Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.10937
Peer-review started: February 3, 2021
First decision: July 16, 2021
Revised: July 22, 2021
Accepted: September 7, 2021
Article in press: September 7, 2021
Published online: December 16, 2021
Processing time: 309 Days and 18.4 Hours
Needle stick and sharps injuries (NSIs) may cause infections among medical personnel. Obesity and overtime work among medical personnel increase the incidence of work injuries.
To investigate whether overtime work and obesity increase the risk of NSIs.
This cross-sectional study used the data of 847 hospital personnel, including 104 doctors, 613 nurses, 67 medical laboratory scientists, 54 specialist technicians, and nine surgical assistants. Of them, 29 participants notified the hospital of having at least one NSI in 2017. The data collected included age, overtime work, body mass index, medical specialty such as doctor or nurse, and professional grade such as attending physician or resident. The χ2 and Fisher’s exact tests were used to compare categorical variables. Multiple logistic regression analysis and the Sobel test were used to assess the risk of NSIs.
Overtime work, body weight, and medical specialty were significantly associated with NSIs (P < 0.05). After adjustment for risk factors, heavy overtime work was an independent risk factor for NSIs, and healthy body weight and nursing specialty were independent protective factors against NSIs. After adjustment for risk factors, medical personnel with healthy body weight has half as many NSIs as those with unhealthy body weight; the proportion of NSIs in doctors with healthy body weight was 0.2 times that in doctors with unhealthy body weight; the proportion of injuries among residents was 17.3 times higher than that among attending physicians; the proportion of injuries among junior nurses was 3.9 times higher than that among experienced nurses; the proportion of injuries among nurses with heavy overtime work was 6.6 times higher than that among nurses with mild overtime work; and the proportion of injuries among residents was 19.5 times higher than that among junior nurses. Heavy overtime work mediated the association of medical specialty with NSIs.
In addition to promoting the use of safety needles and providing infection control education, managers should review overtime schedules, and medical personnel should be encouraged to maintain a healthy weight.
Core tip: Needle stick and sharp injuries (NSIs) are complex multifactorial processes that are commonly observed in physical, psychological, and environmental fields. Therefore, preventing NSIs in medical personnel remains a critical health issue. To reduce the risk of NSIs, other factors affecting their incidence, such as medical specialty and body weight, should be analyzed. We investigated whether overtime and obesity increase the risk of NSIs. We also aimed to provide insights into the development of more effective prevention plans for NSIs. To the best of our knowledge, these findings have never been reported.
- Citation: Chen YH, Yeh CJ, Jong GP. Association of overtime work and obesity with needle stick and sharp injuries in medical practice. World J Clin Cases 2021; 9(35): 10937-10947
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/10937.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.10937
Needlestick and sharp injuries (NSIs) carry the risk of various infections, such as hepatitis B, hepatitis C, and human immunodeficiency virus (HIV) infections[1,2]. In 2000, occupational exposure to percutaneous injuries caused by medical personnel resulted in 16000 cases of hepatitis C, 66000 cases of hepatitis B, and 1000 cases of HIV worldwide[3]. The mean number of NSIs per 100 occupied beds per year was 4.8–7.6 from 2009 to 2011 in Japan[4]. Poor organizational climate and high workloads are associated with NSIs and near-misses in nurses[5]; however, the incidence of NSIs remains higher among doctors, commonly due to stress or overwork, followed by careless attitude[6]. This careless attitude can be effectively reduced by providing preventive education[7-10] and supplying protective equipment for procedures such as intravenous access or blood draws[5]. Some occupational factors, such as long working hours and overtime, can increase the risk of NSIs among medical personnel[11,12]; the risk of work-related injuries due to overtime has also been observed in other occupations[13]. According to the Survey of Occupational Injuries and Illnesses compiled by the United States Department of Labor, overtime work increased the injury hazard rate by 61%. In particular, the injury hazard rate was increased by 37% and 23% for work that lasted more than 12 h daily and 60 h, respectively, per week[13]. To ensure that medical services are promptly delivered, medical personnel routinely extend their working hours in cases of personnel shortage or sudden spikes in demand at the medical site. In Taiwanese hospitals, medical personnel working overtime mainly comprise doctors, 40% of whom work more than 60 h per week. In particular, 97% and 83% of doctors in medical centers and regional hospitals, respectively, work overtime[14].
Obesity has been significantly associated with diseases such as type 2 diabetes, cardiovascular diseases, and several forms of cancer[15] and occupational injuries[16]. Occupational injuries caused by obesity generally comprise sprains, strains, lower limb injuries, and falls[17]. However, a study found no significant relationship between obesity and contact with sharp material agents without adjusting for medical specialty and overtime work[16]. Male health workers were found to be 10 times more likely than female health workers to encounter NSIs[18]. Furthermore, low work experience was associated with high NSI incidence among nurses[9], and resident doctors (RDs) have a higher incidence of NSIs than do attending physicians (APs)[19]. NSI incidence among doctors differed from that among nurses[7], and RDs had a higher incidence than APs and nurses[19].
NSIs are complex multifactorial processes that are related to physical, psychological and environmental fields. Therefore, preventing NSIs in medical personnel remains a critical health issue. To further reduce the risk of NSIs, other factors affecting NSI incidence should be analyzed, such as medical specialty and body weight (BW), and an effective prevention plan should be developed accordingly.
This cross-sectional study used data regarding doctors, nurses, and medical laboratory scientists working in Chung Shan Medical University Hospital, Taichung, Taiwan, recorded during 2017. The following data were collected: sex, age, height, weight, intensity of overtime work, medical specialty (doctor, nurse, medical laboratory scientist, specialist, or surgical assistant), professional level (AP or RD for doctors and N, N1, N2, N3 or N4 for nurses based on The Guidelines of Nursing Clinical Ladder System Program in Hospital). In this study, nurses with the professional level of N, which represents < 1 year of clinical work, were categorized as junior nurses (JNs) and nurses with higher levels were categorized as experienced nurses. We defined a medical laboratory scientist as a professional technician (excluding pathology laboratory personnel), a specialized technician as a specialist nurse in some medical specialty, and a surgical assistant as a person who assists a doctor in performing a surgical operation.
This study included 847 participants (104 doctors, 613 nurses, 67 medical laboratory scientists, 54 specialist technicians, and nine surgical assistants). Among them, 29 notified the hospital of having at least one NSI in 2017; NSIs were recorded by the hospital’s occupational safety and health department. In this study, the aforementioned data were analyzed after depersonalization. Body weight was classified according to the definition of overweight or obesity by the Health Promotion Administration, Ministry of Health and Welfare. Specifically, body mass index (BMI) between 18.5 and 24.0 was considered a healthy BW (HBW), and any other BMI outside this range was considered an unhealthy BW (UHBW). Overtime work was classified according to the workload levels in the Guidelines for Prevention of Diseases Caused by Abnormal Workloads (Second Edition) from the Occupational Safety and Health Administration, Ministry of Labor. Specifically, extra work (both overtime and non-overtime) was categorized as slight (< 45 h/mo), moderate (45–80 h/mo), and heavy (> 80 h/mo) overtime work, respectively.
All statistical analyses were conducted using SAS v6.1 (SAS Institute, Cary, NC, United States). In addition, the χ2 and Fisher’s exact tests were used to compare categorical variables. Multiple logistic regression analysis was used to analyze the correlation of NSI with the study’s main variables. The mediation effect was determined using the following approach proposed by Baron and Kenny (1986)[20]: (1) The independent variable (IV) significantly affects the mediator (first-stage effect); (2) The IV significantly affects the dependent variable (DV) in the absence of the mediator; (3) The mediator has a significant unique effect on the DV (second-stage effect); and (4) The effect of the IV on the DV decreases upon the addition of the mediator to the model. Finally, the Sobel test[21] was conducted to determine the significance of this mediation effect, for which the sample size was required to be at least 200[22]. Before performing the Sobel test, if the IV, mediator, or DV was not continuous, the logistic regression coefficient was standardized: X is an independent variable, Y is a dependent variable and M is an adjusting variable (mediating factor) in a simple mediating model. a is the unary logistic regression coefficient of X against M when M is the dependent variable and X is the independent variable. b is the logistic regression coefficient of M against Y in a simple mediating model. c is the unary logistic regression coefficient of X against Y, and c' is the logistic regression coefficient of X against Y with M as the adjusting variable. Moreover, Sa and Sa were the standard errors of a and b, respectively. Mediation analysis for categorical variables was conducted following the method recommended by Iacobucci (2012)[23].
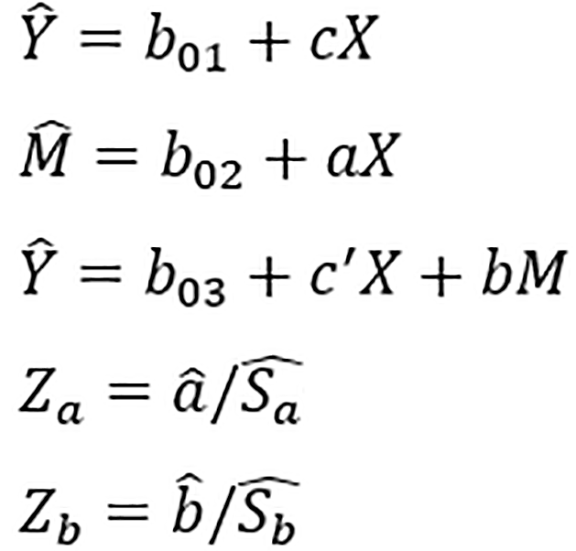
The original Sobel test formula was modified as follows:
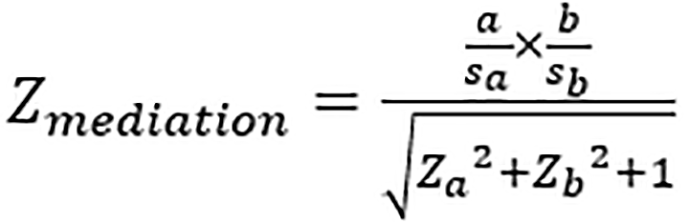
It was considered significant at the α = 0.05 Level if its value exceeded |1.96| (for a two-tailed test with α = 0.05). In this study, statistical significance was indicated by P < 0.05.
This study was approved by Institutional Review Board of Chung Shan Medical University Hospital on December 2, 2019 (CSMUH No: CS19137).
Table 1 presents the participant characteristics, including sex, body weight, and level of overtime work. If the χ2 test’s assumptions were violated, Fisher’s exact test was performed. Medical personnel were classified as doctors, nurses, and others (which included medical laboratory scientists, specialist nurses, and surgical assistants). Different types of medical personnel differed significantly in terms of NSI, sex, age, and moderate or heavy overtime (Table 1). Among them, the proportion of NSIs was the highest among doctors (7.7%). Furthermore, our cohort had an exceptionally low proportion of male nurses, with 95.9% of nurses being female; by contrast, the proportion of female doctors was lower (26.9%). Among the medical specialties, nurses were the youngest, with a mean age of 33.6 years. Moreover, no significant differences were observed in HBW between the three groups. The proportions of moderate and heavy overtime work among doctors (29.8% and 16.3%, respectively) were significantly higher than those among nurses and others.
| Variable | Totaln | NSIs | Female | Age | HBW | Moderate OT | Heavy OT | |||||||||||
| n | % | P1 | n | % | P1 | mean ± SD | P2 | n3 | % | P1 | n | % | P | n | % | P1 | ||
| Profession groups | ||||||||||||||||||
| Doctors | 104 | 8 | 7.7 | a | 28 | 26.9 | c | 40.9 ± 10.4 | c | 53 | 51.0 | NS | 31 | 29.8 | b | 17 | 16.3 | c |
| Nurses | 613 | 16 | 2.6 | 588 | 95.9 | 33.6 ± 8.3 | 354 | 57.8 | 147 | 24.0 | 28 | 4.6 | ||||||
| Others | 130 | 5 | 3.9 | 95 | 73.1 | 40.6 ± 7.1 | 64 | 49.2 | 15 | 11.5 | 0 | 0.0 | ||||||
| Profession grade (doctor) | ||||||||||||||||||
| AP | 71 | 1 | 1.4 | b | 14 | 19.7 | a | 45.5 ± 9.3 | c | 33 | 46.5 | NS | 22 | 31.0 | b | 6 | 8.5 | b |
| RD | 33 | 7 | 21.2 | 14 | 42.4 | 31.0 ± 2.9 | 20 | 60.6 | 9 | 27.3 | 11 | 33.3 | ||||||
| Profession grade (nurse) | ||||||||||||||||||
| N | 129 | 8 | 6.2 | 3 | 119 | 92.2 | NS | 25.3 ± 3.3 | c | 78 | 60.5 | NS | 42 | 32.6 | a | 6 | 4.7 | NS |
| N1 | 134 | 1 | 0.8 | 128 | 95.5 | 29.0 ± 4.9b | 70 | 52.2 | 35 | 26.1 | 3 | 2.2 | ||||||
| N2 | 145 | 3 | 2.1 | 140 | 96.6 | 34.6 ± 6.7 | 84 | 57.9 | 24 | 16.6 | 9 | 6.2 | ||||||
| N3 | 143 | 4 | 2.8 | 140 | 97.9 | 40.5 ± 6.5 | 86 | 60.1 | 29 | 20.3 | 6 | 4.2 | ||||||
| N4 | 62 | 0 | 0 | 61 | 98.4 | 42.3 ± 4.8 | 36 | 58.1 | 17 | 27.4 | 4 | 6.5 | ||||||
Among doctors, APs and RDs differed significantly in terms of NSIs, sex, age, and moderate and heavy overtime, but not in terms of HBW. The proportion of NSIs among RDs (21.2%) was considerably higher than that among APs (21.2% vs 1.4%, P < 0.01). The significant difference in age between RDs and APs was expected due to the training system (45.5 vs 31.0, P < 0.0001). The proportion of moderate overtime was higher among APs than RDs (31.0% vs 27.3%, P < 0.01) but that of heavy overtime was considerably higher among RDs than APs (33.3% vs 8.5%, P < 0.01).
Nurses of different professional grades (N1–N4) differed significantly in terms of age (P < 0.0001) and moderate overtime (P < 0.05). Nurses with the professional level of N had the highest proportion of NSIs (6.2%). Age increased with the professional grade, which was expected due to the nursing clinical ladder system. Among nurses, nurses with the professional level of N had the highest proportion of moderate overtime work (32.6%), but the proportion of heavy overtime work was not the highest in this group (4.7%).
As presented in Table 2, the proportion of NSIs in participants with HBW was 0.5 times [odds ratio (OR) = 0.5, P < 0.05] that in participants with UHBW in the M1 model of all participants. The proportion of NSIs in doctors with HBW was 0.2 times (OR = 0.2, P < 0.05) that in doctors with UHBW in the M2 model of doctors. In addition, the proportion of NSIs in nurses with HBW was 0.5 times that in nurses with UHBW, but the difference was not significant.
| Main effect | ORs of NSIs for All participants | ORs of NSIs for doctors | ORs of NSIs for nurses | ||||||||||
| N | n | M0 | M1 | N | n | M0 | M2 | N | n | M0 | M2 | ||
| Body weight level | HBW | 471 | 11 | 0.5NS | 0.5a | 53 | 2 | 0.3 | 0.2a | 354 | 7 | 0.6 | 0.5 |
| UHBW | 376 | 18 | 1.0 | 1.0 | 51 | 6 | 1.0 | 1.0 | 259 | 9 | 1.0 | 1.0 | |
| OT work | Heavy | 45 | 6 | 5.7b | 4.3a | 17 | 4 | 5.4a | 2.0 | 28 | 2 | 3.7 | 3.8 |
| Moderate | 193 | 7 | 1.4 | 1.2 | 31 | 1 | 0.6 | 0.5 | 147 | 5 | 1.7 | 1.4 | |
| Mild | 609 | 16 | 1.0 | 1.0 | 56 | 3 | 1.0 | 1.0 | 438 | 9 | 1.0 | 1.0 | |
| Type of medical personnel | Doctors | 104 | 8 | 2.1 | 1.3 | - | - | - | - | - | - | - | - |
| Nurses | 613 | 16 | 0.7 | 0.3a | - | - | - | - | - | - | - | - | |
| Others | 130 | 5 | 1.0 | 1.0 | - | - | - | - | - | - | - | - | |
| Professional grade (Doctors) | RD | - | - | - | - | 33 | 7 | 18.9b | 17.3a | - | - | - | - |
| AP | - | - | - | - | 71 | 1 | 1.0 | 1.0 | - | - | - | - | |
| Professional grade (Nurses) | Junior | - | - | - | - | - | - | - | - | 129 | 8 | 3.9b | 3.9b |
| experiencing | - | - | - | - | - | - | - | - | 484 | 8 | 1.0 | 1.0 | |
Table 2 presents a clear effect of heavy overtime work on NSIs: medical personnel with heavy overtime work were 4.3–5.7 times more likely to experience an NSI than those with mild overtime work, and the difference was significant. Similarly, NSIs occurred 5.4 times more proportion in doctors with heavy overtime work (OR = 5.4, P < 0.05) than in those with slight overtime work; however, this effect could be explained by the other effects such as HBW (OR = 0.2, P < 0.05) and RDs (OR = 17.3, P < 0.05). Although nurses with heavy overtime work experienced more NSIs (OR = 3.7 and 3.8) than others, the difference was not significant.
Doctors experienced more NSIs incidence than other types of medical personnel, but the difference was nonsignificant (OR = 1.3–2.1, P > 0.05). After adjustment for other variables (M1 model), the nurse specialty was identified as an independent protective factor for NSIs (OR = 0.3, P < 0.05). Among doctors, regardless of whether adjustments were made for other variables, being an RD was an independent risk factor for NSIs (OR = 18.9, P < 0.01 and OR = 17.3, P < 0.05). Similarly, among nurses, being a JN was also an independent risk factor for NSIs regardless of whether adjustments were made for variables (both OR = 3.9, P < 0.01).
Consequently, RDs and JNs were added to the logistic regression model in Table 3 for further exploring the relationships of BW and overtime work with NSI in professional experience. HBW was a protective factor against NSI occurred regardless of whether adjustments were made for variables (M0, M1, and M2). However, after adjustment for HBW and RD effects, the effect of heavy overtime work was no longer significant (M2, OR = 1.9, P > 0.05). The proportion of NSIs among RDs was 4.1 times (M1, OR = 4.1, P < 0.05) higher than that among JNs without adjustment for variables; this increased to 19.5 times (M2, OR = 19.5, P < 0.05) after adjustment for sex, age, overtime work, and body weight. Therefore, UHBW was determined to be an independent risk factor for NSIs in RDs and JNs.
Table 4 presents the results of multiple logistic regressions after adjusting for age for NSI because experienced nurses have a wider age distribution. The results indicated that the proportion of NSIs among nurses with heavy overtime work was 6.6 times (OR = 6.6, P < 0.05) higher than that among nurses with mild overtime work, and the difference was significant. However, the proportion of NSIs in nurses with HBW was 1.2 times (M1, OR = 1.2, P > 0.05) that of nurses with UHBW, but the difference was not significant.
Table 5 illustrates the significant mediation effects (Zm = 2.5, P < 0.05) of heavy overtime work on the relationship between NSIs and doctors. No mediation effects were noted for the other five combinations.
A cross-sectional study evaluating NSI incidence among 29 doctors and 51 nurses demonstrated that the proportion of NSIs among nurses was 0.2 times that among doctors[6]. A study including NSI data from 2002 to 2007 in a university hospital in Pakistan demonstrated that the number of NSIs has higher in junior doctors than in nurses[7]. The differences between doctors and nurses may stem from differences in their work patterns or attitudes. For example, doctors often experience NSIs during wound irrigation, sutures, incisions, handling body fluids, and tissue sample collection. By contrast, for nurses, injuries often occur during injections, intravenous infusions, heparin cap sealing, intravenous connections, and venous or arterial blood collection[24]. In addition, some studies have determined that the NSI risk is affected by education and work experience[9,10,25] among nurses and by stress and carelessness[6] among doctors. Consistent with this finding, our study indicated that doctors experienced more NSIs than nurses did (7.7% vs 2.6%). In addition, nurses who intensively contact patients were the protective factor of NSIs (OR = 0.3, P < 0.05). Our analysis revealed that the proportion of NSIs 4.1 times (OR = 4.1, P < 0.05) higher among RDs than among JNs; this increased to 19.5 times after adjusting for age and overtime work. Therefore, the NSI risk among RDs may be more serious than expected and has often been ignored in the past.
A cross-sectional survey of staff physicians, RDs, staff dentists, nurses, and laboratory technicians illustrated that RDs were significantly associated with NSIs; NSIs were three times more common among RDs than among APs[19]. The present data indicate a difference of 17.3 times between RDs and APs (21.2% vs 1.4%), which was markedly higher than in past studies. This may be because the numbers of NSIs among APs were low (n = 1), which may have led to the overestimation of this result. Nevertheless, the risk of NSIs among RDs was higher than that among other types of medical personnel; for example this risk was 19.5 times higher in RDs than that in JNs.
Nurses with less work experience have a higher risk of NSIs[5,9]; in particular, nursing work experience of < 5 years was associated with significantly more NSIs than nursing work experience of > 5 years[5,11]. Consistent with these results, our study demonstrated that JNs have a higher risk of NSIs (OR = 3.9, P < 0.001) than experienced nurses after adjustment for other variables.
A cohort study including 11 728 employees revealed that claims costs were 7–11 times higher among those with BMI ≥ 40 compared with those within the recommended weight range[26]. A prospective cohort study of nearly 70 000 public sector employees demonstrated that, compared with employees whose BMI was in the healthy range, overweight or obese employees had an 11%–62% excess risk of occupational injury[16]. In addition, a study involving 7690 employees aged 18–65 years of an aluminum manufacturing company in the USA revealed that the proportion of injuries of participants with overweight or obesity was 1.3–2.2 times higher than those with normal weight[27]. The present results were in agreement with these findings and revealed that the proportion of NSIs among medical personnel with HBW was 0.5 times (OR = 0.5, P < 0.05) that among medical personnel with UHBW. Although we observed a relationship between NSIs and BW, the present study structure and data collected was insufficient to illustrate how BW affects NSIs. However, studies have demonstrated that fatigue increases the risk of NSIs among nurses and medical interns[28,29], and studies on grip strength have identified that, all things being equal, young people with obesity use more energy, have reduced endurance, and have accelerated power loss compared with nonobese young people. However, these obesity-related differences were not observed in the older age group[30]. These studies may explain the positive correlation between obesity and NSIs; obese people are more likely to use their poorer muscle strength improperly and be more prone to fatigue when performing clinical tasks, thus increasing their risk of NSIs.
A strong dose–response effect was noted between work hours and hazard rate[13], and working hours before injury will increase significantly compared to the past[31]. The positive trend between work hours and NSIs was observed in medical personnel: nurses with work hours of > 8 h/d[11] or > 40 h/wk[8] had higher risk of NSIs than those working < 8 h/d or < 40 h/wk. Our study found that the proportion of NSIs in participants with heavy overtime work was 4.3 times (OR = 4.3, P < 0.05) that in those with mild overtime work, but moderate overtime work effect (OR = 1.2, P > 0.05) was not significant; therefore, only heavy overtime work increased the risk of NSIs. Heavy overtime work was a risk factor for NSIs among doctors (OR = 5.4, P < 0.05) without adjustment for any variable, but this relationship was not significant when adjustments were made for sex, overtime work, professional grade, and BW; this was probably due to the higher proportion of heavy overtime work in RDs (33.3%) than in APs (8.5%). A dose–response effect was also noted between overtime work and NSIs for nurses, but it was not significant. However, experienced nurses engaged in heavy overtime work had 6.6 times (OR = 6.6, P < 0.05) more NSIs than those engaged in mild overtime work (Table 4); the effect of moderate overtime work on NSIs was not significant. Therefore, even among experienced nurses, only heavy overtime work affected the risk of NSIs. The proportion of NSIs was related to overtime work, but this relationship was not significant among nurses (Table 2); however, the association between NSIs and overtime work (OR = 6.6–7.0, P < 0.05) was significant among experienced nurses (Table 4). In addition, the mediation analysis (Table 5) demonstrated that heavy overtime work mediated (Zm= 2.5, P < 0.05) the relationship between NSIs and medical specialty, confirming the impact of heavy overtime work on NSI. However, heavy overtime work and HBW were not mediation factors for the relationship between NSIs and experience level for doctors or nurses, indicating that low experience among medical personnel might itself be the cause of NSIs. A study indicated that the incidence of NSIs among first-year RDs was higher than expected—more than 60% during the first 6 mo[32]—implying that education and training may influence the risk of NSIs. Burnout also increases the risk of occupational accidents and its sequelae[33], and it was also a factor influencing NSIs among nurses[34]. Burnout decreases with an increase in professional experience[35]; this may also explain by burnout why RDs experience higher NSIs incidence than Aps. Future studies should comprehensively assess the burnout level of participants.
Because this study only collected data from one hospital, its findings are limited by the data collection method, sample size, as well as the hospital’s environmental facilities, education, and training systems. In addition, because the number of reported NSIs was low, slight variations in the sample could have considerable influence on the conclusions. Moreover, factors such as hospital employees’ work patterns, workload, burnout level, work stress, and willingness to report occupational injuries were not considered in this study. These factors should be incorporated in the questionnaire design of future studies to further control for and discuss these effects on NSI risk. Although our results regarding NSI risk were consistent with those of past studies, this study compared the NSI risk between doctors and nurses, which has been rarely discussed in the literature. The findings can guide NSI prevention strategies in the medical practice.
This study revealed that heavy overtime work and low professional experience were associated with an increased NSI risk, particularly among RDs. Moreover, the present data indicated that HBW may reduce the risk of NSIs, which has rarely been evaluated in other studies. Maintaining an HBW had a protective effect against NSI for RDs and JNs. Therefore, in addition to promoting the use of safety needles and strengthening education and training related to infection control, the overtime schedule of medical personnel should be regularly reviewed; long work hours and excessive overtime should be avoided. Furthermore, strategies aimed at promoting the maintenance of HBW among employees should be implemented, which could further reduce NSI incidence.
Needle stick and sharp injuries (NSIs) may cause infections among medical personnel. Obesity and overtime work among medical personnel increase the incidence of work injuries.
The associations of overtime work and obesity with NSIs are unclear.
The study aimed to investigate whether overtime work and obesity increase the risk of NSIs.
This cross-sectional study used the data of 847 hospital personnel, including 104 doctors, 613 nurses, 67 medical laboratory scientists, 54 specialist technicians, and nine surgical assistants. Of them, 29 participants notified the hospital of having at least one NSI in 2017. The χ2 and Fisher’s exact tests were used to compare categorical variables. Multiple logistic regression analysis and the Sobel test were used to assess the risk of NSIs.
Overtime work, body weight (BW), and medical specialty were significantly associated with NSIs. After adjustment for risk factors, heavy overtime work was an independent risk factor for NSIs, and healthy BW (HBW) and nursing specialty were independent protective factors against NSIs. Also, after adjustment for risk factors, medical personnel with HBW had half as many NSIs as those with unhealthy BW (UHBW); the proportion of NSIs in doctors with HBW was 0.2 times that in doctors with UHBW; the proportion of injuries among residents was 17.3 times higher than that among attending physicians; the proportion of injuries among junior nurses was 3.9 times higher than that among experienced nurses; the proportion of injuries among nurses with heavy overtime work was 6.6 times higher than that among nurses with mild overtime work; and the proportion of injuries among residents was 19.5 times higher than that among junior nurses. Heavy overtime work mediated the association of medical specialty with NSIs.
Heavy overtime work and low professional experience were associated with an increased NSI risk, particularly among resident doctors. Maintaining HBW had a protective effect against NSI for resident doctors and junior nurses.
In addition to promoting the use of safety needles and providing infection control education, managers should review overtime schedules, and medical personnel should be encouraged to maintain an HBW.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Public, environmental and occupational health
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Morozov S S-Editor: Zhang H L-Editor: Kerr C P-Editor: Wang LYT
| 1. | Kermode M, Jolley D, Langkham B, Thomas MS, Crofts N. Occupational exposure to blood and risk of bloodborne virus infection among health care workers in rural north Indian health care settings. Am J Infect Control. 2005;33:34-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 77] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Norsayani MY, Noor Hassim I. Study on incidence of needle stick injury and factors associated with this problem among medical students. J Occup Health. 2003;45:172-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Prüss-Ustün A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005;48:482-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 415] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 4. | Yoshikawa T, Wada K, Lee JJ, Mitsuda T, Kidouchi K, Kurosu H, Morisawa Y, Aminaka M, Okubo T, Kimura S, Moriya K. Incidence rate of needlestick and sharps injuries in 67 Japanese hospitals: a national surveillance study. PLoS One. 2013;8:e77524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Clarke SP, Rockett JL, Sloane DM, Aiken LH. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near-misses in hospital nurses. Am J Infect Control. 2002;30:207-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 180] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 6. | Zafar A, Aslam N, Nasir N, Meraj R, Mehraj V. Knowledge, attitudes and practices of health care workers regarding needle stick injuries at a tertiary care hospital in Pakistan. J Pak Med Assoc. 2008;58:57-60. [PubMed] |
| 7. | Zafar A, Habib F, Hadwani R, Ejaz M, Khowaja K, Khowaja R, Irfan S. Impact of infection control activities on the rate of needle stick injuries at a tertiary care hospital of Pakistan over a period of six years: an observational study. BMC Infect Dis. 2009;9:78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Nsubuga FM, Jaakkola MS. Needle stick injuries among nurses in sub-Saharan Africa. Trop Med Int Health. 2005;10:773-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 91] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Cho E, Lee H, Choi M, Park SH, Yoo IY, Aiken LH. Factors associated with needlestick and sharp injuries among hospital nurses: a cross-sectional questionnaire survey. Int J Nurs Stud. 2013;50:1025-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 10. | Smith DR, Choe MA, Jeong JS, Jeon MY, Chae YR, An GJ. Epidemiology of needlestick and sharps injuries among professional Korean nurses. J Prof Nurs. 2006;22:359-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Ilhan MN, Durukan E, Aras E, Türkçüoğlu S, Aygün R. Long working hours increase the risk of sharp and needlestick injury in nurses: the need for new policy implication. J Adv Nurs. 2006;56:563-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Lo WY, Chiou ST, Huang N, Chien LY. Long work hours and chronic insomnia are associated with needlestick and sharps injuries among hospital nurses in Taiwan: A national survey. Int J Nurs Stud. 2016;64:130-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Dembe AE, Erickson JB, Delbos RG, Banks SM. The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occup Environ Med. 2005;62:588-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 336] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 14. | Fang Mao C, Hsu Y-Y, Mao C-C, Lu S-Y, Chen M-L. A field study of overtime work and shift work for hospital employees in Taiwan. J Occup Saf Health. 2011;19:233-246. |
| 15. | Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378:815-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1835] [Cited by in RCA: 1789] [Article Influence: 127.8] [Reference Citation Analysis (0)] |
| 16. | Kouvonen A, Kivimäki M, Oksanen T, Pentti J, De Vogli R, Virtanen M, Vahtera J. Obesity and occupational injury: a prospective cohort study of 69,515 public sector employees. PLoS One. 2013;8:e77178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Janssen I, Bacon E, Pickett W. Obesity and its relationship with occupational injury in the canadian workforce. J Obes. 2011;2011:531403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Dilie A, Amare D, Gualu T. Occupational Exposure to Needle Stick and Sharp Injuries and Associated Factors among Health Care Workers in Awi Zone, Amhara Regional State, Northwest Ethiopia, 2016. J Environ Public Health. 2017;2017:2438713. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Moro PL, Moore A, Balcacer P, Montero A, Diaz D, Gómez V, Garib Z, Weniger BG. Epidemiology of needlesticks and other sharps injuries and injection safety practices in the Dominican Republic. Am J Infect Control. 2007;35:552-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1966] [Cited by in RCA: 3077] [Article Influence: 78.9] [Reference Citation Analysis (0)] |
| 21. | Sobel ME. Asymptotic Confidence Intervals for Indirect Effects in Structural Equation Models. In: Leinhart S. Sociological Methodology. San Francisco: Jossey-Bass, 1982: 290-312. |
| 22. | Stone CA, Sobel ME. The robustness of estimates of total indirect effects in covariance structure models estimated by maximum. Psychometrika. 1990;55:337-352. |
| 23. | Lacobucci D. Mediation analysis and categorical variables: The final frontier. J Consum Psych. 2012;22:582-594. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Gu Y, Chen C, Cheng KP, Tu ZB, Zhang XJ. Analysis of needlestick and sharps injuries among medical staff in upper first-class hospital. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2013;31:41-44. [DOI] [Full Text] |
| 25. | Habib H, Khan EA, Aziz A. Prevalence and Factors Associated with Needle Stick Injuries among Registered urses in Public Sector Tertiary Care Hospitals of Pakistan. Int J Collabor Res Inter Med & Public Health. 2011;3:124-130. |
| 26. | Ostbye T, Dement JM, Krause KM. Obesity and workers' compensation: results from the Duke Health and Safety Surveillance System. Arch Intern Med. 2007;167:766-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 156] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 27. | Pollack KM, Sorock GS, Slade MD, Cantley L, Sircar K, Taiwo O, Cullen MR. Association between body mass index and acute traumatic workplace injury in hourly manufacturing employees. Am J Epidemiol. 2007;166:204-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 28. | Smith DR, Mihashi M, Adachi Y, Nakashima Y, Ishitake T. Epidemiology of needlestick and sharps injuries among nurses in a Japanese teaching hospital. J Hosp Infect. 2006;64:44-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 69] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 29. | Fisman DN, Harris AD, Rubin M, Sorock GS, Mittleman MA. Fatigue increases the risk of injury from sharp devices in medical trainees: results from a case-crossover study. Infect Control Hosp Epidemiol. 2007;28:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 30. | Mehta RK, Cavuoto LA. The effects of obesity, age, and relative workload levels on handgrip endurance. Appl Ergon. 2015;46 Pt A:91-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Vegso S, Cantley L, Slade M, Taiwo O, Sircar K, Rabinowitz P, Fiellin M, Russi MB, Cullen MR. Extended work hours and risk of acute occupational injury: A case-crossover study of workers in manufacturing. Am J Ind Med. 2007;50:597-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Marnejon T, Gemmel D, Mulhern K. Patterns of Needlestick and Sharps Injuries Among Training Residents. JAMA Intern Med. 2016;176:251-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 33. | Kotti N, Hajjaji M, Kchaou A, Sellami I, Masmoudi ML, Masmoudi J, Hammami Jmal K. Burnout and occupational accident. European Psychiatry. 2017;41:S324-S325. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 34. | Wang S, Yao L, Li S, Liu Y, Wang H, Sun Y. Sharps injuries and job burnout: a cross-sectional study among nurses in China. Nurs Health Sci. 2012;14:332-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 35. | Bogiatzaki V, Frengidou E, Savakis E, Trigoni M, Galanis P, Anagnostopoulos F. Empathy and Burnout of Healthcare Professionals in Public Hospitals of Greece. Int J Caring Sci. 2019;12:611-626. |








