Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.11095
Peer-review started: July 9, 2021
First decision: July 26, 2021
Revised: August 7, 2021
Accepted: October 27, 2021
Article in press: October 27, 2021
Published online: December 16, 2021
Processing time: 153 Days and 15 Hours
Lingual nerve injury (LNI) is a rare complication following the use of laryngeal mask airway (LMA). The occurrence of this unexpected complication causes uncomfortable symptoms in patients and worsens their quality of life. We present an unusual case of LNI caused by the use of an LMA in percutaneous nephrolithotomy (PCNL).
A 49-year-old man presented to our hospital with a 3-year history of intermittent left lower back pain. Abdominal computed tomography showed a 25 mm × 20 mm stone in the left renal pelvis. PCNL surgery using LMA was performed to remove the renal stone. The patient reported numbness on the tip of his tongue after the operation, but there were no signs of swelling or trauma. The patient was diagnosed with LNI after other possible causes were ruled out. The symptom of numbness eventually improved after conservative medical therapy for 1 wk. The patient completely recovered 3 wk after surgery.
This is the first case report describing LNI with the use of LMA in PCNL. In our case, an inappropriate LMA size, intraoperative movement, and a specific surgical position might be potential causes of this rare complication.
Core Tip: This is the case report of a 49-year-old male patient who reported numbness on the tip of his tongue after a percutaneous nephrolithotomy surgery. A diagnosis of lingual nerve injury caused by laryngeal mask airway (LMA) was made after ruling out other possible causes. The occurrence of this rare complication may be associated with several factors, such as inappropriate LMA size, intraoperative movement, and special surgical position. The patient completely recovered after 3 wk of conservative medical therapy.
- Citation: Wang ZY, Liu WZ, Wang FQ, Chen YZ, Huang T, Yuan HS, Cheng Y. Lingual nerve injury caused by laryngeal mask airway during percutaneous nephrolithotomy: A case report. World J Clin Cases 2021; 9(35): 11095-11101
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/11095.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.11095
Lingual nerve injury (LNI) is an extremely rare complication after general anesthesia and is mostly related to the use of airway devices[1]. LNI commonly manifests as paresthesia, including unilateral or bilateral numbness, altered taste sensation, and loss of gustatory function. Compression of the surrounding tissues due to overinflation of the mask cuff is considered to be the most likely cause of LNI[2]. We report a rare case of LNI after laryngeal mask airway (LMA) use in a kidney stone patient and present a literature review. The patient underwent percutaneous nephrolithotomy (PCNL) to remove stones from the left kidney and reported tongue tip numbness after the surgery. The numbness symptom was thought to be associated with the use of LMA and disappeared after 3 wk of drug therapy.
A 49-year-old male patient was admitted to our clinic with a chief complaint of left lower back pain.
The patient experienced intermittent lower back pain on the left side that worsened when tired. He had a 3-year history of this symptom.
The patient had a history of hypertension that was well controlled by medicine.
The patient was a heavy smoker and smoked at least two packs of cigarettes a day for 30 years. His family history did not reveal anything of significance to the present illness.
The patient’s vital signs were within normal limits. Physical examination revealed percussion tenderness over the left kidney region.
Routine urinalysis revealed a white blood cell count of 61/µL, and the result of the urine culture was negative.
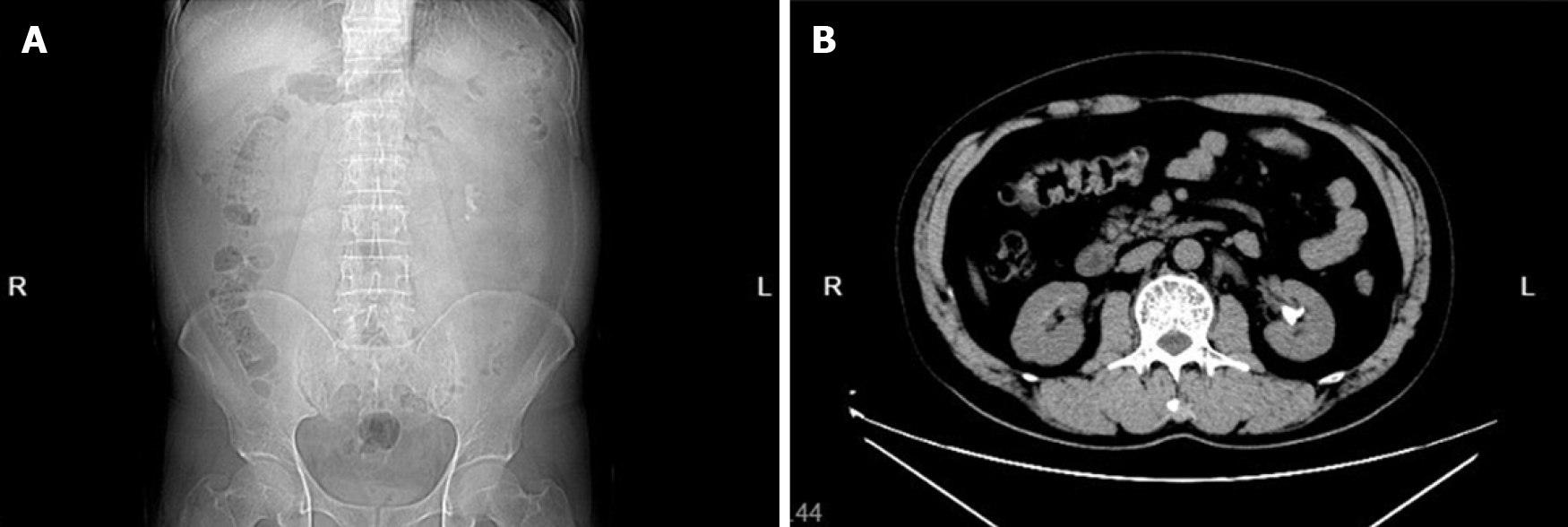
An abdominal computed tomography scan showed a 25 mm × 20 mm stone in the left renal pelvis (Figure 1).
The patient underwent PCNL in a prone position to remove left renal calculi. The operation was performed by a surgeon who had previously performed thousands of PCNL surgeries. The preoperative airway evaluation was normal and revealed Mallampati class I and a full set of normally arranged teeth. After intravenous anesthesia induction, a size 4 LMA (Shanyou Ltd., Hangzhou, Zhejiang Province, China) was successfully inserted and fixed on the first attempt. Continuous intravenous infusion of propofol (6-10 mg/kg/h) was used to maintain anesthesia. Then, the patient was turned over to the prone position, and his head was held in a right-side position during the entire surgical procedure.
The surgery was uneventful and lasted for 80 min. The LMA was removed successfully in the recovery room. The patient found numbness at the tip of his tongue when he returned to the ward. There was no marked swelling, hematoma, or sign of trauma to the tongue or oral cavity (Figure 2). A brain magnetic resonance imaging scan was performed on day 2 postoperatively and showed no abnormalities. We consulted with a neurologist, and no organic disease was found.
According to the patient’s presentation and clinical examinations, the most likely diagnosis was LNI secondary to compression by LMA.
To the best of our clinical judgment, nerve injury in the patient was mild (Sunderland grade I) in severity, and conservative treatment was elected. Neurotrophic drugs could promote the biosynthesis of phospholipids and proteins, which are beneficial for neurological recovery. The patient was treated by oral administration of methylcobalamin and vitamin B1. We communicated with the patient extensively to relieve his anxiety.
The numbness symptom gradually improved after 1 wk. The patient was subsequently discharged to his home and received weekly telephone calls for follow-up. The numbness resolved completely 3 wk after discharge.
Supraglottic airway devices, including classic LMA and other variants, are widely used in general anesthesia surgery. LNI following LMA is an extremely rare complication after general anesthesia. This unexpected complication can cause bothersome symptoms that worsen patients’ quality of life. A retrospective matched case-control study showed that the incidence rate of LNI among patients receiving general anesthesia with airway devices is 0.066%[3]. We found 18 cases of lingual nerve injuries correlated with different LMAs over the last 20 years in the literature (Table 1). The symptoms of LNI appeared immediately after anesthesia to 24 h after surgery. Most patients recovered from their symptoms spontaneously within 6 mo.
| Ref. | Age (yr) | Gender | Weight (kg) | Position | Size of device | Duration of surgery (min) | N2O used | Location | Symptoms | Time of onset | Management | Time to recovery |
| Classic LMA | ||||||||||||
| Koyama et al[8], 2006 | 20 | M | NR | NR | NR | NR | Yes | NR | Taste loss | 24 h | NR | 6 mo |
| Arimune[9], 2007 | 27 | M | NR | Supine | NR | NR | NR | Unilateral | Taste disturbance | NR | NR | |
| Cardoso et al[10], 2007 | 36 | F | 60 | Supine | 3 | 120 | NR | Bilateral | Numbness; Taste disturbance | 1 h | Conservative | 3 wk |
| Fideler and Schroeder[11], 2009 | 32 | F | NR | Supine | 4 | 60 | NR | Unilateral | Numbness; Taste disturbance | Few hours | Conservative | 4 d |
| Inácio et al[12], 2010 | 55 | F | 75 | Supine | 4 | 150 | NR | Bilateral | Numbness; Taste disturbance | 1 h | Conservative | 2 wk |
| Foley et al[4], 2010 | 21 | M | 79 | Supine | 5 | 45 | No | Unilateral | Numbness; Taste disturbance | Few hours | Conservative | 4 wk |
| Foley et al[4], 2010 | 50 | F | 101 | Lithotomy | 3 | 70 | Yes | Unilateral | Numbness | PACU | Conservative | 4 wk |
| El Toukhy and Tweedie[13], 2012 | 36 | F | NR | Supine | 4 | 180 | No | Bilateral | Numbness; Taste disturbance | Few hours | Conservative | 6 wk |
| Dhillon and O’Leary[14], 2012 | 52 | F | NR | Supine | 4 | 60 | No | Bilateral | Numbness; Taste disturbance | Instant | Conservative | 4 wk |
| Present case, 2021 | 49 | M | 75 | Prone | 4 | 80 | No | Unilateral | Numbness | Few hours | Conservative | 3 wk |
| LMA ProSeal | ||||||||||||
| Brimacombe et al[2], 2005 | 61 | M | 74 | Semi-beach chair | 5 | 150 | Yes | Unilateral | Numbness; Taste disturbance | Instant | Conservative | 15 d |
| Brimacombe and Keller[15], 2005 | 64 | F | 76 | Supine | 4 | 45 | No | Unilateral | Numbness | 2 h | Conservative | 10 h |
| LMA Supreme | ||||||||||||
| Rujirojindakul et al[7], 2012 | 43 | F | 65 | Prone | 4 | 75 | No | Tongue tip | Numbness | 24 h | Conservative | 2 wk |
| Thiruvenkatarajan et al[5], 2014 | 45 | F | 61 | Supine | 3 | 105 | No | Tongue tip | Numbness | Instant | Conservative | 3 wk |
| I-gel | ||||||||||||
| Renes et al[16], 2011 | 69 | M | 78 | Supine | 4 | 45 | NR | Bilateral | Numbness; Taste disturbance | Few hours | Conservative | 8 wk |
| Rujirojindakul et al[7], 2012 | 33 | F | 53 | Lithotomy | 3 | 45 | No | Tongue tip | Numbness | 24 h | Conservative | 2 wk |
| Jenkinson et al[17], 2014 | 64 | M | NR | Supine | 4 | 300 | NR | Unilateral | Sensation loss | PACU | NR | 6 wk (90% recovery) |
| Ueshima et al[18], 2016 | 53 | F | 78 | Supine | 4 | NR | NR | Bilateral | Numbness | 24 h | Conservative | 2 wk |
| Mehta et al[19], 2017 | 32 | M | NR | Supine | NR | NR | NR | Unilateral | Numbness | Few hours | Conservative | 6 wk |
The lingual nerve is distributed in the sublingual region, sublingual gland, and anterior two-thirds of the tongue, the latter of which is its main area. It provides taste and tactile sensations to the anterior two-thirds of the tongue through its branches. This nerve originates from the mandibular branch of the trigeminal nerve and carries taste fibers from the chorda tympani. It is superficially located on the distal medial side of the mandibular third molar, with only a thin layer of mucosal tissue covering the surface. It is in front of the inferior alveolar nerve, arching downward along the outside of the hyoglossus muscle to the tongue's inferior surface, which lies directly under the mucosa of the tongue[4]. It is vulnerable to injury when the lingual nerve is located in these superficial positions. LNI presents as paresthesia in the anterior two-thirds of the tongue, including unilateral numbness, altered taste sensation, and loss of gustatory function. Due to the particularity of the lingual nerve distribution area, patients with LNI may also have difficulty chewing and speaking, causing social and psychological complications. It is necessary to differentiate LNI from glossopharyngeal nerve injury, the primary symptom of which is sensory disturbance at the rear of the tongue.
Several risk factors for LNI after general anesthesia have been reported in the literature, including the selection of a small laryngeal mask, the use of nitrous oxide (N2O), and mechanical forces generated by surgical manipulation[1,2,5]. It is necessary to consider the shape and size of the patient’s oropharynx when selecting the LMA size. Using a larger mask in which the cuff is not visible in the back of the mouth and the cuff volume is inflated to the minimum necessary level seems to be an appropriate technique[1]. Using an inappropriate LMA size prevents satisfactory sealing, and too much gas is injected into the mask cuff. The lingual nerve might be compressed and injured by the overfilled cuff. Because of the special physical properties of N2O, it diffuses into the cuff and causes the cuff pressure to increase gradually. It is important to monitor the cuff pressure if N2O is used during surgery. The traction forces resulting from surgical procedures on the head and neck regions place additional stress on the tongue tissue through the airway device, potentially causing LNI.
The diagnosis of LNI mainly depends on a detailed invasive manipulation history and clinical symptoms and signs. Basic neurological assessments such as light touch, pin prick, and two-point discrimination may assist in LNI diagnosis and monitoring. Determining the grade of nerve injury before treatment is the key to successful treatment. Similar to most lingual nerve injuries following LMA, the injury that our patient experienced was considered a grade I injury according to the Sunderland classification[6]. Conservative medication is the most commonly used treatment for LNI following LMA. After 3 wk of drug therapy, the patient achieved complete remission of tongue tip numbness. Most patients fully recover within 4 wk, and no case of permanent nerve injury has been reported in the literature.
Several strategies are suggested to prevent this rare complication. It is vital to select LMA size in the context of not only sex but also other factors, such as oropharynx space, physical stature, and body mass index. The LMA should be inserted gently and carefully fixed. Attention should be given to whether the LMA is displaced when moving the patient; if so, the LMA should be adjusted in time. During the operation, the cuff pressure must be monitored to keep it less than 44 mmHg[7]. If the operation time is long, the LMA should be deflated for 2 min every 1-2 h to improve regional circulation. However, before deflating the LMA, it is necessary to clean up the pharynx secretions and ensure airway patency.
PCNL is an effective surgical method for the treatment of kidney stones. The prone position has been the most widely used position in PCNL surgery, but low comfort and complications are the major drawbacks of this special position. Anesthesia-related complications after prone positioning are associated with many factors, such as changes in heart functions, malposition of airway devices, and excessive movement of the head and neck. To the best of our knowledge, this is the first report describing LNI caused by using an LMA during PCNL. We suspect that there are three possible causes associated with this infrequent complication. First, the size 4 LMA selected may not have been suitable for the patient. For a better sealing effect, excessive gas was injected into the cuff, causing the cuff to excessively expand and compress surrounding tissues. Second, the patient was passively moved from the supine position to the prone position under general anesthesia for surgery. Prolonged retraction of the nerve from positional changes of the body and head is a potential cause of LNI. Third, due to the influence of gravity, the pressure of the pharynx on the LMA in the prone position is greater than that in the supine position. This causes additional inflation of the cuff, which consequently leads to compression of the lingual nerve.
As LMA is widely used during general anesthesia, it is necessary to be aware of this potential rare complication and try to avoid it. In addition to inappropriate LMA size, intraoperative movement and special surgical position may increase the potential for LNI. The nerve injury symptoms usually disappear on their own, and no surgery is needed. Telephone follow-up is necessary, and patients should be reassured that they can recover from their injury completely in a short period.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ferreira GSA, Mastrantonakis K S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Yan JP
| 1. | Thiruvenkatarajan V, Van Wijk RM, Rajbhoj A. Cranial nerve injuries with supraglottic airway devices: a systematic review of published case reports and series. Anaesthesia. 2015;70:344-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Brimacombe J, Clarke G, Keller C. Lingual nerve injury associated with the ProSeal laryngeal mask airway: a case report and review of the literature. Br J Anaesth. 2005;95:420-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Su YK, Wang JH, Hsieh SY, Liu XZ, Lam CF, Huang SC. Incidence and risk factors for postoperative lingual neuropraxia following airway instrumentation: A retrospective matched case-control study. PLoS One. 2018;13:e0190589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Foley E, Mc Dermott TE, Shanahan E, Phelan D. Transient isolated lingual nerve neuropraxia associated with general anaesthesia and laryngeal mask use: two case reports and a review of the literature. Ir J Med Sci. 2010;179:297-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Thiruvenkatarajan V, Van Wijk RM, Elhalawani I, Barnes AM. Lingual nerve neuropraxia following use of the Laryngeal Mask Airway Supreme. J Clin Anesth. 2014;26:65-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Sunderland S. A classification of peripheral nerve injuries producing loss of function. Brain. 1951;74:491-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 911] [Cited by in RCA: 822] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 7. | Rujirojindakul P, Prechawai C, Watanayomnaporn E. Tongue numbness following laryngeal mask airway Supreme™ and i-gel™ insertion: two case reports. Acta Anaesthesiol Scand. 2012;56:1200-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Koyama T, Ichizawa A, Fukami N, Arai K, Hirata S, Mishima S. [Taste loss following the use of the laryngeal mask airway]. Masui. 2006;55:445-446. [PubMed] |
| 9. | Arimune M. [Taste disturbance after general anesthesia with classic laryngeal mask airway (CLM)]. Masui. 2007;56:820-821. [PubMed] |
| 10. | Cardoso HE, Kraychete DC, Lima Filho JA, Garrido LS, Rocha AP. [Temporary lingual nerve dysfunction following the use of the laryngeal mask airway: report]. Rev Bras Anestesiol. 2007;57:410-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Fideler FJ, Schroeder TH. Cranial nerve injuries from a laryngeal mask airway. Eur J Anaesthesiol. 2009;26:980-981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Inácio R, Bastardo I, Azevedo C. Lingual Nerve Injury: a complication associated with the classic laryngeal mask airway? Int J Anesthesiol. 2010;2. |
| 13. | El Toukhy M, Tweedie O. Bilateral lingual nerve injury associated with classic laryngeal mask airway: a case report. Eur J Anaesthesiol. 2012;29:400-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Dhillon SS, O'Leary K. Lingual nerve paralysis after endobronchial ultrasound utilizing laryngeal mask airway. J Bronchology Interv Pulmonol. 2012;19:72-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Brimacombe J, Keller C. Salivary gland swelling and lingual nerve injury with the ProSeal laryngeal mask airway. Eur J Anaesthesiol. 2005;22:954-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Renes SH, Zwart R, Scheffer GJ, Renes S. Lingual nerve injury following the use of an i-gel laryngeal mask. Anaesthesia. 2011;66:226-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Jenkinson A, Crosher R, Mohammed-Ali R, Parsons K. Lingual nerve injury following use of a supraglottic airway device. Br J Oral Maxillofac Surg. 2014;52:279-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Ueshima H, Okumura N, Otake H. Lingual nerve palsy after i-gel® use. J Anesth. 2016;30:1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Mehta M, Ramasamy P, Mushambi MC, Gauthama P. Unilateral lingual and hypoglossal nerve palsies following use of I-gel for failed intubation. Int J Obstetric Anesth. 2017;31:S60. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |