Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.11056
Peer-review started: June 10, 2021
First decision: July 15, 2021
Revised: July 28, 2021
Accepted: September 16, 2021
Article in press: September 16, 2021
Published online: December 16, 2021
Processing time: 182 Days and 21.2 Hours
Low-grade appendiceal mucinous neoplasm (LAMN) is extremely rare and easily misdiagnosed before surgery.
We report the treatment of an asymptomatic case of LAMN diagnosed by magnetic resonance imaging (MRI) and surgical findings. A 70-year-old woman presented with an adnexal mass found by physical examination in July 2020. Gynecologic ultrasonography revealed a cystic mass in the right adnexa, and computed tomography showed a cystic mass in the pelvic cavity. All tumor markers were normal. A further MRI examination suggested mucinous neoplasm in the right pelvic cavity, excluding the possibility of adnexal cyst. Laparoscopic exploration found a huge cystic mass of about 10 cm × 7 cm that originated from the apex of the appendix, with spontaneous rupture. LAMN was confirmed by pathological examination. As of May 2021, no disease recurrence occurred after an open appendectomy.
This case indicates that we should pay more attention to female patients who are clinically diagnosed with an adnexal mass at admission,. The physical examination should be done carefully, and the laboratory and imaging examination results should be comprehensively analyzed to avoid misdiagnosis and to ensure prompt diagnosis and treatment, and to improve prognosis. MRI may be a better option for the diagnosis of appendiceal mucinous neoplasm.
Core Tip: Low-grade appendiceal mucinous neoplasm (LAMN) is extremely rare and easily misdiagnosed before surgery. We report the treatment of an asymptomatic case of LAMN diagnosed by magnetic resonance imaging and surgical findings. This case indicates that we should pay more attention to female patients who are clinically diagnosed with an adnexal mass at admission,. The physical examination should be done carefully, and the laboratory and imaging examination results should be comprehensively evaluated to avoid misdiagnosis and ensure prompt diagnosis and treatment, and to improve prognosis.
- Citation: Xu R, Yang ZL. Treatment of a giant low-grade appendiceal mucinous neoplasm: A case report. World J Clin Cases 2021; 9(35): 11056-11060
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/11056.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.11056
Low-grade appendiceal mucinous neoplasm (LAMN) is a rare heterogeneous disease, characterized by well-differentiated tumors. It is often complicated by spontaneous or iatrogenic rupture that results in pseudomyxoma or distant metastasis of the abdominal wall, which can be life threatening[1]. LAMN is easily misdiagnosed because most patients are asymptomatic. It is generally found during the surgery because of the difficulty of preoperative diagnosis. Here, we report a case of LAMN diagnosed by magnetic resonance imaging (MRI) and surgical findings.
The patient presented with an adnexal mass found by physical examination more than 1 mo previously.
On August 23, 2020, a 70-year-old postmenopausal woman who presented with an adnexal mass found by physical examination 1 mo previously was admitted to the department of gynecology at our hospital. She did not complain of any clinical symptoms or discomfort.
The past medical history was unremarkable. One month prior, a right adnexal mass was found by ultrasonography at the local hospital.
The patient had no remarkable personal or family history.
Upon arrival at our hospital, the patient was well-nourished, and without pain, pallor, or jaundice. Abdominal examination revealed distension without tenderness.
Laboratory examination demonstrated found hemoglobin: 10.3 g/dL, leucocyte count: 4.86 × 109/L, hematocrit: 31.7%, and platelet count: 210 × 109/L. Liver and renal function tests, and the coagulation profile were all within normal ranges. Cancer antigen markers including carcinoembryonic antigen and carbohydrate antigen 19.9 were all within normal ranges.
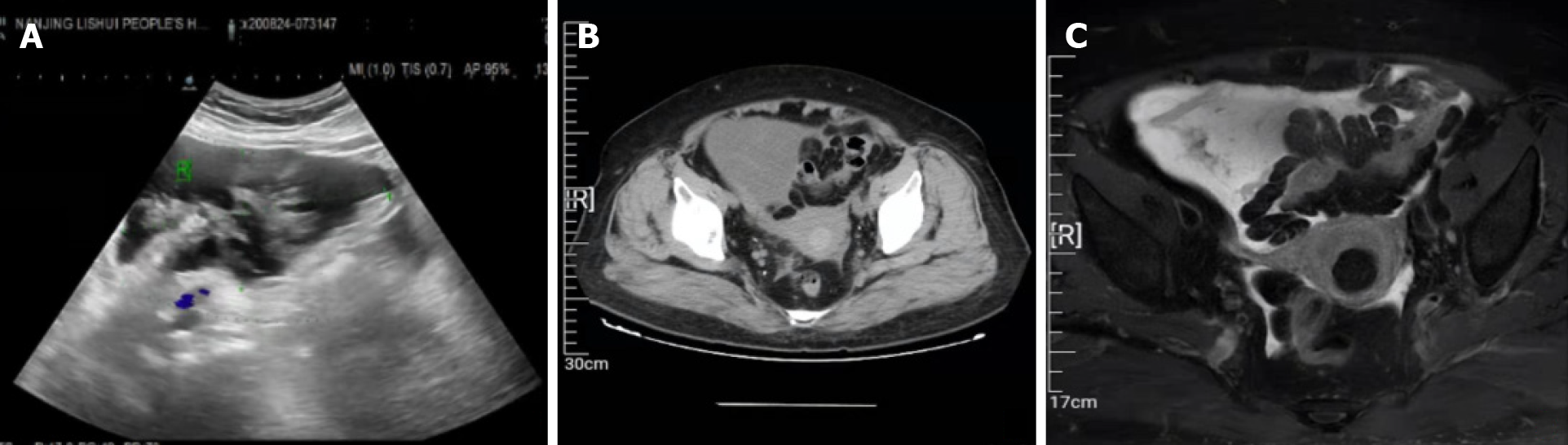
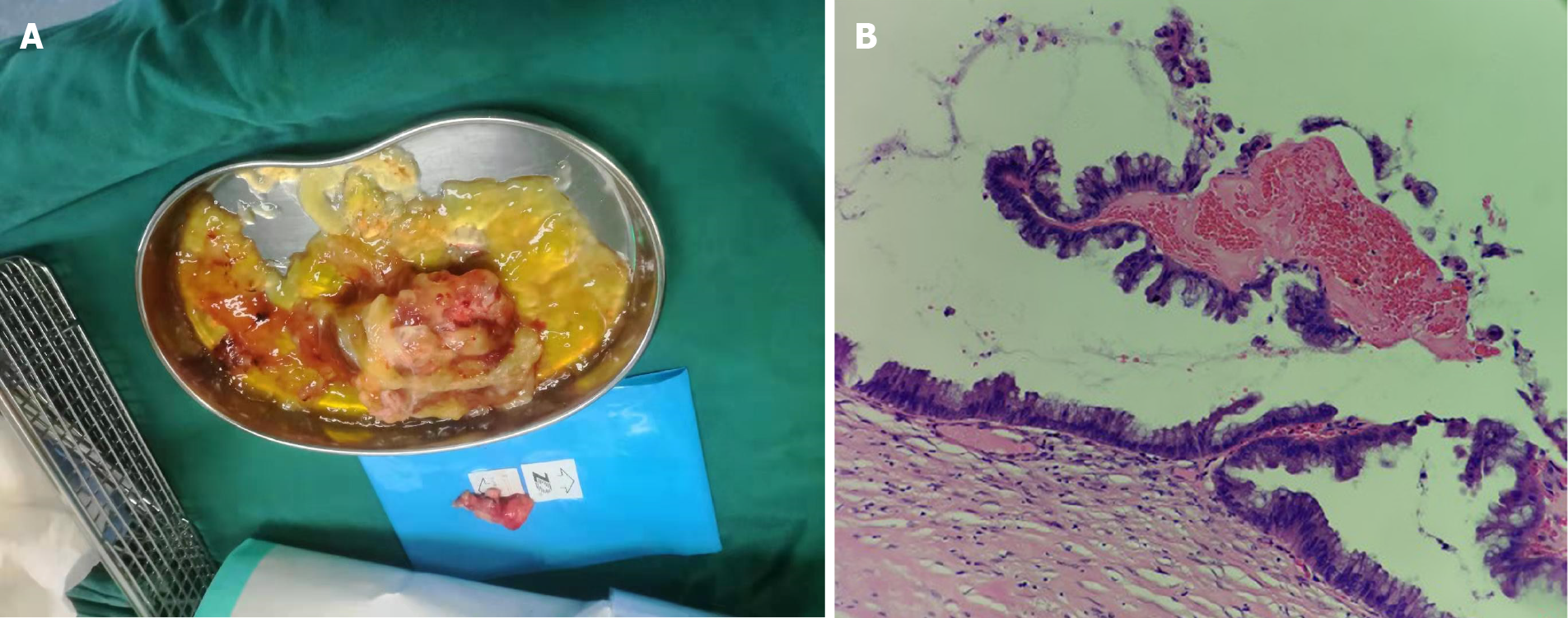
B-ultrasound re-examination at our hospital showed a small amount of pelvic effusion (122 mm × 64 mm) in the right adnexal area (Figure 1A). No tenderness or rebound pain was found in the lower abdomen, and a mass of about 12 cm × 6 cm in the pelvic cavity with a tough texture and low mobility was detected by palpation. Whole abdomen computed tomography (CT) showed a small amount of effusion in the pelvic cavity, with lesions on the right (Figure 1B). The irregular cyst wall and thick soft tissue seen in the CT image might have resulted from tumor transformation. However the tumor markers were all normal. An MRI examination suggested a mucinous neoplasm in the right pelvic cavity (Figure 1C). It was not clear whether the neoplasm originated from abdominal mesodermal tissue or the appendix. The patient was transferred to the general surgery department. During laparoscopic exploration, a large amount of jelly-like mucosubstance was found in the right lower abdomen and pelvic cavity, and a huge cystic mass of about 10 cm × 7 cm originating from the apex of the appendix were found (Figure 2A).
Giant low-grade appendiceal mucinous neoplasm.
An open appendectomy was performed, followed by peritoneal lavage and drainage. Postoperative pathological examination revealed a LAMN (Figure 2B). Anti-infective and symptomatic treatments were given after surgery; no obvious abnormalities was found on whole abdomen CT.
Tumor markers and a colonoscopy performed 3 mo after surgery were all normal. No disease recurrence or other conditions were found on follow-up in May 2021.
Appendiceal mucinous neoplasm accounts for 8%-10% of appendiceal tumors and 58% of malignant appendiceal tumors. The incidence is 0.2%-0.3% in patients who underwent appendectomy. LAMN is a borderline or low-grade malignant tumor, regardless of rupture, and is characterized by implantation metastasis and a rate of recurrence rate[2-4]. Its pathogenesis involves atypical hyperplasia of the glandular appendix epithelium that obstructs the appendix with a gradual accumulation of mucus resulting in increased pressure. Mucus penetrates the muscularis mucosa and produces mucinous masses around the appendix and in the retroperitoneum[5,6]. Most cases are asymptomatic, and in the absence of acute infection, the symptoms and signs of LAMN resemble those of chronic appendicitis. A correct diagnosis may be difficult, but on physical examination large tumors can be found as a complete oval mass with no surrounding adhesions. An appendiceal mucinous cyst that forms from an appendiceal lesion can easily be misdiagnosed as a common appendiceal abscess, right adnexal cyst, and so on[7,8]. A recent case report described a patient with LAMN that was initially diagnosed as an ovarian tumor[9]. As in this case, an appendiceal mucinous neoplasm should still be taken into consideration even if the tumor marker results are negative.
Abdominal ultrasound and CT are auxiliary diagnostic methods that can distinguish appendiceal mucinous cysts from other lesions before surgery[10,11]. Color Doppler ultrasound for mucinous cystadenoma of the appendix shows a dark liquid area in the appendix, with a small number of small flocculent light spots. Ultrasound exhibits better sound transmission, a round or oval shape, and smooth wall. There were no findings suggestive of LAMN by echo. CT is a more accurate imaging method for the diagnosis of appendiceal mucinous neoplasms, and shows a cystic mass closely adjacent to the cecum, with a round or long tubular shape, thin wall, and a smooth and regular outline, suggesting LAMN. When CT shows an irregular cyst wall and thick soft tissue, it is more likely to be malignant[10]. In this case, gynecologic ultrasonography revealed a cystic mass in the right adnexa, and CT showed a cystic mass in the pelvic cavity. However, there was still a possibility that it was an adnexal cyst. MRI performed with a variety of sequences and scanning methods, and high tissue resolution can clearly and consistently distinguish the wall and fluid of the appendiceal mucinous cyst, and more accurately show the integrity and boundary of the cyst wall. In this case, additional MRI evaluation showed typical manifestations of appendiceal cysts. The lesion was located in the right lower abdomen, had a with clear boundary, and was closely related to the cecum, which showed changes in external pressure. MRI had uniform long T1 and long T2 signals, and the cyst wall was thin and uniform, with similar signals to those of the intestinal wall. The cross section of the mass was round or elliptical, and the sagittal or coronal plane presented as a long tubular or gourd-shaped structure[12,13]. We thus successfully excluded the possibility of adnexal cyst by MRI. Subsequent surgery and pathological examination finally confirmed the diagnosis of LAMN.
Surgery is still the only treatment option for appendiceal mucinous neoplasms. Iatrogenic rupture of the tumor should be avoided during surgery to reduce the risk of implantation metastasis and disease recurrence. Unfortunately, preoperative abdominal ultrasound and CT examinations had shown effusion in the pelvic cavity. Spontaneous rupture of the tumor and the spread of mucus to the abdominal cavity were observed during laparoscopic exploration, indicating that the patient might have a relatively high risk of disease recurrence. Open surgery was performed after finding the spontaneous rupture of the tumor. Although appendectomy and peritoneal lavage and drainage were performed, and a negative incision margin was obtained, postoperative follow-up should be continued for a long time. Chen et al[14] reported a patient with recurrence of appendix mucinous adenocarcinoma at 26 mo after appendectomy.
LAMN is a rare clinical or imaging diagnosis. The female appendix is adjacent to the adnexa, which may lead to a misdiagnosis of either an appendiceal cyst or adnexal mass. The diagnosis and treatment of this patient suggested that for female patients who are clinically diagnosed with an adnexal mass at admission, we must broaden our minds and look further. Diagnosis should not be limited to the common diseases that we are familiar with. The physical examination should be done carefully, and the laboratory and imaging examination results should be comprehensively analyzed to reduce the possibility of misdiagnosis and to ensure prompt diagnosis and treatment, and to improve patient prognosis. MRI may be a better option for the diagnosis of appendiceal mucinous neoplasms.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Gastroenterology and Hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kitagawa Y, Samara AA S-Editor: Wang JL L-Editor: Filipodia P-Editor: Guo X
| 1. | Shaib WL, Assi R, Shamseddine A, Alese OB, Staley C 3rd, Memis B, Adsay V, Bekaii-Saab T, El-Rayes BF. Appendiceal Mucinous Neoplasms: Diagnosis and Management. Oncologist. 2017;22:1107-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 134] [Article Influence: 16.8] [Reference Citation Analysis (3)] |
| 2. | Ramaswamy V. Pathology of Mucinous Appendiceal Tumors and Pseudomyxoma Peritonei. Indian J Surg Oncol. 2016;7:258-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (2)] |
| 3. | Motsumi MJ, Motlaleselelo P, Ayane G, Sesay SO, Valdes JR. A case report of a giant appendiceal mucocele and literature review. Pan Afr Med J. 2017;28:106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Padmanaban V, Morano WF, Gleeson E, Aggarwal A, Mapow BL, Stein DE, Bowne WB. Incidentally discovered low-grade appendiceal mucinous neoplasm: a precursor to pseudomyxoma peritonei. Clin Case Rep. 2016;4:1112-1116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Pai RK, Longacre TA. Appendiceal mucinous tumors and pseudomyxoma peritonei: histologic features, diagnostic problems, and proposed classification. Adv Anat Pathol. 2005;12:291-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 127] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | Rampone B, Roviello F, Marrelli D, Pinto E. Giant appendiceal mucocele: report of a case and brief review. World J Gastroenterol. 2005;11:4761-4763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 57] [Cited by in RCA: 56] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Aleter A, El Ansari W. Incidental appendiceal mucinous neoplasm mimicking a left adnexal mass: A case report. Int J Surg Case Rep. 2020;74:132-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Omari AH, Khammash MR, Qasaimeh GR, Shammari AK, Yaseen MK, Hammori SK. Acute appendicitis in the elderly: risk factors for perforation. World J Emerg Surg. 2014;9:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 82] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 9. | Perivoliotis K, Christodoulidis G, Samara AA, Sgantzou IK, Floros T, Volakakis G, Karasavvidou F, Tepetes K. Low-Grade Appendiceal Mucinous Neoplasm (LAMN) Primarily Diagnosed as an Ovarian Mucinous Tumor. Case Rep Surg. 2021;2021:5523736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Yang JM, Zhang WH, Yang DD, Jiang H, Yu L, Gao F. Giant low-grade appendiceal mucinous neoplasm: A case report. World J Clin Cases. 2019;7:1726-1731. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Cubro H, Cengic V, Burina N, Kravic Z, Beciragic E, Vranic S. Mucocele of the appendix presenting as an exacerbated chronic tubo-ovarian abscess: A case report and comprehensive review of the literature. Medicine (Baltimore). 2019;98:e17149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Pickhardt PJ, Levy AD, Rohrmann CA Jr, Kende AI. Primary neoplasms of the appendix: radiologic spectrum of disease with pathologic correlation. Radiographics. 2003;23:645-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 202] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 13. | Tirumani SH, Fraser-Hill M, Auer R, Shabana W, Walsh C, Lee F, Ryan JG. Mucinous neoplasms of the appendix: a current comprehensive clinicopathologic and imaging review. Cancer Imaging. 2013;13:14-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 90] [Article Influence: 7.5] [Reference Citation Analysis (1)] |
| 14. | Chen W, Ye JW, Tan XP, Peng X, Zhang Y, Liang JL, Huang MJ. A case report of appendix mucinous adenocarcinoma that recurred after additional surgery and a brief literature review. BMC Surg. 2020;20:182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |