Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.10994
Peer-review started: April 28, 2021
First decision: May 23, 2021
Revised: May 29, 2021
Accepted: July 6, 2021
Article in press: July 6, 2021
Published online: December 16, 2021
Processing time: 225 Days and 17.3 Hours
Klippel-Trenaunay syndrome (KTS) is a rare congenital disorder. A detailed prenatal ultrasound examination plays an important role in the diagnosis of KTS and the subsequent counseling and follow-up of the patient.
A 25-year-old woman attended our department for a regular examination. The whole of the right lower extremity and right buttock were observed to be markedly thicker compared to the left one at 18 wk of gestation. However, the lengths of the right femur, tibia and fibula were in the normal range. No marked edema and fluid/cystic spaces were detected in the lower limbs. There were no other organ abnormalities. The vasculature in the right limb was visibly dilated, with much higher intensive blood flow signals. No congenital embryonic veins were visible in both limbs. The right lower limb exhibited much more hypertrophy compared to the left limb two weeks later. Amniocentesis and genetic tests showed normal results with 46 XX. Despite the normal karyotype, the family opted to terminate the pregnancy. The post-mortem examination confirmed asymmetric hypertrophy of the right limb in the fetus and revealed a large area of marked dark-purple superficial capillary malformations occupying the skin of the right lower extremity. The enlargement of veins and soft tissue hypertrophy were also seen on postnatal X-ray and Magnetic Resonance Imaging. Autopsy revealed severe congestion in the right lower limb. A final diagnosis of KTS was made.
KTS may be diagnosed prenatally based on the typical features observed during ultrasound examination.
Core Tip: Klippel–Trenaunay syndrome (KTS) is a rare congenital disorder. The prenatal ultrasound features include hypertrophy of one extremity, a difference between the length of the bones of the extremities, multiple cystic lesions of the extremities or internal organs, increasing blood flow signals and dilated veins or persistence of the embryonic veins. KTS may be diagnosed based on these typical characteristics in utero.
- Citation: Pang HQ, Gao QQ. Prenatal ultrasonographic findings in Klippel-Trenaunay syndrome: A case report. World J Clin Cases 2021; 9(35): 10994-10998
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/10994.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.10994
Klippel–Trenaunay syndrome (KTS) is a rare congenital disorder characterized by a classical triad of port-wine stains, varicosities, bone and soft tissue hypertrophy, and other complications such as lymphedema and lymphangiomas, which may involve any region of the body[1]. The etiology of this disease remains unclear. Most cases can be diagnosed through a complete history and clinical examination after birth[2]. The detailed prenatal images and follow-up are crucial for the diagnosis of KTS and the subsequent counseling and management of the patient. Ultrasonographic detection is an essential method for the diagnosis of KTS in utero[3]. The present study documents the prenatal ultrasound findings of a case of KTS.
A 25-year-old woman attended our department for a regular examination.
The patient was 18 wk of gestation, with regular menstrual period and was gravida 1 parity 0. There was no history of other diseases during pregnancy.
The patient had no significant medical history.
The personal and family history did not reveal any problems, including a history of vascular disorders.
On admission, her temperature was 36.7°C, respiratory rate was 23 breaths/min, and blood pressure was 120/80 mmHg. The obstetric examination revealed that the fundal height and abdominal circumference of the patient were consistent with her gestational age.
Her nuchal translucency measurement and triple test results were normal.
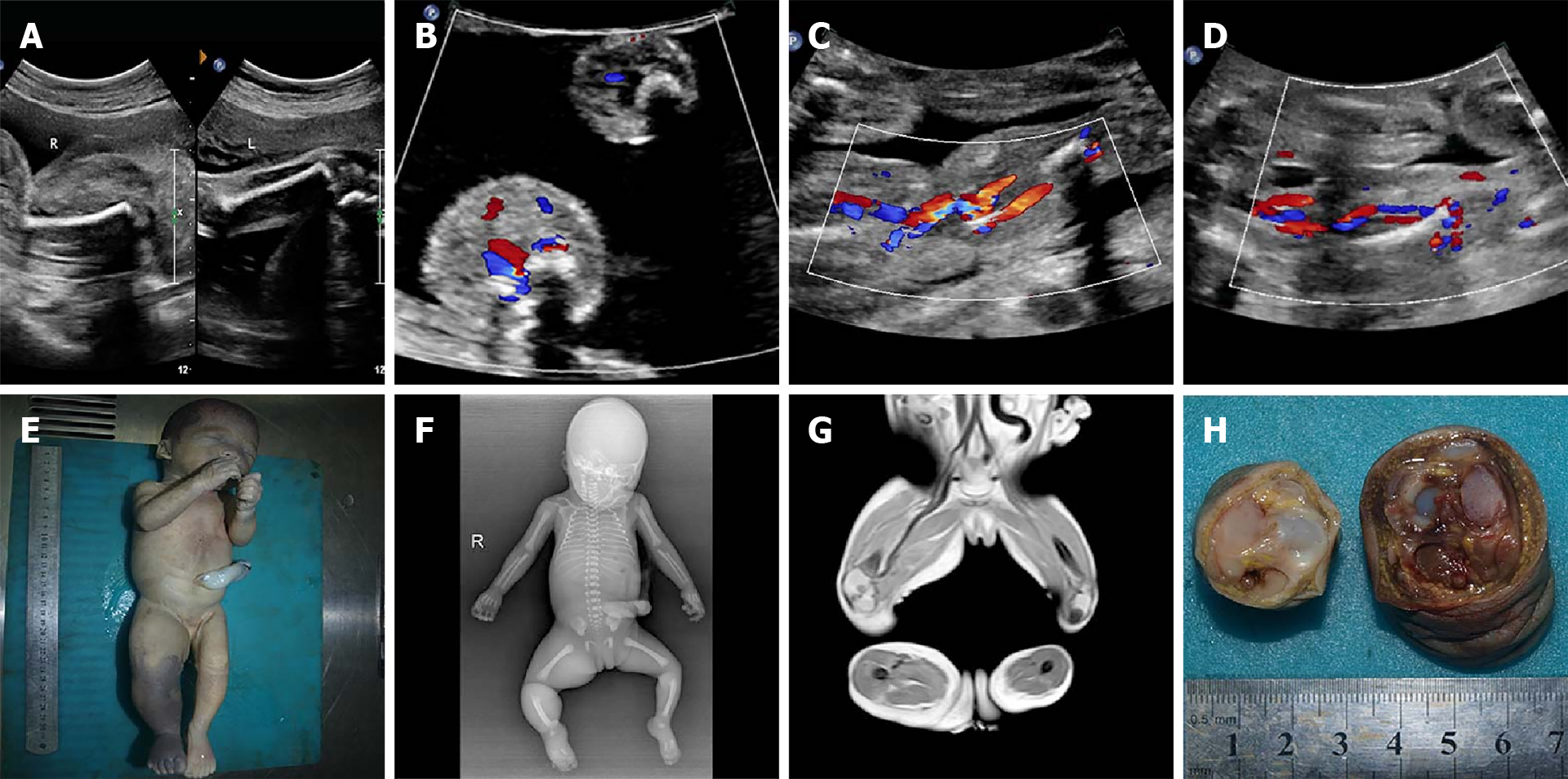
The whole of the right lower extremity and right buttock were observed to be markedly thicker compared to the left one at 18 wk of gestation. However, the lengths of the right femur, tibia, and fibula were in the normal range. No marked edema and fluid/cystic spaces were detected in the lower limbs (Figure 1A and B). There were no other organ abnormalities. On the basis of these characteristics on ultrasound images, a diagnosis of KTS was suspected. Therefore, a detailed examination of the lower-limb vascular system was performed. The external iliac veins, great saphenous veins, femoral/popliteal veins, and the lateral thigh area in both lower limbs were carefully examined. The vasculature in the right limb was visibly dilated, with much higher intensive blood flow signals. No congenital embryonic veins were visible in both limbs (Figure 1C and D). Examination of the vascular system also supported the diagnosis of KTS. In the examination conducted two weeks later, the right lower limb exhibited much more hypertrophy compared to the left limb. Amniocentesis and genetic tests showed normal results with 46 XX.
The post-mortem examination confirmed asymmetric hypertrophy of the right limb and revealed a large area of marked dark-purple superficial capillary malformations occupying the skin of the right lower extremity (Figure 1E). Enlargement of the veins and soft tissue hypertrophy were also observed in the postnatal X-ray and magnetic resonance imaging (MRI), although embryonic veins were absent (Figure 1F and G). Autopsy revealed severe congestion in the right lower limb (Figure 1H).
Following consultation with the geneticists and the professor of a vascular malformation clinic, a final diagnosis of KTS was made.
Despite the normal karyotype, the family opted to terminate the pregnancy after a counseling session with the obstetric/pediatric team, considering a range of possible outcomes, including significant disability.
The patient underwent termination of the pregnancy. Two years later, the patient became pregnant and delivered a healthy female infant.
KTS is a rare and sporadic congenital disorder, which presents at birth, early infancy or childhood. The proposed pathogenesis of the disease mainly includes deep vein atresia, chronic venous hypertension, persistence of the embryological vascular system and mesodermal anomaly[1].
The etiology of KTS remains unknown. Most reported cases have not been associated with chromosome abnormalities. Whelan et al[4] reported a case of KTS associated with a single gene defect at 5q or 11p, thus, demonstrating that this genetic defect may result in increased angiogenesis leading to KTS[5]. In addition, a case with a terminal 2q37.3 deletion[6] and a case of loss of heterozygosity for 1q21.2 q44[7] were also reported.
Most of the reported cases had no genetic characteristics except a case with unproven autosomal dominant inheritance[8]. Most KTS cases were unilateral and affected the lower extremities. Both upper and lower limbs might be involved in 10% of patients. According to published reports, hemangioma lesions can also involve other organs and body parts, such as the liver, lung, spinal cord, cranial area, skull, intestinal tract, urinary tract, testis, adrenal glands, and peritoneal and retroperitoneal cavity[7,9-11].
Most patients have skin vascular nevi or wine stains to some extent and hypertrophy of the skeleton and soft tissue; thus, they were diagnosed according to these typical signs at birth[1]. A deep tissue cavernous hemangioma may gradually appear and aggravate in later childhood. The prenatal ultrasound features in utero have been described in many studies[8,12-14]. They include marked asymmetrical hypertrophy of limbs, thickening of the subcutaneous soft tissue, multiple cystic lesions, increasing blood flow signals, dilated veins or persistence of embryonic veins. It is difficult to detect skin capillary malformations, we speculate that the fetoscope may be a useful tool to observe fetal skin vascular nevi or wine stains in utero.
One of the main features of KTS is anomaly of the limb vein system, which appears as the persistence of embryonic veins, and varicose enlargement hypoplasia of the limb venous system. Assimakopoulos et al[9] revealed a case associated with a hypertrophied great saphenous vein. We also found more blood flow signals and the dilation of deep veins, which was confirmed by MRI and autopsy after induced abortion in our case. These findings indicated that it is feasible to carry out a thorough prenatal ultrasound examination of the venous system in the lower extremities to obtain more information in order to diagnose KTS.
The clinical presentation varies from minimally symptomatic disease to life-threatening bleeding and embolism. The prognosis is correlated with the size of the masses and their growth. There were large and extensive anechoic areas or the involvement of internal organs in reviewed cases with poor prognosis[3]. Therefore, the ultrasound scan should be repeated and the area and progress of the cystic lesions monitored, which may increase the risk of intrauterine heart failure and bleeding in the postnatal stage.
It is worth noting that there are many more reported cases after birth than in utero. This indicates that many cases of fetal KTS are not diagnosed prenatally as the lesions are minimal or complex, and it is difficult to make an accurate diagnosis. KTS should be suspected when there is hypertrophy of one of the extremities, discrepancy in the bone length, surface masses on the limbs and/or trunk, and unexplained cystic lesions of the internal organs or limbs. Therefore, necessary examinations should be performed to determine the location and severity of the lesions and to provide a reliable basis for the selection of appropriate treatment methods. MRI is another useful method, which can offer more detail on the soft tissue and vasculature.
KTS may be diagnosed prenatally based on the typical features on ultrasound examination. Timely prenatal diagnosis and follow-up are important for subsequent prenatal counseling and adjustment of medical care and choices according to each case.
We would like to thank Professor Hong Luo and Dr. Bo Zhang for their contribution to this report by providing additional data and support.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Stan F S-Editor: Fan JR L-Editor: Webster JR P-Editor: Guo X
| 1. | Asghar F, Aqeel R, Farooque U, Haq A, Taimur M. Presentation and Management of Klippel-Trenaunay Syndrome: A Review of Available Data. Cureus. 2020;12:e8023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Wang SK, Drucker NA, Gupta AK, Marshalleck FE, Dalsing MC. Diagnosis and management of the venous malformations of Klippel-Trénaunay syndrome. J Vasc Surg Venous Lymphat Disord. 2017;5:587-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 3. | Ivanitskaya O, Andreeva E, Odegova N. Prenatal diagnosis of Klippel-Trenaunay syndrome: Series of four cases and review of the literature. Ultrasound. 2020;28:91-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Whelan AJ, Watson MS, Porter FD, Steiner RD. Klippel-Trenaunay-Weber syndrome associated with a 5:11 balanced translocation. Am J Med Genet. 1995;59:492-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 72] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Tian XL, Kadaba R, You SA, Liu M, Timur AA, Yang L, Chen Q, Szafranski P, Rao S, Wu L, Housman DE, DiCorleto PE, Driscoll DJ, Borrow J, Wang Q. Identification of an angiogenic factor that when mutated causes susceptibility to Klippel-Trenaunay syndrome. Nature. 2004;427:640-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 221] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 6. | Puiu I, Stoica A, Sosoi S, Puiu A, Ioana M, Burada F. Terminal deletion 2q37.3 in a patient with Klippel-Trenaunay-Weber syndrome. Fetal Pediatr Pathol. 2013;32:351-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Yu D, Sun L, Chen T. Prenatal ultrasound diagnosis of Klippel-Trenaunay-Weber syndrome associated with umbilical cord hemangioma. J Clin Ultrasound. 2021;49:254-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Chen CP, Lin SP, Chang TY, Lee HC, Hung HY, Lin HY, Huang JP, Wang W. Prenatal sonographic findings of Klippel-Trénaunay-Weber syndrome. J Clin Ultrasound. 2007;35:409-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Assimakopoulos E, Zafrakas M, Athanasiades A, Peristeri V, Tampakoudis P, Bontis J. Klippel-Trenaunay-Weber syndrome with abdominal hemangiomata appearing on ultrasound examination as intestinal obstruction. Ultrasound Obstet Gynecol. 2003;22:549-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Meholic AJ, Freimanis AK, Stucka J, LoPiccolo ML. Sonographic in utero diagnosis of Klippel-Trenaunay-Weber syndrome. J Ultrasound Med. 1991;10:111-114. [PubMed] [DOI] [Full Text] |
| 11. | Seoud M, Santos-Ramos R, Friedman JM. Early prenatal ultrasonic findings in Klippel-Trenaunay-Weber syndrome. Prenat Diagn. 1984;4:227-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Coombs PR, James PA, Edwards AG. Sonographic identification of lower limb venous hypoplasia in the prenatal diagnosis of Klippel-Trénaunay syndrome. Ultrasound Obstet Gynecol. 2009;34:727-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Peng HH, Wang TH, Chao AS, Chang YL, Shieh SC, Chang SD. Klippel-Trenaunay-Weber syndrome involving fetal thigh: prenatal presentations and outcomes. Prenat Diagn. 2006;26:825-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Sahinoglu Z, Uludogan M, Delikara NM. Prenatal sonographic diagnosis of Klippel-Trenaunay-Weber syndrome associated with umbilical cord hemangioma. Am J Perinatol. 2003;20:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |