | Age (yr) | Hearing loss | Tinnitus | Curve type | ||||||||
| Left | Right | Male | Female | Yes | No | No | Light | Middle | Severe | A | B | C | ||
| 1 | √ | √ | 37 | √ | √ | √ | ||||||||
| 2 | √ | √ | 38 | √ | √ | √ | ||||||||
| 3 | √ | √ | 47 | √ | √ | √ | ||||||||
| 4 | √ | √ | 63 | √ | √ | √ | ||||||||
| 5 | √ | √ | 59 | √ | √ | √ | ||||||||
| 6 | √ | √ | 67 | √ | √ | √ | ||||||||
| 7 | √ | √ | 34 | √ | √ | √ | ||||||||
| 8 | √ | √ | 64 | √ | √ | √ | ||||||||
| Total | 6 | 2 | 2 | 6 | 51.1 ± 13.60 | 8 | 0 | 6 | 0 | 2 | 0 | 1 | 7 | 0 |
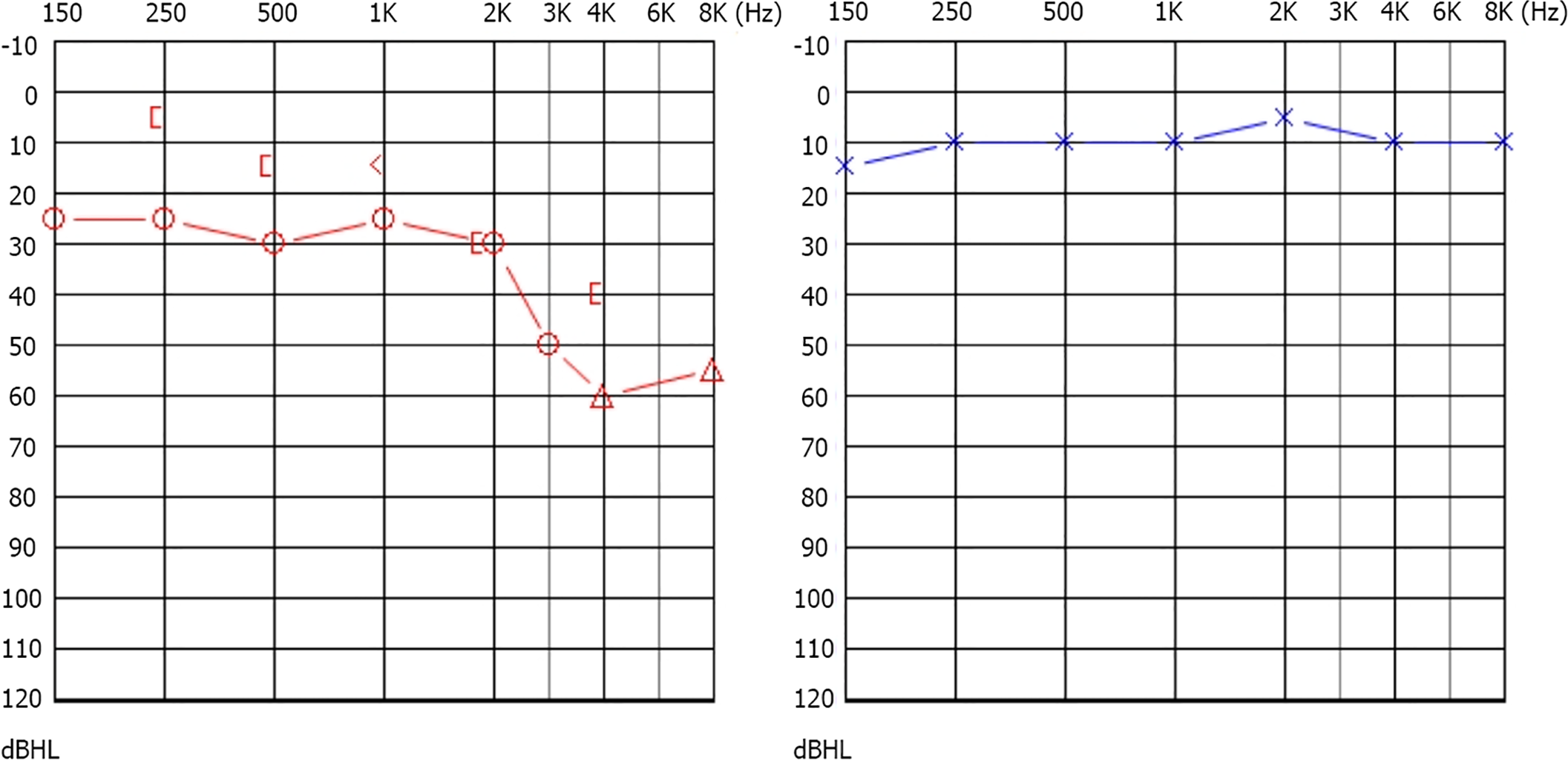
The bone conduction and air conduction threshold values of the affected ears and healthy ears at different frequencies are listed in Table 2. Table 2 shows that the hearing threshold values of the affected ears were significantly higher than those of the contralateral healthy ears over 0.5, 1, 2 and 4 kHz for bone conduction (P < 0.05) and at all frequencies for air conduction. The audiogram data clearly showed that conductive hearing loss was observed at low frequencies, and mixed or sensorineural hearing loss was seen at high frequencies (Figure 1). Bone conduction hearing was impaired at 2 kHz in all patients, i.e., an incidence rate of 100%. The average hearing threshold of the affected frequencies was 37.19 ± 9.49 dB.
| Group | No. | 0.25 kHz, BC | 0.5 kHz, BC | 1 kHz, BC | 2 kHz, BC | 4 kHz, BC |
| Affected ears | 8 | 9.38 ± 5.60 | 17.50 ± 9.63 | 18.75 ± 9.16 | 33.12 ± 12.51 | 39.38 ± 17.41 |
| Healthy ears | 8 | 8.13 ± 5.30 | 13.13 ± 5.30 | 11.25 ± 6.40 | 17.50 ± 8.86 | 22.50 ± 11.34 |
| Z | -0.220 | -1.282 | -1.973 | -2.570 | -2.161 | |
| P | 0.826 | 0.200 | 0.048 | 0.010 | 0.031 | |
| Group | No. | 0.25 kHz, AC | 0.5 kHz, AC | 1 kHz, AC | 2 kHz, AC | 4 kHz, AC |
| Affected ears | 8 | 28.13 ± 11.63 | 31.88 ± 15.34 | 38.75 ± 18.27 | 38.75 ± 16.42 | 56.25 ± 22.16 |
| Healthy ears | 8 | 8.13 ± 5.30 | 13.13 ± 5.30 | 11.25 ± 6.40 | 17.50 ± 8.86 | 22.50 ± 11.34 |
| Z | -2.965 | -2.971 | -3.242 | -2.797 | -2.905 | |
| P value | 0.003 | 0.003 | 0.001 | 0.005 | 0.004 |
The frequency ranges of 0.25–1 kHz and 2–4 kHz were defined as low and high frequencies, respectively. The bone conduction threshold values at low frequencies were close to normal, and hearing loss was observed at high frequencies, with significant difference (P < 0.05) (Table 3). The average ABG was greater in the low frequency group, but the difference between the two groups was not statistically significant (Table 3).
| Group | 0.25-1 kHz | 2-4 kHz | Z | P value |
| Average BC threshold | 15.25 ± 6.52 | 36.25 ± 6.52 | -2.897 | 0.004 |
| Air-bone gap | 16.25 ± 11.64 | 11.56 ± 6.80 | -0.527 | 0.598 |
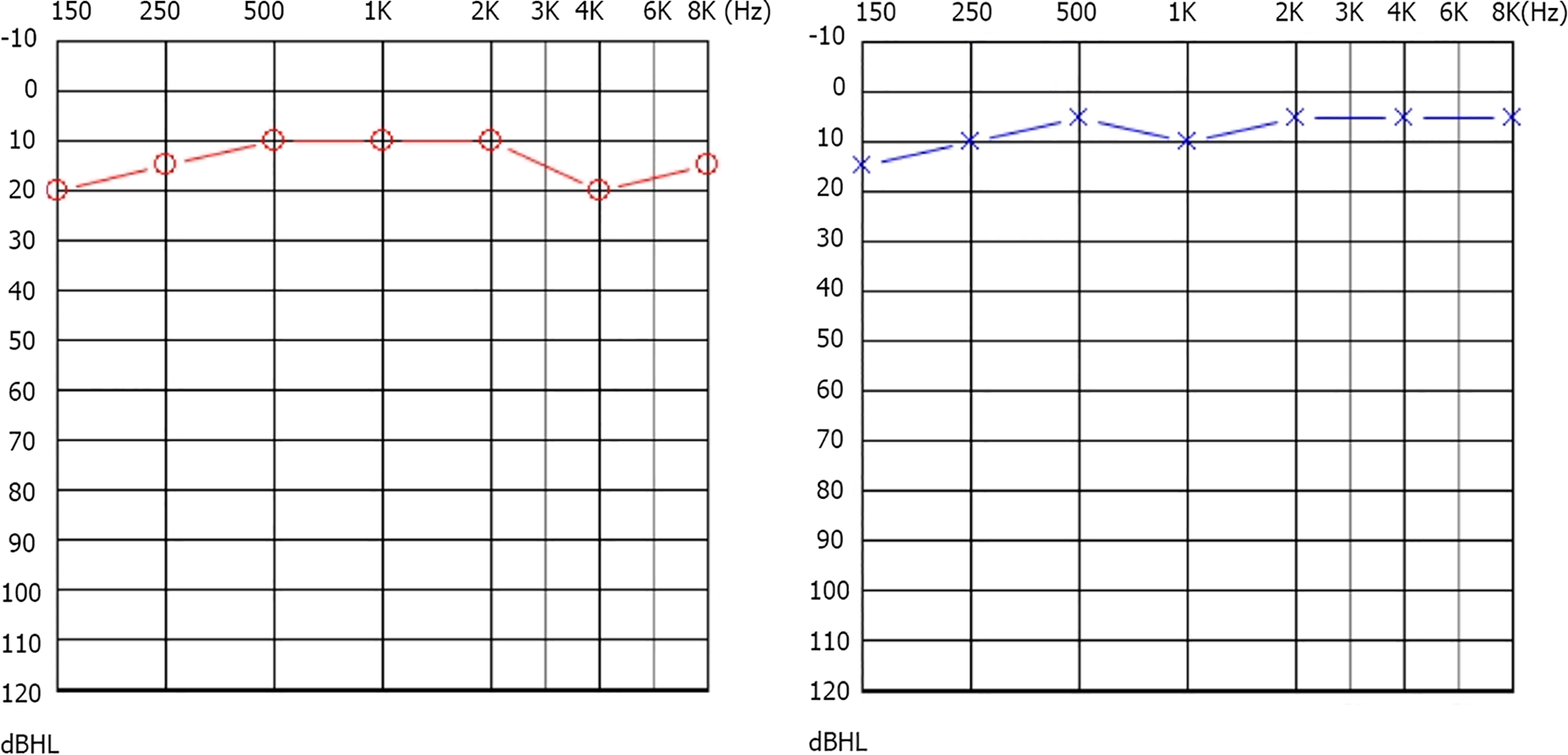
The average interval from disease onset to the start of treatment was 8.63 ± 10.60 d (range, 3–30 d). All eight patients received TTP and intratympanic methylprednisolone injection (the average number of injections was 2), and were cured after treatment. The average hearing threshold value at the affected frequencies post-treatment was significantly lower than the pre-treatment value (P < 0.05), whereas it was not significantly different from that of the healthy ears (P > 0.05) (Table 4). The audi
| Group | Mean hearing threshold at affected frequencies (dB HL) | Z | P value |
| Pre-treatment | 37.19 ± 9.49 | -2.804 | 0.005 |
| Healthy ears | 19.69 ± 7.95 | ||
| Post-treatment | 21.66 ± 9.14 | -0.370 | 0.712 |
| Group | Air-bone gap (dB HL) | Z | P value |
| Pre-treatment | 14.38 ± 9.40 | -3.165 | 0.002 |
| Post-treatment | 3.25 ± 2.71 |
The pathogenesis of sensorineural hearing loss in patients with AOM has been investigated, and the leading proposed theory is that an inflammation induces increased permeability of RWM, which allows the entry of endotoxins and ionic disequilibrium in the cochlea[17]. The bacterial (e.g., Streptococcus pneumoniae) byproducts and inflammatory mediators associated with AOM have been proven to enhance the permeability of RWM and cause subsequent cochlear damage[16,18,19]. It was found that the resulting hearing loss predominantly affected the hearing threshold values at high frequencies, which supports the above-mentioned theory[20]. In this study, it was found that the audiological characteristics of the patients with AOM-associated sudden hearing loss were as follows: ABG at low frequencies and bone conduction hearing loss at high frequencies. These results were in accordance with a previous case report, in which a female patient who was diagnosed with AOM-associated bilateral sudden hearing loss presented with higher hearing threshold values for both bone and air conduction at 2 and 4 kHz frequencies[13]. Despite the similar results reported in several studies, the pathological explanation for the elevation in hearing thresholds at high frequencies following AOM with effusion has not been fully elucidated. It is noteworthy that the prognosis of low frequency hearing loss was demonstrated to be better than that of high frequency. Patients with low frequency hearing loss showed a significantly higher recovery rate (74.1%, 40/54) than those with high frequency hearing loss (45.6%, 26/57) (P < 0.001)[21]. High-frequency hearing loss has also been associated with various symptoms such as deterioration in music perception[22]. In addition, a longitudinal cohort study showed that patients who had chronic sup
Currently, the front-line treatment choices for AOM, according to the guidelines and clinicians, are antibiotics and myringotomy, alone or in combination with ventilation tube placement. Song et al[9] suggested that early myringotomy (with or without placing ventilation tubes) and antibiotics significantly improved clinical outcomes of eight patients with AOM. As for the sudden sensorineural hearing loss, it was recommended by the American Academy of Otolaryngology guidelines that systemic corticosteroids and/or hyperbaric oxygen therapy should be adopted as soon as the diagnosis was made, if needed an intratympanic steroid injection was recommended as a possible salvage therapy[11].
However, there is no standard treatment modality for patients with AOM-associated sudden deafness due to limited evidence and rarity of the disease. In the current study, antibiotics and intravenous methylprednisolone were administered in all eight patients; however, the treatment was ineffective. A combination treatment of TTP and intratympanic methylprednisolone injection was applied as a salvage and exploratory therapy. All the patients in this study showed improvement in BC threshold values at the affected frequencies and showed improvement in ABG. The results were in accordance with a previous study. Seven patients with sen
However, further well-designed studies are needed to verify the findings of the current study as there were some limitations to this study. Firstly, AOM-associated sudden hearing loss is a rare disease in adults, thus, the sample size of this study was too small. Secondly, a control group in which no further treatment was provided after failure of the first treatment was not accommodated in this study. Hence in the future, well-designed studies with a larger sample size are required to further corroborate findings of this study.
In summary, the current case study indicated that AOM may rarely induce sudden sensorineural hearing loss, and high frequencies (2–4 kHz) are often involved. Combination therapy with TTP and intratympanic methylprednisolone injection may be a good salvage treatment modality for patients with AOM-associated sudden hearing loss after failure of conventional treatment.
Acute otitis media (AOM) is a common disease in children, affecting > 80% of children before the age of 3 years. AOM-associated sudden sensorineural hearing loss is a rare otological disorder, and the mechanism and treatment methods remain to be investigated.
If AOM-associated sudden hearing loss is not treated on time, it might cause permanent hearing loss. Therefore, early diagnosis and treatment of AOM-associated sudden hearing loss are important.
This study aimed to describe the audiological features of the patients with AOM-associated sudden hearing loss and evaluate the clinical efficacy of tympanostomy tube placement (TTP) and intratympanic methylprednisolone injection after failure of conventional medical therapy.
Patients with AOM-associated sudden hearing loss who visited the Department of Otolaryngology of Beijing Tsinghua Changgung Hospital between October 1, 2018 and June 1, 2020 and were ineffectively treated by conventional medical therapy were enrolled in this study. Basic data were collected, and pure-tone audiometry was performed to assess the audiological characteristics. Combination therapy with TTP and intratympanic methylprednisolone injection was given to the patients.
Mixed or sensorineural hearing loss was observed at high frequencies (2–4 kHz). All the patients in this study were cured after TTP and intratympanic methylprednisolone. After treatment, the average hearing threshold at affected frequencies was significantly lower than those in the pretreatment group and was similar to those in the healthy ears.
Our study indicated that AOM may rarely induce sudden sensorineural hearing loss, and high frequencies (2–4 kHz) are often involved. Combination therapy with TTP and intratympanic methylprednisolone injection may be a good salvage treatment modality for patients with AOM-associated sudden hearing loss after failure of conventional treatment.
Our study may bring more chances for recovery of patients with AOM-associated sudden hearing loss after failure of conventional treatment. However, our findings remain to be verified by well-designed studies with a large sample size.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Otorhinolaryngology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Byeon H S-Editor: Wu YXJ L-Editor: Kerr C P-Editor: Wu YXJ
| 1. | Leung AKC, Wong AHC. Acute Otitis Media in Children. Recent Pat Inflamm Allergy Drug Discov. 2017;11:32-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Cartel JL, Sechan Y, Boutin JP, Celerier P, Plichart R, Roux JF. Ivermectin for treatment of bancroftian filariasis in French Polynesia: efficacy in man, effect on transmission by vector Aedes polynesiensis. Trop Med Parasitol. 1990;41:241-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 770] [Cited by in RCA: 663] [Article Influence: 51.0] [Reference Citation Analysis (0)] |
| 3. | Vergison A, Dagan R, Arguedas A, Bonhoeffer J, Cohen R, Dhooge I, Hoberman A, Liese J, Marchisio P, Palmu AA, Ray GT, Sanders EA, Simões EA, Uhari M, van Eldere J, Pelton SI. Otitis media and its consequences: beyond the earache. Lancet Infect Dis. 2010;10:195-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 223] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 4. | Marom T, Nokso-Koivisto J, Chonmaitree T. Viral-bacterial interactions in acute otitis media. Curr Allergy Asthma Rep. 2012;12:551-558. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Pagrani M, Srivastava A, Mohan C. Adult onset acute otitis media - a preliminary report. J Evolutio Med Dental Sciences-Jemds. 2014;3:5094-5099. [DOI] [Full Text] |
| 6. | Park JH, Park SJ, Kim YH, Park MH. Sensorineural hearing loss: a complication of acute otitis media in adults. Eur Arch Otorhinolaryngol. 2014;271:1879-1884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Kasemodel ALP, Costa LEM, Monsanto RDC, Tomaz A, Penido NO. Sensorineural hearing loss in the acute phase of a single episode of acute otitis media. Braz J Otorhinolaryngol. 2020;86:767-773. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Margolis RH, Hunter LL. Audiologic evaluation of the otitis media patient. Otolaryngol Clin North Am. 1991;24:877-899. [PubMed] |
| 9. | Song JE, Sapthavee A, Cager GR, Saadia-Redleaf MI. Pseudo-sudden deafness. Ann Otol Rhinol Laryngol. 2012;121:96-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Chandrasekhar SS, Tsai Do BS, Schwartz SR, Bontempo LJ, Faucett EA, Finestone SA, Hollingsworth DB, Kelley DM, Kmucha ST, Moonis G, Poling GL, Roberts JK, Stachler RJ, Zeitler DM, Corrigan MD, Nnacheta LC, Satterfield L. Clinical Practice Guideline: Sudden Hearing Loss (Update). Otolaryngol Head Neck Surg. 2019;161:S1-S45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 391] [Article Influence: 78.2] [Reference Citation Analysis (0)] |
| 11. | Stachler RJ, Chandrasekhar SS, Archer SM, Rosenfeld RM, Schwartz SR, Barrs DM, Brown SR, Fife TD, Ford P, Ganiats TG, Hollingsworth DB, Lewandowski CA, Montano JJ, Saunders JE, Tucci DL, Valente M, Warren BE, Yaremchuk KL, Robertson PJ; American Academy of Otolaryngology-Head and Neck Surgery. Clinical practice guideline: sudden hearing loss. Otolaryngol Head Neck Surg. 2012;146:S1-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 623] [Cited by in RCA: 659] [Article Influence: 50.7] [Reference Citation Analysis (0)] |
| 12. | Heywood RL, Ifeacho SN, Narula AA. Effect of intratympanic steroid administration on sensorineural hearing loss associated with acute otitis media. J Laryngol Otol. 2016;130:532-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Smith A, Gutteridge I, Elliott D, Cronin M. Acute otitis media associated bilateral sudden hearing loss: case report and literature review. J Laryngol Otol. 2017;131:S57-S61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Stenner M, Jecker P, Gouveris H, Mann W. [Treatment of sensorineural hearing loss in acute viral otitis media with intratympanic dexamethasone and hyaluronic acid in comparison with intravenous therapy]. Laryngorhinootologie. 2006;85:32-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Bhutta MF, Lambie J, Hobson L, Williams D, Tyrer HE, Nicholson G, Brown SDM, Brown H, Piccinelli C, Devailly G, Ramsden J, Cheeseman MT. Transcript Analysis Reveals a Hypoxic Inflammatory Environment in Human Chronic Otitis Media With Effusion. Front Genet. 2019;10:1327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Schachern P, Tsuprun V, Cureoglu S, Ferrieri P, Briles D, Paparella M, Juhn S. The round window membrane in otitis media: effect of pneumococcal proteins. Arch Otolaryngol Head Neck Surg. 2008;134:658-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery; Society of Otorhinolaryngology Head and Neck Surgery CMA. [Guideline of diagnosis and treatment of sudden deafness (2015)]. Zhonghua ErBiYanHouTouJing WaiKe ZaZhi. 2015;50:443-447. |
| 18. | Juhn SK, Jung MK, Hoffman MD, Drew BR, Preciado DA, Sausen NJ, Jung TT, Kim BH, Park SY, Lin J, Ondrey FG, Mains DR, Huang T. The role of inflammatory mediators in the pathogenesis of otitis media and sequelae. Clin Exp Otorhinolaryngol. 2008;1:117-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 114] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 19. | Joglekar S, Morita N, Cureoglu S, Schachern PA, Deroee AF, Tsuprun V, Paparella MM, Juhn SK. Cochlear pathology in human temporal bones with otitis media. Acta Otolaryngol. 2010;130:472-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 20. | Cordeiro FP, da Costa Monsanto R, Kasemodel ALP, de Almeida Gondra L, de Oliveira Penido N. Extended high-frequency hearing loss following the first episode of otitis media. Laryngoscope. 2018;128:2879-2884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | Choo OS, Yang SM, Park HY, Lee JB, Jang JH, Choi SJ, Choung YH. Differences in clinical characteristics and prognosis of sudden low- and high-frequency hearing loss. Laryngoscope. 2017;127:1878-1884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Moreno-Gómez FN, Véliz G, Rojas M, Martínez C, Olmedo R, Panussis F, Dagnino-Subiabre A, Delgado C, Delano PH. Music Training and Education Slow the Deterioration of Music Perception Produced by Presbycusis in the Elderly. Front Aging Neurosci. 2017;9:149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Aarhus L, Tambs K, Hoffman HJ, Engdahl B. Childhood otitis media is associated with dizziness in adulthood: the HUNT cohort study. Eur Arch Otorhinolaryngol. 2016;273:2047-2054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |