Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.10956
Peer-review started: June 19, 2021
First decision: July 16, 2021
Revised: August 26, 2021
Accepted: October 25, 2021
Article in press: October 25, 2021
Published online: December 16, 2021
Processing time: 174 Days and 3.7 Hours
More than ten special scales are available to predict the risk of pressure ulcers in children. However, the performances of those scales have not yet been compared in China.
To compare the Waterlow, Braden Q, and Glamorgan scales, and identify more suitable pressure ulcer evaluation scale for the pediatric intensive care unit (PICU).
Trained nurses used the Waterlow, Braden Q, and Glamorgan scales to assess pediatric patients at Sun Yat-sen Memorial Hospital (China) within 24 h of admission from May 2017 to December 2020 in two stages. Skin examination was carried out to identify pressure ulcers every 3 d for 3 wk.
The incidence of pressure ulcers was 3/28 (10.7%) in the PICU and 5/314 (1.6%) in the general pediatric ward. For children in the general ward, the Waterlow, Braden Q, and Glamorgan scales had comparable area under the operating characteristic curve (AUC) of 0.870, 0.924, and 0.923, respectively, and optimal cut-off values of 14, 14, and 29 points. For PICU, the Waterlow, Braden Q, and Glamorgan scales had slightly lower AUC of 0.833, 0.733, and 0.800, respectively, and optimal cut-off values of 13, 16, and 27 points. Braden Q demonstrated a satisfactory specificity, and during the second stage of the study for PICU patients, the AUC of the Braden Q scale was 0.810, with an optimal cut-off value of 18.35 points.
The Waterlow, Braden Q, and Glamorgan scales have comparable performance, while the Braden Q scale demonstrates a better specificity and can be successfully used by pediatric nurses to identify patients at high risk of pressure ulcers in PICU.
Core Tip: The present study explored and analyzed commonly used Waterlow, Braden Q, and Glamorgan scales for the predictive diagnostic value of pressure ulcers in pediatric patients. In this study, the Braden Q scale had the highest specificity, which might serve as a valuable tool to predict pressure ulcers in pediatric intensive care unit (PICU) patients. The Waterlow, Braden Q, and Glamorgan scales have comparable performance, while the Braden Q scale demonstrated a better specificity and can be successfully used by pediatric nurses to identify patients at high risk of pressure ulcers in PICU.
- Citation: Luo WJ, Zhou XZ, Lei JY, Xu Y, Huang RH. Predictive risk scales for development of pressure ulcers in pediatric patients admitted to general ward and intensive care unit. World J Clin Cases 2021; 9(35): 10956-10968
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/10956.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.10956
Children admitted to the medical care centers are at an increased risk of pressure ulcers[1-3]. The prevalence of pressure ulcers in pediatric patients ranges from 1.72% to 18.6% in different countries and ages and is higher in pediatric intensive care units (PICUs) than in general pediatric wards[4-6]. Owing to the unstable hemodynamic status and the prolonged bed rest, hospitalized children have a high risk of pressure ulcers. Additionally, compared to adults, hospitalized children have more difficulty expressing pain, discomfort, or the need for repositioning[7]. Pressure ulcers in children could have detrimental effects, including pain, infection, negative psychosocial impact due to scarring or alopecia, prolonged hospitalization time, and increased treatment costs[8]. Thus, identifying pediatric patients at risk for pressure ulcer development would allow timely intervention to prevent the occurrence of pressure sores.
Outside of China, at least 12 pediatric risk assessment scales for pressure ulcers have been described and assessed in the clinical setting, including the Braden Q[9], Glamorgan[10], and Waterlow scales[11]. The Braden Q scale was frequently used to assess the risk in pediatric patients[12] and validated in patients aged 3 wk to 8 years using receiver operating characteristic (ROC) curve analysis. Subsequently, the development of pressure ulcers was predicted based on an area under the ROC curve (AUC) of 0.83 and a cut-off score of 16 points, a sensitivity of 0.88, and a specificity of 0.58[13,14]. A meta-analysis showed that the pooled sensitivity and specificity of the Braden Q scale for pediatric patients were 0.73 and 0.61, respectively[15], and another meta-analysis provided the same conclusion[16]. The Glamorgan scale has also been validated for use in children[10], with a sensitivity of 0.984 and specificity of 0.674 at a cut-off score of 15 points[10], although one study has questioned its validity in a low-risk setting[17]. The Waterlow scale has a high specificity and low sensitivity and is recommended for use in conjunction with clinical evaluation[18].
A small number of studies have compared the utilities of different risk assessment scales in the prediction of pressure ulcer development in children. Anthony et al[19] compared the Braden Q, Glamorgan, and Garvin scales and concluded that the Glamorgan risk assessment scale had the best predictive ability. Conversely, Willock et al[8] found that the Braden Q and Glamorgan scales performed similarly when used in neonatal and PICUs and that the Braden Q scale might have an advantage over the Glamorgan scale in general pediatric wards. Kottner et al[20] conducted a systematic review of 15 publications utilizing 12 different pediatric pressure ulcer risk scales and concluded that no single instrument could be considered superior to the others. Thus, despite the availability of numerous scales to assess the risk of pressure ulcers in children, the tool with the best predictive utility in clinical practice is yet to be identified. Interestingly, the optimum risk assessment scale might vary depending on the patient’s anatomy, physiology, and health condition, which could depend on age and whether the patient is in a general pediatric ward or PICU.
In China, only a few studies have evaluated pediatric pressure ulcer risk assessment scales[21,22], and the clinical nursing practice guidelines also lack evidence-based research. In addition, the majority of pediatric pressure ulcer prevention programs are derived from adult assessment scales, ignoring the anatomical and physiological differences between adults and children. Based on these, there is an urgent need for validating and comparing different approaches to the pressure ulcer risk assessment in China. The present study aimed to evaluate the Waterlow, Braden Q, and Glamorgan risk assessment scales in pediatric patients admitted to the Sun Yat-sen Memorial Hospital (China), in order to identify more suitable pressure ulcer evaluation scale for the PICU.
This prospective cohort study enrolled children admitted to the general pediatric ward and PICU of our hospital in two stages, from May 2017 to August 2017 (first stage) and from January 2018 to December 2021 (second stage), respectively.
The inclusion criteria were as follows: (1) Age 28 d-14 years; (2) Admitted to the general pediatric ward or PICU of our hospital; (3) Stayed in the ward/PICU for at least 24 h; and (4) No pressure ulcers were present at the time of admission. The exclusion criterion were as follows: (1) Lost to follow-up, i.e., a full dataset for skin assessment was not available for the 3-wk follow-up period due to termination of the assessments (for whatever reason); (2) Discharge from the hospital; or (3) Death.
This study was approved by the ethics committee of Sun Yat-sen Memorial Hospital [approval number: 2017(23)]. All patients or their legal guardians provided informed written consent before participation in the study.
The participating nurses administered the Waterlow, Braden Q, and Glamorgan risk assessment tools to each child within 24 h of admission, in accordance with the scoring rules of each scale. All participating nurses had undergone standardized training and assessment in the administration of these scales to maximize the consistency and reliability of the evaluation[14]. The Waterlow scale contains several items (build/weight for height, visual assessment of the skin, sex/age, continence, mobility, appetite, tissue malnutrition, neurological deficit, major surgery/trauma, and medication) and identifies three risk categories: At risk (score 10-14), high risk (score 15-19), and very high risk (score ≥ 20)[11]. The Braden Q scale consists of seven subscales (mobility, activity, sensory perception, moisture, friction and shear, nutrition, and tissue perfusion/oxygenation) each scored 1-4, with the total score ranging from 7 (highest risk) to 28 (lowest risk)[9]. The Glamorgan scale contains nine items (mobility, equipment/objects/hard surface pressing on the skin, significant anemia, persistent pyrexia, poor peripheral perfusion, inadequate nutrition, low serum albumin, weight, and incontinence) with the total score ranging from 0 to 42[10].
Six nurses were selected for data collection, among those who have more than 3 years of experience in the pediatric pressure ulcers care. Selected nurses have completed unified training and assessment to ensure reliability and consistency of the evaluation. Two nurses as a group collected the data for skin assessment simultaneously to ensure the accuracy of data collection.
Each patient was followed for 3 wk with regular skin assessments to check for the development of any pressure ulcers. These skin assessments were performed by trained nurses blinded to the risk assessment scale scores. The first assessment was made 24 h after admission, and subsequent assessments were made every 3 d. Therefore, a total of eight skin assessments were carried out for each patient. Any pressure ulcers identified were classified as stage 1 (intact skin with localized non-branchable erythema), stage 2 (partial-thickness skin loss with exposure of dermis), stage 3 (full-thickness skin loss), or stage 4 (full-thickness skin and tissue loss) based on the 2016 revised version of the National Pressure Ulcer Advisory Panel staging system[23].
Statistical analyses were performed using SPSS 22.0 (Inclusion Body Myositis Corp, Armonk, New York, United States). ROC curve analysis was used to analyze the ability of each scale to predict the development of pressure ulcers. The AUC, optimal cut-off value, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated.
A total of 342 children admitted during the first stage of the study were included in the final analysis; 28 patients (mean age: 78.3 ± 15.3 mo; 13 males, 46.4%) were admitted to the PICU and 314 (mean age: 56.7 ± 19.4 mo; 197 males, 62.7%) were admitted to the general ward. The baseline characteristics of the study participants are summarized in Table 1. Among them, children with blood tumors accounted for 64.3% of the total patients in intensive care unit and 42.4% of the total patients in the general ward.
| Characteristic | Intensive care unit (n = 28) | General pediatric ward (n = 314) |
| Age (mo) | 78.3 ± 15.3 | 56.7 ± 19.4 |
| Male, n | 13 (46.4%) | 197 (62.7%) |
| Waterlow scale score | 10.9 ± 6.0 | 4.6 ± 2.7 |
| Braden Q scale score | 17.8 ± 4.3 | 24.6 ± 3.5 |
| Glamorgan scale score | 26.9 ± 5.6 | 7.5 ± 9.2 |
| Patients with squeezing or rubbing of the skin, n | 28 (100%) | 57 (18.2%) |
| Patients with pain at admission, n | 8 (28.6%) | 11 (3.5%) |
| Patients with mechanical ventilation, n | 19 (67.9%) | 7 (2.3%) |
| Patients with blood tumor, n | 18 (64.3%) | 133 (42.4%) |
| Death, n | 4 (14.2%) | 1 (0.3%) |
A total of 349 children were admitted to the PICU during the second stage of the study; among them, 7 were admitted for < 24 h. Finally, a total of 342 children (mean age: 70.3 ± 49.8 mo; 188 males, 55.0%) were included in the final analysis. The baseline characteristics of the study participants are summarized in Table 2.
| Characteristic | Intensive care unit (n = 342) |
| Age (mo) | 70.3 ± 49.8 |
| Male, n | 188 (55.0%) |
| Length of stay > 1 d ≤ 10 d, n | 291 (85.0%) |
| Length of stay > 10 d, n | 51 (14.9%) |
| Braden Q scale score | 26.9 ± 5.6 |
| Patients with blood tumor, n | 210 (61.4%) |
| Patients with immune system diseases, n | 30 (8.77%) |
| Patients with respiratory diseases, n | 41 (12.0%) |
| Postoperative patients, n | 48 (14.0%) |
| Other patients, n | 13 (3.8%) |
| Pressure ulcer incidence, n | 13 (3.8%) |
| Patients with mechanical ventilation, n | 19 (67.9%) |
| Transfer out | 281 (82.2%) |
| Leave hospital | 39 (11.41%) |
| Death, n | 22 (6.43%) |
The incidence of pressure ulcers during the 3-wk follow-up during the first stage was 3/28 (10.7%) for children in the ICU and 5/314 (1.6%) for children in the general ward. For children in the ICU, one ulcer (3.6%) was stage 1, and two ulcers (7.1%) were stage 2. For children in the general ward, three ulcers (1.0%) were stage 1, and two ulcers (0.6%) were stage 2. The locations of the pressure ulcers are listed in Table 3.
| Characteristic | Intensive care unit (n = 28) | General pediatric ward (n = 314) |
| Pressure ulcer incidence | 3 (10.7%) | 5 (1.6%) |
| NPUAP stage | ||
| Stage 1 | 1 (3.6%) | 3 (1.0%) |
| Stage 2 | 2 (7.1%) | 2 (0.6%) |
| Location of pressure ulcer | ||
| Scalp | 1 (33.3%) | 0 |
| Nose | 1 (33.3%) | 0 |
| Face | 0 | 2 (40%) |
| Toe | 0 (0%) | 2 (40%) |
| Thumb | 0 | 1 (20%) |
| Ankle | 1 (33.3%) | 0 |
| Patients with mechanical ventilation, n | 0 (0%) | 5 (100%) |
The incidence of pressure ulcers during the second stage was 13/342 (3.8%) for children in the ICU. Among these, nine ulcers (2.6%) were stage 1 and four (1.2%) were stage 2. The locations of the pressure ulcers are presented in Table 4.
| Characteristic | Intensive care unit (n = 13) |
| Pressure ulcer incidence, n | 13 (3.8%) |
| Patients with mechanical ventilation, n | 12 (92.3%) |
| Patients with blood tumor, n | 7 (61.4%) |
| Postoperative patients, n | 6 (14.0%) |
| NPUAP stage | |
| Stage 1 | 9 (69.2%) |
| Stage 2 | 4 (30.8%) |
| Location of pressure ulcer | |
| Occiput | 3 |
| Nose | 3 |
| Buttocks | 2 |
| Ear | 1 |
| Head | 1 |
| Cervix | 1 |
| Heel | 1 |
| Toe | 1 |
| Transfer out | 11 (84.6%) |
| Leave hospital | 1 (7.7%) |
| Death, n | 1 (7.7%) |
For the second stage of the study, pressure ulcers were detected in 12/13 (92.3%) patients; seven cases had hematological tumor disease, including five cases (5/7, 71.4%) with hematopoietic stem cell transplantation, and four/six (66.7%) of the remaining cases after surgery required follow-up chemotherapy after tumor biopsy. Therefore, 11/13 (85%) cases of pressure ulcers had malignant tumors. Barthel rating scale was used to evaluate the patients’ performance in activities of daily living. The scores of 13 patients were 10-25 points, which belonged to severe dependence. Based on the children’s body mass index (BMI), assessed according to the criteria of the World Health Organization, there were four cases with BMI < 1 standard deviation (SD), one with BMI < 2 SD, and three with BMI < 3 SD (Table 5).
| Inpatient number | Sex (M/F) | Age (mo) | Weight (kg) | Main diagnosis | Other diagnosis | Time of staying in PICU (d) | Branden Q score | Barthel score | BMI score |
| 1047089 | F | 60 | 18.5 | Primary lymphoma of bone (stage IV) | After resection of left occipital tumor | 4 | 14 | 10 | 18.5 |
| 1093493 | F | 60 | 21 | T1-7 mixed intraspinal and extraspinal ganglioneuroblastoma (low risk) | 2 | 13 | 10 | 20 | |
| 632852 | F | 108 | 33 | Severe aplastic anemia after hematopoietic stem cell transplantation | Intracranial hemorrhage; graft versus host disease | 26 | 18 | 20 | 21.1 |
| 1116677 | F | 133 | 32 | Left thalamic and intraventricular variant astrocytoma (WHO stage III) | 6 | 15 | 10 | 15 | |
| 1126874 | F | 6 | 6.5 | Postoperative complications of resection of right skull base myofibroblastoma | Bronchopneumonia | 15 | 13 | 10 | 15.4 |
| 1066251 | M | 144 | 25 | Acute lymphoblastic leukemia after hematopoietic stem cell transplantation | Severe pneumonia; hyperacute graft versus host disease | 19 | 18 | 25 | 11.3 |
| 831463 | M | 156 | 45 | Cervical spinal cord injury | Multiple cervical fractures | 40 | 13 | 10 | 15.9 |
| 829101 | M | 48 | 17.7 | Severe aplastic anemia after hematopoietic stem cell transplantation | Acute graft versus host disease (stage IV) | 42 | 10 | 10 | 18.1 |
| 850224 | F | 110 | 24 | Postoperative complications of resection of ameloblastoma of left mandible | 3 | 14 | 10 | 13.2 | |
| 825633 | M | 36 | 10 | Acute lymphoblastic leukemia after hematopoietic stem cell transplantation | Severe pneumonia; hyperacute graft versus host disease (stage IV) | 11 | 16 | 10 | 11.8 |
| 868274 | F | 8 | 5 | Postoperative complications of right submandibular gland cyst resection | Protein energy malnutrition | 5 | 16 | 10 | 11.1 |
| 858433 | F | 121 | 25 | Right mandible osteosarcoma after surgery and chemotherapy | Abnormal liver function | 7 | 16 | 10 | 14.8 |
| 852006 | M | 24 | 12.4 | Acute lymphoblastic leukemia after hematopoietic stem cell transplantation | Severe pneumonia; acute graft versus host disease | 37 | 12 | 10 | 17.2 |
During the second stage, the laboratory examination of patients with pressure ulcer showed that the D-dimer results of 11 (84.6%) patients were > 0.55, and the C-reactive protein level in 10/13 (76.9%) patients was > 5. Furthermore, 9/13 (69.2%) patients had anemia with varying hemoglobin values (hemoglobin < 100 g/L; Table 6).
| Inpatient number | White blood cell count | Red blood cell count | Hemoglobin value | Platelet calculation | Blood pH value | CRP | D-Dimer (0-0.55) |
| 1047089 | 2.92 | 3.09 | 88 | 594 | 7.314 | 9.3 | 4.1 |
| 1093493 | 12.11 | 3.65 | 114 | 227 | 7.401 | < 5 | 1.35 |
| 632852 | 1.57 | 2.57 | 71 | 43 | 7.438 | 102.3 | 2.37 |
| 1116677 | 13.71 | 3.23 | 97 | 194 | 7.435 | 75.1 | 2.77 |
| 1126874 | 6.24 | 3.37 | 91 | 247 | 7.301 | 62 | 0.23 |
| 1066251 | 9.56 | 2.86 | 108 | 66 | 7.374 | < 5 | 0.33 |
| 831463 | 9.56 | 2.86 | 108 | 66 | 7.385 | < 5 | 0.33 |
| 829101 | 13.8 | 2.97 | 87 | 375 | 7.392 | < 5 | 7.85 |
| 850224 | 9.66 | 2.48 | 75 | 28 | 7.331 | 57.9 | 2.59 |
| 825633 | 11.7 | 2.69 | 78 | 220 | 7.439 | 58.7 | 1.27 |
| 868274 | 5.68 | 3.63 | 101 | 67 | 7.441 | 18.3 | 7.8 |
| 858433 | 9.93 | 4.45 | 110 | 643 | 7.35 | 23.9 | 1.48 |
| 852006 | 5.61 | 2.88 | 89 | 239 | 7.402 | 72.2 | 2.65 |
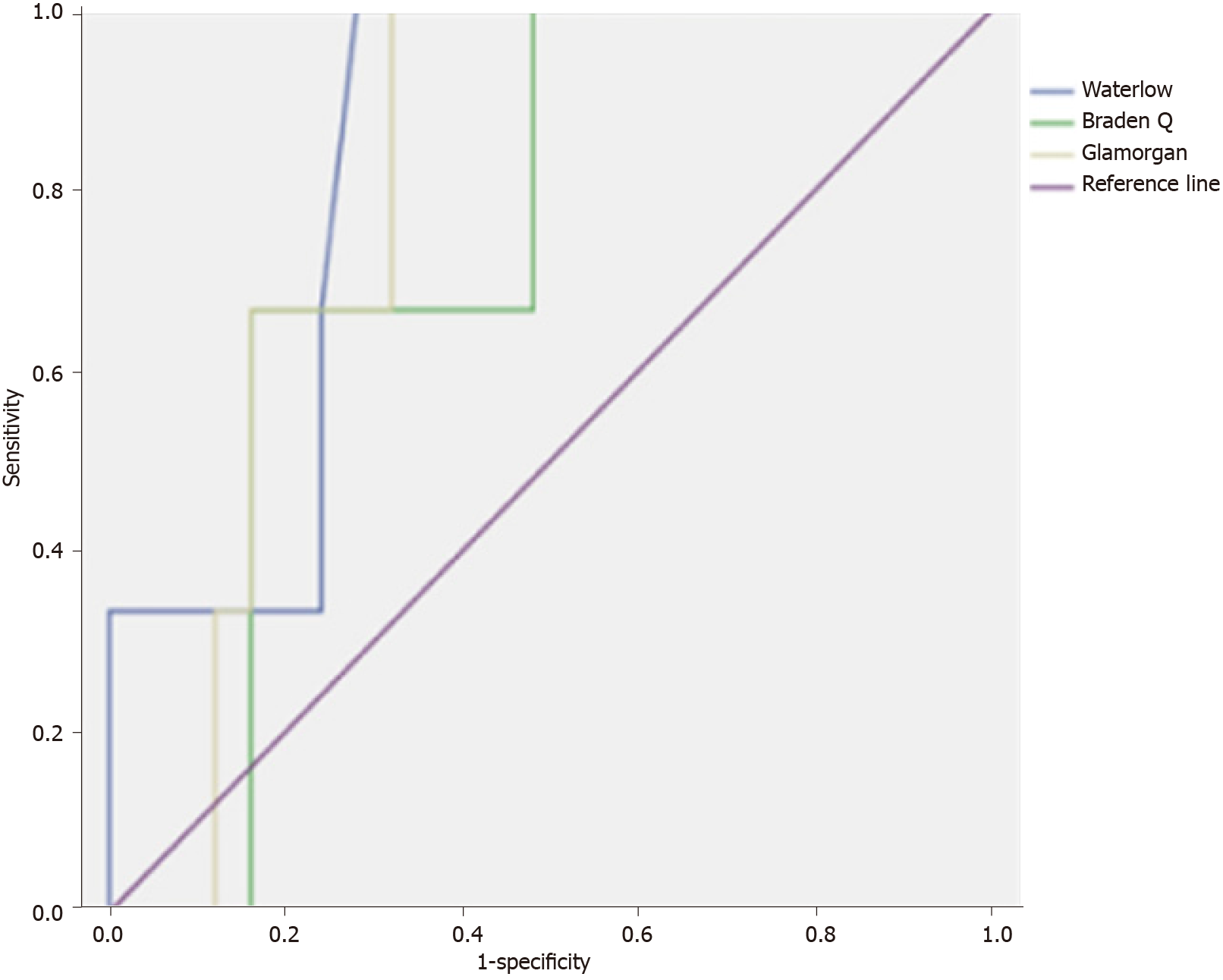
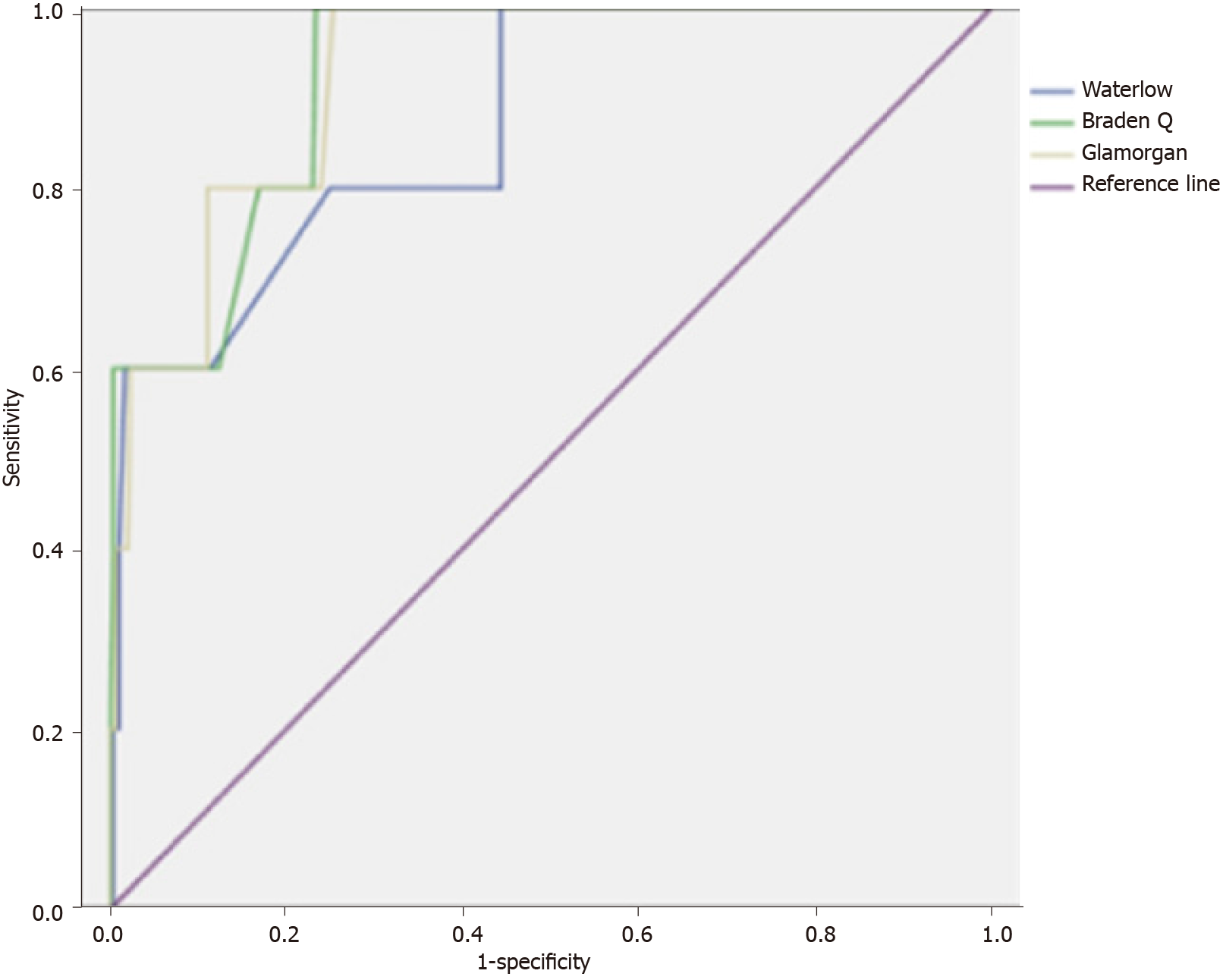
For children in the ICU, the AUC values for the Waterlow, Braden Q, and Glamorgan scales were 0.833, 0.733, and 0.800, respectively (Figure 1). Although this indicated that the Waterlow scale might have the best overall accuracy in predicting the development of pressure ulcers in the PICU, the interpretation should be made with caution due to the wide 95% confidence intervals (CIs) (Table 3). The Waterlow, Braden Q, and Glamorgan scales had optimal cut-off values of 13, 16, and 27 points, respectively. With the optimal cut-off value, the sensitivity was 0.667 for all three scales, while the specificity was 0.720 for the Waterlow scale, 0.840 for the Braden Q scale, and 0.720 for the Glamorgan scale. Table 3 compares the sensitivity, specificity, PPV, and NPV between the three risk assessment scales for PICU patients.
For children admitted to the general ward, the Waterlow, Braden Q, and Glamorgan scales had an AUC of 0.870, 0.924, and 0.923, respectively (Figure 2). Although this suggested a superior overall predictive accuracy for the Braden Q and Glamorgan tools when used in general wards, no definitive conclusion could be drawn due to the substantial overlap of the 95%CIs (Table 3). The optimal cut-off values for the Waterlow, Braden Q, and Glamorgan scales were 14, 14, and 29 points, respectively. At the appropriate optimal cut-off value, the Waterlow, Braden Q, and Glamorgan scales had a sensitivity of 0.600 and specificity of 0.990, 0.980, and 0.790, respectively. Table 3 lists the sensitivity, specificity, PPV, and NPV for the three risk assessment scales when used in the patients in the general ward.
The main finding of the present study was that all three risk assessment scales showed a reasonable performance in the prediction of pressure ulcer development in hospitalized pediatric patients. The Waterlow scale had the highest AUC value among the three instruments for children in the ICU, while the Braden Q and Glamorgan scales had high AUC values for children in the general ward. Together, our data suggest that the optimal instrument needs to be selected according to the clinical setting.
In the present study, the AUC values of the Waterlow, Braden Q, and Glamorgan scales were 0.833, 0.733, and 0.800, respectively, in the PICU and 0.870, 0.924, and 0.923, respectively, in the general ward (Table 7). The AUC value range was 0.5-1.0; a high value reflected better overall diagnostic/predictive accuracy in the clinical setting[24]. Thus, based on the AUC values, our findings indicated that the Waterlow scale might exhibit the best overall accuracy in the PICU, whereas the Braden Q and Glamorgan instruments might have superior accuracy in the general pediatric ward. However, these interpretations should be made with caution due to the large overlap of 95%CIs and would need to be tested in a future study with large sample size.
| Scale | AUC (95%CI) | Optimal cut-off | Sensitivity | Specificity | PPV | NPV |
| Intensive care unit | ||||||
| Waterlow | 0.833 (0.653-1.000) | ≤ 13 | 0.667 | 0.720 | 0.100 | 0.900 |
| Braden Q | 0.733 (0.508-0.959) | ≤ 16 | 0.667 | 0.840 | 0.090 | 0.910 |
| Glamorgan | 0.800 (0.629-0.971) | ≤ 27 | 0.667 | 0.720 | 0.100 | 0.900 |
| General ward | ||||||
| Waterlow | 0.870 (0.718-1.000) | ≤ 14 | 0.600 | 0.990 | 0.010 | 0.990 |
| Braden Q | 0.924 (0.838-1.000) | ≤ 14 | 0.600 | 0.980 | 0.010 | 0.990 |
| Glamorgan | 0.923 (0.839-1.000) | ≤ 29 | 0.600 | 0.790 | 0.013 | 0.987 |
In the present study, the optimal cut-off values for the Waterlow, Braden Q, and Glamorgan scales were 13, 16, and 27 points, respectively, when administered to patients in the PICU and 14, 14, and 29 points, respectively, when administered to patients in the general ward. In the PICU, the sensitivity of all three scales was 0.667, while the specificity was 0.720, 0.840, and 0.720 for the Waterlow, Braden Q, and Glamorgan scales, respectively. Although the AUC value was the highest for the Waterlow scale, the Braden Q scale had the highest specificity suggesting that it may be the most useful tool for PICU. In the general ward, the sensitivity was 0.600 for all three scales, and the specificity was 0.990, 0.980, and 0.790 for the Waterlow, Braden Q, and Glamorgan scales, respectively. Thus, the Braden Q and Waterlow scales had better specificities than the Glamorgan scale. Although our data are preliminary, we tentatively suggested that the Braden Q tool has the best overall performance in both the general pediatric ward and the PICU.
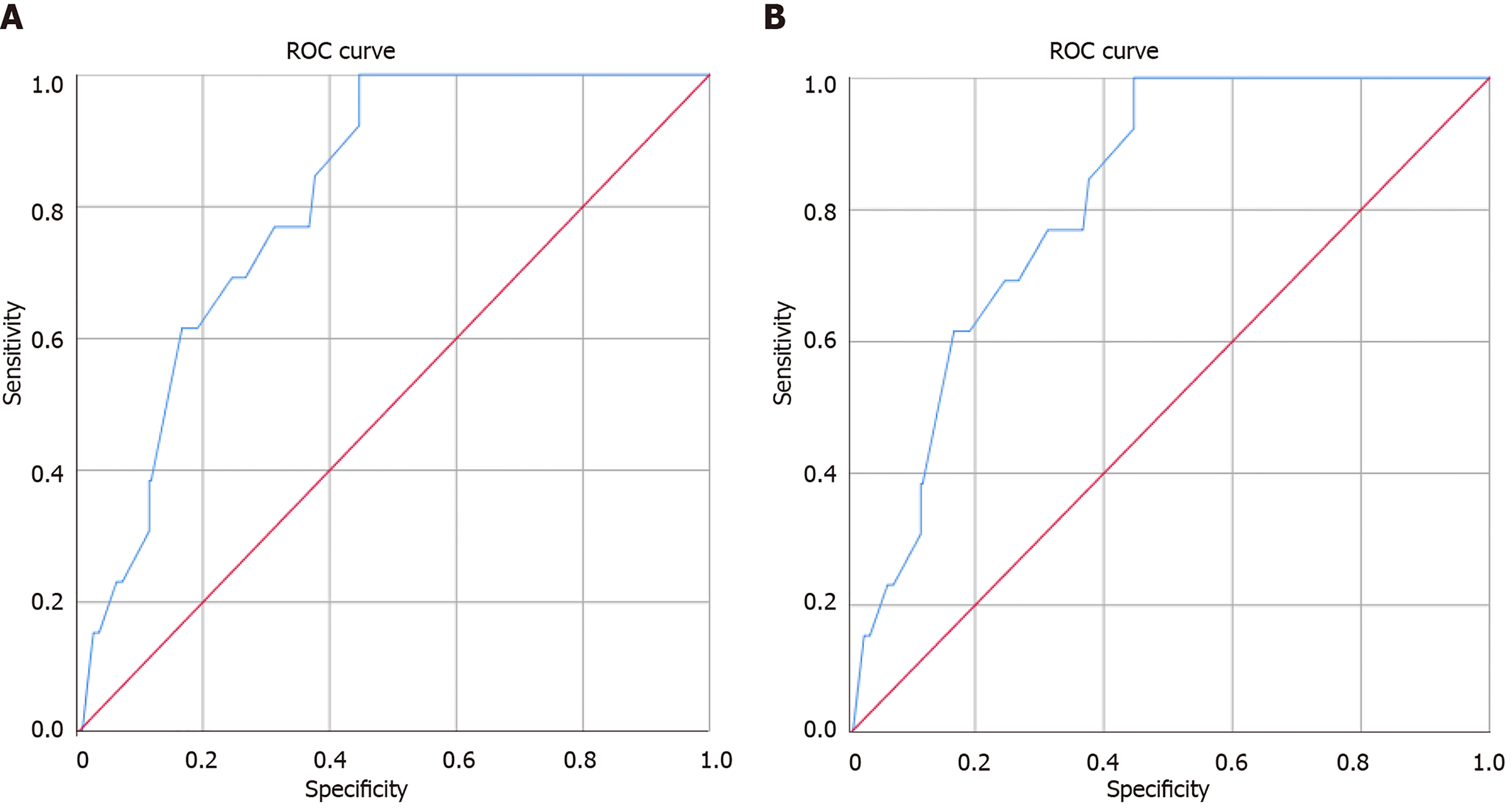
According to the previously obtained results, the Braden Q scale demonstrated the most satisfactory performance and we used it to predict pressure ulcers in pediatric patients during the second stage of the study, from January 2018 to December 2020. The AUC value of the Braden Q scale was 0.810, the optimal cut-off value was 18.35 points, the sensitivity was 1.0, and the specificity was 0.553, which were slightly higher compared to results obtained during the first stage (Figure 3).
In previous studies, the Braden Q scale had a sensitivity of 0.88 and specificity of 0.58[13,14], while the Glamorgan scale had a sensitivity of 0.984 and specificity of 0.674[10]. Although the previous studies did not distinguish between patients in the PICU and general ward, the sensitivity values were higher and specificity values lower than those obtained in both settings (i.e., PICU and general ward) in our study. Other studies conducted in the PICU yielded a sensitivity of 0.88 (cut-off value 20 points) for the Waterlow scale, 0.83 (cut-off value 16 points) for the Braden Q scale, and 0.87 (cut-off value 29 points) for the Glamorgan scale, while the sensitivity values for children in the general ward were 0.83 (cut-off value 25 points) for the Waterlow scale, 0.87 (cut-off value 18 points) for the Braden Q scale, and 0.98 (cut-off value 33 points) for the Glamorgan scale[17]. Furthermore, the AUC values for the Waterlow, Braden Q, and Glamorgan scales in previous studies were 0.69, 0.83, and 0.73, respectively, in the PICU and 0.45, 0.83, and 0.47, respectively, in the general ward[25,26]. These data differed slightly from those reported in the present study, which could be attributed to the varied underlying medical conditions and general health status of the patients between different studies. These discrepancies might have influenced the risk of the development of pressure ulcers and their incidence.
Concurrently, in order to confirm the integrity of the results obtained in the first stage of the study, the second stage was undertaken in order to evaluate Braden Q scale performance in PICU from January 2018 to December 2020. The results showed that the Braden Q scale had an optimal AUC value in predicting pressure ulcers in PICU, which was slightly better than the previous data in 2017, supporting the hypothesis that the Braden Q scale could successfully predict the occurrence of pressure ulcers in PICU. In addition, 60% of the children with severe diseases included in the second stage of the study had blood cancer and the Braden Q scale was useful in predicting the pressure ulcer in this group of patients. Conversely, for children with pressure ulcers, during both stages of the study, mechanical ventilation was associated with an increased risk, which needs further follow-up.
The second stage of the study included 342 cases from 2018 to 2020, and children with blood cancer accounted for a large proportion of the patients. Among the 13 cases of pressure ulcer, 92.3% were on ventilator-assisted breathing, and in those who developed pressure ulcer, the hemoglobin level was low (55-114) g/L in 9 (69.2%) cases and < 100 g/L in 9 (21.1%) cases. In addition, nutritional status, tissue perfusion, and oxygenation are reflected in the Braden Q scale, thus we recommend closer observation in the above issues to prevent the occurrence of pressure ulcers (Table 8). The scoring for some of the items in these risk assessment scales was subjective, resulting in disparities between results, obtained in different stages. The values should be adjusted in accordance with the patient’s test results, the score of physical indicators, and the objective values from the nursing records, such as blood pressure and excretion.
| Inpatient number | Mobility | Activity | Sensory perception | Moisture | Friction-shear | Nutrition | Tissue perfusion and oxygenation | Total score |
| 1047089 | 1 | 1 | 1 | 3 | 2 | 2 | 4 | 14 |
| 1093493 | 1 | 1 | 1 | 3 | 2 | 1 | 4 | 13 |
| 632852 | 3 | 1 | 4 | 4 | 3 | 1 | 2 | 18 |
| 1116677 | 1 | 1 | 1 | 4 | 2 | 2 | 4 | 15 |
| 1126874 | 1 | 1 | 2 | 3 | 1 | 2 | 3 | 13 |
| 1066251 | 3 | 1 | 4 | 4 | 2 | 2 | 2 | 18 |
| 831463 | 1 | 1 | 1 | 4 | 2 | 2 | 3 | 13 |
| 829101 | 2 | 1 | 3 | 4 | 1 | 1 | 2 | 10 |
| 850224 | 1 | 1 | 1 | 4 | 2 | 2 | 3 | 14 |
| 825633 | 3 | 1 | 3 | 2 | 3 | 1 | 3 | 16 |
| 868274 | 1 | 1 | 3 | 2 | 3 | 2 | 4 | 16 |
| 858433 | 1 | 1 | 1 | 4 | 3 | 3 | 3 | 16 |
| 852006 | 1 | 1 | 1 | 4 | 2 | 1 | 2 | 12 |
The data obtained from the first stage in 2017 or second stage in 2018-2020 differ from some of the reports published previously. Nonetheless, our results provide information on the putative clinical application of the three risk assessment scales in the prediction of pressure ulcer development in hospitalized children. In our study, the Braden Q scale was an optimal tool for predicting pressure ulcers in PICU patients and additional studies across multiple centers with a larger sample size would substantiate the current findings.
In addition, the constituent items of the Braden Q scale include hemoglobin content, blood oxygen saturation and friction items of independent patients. These items can better reflect the status of children with blood tumors. The Braden Q scale demonstrated the highest specificity and could be successfully used as a tool for the prediction of pressure ulcers in PICU patients.
The Waterlow, Braden Q, and Glamorgan scales have comparable performance, while the Braden Q scale demonstrates a better specificity and can be successfully used by pediatric nurses to identify patients at high risk of pressure ulcers in PICU.
Many scales are available to predict the risk of pressure ulcers in children. However, the performances of those scales have not yet been compared in China.
To explore the value of pressure ulcer evaluation scales in Chinese pediatric patients.
To compare the Waterlow, Braden Q, and Glamorgan scales, and identify more suitable pressure ulcer evaluation scale for the pediatric intensive care unit (PICU).
Trained nurses used the Waterlow, Braden Q, and Glamorgan scales to assess pediatric patients at Sun Yat-sen Memorial Hospital (China) within 24 h of admission, from May 2017 to December 2020 in two stages. Skin examination was carried out to identify pressure ulcers every 3 d for 3 wk.
For PICU, the Waterlow, Braden Q, and Glamorgan scales had slightly lower area under the operating characteristic curve (AUC) of 0.833, 0.733, and 0.800, respectively, and optimal cut-off values of 13, 16, and 27 points. Braden Q demonstrated a satisfactory specificity, and during the second stage of the study for PICU patients, the AUC of the Braden Q scale was 0.810, with an optimal cut-off value of 18.35 points.
The Waterlow, Braden Q, and Glamorgan scales have comparable performance, while the Braden Q scale demonstrates a better specificity and can be successfully used by pediatric nurses to identify patients at high risk of pressure ulcers in PICU.
In our study, the Braden Q scale is an optimal tool for predicting pressure ulcers in PICU patients, and additional studies across multiple centers with a larger sample size would substantiate the current findings.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: KHURRAM MF S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Freundlich K. Pressure Injuries in Medically Complex Children: A Review. Children (Basel). 2017;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Pellegrino DMS, Chacon JMF, Blanes L, Ferreira LM. Prevalence and incidence of pressure injuries in pediatric hospitals in the city of São Paulo, SP, Brazil. J Tissue Viability. 2017;26:241-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Razmus I, Bergquist-Beringer S. Pressure Injury Prevalence and the Rate of Hospital-Acquired Pressure Injury Among Pediatric Patients in Acute Care. J Wound Ostomy Continence Nurs. 2017;44:110-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Hu J. Incidence and prevalence of medical device-related pressure ulcers in children and adults. Evid Based Nurs. 2020;23:62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Anthony D, Alosaimi D, Shiferaw WS, Korsah K, Safari R. Prevalence of pressure ulcers in africa: A systematic review and meta-analysis. J Tissue Viability. 2021;30:137-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Sánchez-Lorente MM, Sanchis-Sánchez E, García-Molina P, Balaguer-López E, Blasco JM. Prevalence of pressure ulcers in the paediatric population and in primary health care: An epidemiological study conducted in Spain. J Tissue Viability. 2018;27:221-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Cummins KA, Watters R, Leming-Lee T'. Reducing Pressure Injuries in the Pediatric Intensive Care Unit. Nurs Clin North Am. 2019;54:127-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Willock J, Habiballah L, Long D, Palmer K, Anthony D. A comparison of the performance of the Braden Q and the Glamorgan paediatric pressure ulcer risk assessment scales in general and intensive care paediatric and neonatal units. J Tissue Viability. 2016;25:119-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Quigley SM, Curley MA. Skin integrity in the pediatric population: preventing and managing pressure ulcers. J Soc Pediatr Nurs. 1996;1:7-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 79] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 10. | Willock J, Baharestani MM, Anthony D. The development of the Glamorgan paediatric pressure ulcer risk assessment scale. J Wound Care. 2009;18:17-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Waterlow J. Pressure sores in children: risk assessment. Paediatr Nurs. 1998;10:22-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Razmus I, Bergquist-Beringer S. Pressure Ulcer Risk and Prevention Practices in Pediatric Patients: A Secondary Analysis of Data from the National Database of Nursing Quality Indicators®. Ostomy Wound Manage. 2017;63:28-32. [PubMed] |
| 13. | Curley MA, Razmus IS, Roberts KE, Wypij D. Predicting pressure ulcer risk in pediatric patients: the Braden Q Scale. Nurs Res. 2003;52:22-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 114] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 14. | Noonan C, Quigley S, Curley MA. Using the Braden Q Scale to Predict Pressure Ulcer Risk in pediatric patients. J Pediatr Nurs. 2011;26:566-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Liao Y, Gao G, Mo L. Predictive accuracy of the Braden Q Scale in risk assessment for paediatric pressure ulcer: A meta-analysis. Int J Nurs Sci. 2018;5:419-426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Chun X, Lin Y, Ma J, He J, Ye L, Yang H. Predictive efficacy of the Braden Q Scale for pediatric pressure ulcer risk assessment in the PICU: a meta-analysis. Pediatr Res. 2019;86:436-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Kottner J, Kenzler M, Wilborn D. Interrater agreement, reliability and validity of the Glamorgan Paediatric Pressure Ulcer Risk Assessment Scale. J Clin Nurs. 2014;23:1165-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Charalambous C, Koulori A, Vasilopoulos A, Roupa Z. Evaluation of the Validity and Reliability of the Waterlow Pressure Ulcer Risk Assessment Scale. Med Arch. 2018;72:141-144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Anthony D, Willock J, Baharestani M. A comparison of Braden Q, Garvin and Glamorgan risk assessment scales in paediatrics. J Tissue Viability. 2010;19:98-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Kottner J, Hauss A, Schlüer AB, Dassen T. Validation and clinical impact of paediatric pressure ulcer risk assessment scales: A systematic review. Int J Nurs Stud. 2013;50:807-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Zhang X. Ertong yachuang fengxian pinggu gongju de yanjiu xianzhuang. Chinese General Practice Nursing. 2020;18 (20):2497-2499. [DOI] [Full Text] |
| 22. | Jiang CW, Y Q, Tu GF. Liangzhong liangbiao yuce xinshegner zhongzheng jianhu bingfang huanzhe yachuang fengxian de xiaoneng bijiao. Chinese Journal of Reproductive Health. 2017;28 (06):549-515. [DOI] [Full Text] |
| 23. | Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised Pressure Injury Staging System. J Wound Ostomy Continence Nurs. 2016;43:585-597. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 430] [Cited by in RCA: 663] [Article Influence: 82.9] [Reference Citation Analysis (0)] |
| 24. | Tang LL, Zhang W, Li Q, Ye X, Chan L. Least squares regression methods for clustered ROC data with discrete covariates. Biom J. 2016;58:747-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Wang YB. Waterlow pressure sores Risk Factor Assessment Table to evaluate the effectiveness of preventing pressure sores. Zhongguo shiyong huli zazhi. 2015;31 (5):359-360. |
| 26. | Lu YFL, J H, Lu XW. Braden-Q ertong yachuang pinggu liangbiao de yucexing yanjiu. Shanghai jiaotong daxue xuebao (Yixue ban). 2013;33 (5):561-564. |