Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.11024
Peer-review started: May 23, 2021
First decision: July 15, 2021
Revised: July 26, 2021
Accepted: October 25, 2021
Article in press: October 25, 2021
Published online: December 16, 2021
Processing time: 200 Days and 15.6 Hours
The orbital venous malformation is quite common in orbital diseases. Clinically, it is usually characterized by proptosis. However, among patients with distensible venous malformations, if the lesions continuously progress, they may induce enlargement of the orbital bone or orbital lipoatrophy, which in turn leads to enophthalmos.
Here, we report a patient who presented with enophthalmos and had a severe absence of intra-orbital fat secondary to orbital venous malformation. The patient was a 66-year-old female with a 20-year history of enophthalmos. Hertel exophthalmometry readings in a relaxed upright position were 4 mm OD and 13 mm OS with a 97 mm base. It was determined that she had positional “proptosis”. Physical examination also revealed a bulging mass on her hard palate. Computed tomographic scan and magnetic resonance imaging showed an expansion of the right orbit with local bony defects and multiple soft-tissue masses.
Long-term lack of awareness about the presence of orbital venous malformations, persistent venous congestion could lead to compression of the orbital fat, which in turn induces atrophy or the absence of intra-orbital fat.
Core Tip: Timely diagnosis and treatment are critical to prevent secondary irreversible lesions. In patients with severe orbital venous malformations, delayed diagnosis and treatment may induce atrophy or the absence of intra-orbital fat. This case report provides a cautionary tale for patients with a long history of orbital venous malformations.
- Citation: Yang LD, Xu SQ, Wang YF, Jia RB. Severe absence of intra-orbital fat in a patient with orbital venous malformation: A case report. World J Clin Cases 2021; 9(35): 11024-11028
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/11024.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.11024
The orbital venous malformation is very common in orbital diseases, which is characterized by a high incidence, high recurrence rate and limited treatment methods[1]. Superficial lesions of orbital venous malformation can be found at birth and grow in proportion to the body[2]. More than 90% of orbital venous malformations are solitary and sporadic lesions, and the remaining 10% are multiple, wide-ranging or with comorbidities[1]. The physical examination findings of orbital venous malformations were mainly presented as proptosis, compressible lesions and positive body position test[3]. In this case report, we report a case of a 66-year-old female who suffered a severe enophthalmos caused by a long history of orbital venous malformations. She was admitted to the hospital for treatment. Radiological features presented local bone defects in the right orbit, atrophy of orbital fat in the right orbit and venous calculi in addition to the space-occupying lesions of the malformed vein. As lipoatrophy was irreversible and untreatable in this patient, we finally performed a modified Hotz procedure for correction of her entropion.
A 66-year-old female presented with enophthalmos and entropion in her right eye for 20 years and aggravated for 1 year.
The patient had a history of orbital venous malformation for more than 20 years. In the last year, she had noticed decreased vision in her right eye under no obvious predisposing causes. She also complained of ocular discomfort caused by entropion. Now she was admitted to the hospital due to the worsening symptoms.
She had a 7-year history of hypertension. The blood pressure was controlled at 130/80 mmHg under the treatment of nifedipine controlled-release tablets.
She was first found to have a venous malformation of the right buccal 30 years ago. Her anamnesis was significant for surgical treatment for buccal vascular anomalies.
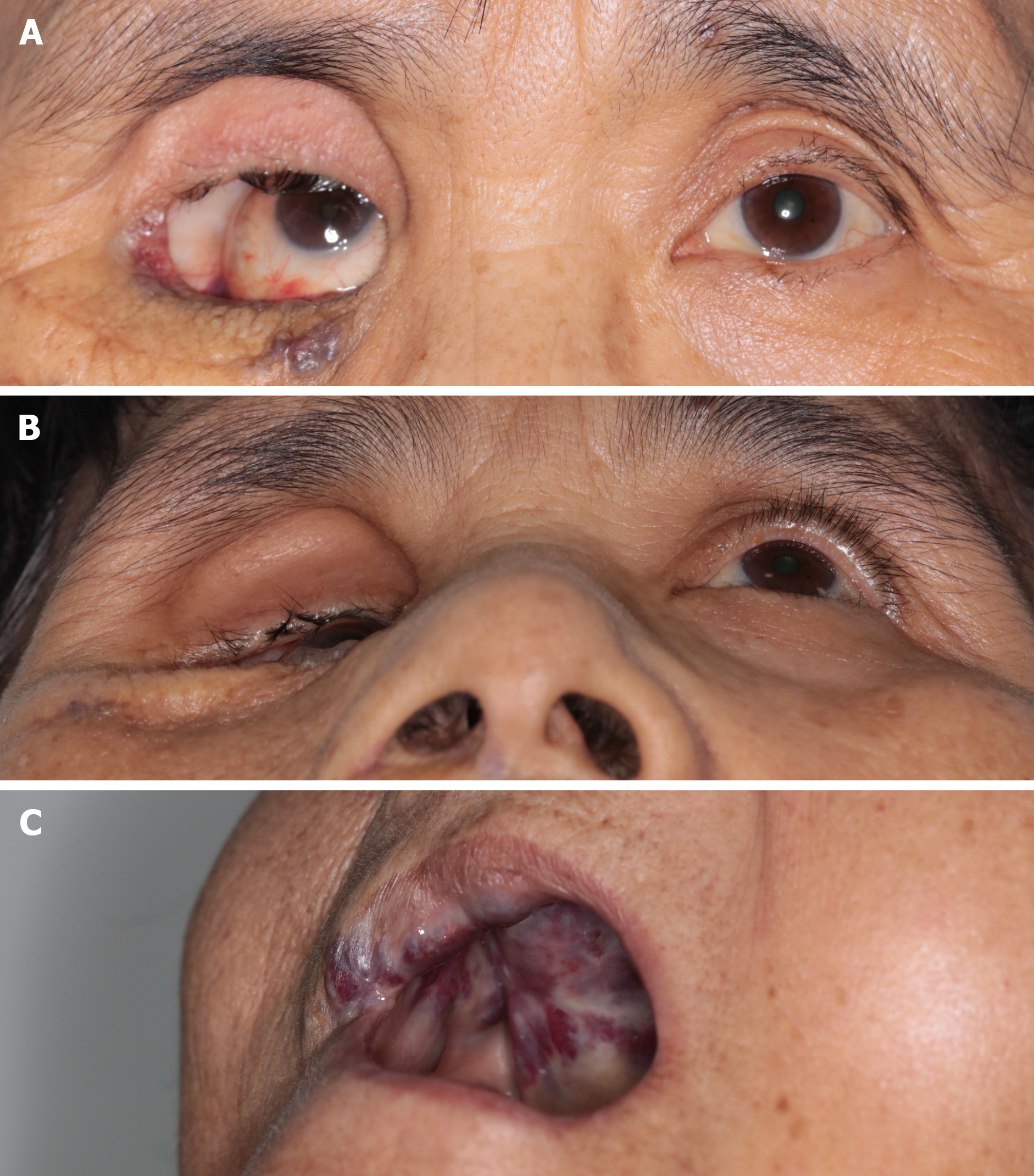
She was found to have a severe absence of intra-orbital fat with her right eye sunken backward in the bony orbit. There was a separation of the eyelid and eyeball, where the upper orbit-temporal region could be observed (Figure 1A and B). Hertel exophthalmometry readings in a relaxed upright position were 4 mm OD and 13 mm OS with a 97 mm base. It was determined that she had positional “proptosis” (com
There were no significant changes.
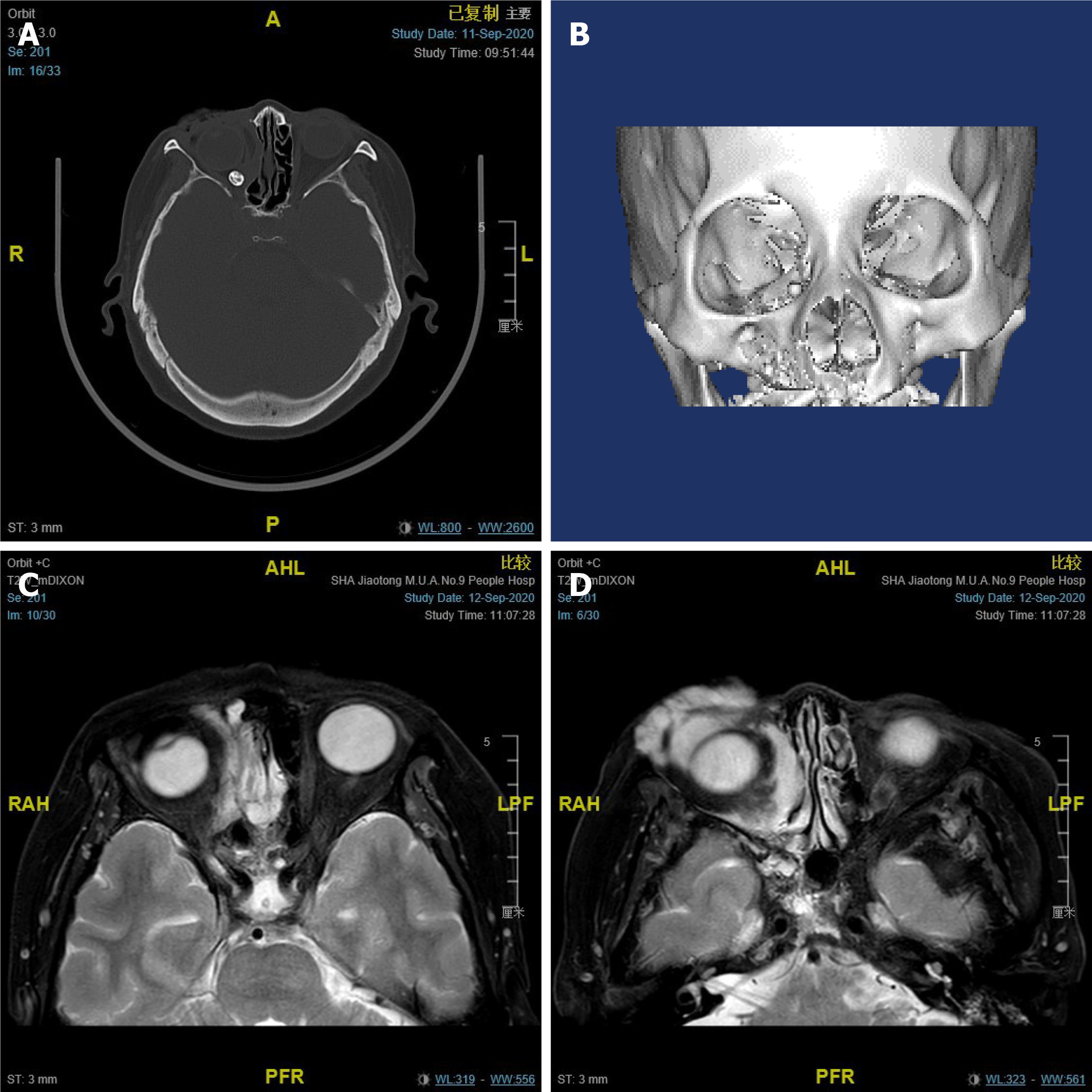
A plain computed tomographic scan detected enophthalmos with local bony defects on the right orbit. Phlebolith was visualized (Figure 2A). 3D modeling presented an obvious expansion of the right orbital cavity (Figure 2B). The absence of orbital soft tissue around her right eye was observed through magnetic resonance imaging (MRI), which also showed an irregular soft tissue mass with indistinct borders inside and outside the muscle pyramid in the right orbit that could become enlarged after pressurizing (Figure 2C and D).
Orbital venous malformation and entropion on the right eye. Persistent venous congestion leads to compression of the orbital fat, which in turn induces atrophy or the absence of intra-orbital fat.
A modified Hotz procedure for correction of entropion was adopted to improve her symptoms of ocular discomfort caused by entropion.
After the operation, the fluid infusion was given for the symptomatic treatment. The patient experienced no complications during hospitalization and was discharged four days after surgery. Strenuous exercise was not recommended.
Enophthalmos is the posterior movement of the eyeball within the bony orbit due to a change in the volume of the eyeball or orbital soft tissues relative to the orbital bones. Orbital soft tissues, including muscles and intra-orbital fat, are important components of orbital contents, accounting for approximately 50% of orbital cavity volume[4,5]. The causes of enophthalmos can be divided into two categories: expansion of the orbital cavity and reduction of the orbital content volume. There are several conditions that can lead to the expansion of the orbital cavity, including orbital trauma, orbital bone defects, maxillary atelectasis and some orbital surgeries. Other conditions that can cause a reduction in the orbital content volume include orbital fat atrophy, orbital inflammation, resolved pseudotumors with fibrosis, Parry-Romberg syndrome, contraction of ocular muscle and sequelae of surgery[6].
The orbital vascular malformation is quite common in orbital diseases. According to angiogenesis, malformations can be classified as venous, arterial, lymphatic, or mixed[4]. As the most common type of vascular malformation in the orbit, orbital venous malformation can be divided into distensible and non-distensible lesions. Because of the communication of the distensible malformation and the venous circulation, patients with distensible lesions are often characterized by a positive response to the Valsalva maneuver, postural globe displacement or proptosis. However, if the lesions continuously progress, they may induce enlargement of the orbital bone or orbital lipoatrophy, which in turn leads to enophthalmos[7].
Here, we report a patient who had a severe absence of intra-orbital fat with her right eye sunken backward in the bony orbit in a relaxed upright position. As a rare symptom of orbital venous malformation, entropion occurred in this patient because of extreme enophthalmos.
Considering that she had a long medical history of orbital venous malformation, it is likely that persistent venous congestion led to compression of the orbital fat, which induced orbital lipoatrophy. Venous malformation lesions are not solitary but widespread in this patient. In addition to orbital venous malformation, MRI detected multiple expansive soft tissue masses involving the upper lip and cheek. Physical examination also revealed a bulging mass on her hard palate.
Clinically, sclerotherapy, laser therapy, embolization, surgical resection, and radiotherapy are commonly used in the treatment of orbital venous malformation[4]. For this patient, considering that the lesions were multiple, involved deep structures and had a long duration, an effective treatment for orbital venous malformation was lacking. There are several existing therapeutic options for the treatment of orbital lipoatrophy, such as artificial material filling, lipoinjection or lipofilling. However, these treatments do not completely resolve orbital venous malformations and even have a risk of thrombohemorrhagic events. The persistence of venous malformations will compress periorbital tissue and affect the curative effect. As lipoatrophy was irreversible and untreatable in this patient, we finally performed a modified Hotz procedure for correction of her entropion. For bulging mass located on the hard palate of this patient, maxillofacial surgery recommended sclerotherapy. However, the patient rejected treatment, fearing the risks and the uncertain consequences of the sclerotherapy.
In conclusion, we reported on our case of a rare presentation of an absence of intra-orbital fat secondary to orbital venous malformation. We revealed that with a long-term lack of awareness about the presence of orbital venous malformations, persistent venous congestion leads to compression of the orbital fat, which in turn induces atrophy or the absence of intra-orbital fat. Both patients and physicians should be made aware that timely diagnosis and treatment are critical to prevent secondary irreversible lesions. This kind of case report could provide practical clinical experience for clinicians to improve the management of this disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Trifan A S-Editor: Liu M L-Editor: A P-Editor: Liu M
| 1. | Dompmartin A, Vikkula M, Boon LM. Venous malformation: update on aetiopathogenesis, diagnosis and management. Phlebology. 2010;25:224-235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 239] [Cited by in RCA: 203] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 2. | Seront E, Vikkula M, Boon LM. Venous Malformations of the Head and Neck. Otolaryngol Clin North Am. 2018;51:173-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 3. | Lee BB, Baumgartner I, Berlien P, Bianchini G, Burrows P, Gloviczki P, Huang Y, Laredo J, Loose DA, Markovic J, Mattassi R, Parsi K, Rabe E, Rosenblatt M, Shortell C, Stillo F, Vaghi M, Villavicencio L, Zamboni P; International Union of Phlebology. Diagnosis and Treatment of Venous Malformations. Consensus Document of the International Union of Phlebology (IUP): updated 2013. Int Angiol. 2015;34:97-149. [PubMed] |
| 4. | Du Y, Lu BY, Chen J, He JF. Measurement of the Orbital Soft Tissue Volume in Chinese Adults Based on Three-Dimensional CT Reconstruction. J Ophthalmol. 2019;2019:9721085. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Regensburg NI, Wiersinga WM, van Velthoven ME, Berendschot TT, Zonneveld FW, Baldeschi L, Saeed P, Mourits MP. Age and gender-specific reference values of orbital fat and muscle volumes in Caucasians. Br J Ophthalmol. 2011;95:1660-1663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Koo L, Hatton MP, Rubin PA. When is enophthalmos "significant"? Ophthalmic Plast Reconstr Surg. 2006;22:274-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Li T, Jia R, Fan X. Classification and treatment of orbital venous malformations: an updated review. Front Med. 2019;13:547-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |