Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.11043
Peer-review started: June 9, 2021
First decision: July 16, 2021
Revised: July 27, 2021
Accepted: September 15, 2021
Article in press: September 15, 2021
Published online: December 16, 2021
Processing time: 184 Days and 0.5 Hours
Pneumothorax is one of the most common causes of acute dyspnea. In patients under general anesthesia, the symptoms may not be obvious, which may delay diagnosis and treatment. Computed tomography is the gold standard for the diagnosis of pneumothorax, but is not suitable for rapid diagnosis of this complication. In contrast, lung ultrasonography can provide rapid diagnosis and treatment of pneumothorax.
The patient was a 53-year-old man admitted for rupture of the spleen caused by an accidental fall and emergency splenectomy was planned. Anesthesia was induced, and tracheal intubation was performed successfully with a video laryngoscope. About 2 min after tracheal intubation, the airway peak pressure increased to 50 cm H2O and the oxygen saturation dropped to 70%. According to the BLUE protocol, a recommended area of the chest was scanned by ultrasound. The pleural slide sign disappeared and obvious parallel line sign could be seen in the left lung. The boundary of pneumothorax (lung points) were rapidly confirmed by ultrasound. To avoid lung injury, a closed thoracic drainage tube was placed in the involved area. On day 9 after surgery, the patient was discharged from the hospital without any complications.
Perioperative pneumothorax is rare but dangerous. It can be rapidly diagnosed and treated with ultrasound guidance.
Core Tip: Perioperative pneumothorax is a rare but dangerous complication that req
- Citation: Zhang G, Huang XY, Zhang L. Ultrasound guiding the rapid diagnosis and treatment of perioperative pneumothorax: A case report. World J Clin Cases 2021; 9(35): 11043-11049
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/11043.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.11043
Pneumothorax is one of the most common causes of acute dyspnea. Sudden chest pain, shortness of breath, or even respiratory failure are the main clinical features. Because of the sudden change in pressure in the pleural cavity, the venous return blood flow is blocked and the stability of the circulatory system is affected. Therefore, early diagnosis and treatment are urgently needed. In patients under general anesthesia, the symptoms may not be obvious, which can delay diagnosis and treatment. Pneumothorax is a rare but serious perioperative complication leading to perilous hypoxemia during general anesthesia. Especially for patients with poor cardiopulmonary reserve, early diagnosis has a great impact on the prognosis[1].
Although chest computed tomography (CT) is the gold standard for the diagnosis of pneumothorax[2], it is not suitable for rapid diagnosis because of its high radiation exposure and long transport time. In contrast, lung ultrasound (LUS) has the adva
It was first reported that pneumothorax can be diagnosed by ultrasound in 1987. Wernecke et al[4] reported that it can be indicated by the disappearance of lung sliding. When pneumothorax is suspected during surgery, ultrasound scanning can be performed rapidly in the suspected area following the BLUE protocol[5]. Abnormal sonographic signs such as the pleural slide sign, parallel line sign in M-mode, and lung points indicate pneumothorax. Moreover, lung points can not only be a gold standard for the diagnosis of pneumothorax, but also determine the boundary of the pneumothorax and guide the placement of a closed thoracic drainage tube. It takes 2-3 min to complete the examination, and pneumothorax can be excluded or diagnosed within 1 min[6]. In this case, the prompt ultrasound diagnosis and treatment of pneumothorax resulted in an excellent patient prognosis.
A 53-year-old man (85 kg and 170 cm) was admitted for rupture of spleen caused by an accidental fall.
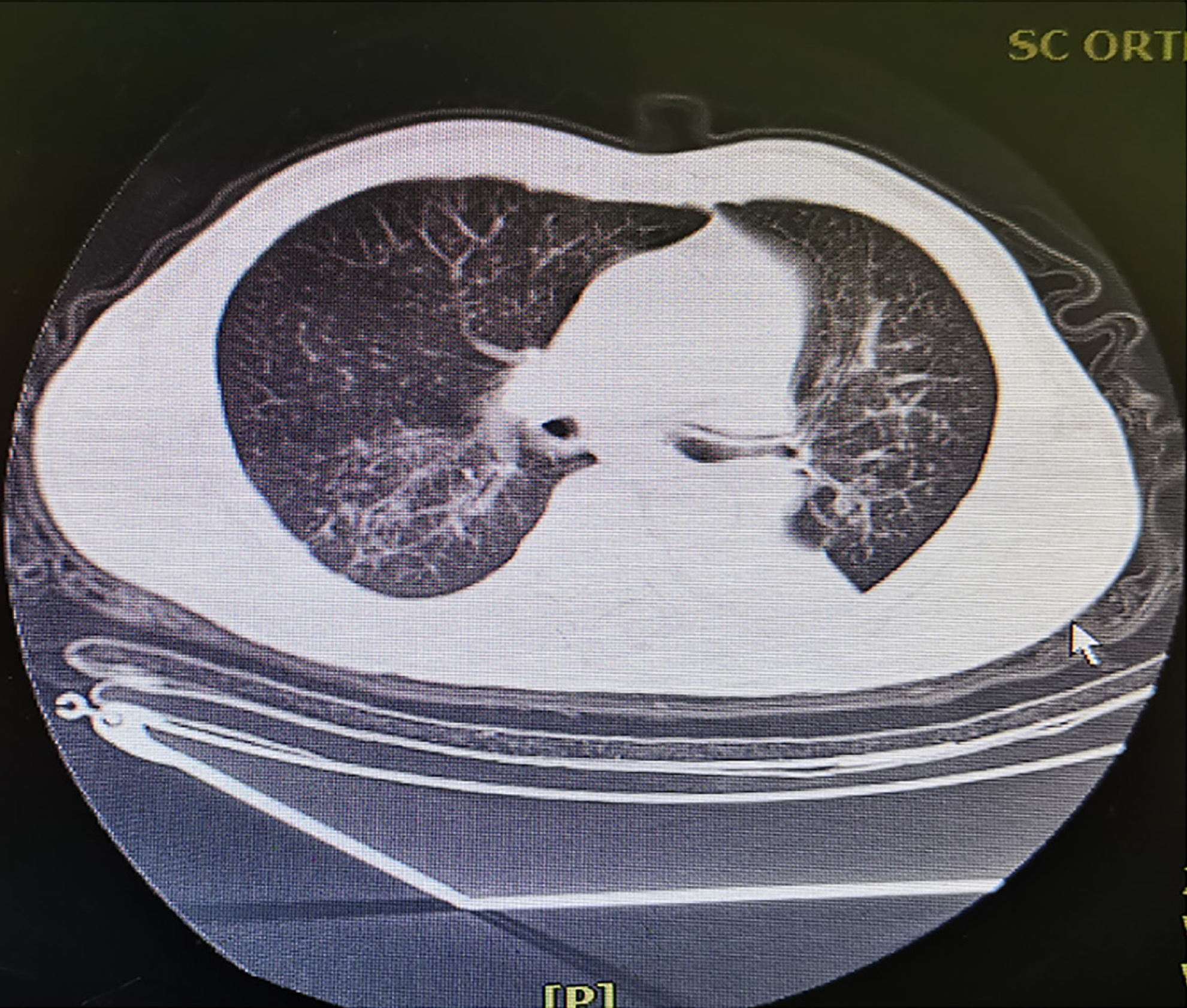
Emergency splenectomy was planned under general anesthesia. Preoperative emergency ultrasound examination including the heart, chest, and abdomen were performed, and it was found that spleen had been ruptured and was accompanied by active bleeding, complicated with progressive hemochrome reduction, which was the main reason for the patient to undergo emergency surgery. Preoperative ultrasound showed no heart or chest abnormalities. The patient did not complain of dyspnea preoperatively, and preoperative CT showed no hemothorax or pneumothorax (Figure 1). Initial vital signs before anesthesia were a blood pressure of 126/82 mm Hg, heart rate of 75 bpm, and an oxygen partial pressure (SpO2) of 95% while inhaling air. Anesthesia was induced with sufentanil 0.3 µg/kg, rocuronium 0.1 mg/kg, and propofol 3 mg/kg. Tracheal intubation was successfully performed with video laryngoscopy, and positive pressure ventilation was performed with an airway peak pressure of 14 cm H2O. Because the patient's thick chest wall, breath sounds were difficult to auscultate. About 2 min after tracheal intubation, it was difficult to ventilate. The airway peak pressure increased progressively, reaching a maximum of 50 cm H2O and SpO2 dropped, reaching a minimum of 70%. Because of obesity and the thick chest wall, the cause of respiratory failure could not be determined by traditional auscultation. Following the BLUE protocol, a recommended area of the chest was scanned by bedside ultrasound. The pleural slide sign disappeared in the upper and lower blue points of the left lung, and in M-mode, an obvious parallel line sign could be seen below the pleura. The boundary of pneumothorax (lung points) was rapidly confirmed by ultrasound. To avoid lung injury and secondary pneumothorax, a closed thoracic drainage tube was placed in the area guided by ultrasound. The interval from suspicion of pneumothorax to placement of the drainage tube was less than 3 min. After many bubbles had emerged from the water seal bottle, the airway pressure dropped to 20 cm H2O and the SpO2 returned to 96%-100%. After the patient's vital signs stabilized, the splenectomy continued and was successfully completed. The patient was sent to the intensive care unit (ICU) with a endotracheal tube for further treatment after surgery. On day 1 after surgery, the endotracheal tube was removed. On day 6, the closed thoracic drainage tube was removed. On day 9, the patient was disc
Anemia (hemoglobin 85 g/L).
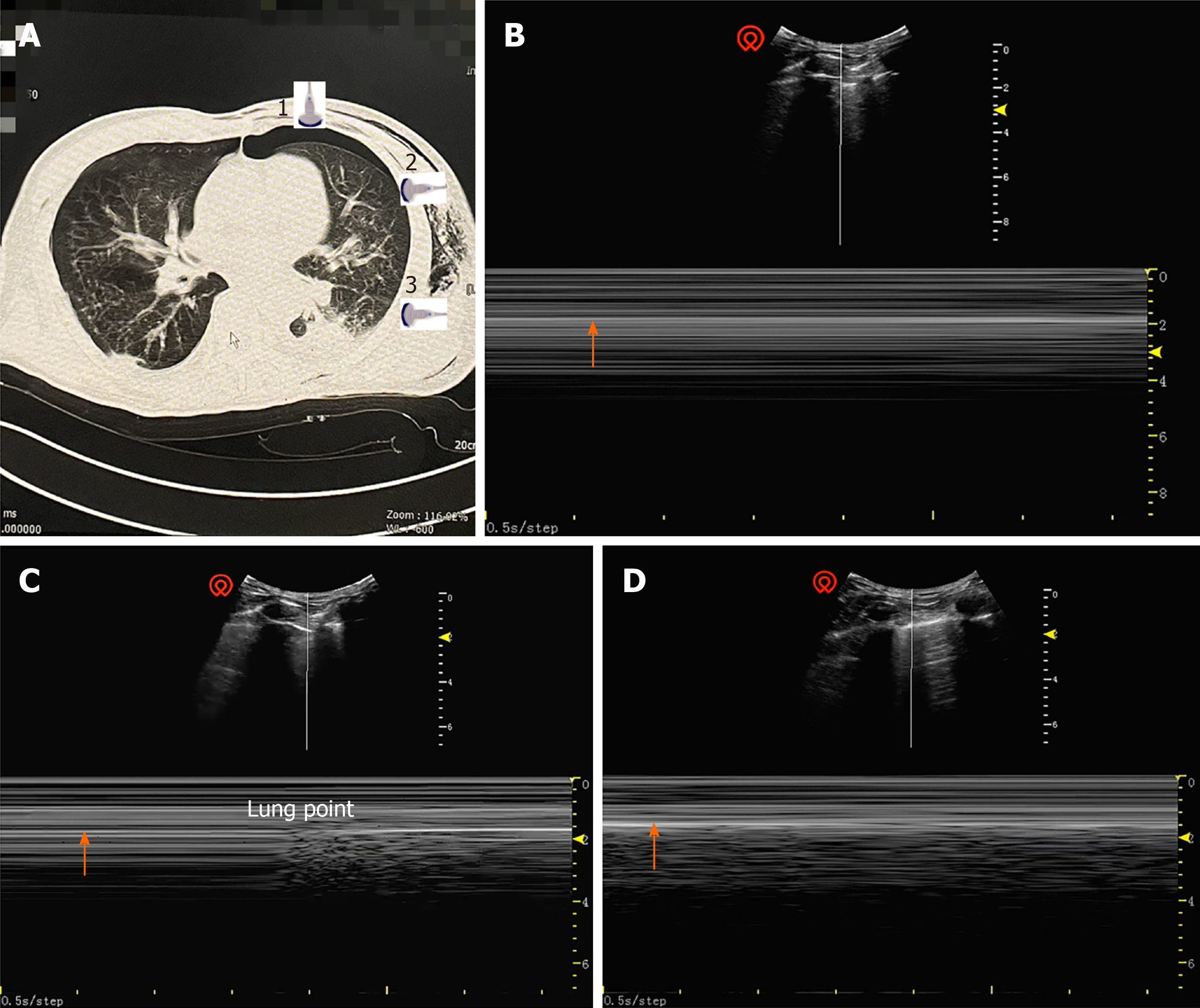
Focused assessment with sonography in trauma (FAST) has been extensively utilized and studied in blunt and penetrating trauma[7]. Following the FAST protocol, organ damage can be rapidly evaluated by the amount of free fluid in the chest, abdominal, and pelvic cavities. In this case, preoperative emergency ultrasound examination of the heart, chest and abdomen found that spleen had been ruptured and active bleeding was complicated by progressive hemochrome reduction, which was also the main reason for the patient to undergo emergency surgery. Preoperative ultrasound showed no abnormalities in the heart or chest. Following the BLUE protocol, LUS confirmed that the pleural slide sign had disappeared in the recommended area of the left lung, and in M-mode, an obvious parallel line sign was seen below the pleura (Figure 2B). The boundary of the pneumothorax (lung points) was rapidly confirmed by ultrasound (Figure 2C).
A clear diagnosis perioperative pneumothorax was based on imaging examination and intraoperative findings.
To avoid lung injury and secondary pneumothorax, a closed thoracic drainage tube was placed in the area guided by ultrasound. From suspicion of pneumothorax to the placement of closed thoracic drainage tube, the total time was less than 3 min.
After a large number of bubbles emerged from the water seal bottle, the airway pressure dropped to 20 cm H2O and the oxygen saturation returned to 96%-100%. After the patient's vital signs stabilized, the splenectomy continued and was successfully completed. The patient was sent to ICU with a endotracheal tube for further treatment after surgery. On day 1 after surgery, the endotracheal tube was removed. On day 6, the drainage tube was removed. On day 9, the patient was discharged from the hospital without any complications.
If pneumothorax occurs under general anesthesia, positive pressure ventilation causes accumulation of a large amount of air in the pleural space, leading intractable hypoxemia. Because of absence of specific symptoms like chest pain, cough, and dyspnea under general anesthesia, pneumothorax may be not diagnosed promptly. Pathological changes leading by pneumothorax can provide a large amount of diagnostic information. Because of the high sensitivity of CT, it is the gold standard for the diagnosis of pneumothorax. However, patients often require long-distance transport for CT examination, which is time-consuming and risky for critical patients. It is not suitable for the rapid diagnosis required for perioperative pneumothorax. Ultrasound is a reliable modality to provide rapid and accurate information, it has been shown that pulmonary ultrasound is superior to X-ray for the diagnosis of lung disease[8]. The diagnostic accuracy of ultrasound for a variety of lung diseases is comparable to CT, and it is becoming the preferred tool for rapid assessment of pulmonary disease[9].
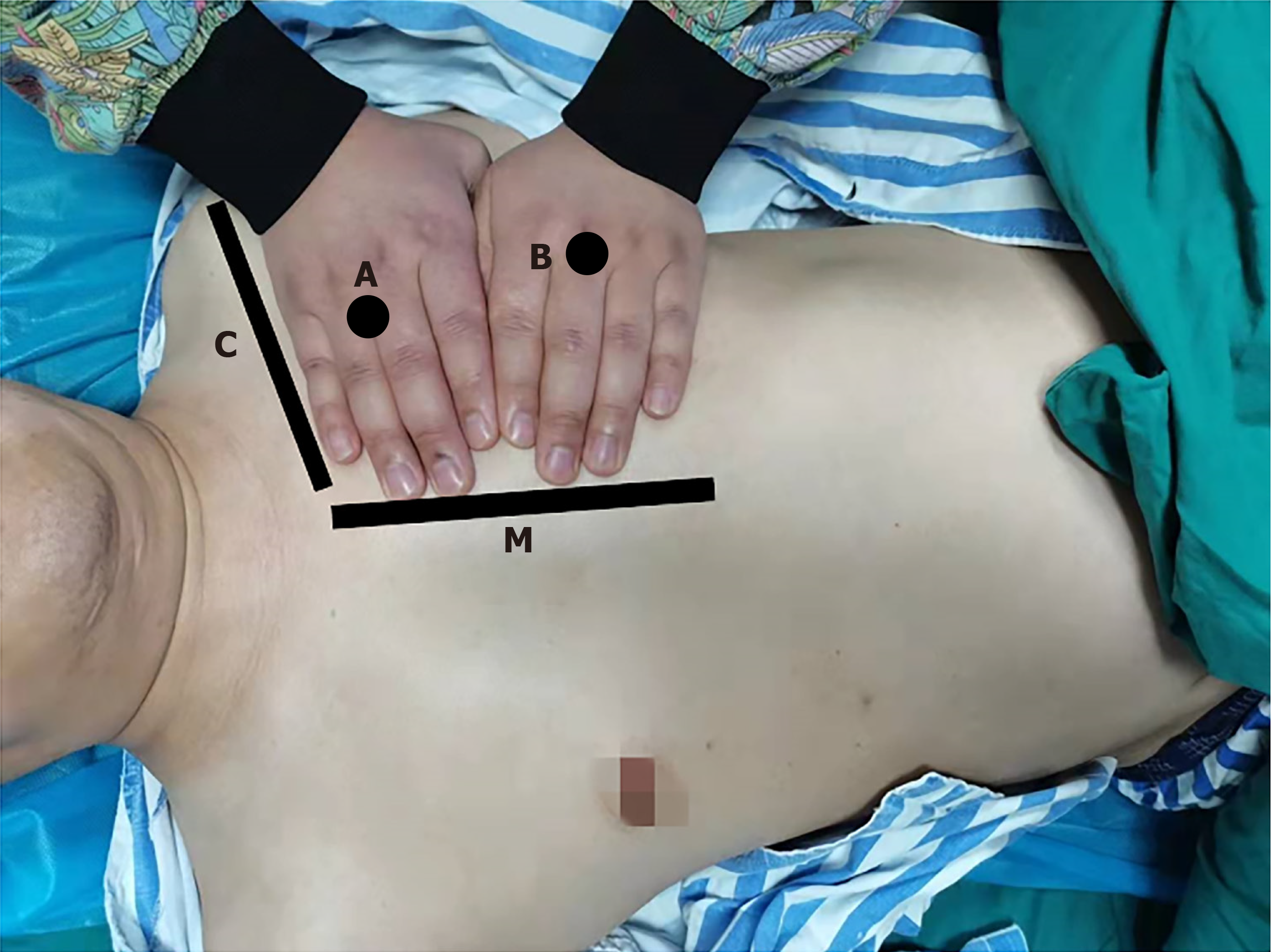
The examiner's hands place on the patient's anterior chest wall (excluding the thumbs), with the little finger of the upper hand close to the clavicle and the fingertips close to the median sternal line. The upper BLUE point is at the third and fourth metacarpophalangeal joints of the upper hand, and the lower BLUE point is at the center of the lower palm. The two points are thought to be the highest points at which gas is the most concentrated. The two BLUE points are recommended for rapid diagnosis or exclusion of pneumothorax during the perioperative period (Figure 3). It was reported that small-volume pneumothorax caused by blunt trauma mainly occured in the parasternal regions[10], which was consistent with the BLUE protocol recommend
Ultrasound diagnosis of pneumothorax is based on both exclusion and confirmed diagnosis. If pneumothorax is suspected in perioperative period, bedside ultrasound should be performed immediately. Pneumothorax can be excluded by the pleural slide sign[12], which is a normal pulmonary sign of relative movement between the visceral and parietal pleura which is visible by ultrasound during respiratory movement. The negative predictive value for the diagnosis of pneumothorax by pleural slide sign has been reported as 100%. Pneumothorax can thus be excluded quickly and accurately by the existence of the surface pleural slide sign[13]. When pneumothorax is present, the visceral and parietal pleurae will be separated by gas. Therefore, the disappearance of the pleural slide sign on ultrasound is the initial step in the diagnosis of pneumothorax[14]. However, the positive predictive value of the disappearance of pleural slide sign for the diagnosis of pneumothorax is estimated as 87% in the normal population, 56% in ICU patients, and only 27% in cases of respiratory failure[15]. Tracheal intubation, single lung ventilation, atelectasis, pulmonary fibrosis, ARDS, pleural adhesion, phrenic nerve palsy, cardiac and respiratory arrest, and other factors may also lead disappearance of the pleural slide sign. In M-mode echocardiography, normal lung tissue resembles a beach with respiratory movement (Figure 2). Without respiratory movement, lung tissue in cases of pneumothorax resembles parallel lines (Figure 2). Ultrasound diagnosis of pneumothorax depends on lung point and is regarded as a gold standard with a specificity of 100%. For the patients with pneumothorax, as the probe moves laterally along the chest wall, a specific area (lung point) can be detected. A pleural slide sign, meaning that the parietal pleura is in contact with the visceral pleura, is observed on one side, and no slide is observed on the other, which means that the pleurae are separated by air[16]. The lung points can slide along the pleural line with respiratory movements, and determine the boundary of pneumothorax[15]. Lung points indicates the area of transition between collapsed lung tissue, with loss of sliding between the pleurae, and normal lung tissue. In M-mode echocardiography, A "beach sign," which indicates normal tissue, suddenly changes to a "parallel lines sign," which indicates pneumothorax[14] (Figure 2).
In addition to the rapid diagnosis of perioperative pneumothorax, pulmonary ultrasound can also be used to guide the management of pneumothorax. In this case, once the pneumothorax was diagnosed, ultrasound was used to guide the placement of a closed thoracic drainage tube by indicating the pneumothorax boundary (lung points). After drainage, the patient's airway pressure significantly decreased and oxygenation returned to normal. Pulmonary ultrasound to guide catheter location has the advantages of increased safety and reduced risk. A meta-analysis has shown that ultrasound-guided thoracic puncture reduced the incidence of secondary pneumothorax[17]. Patel et al[18] reported that ultrasound-guided thoracic catheterization reduced the cost of treatment, length of hospital stay, and incidence of complications such as pneumothorax and hemorrhage. Lung ultrasound is easy to learn. In a randomized controlled trial, anesthesiologists were found to be proficient in diagn
Although ultrasound can help anesthesiologists diagnose pneumothorax quickly and conveniently, there are limitations. It is difficult to obtain satisfactory images in patients with open trauma, obesity, or pulmonary disease, which may lead a missed diagnosis of pneumothorax[20]. Many studies have confirmed lung points as the gold standard to diagnose pneumothorax by ultrasound, but a lung point detected by ultrasound in an 83-year-old patient, was found to be a pulmonary bulla on CT and X-ray examination. That was the first reported case of lung points in a patient who was not diagnosed with pneumothorax[14]. Mild and moderate pneumothorax can be diagnosed by lung points, but lung points may not be seen in severe pneumothorax because of complete disappearance of lung sliding and the parallel lines sign.
Perioperative pneumothorax is a rare but dangerous complication requiring urgent diagnosis and treatment. Once it occurs, the positive pressure generated by mechanical ventilation may cause the lung on the affected side to collapse rapidly, leading intractable hypoxemia. Lung ultrasound is a bedside modality that is becoming widely used for the rapid diagnosis and treatment of pneumothorax
The authors thank the patient and his family for the consent to share this case.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Deshwal H, Hefny AF, Rathnaswami A, Sharma S S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Yu HG
| 1. | Mirabile C, Malekzadeh-Milani S, Vinh TQ, Haydar A. Intraoperative hypoxia secondary to pneumothorax: The role of lung ultrasound. Paediatr Anaesth. 2018;28:468-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2012;5:76-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 126] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 3. | Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, Melniker L, Gargani L, Noble VE, Via G, Dean A, Tsung JW, Soldati G, Copetti R, Bouhemad B, Reissig A, Agricola E, Rouby JJ, Arbelot C, Liteplo A, Sargsyan A, Silva F, Hoppmann R, Breitkreutz R, Seibel A, Neri L, Storti E, Petrovic T; International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1739] [Cited by in RCA: 1880] [Article Influence: 144.6] [Reference Citation Analysis (0)] |
| 4. | Wernecke K, Galanski M, Peters PE, Hansen J. Pneumothorax: evaluation by ultrasound--preliminary results. J Thorac Imaging. 1987;2:76-78. [PubMed] |
| 5. | Lichtenstein DA. Ultrasound examination of the lungs in the intensive care unit. Pediatr Crit Care Med. 2009;10:693-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Dulchavsky SA, Schwarz KL, Kirkpatrick AW, Billica RD, Williams DR, Diebel LN, Campbell MR, Sargysan AE, Hamilton DR. Prospective evaluation of thoracic ultrasound in the detection of pneumothorax. J Trauma. 2001;50:201-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 148] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 7. | Richards JR, McGahan JP. Focused Assessment with Sonography in Trauma (FAST) in 2017: What Radiologists Can Learn. Radiology. 2017;283:30-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 92] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 8. | Ma H, Huang D, Zhang M, Huang X, Ma S, Mao S, Li W, Chen Y, Guo L. Lung ultrasound is a reliable method for evaluating extravascular lung water volume in rodents. BMC Anesthesiol. 2015;15:162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Lanks CW, Correa V. Advantages of Cardiopulmonary Ultrasound in Post-Cardiopulmonary Resuscitation Tension Pneumothorax. J Ultrasound Med. 2018;37:819-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Hefny AF, Kunhivalappil FT, Paul M, Almansoori TM, Zoubeidi T, Abu-Zidan FM. Anatomical locations of air for rapid diagnosis of pneumothorax in blunt trauma patients. World J Emerg Surg. 2019;14:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Lichtenstein D. Novel approaches to ultrasonography of the lung and pleural space: where are we now? Breathe (Sheff). 2017;13:100-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 12. | Yin MG, Wang XT, Liu DW, Chao YG, Guan XD, Kang Y, Yan J, Ma XC, Tang YQ, Hu ZJ, Yu KJ, Chen DC, Ai YH, Zhang LN, Zhang HM, Wu J, Liu LX, Zhu R, He W, Zhang Q, Ding X, Li L, Li Y, Liu HT, Zeng QB, Si X, Chen H, Zhang JW, Xu QH, Chen WJ, Chen XK, Huang DZ, Cai SH, Shang XL, Guan J, Du J, Zhao L, Wang MJ, Cui S, Wang XM, Zhou R, Zeng XY, Wang YP, Lyu LW, Zhu WH, Zhu Y, Duan J, Yang J, Yang H; Chinese Critical Ultrasound Study Group; Gritical Hemodynamic Therapy Collabration Group. [Technical specification for clinical application of critical ultrasonography]. Zhonghua Nei Ke Za Zhi. 2018;57:397-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 13. | Trovato FM, Catalano D, Trovato GM. Thoracic ultrasound: An adjunctive and valuable imaging tool in emergency, resource-limited settings and for a sustainable monitoring of patients. World J Radiol. 2016;8:775-784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Aziz SG, Patel BB, Ie SR, Rubio ER. The Lung Point Sign, not Pathognomonic of a Pneumothorax. Ultrasound Q. 2016;32:277-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Abbas A, Embarak S, Walaa M, Lutfy SM. Role of diaphragmatic rapid shallow breathing index in predicting weaning outcome in patients with acute exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:1655-1661. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Skaarup SH, Folkersen BH. Ultrasound-assisted aspiration of loculated pneumothorax: A new technique. J Clin Ultrasound. 2016;44:326-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Gordon CE, Feller-Kopman D, Balk EM, Smetana GW. Pneumothorax following thoracentesis: a systematic review and meta-analysis. Arch Intern Med. 2010;170:332-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 209] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 18. | Patel PA, Ernst FR, Gunnarsson CL. Ultrasonography guidance reduces complications and costs associated with thoracentesis procedures. J Clin Ultrasound. 2012;40:135-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 19. | Edrich T, Stopfkuchen-Evans M, Scheiermann P, Heim M, Chan W, Stone MB, Dankl D, Aichner J, Hinzmann D, Song P, Szabo AL, Frendl G, Vlassakov K, Varelmann D. A Comparison of Web-Based with Traditional Classroom-Based Training of Lung Ultrasound for the Exclusion of Pneumothorax. Anesth Analg. 2016;123:123-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 20. | Shostak E, Brylka D, Krepp J, Pua B, Sanders A. Bedside sonography for detection of postprocedure pneumothorax. J Ultrasound Med. 2013;32:1003-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |