Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.10927
Peer-review started: January 16, 2021
First decision: May 4, 2021
Revised: May 19, 2021
Accepted: October 27, 2021
Article in press: October 27, 2021
Published online: December 16, 2021
Processing time: 327 Days and 20.4 Hours
Abdominal pain in chronic pancreatitis (CP) may require invasive interventions. Surgical procedures are rare, and little is known about the long-term results.
To study the nationwide frequency of pancreatic surgery for CP in Finland, and postoperative symptoms and quality of life (QoL).
All patients in Finland with a diagnosis of CP who had undergone pancreatic surgery during 2000-2008 were selected from a national register. Only patients with CP as an indication for pancreatic surgery were included. Medical records were studied and questionnaires QLQ-C30, PAN26 and AUDIT, and symptom questionnaires were sent out.
During the 9-year period, pancreatic surgery for CP was performed on 30 patients [77% men, median age 45 (21-62) years]. Eighty-three percent underwent endoscopic procedures before surgery. Surgery was performed a median 2 (0-10) years after the original CP diagnosis, and 17% developed postoperative complications. Primary pain relief after surgery was reported in 70% of cases. Need for strong pain medication was lower after surgery. Eight of 21 (38%) returned the questionnaires and 88% reported that surgery had reduced their pain and 63% were almost or entirely pain-free at a median 14 (10-18) years after surgery. QoL results did not differ from those in our control Finnish CP group.
Surgery for CP is rare in Finland and most patients had prior endoscopic procedures. Patients who returned the questionnaires reported less pain and good QoL during the 14-year follow-up.
Core Tip: Our study provides valuable insight on the current state of chronic pancreatitis (CP) surgery for chronic pain in Finland. We included all the CP patients who underwent surgery for CP symptoms during 2000-2008 in Finland. We found that surgery is rare. We estimate that 0.6%-0.8% of CP patients undergo surgery for CP pain, which produces good long-term effects. Opiate usage was reduced after surgery. Most of the patients had undergone endoscopic procedures before surgery. Complications after CP surgery were rare.
- Citation: Parhiala M, Sand J, Laukkarinen J. Surgery for chronic pancreatitis in Finland is rare but seems to produce good long-term results. World J Clin Cases 2021; 9(35): 10927-10936
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/10927.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.10927
Chronic pancreatitis (CP) leads to permanent morphological changes in the pancreatic tissue such as ductal lesions and calcifications. Persistent inflammation may cause abdominal pain and also lead to pancreatic insufficiency, seen as secondary diabetes and malnutrition as well as various complications[1-4].
There are several mechanisms behind CP pain. High pressure in the pancreatic ducts due to pseudocysts or strictures may cause pain. High alcohol consumption and smoking may lead to oxidative stress, increasing pain. Exocrine insufficiency may result in low vitamin and antioxidant levels, causing pain. Even pancreatic ischemia may be behind the development and pain of CP[5-9].
Conservative pain treatment is often not enough and invasive treatments such as endoscopic stenting and surgery are needed. Endoscopic treatments, such as pancreatic stenting and celiac plexus interventions, are less invasive than surgery, but the long-term results may be of limited benefit[10-13].
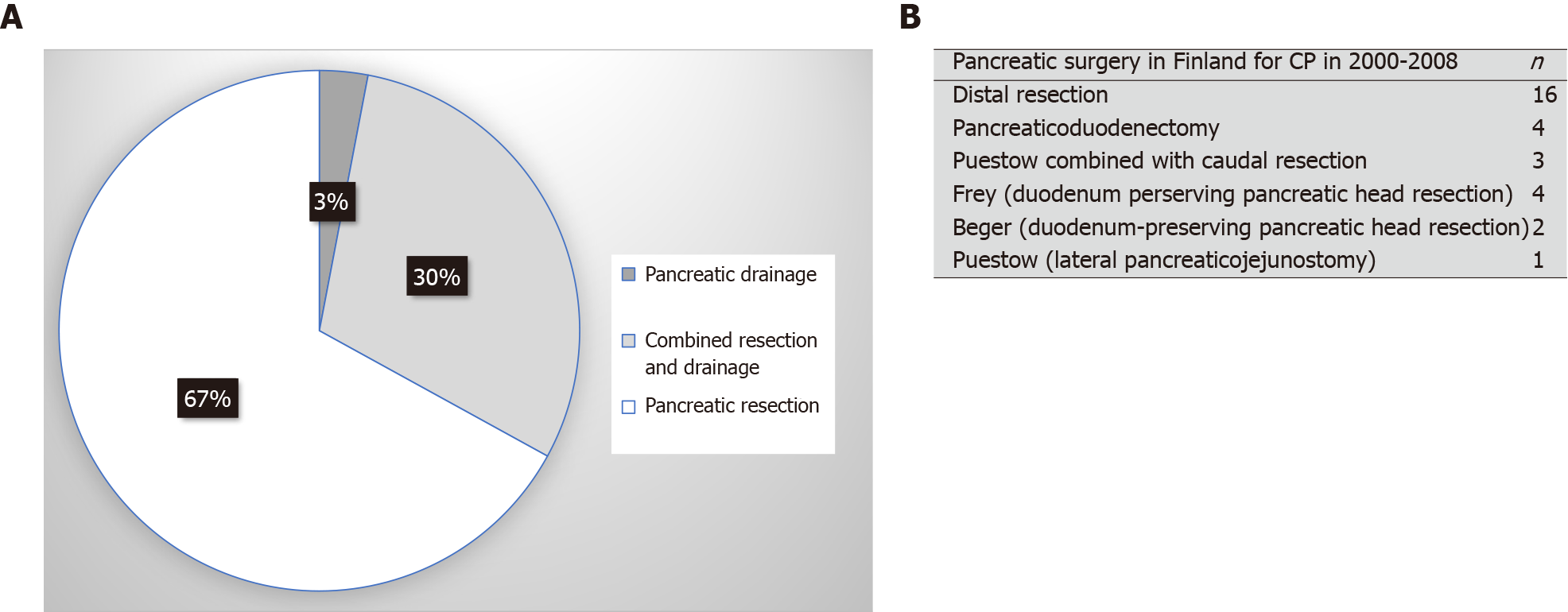
Surgery for CP is planned individually depending on the pancreatic findings. Surgical methods can be classified as pancreatic drainage, pancreatic resection or a combination of these. The earliest surgery for CP was pancreaticoduodenectomy (PD)[14-17]. Duodenum-preserving surgery for CP includes the Frey, Puestow, Berger and Berne modifications, where pancreatic tissue is resected and/or drained and a pancreatojejunostomy is performed using a Roux-Y jejunal loop[18-23].
Surgery for CP is rare and no universal recommendations exist. Some evidence suggests that earlier surgery for CP may improve results. To the best of our knowledge, there are no nationwide data in Finland on the frequency of the various surgical procedures, or on the effect on pain and quality of life (QoL) during long-term follow-up after surgery.
The aim of this study was to investigate the variety of surgical procedures used and their impact during a long-term follow-up on symptoms and QoL in patients operated on for CP nationwide in Finland in 2000-2008.
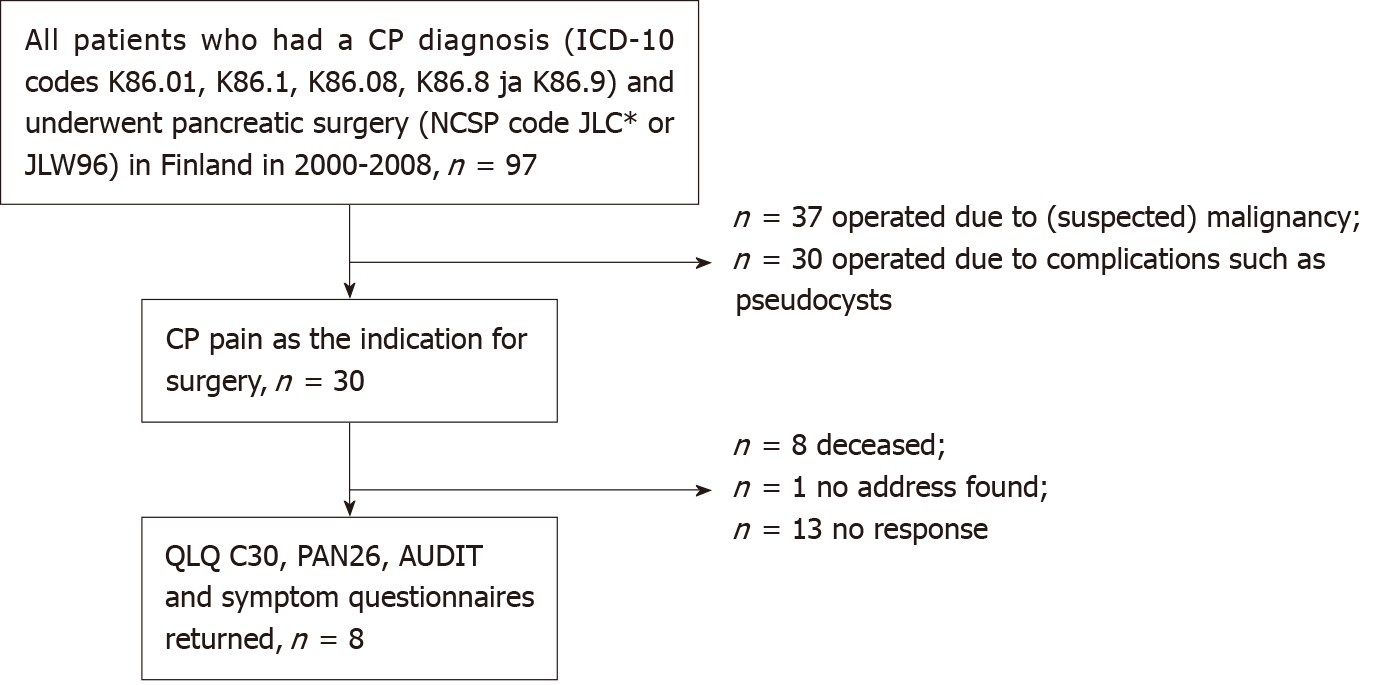
All the pancreatic resections [Nordic Classification of Surgical Procedures codes JLC* (resection of the pancreas) or JLW96 (other operations on pancreas)] performed in Finland during 2000-2008 for a diagnosis of CP (ICD-10 code: K86.01, K86.1, K86.08, k86.8 and K86.9) were selected from the Finnish National Institute for Health and Welfare HILMO register. There were 97 patients. After reviewing their medical records, only 30 patients with CP as an indication for pancreatic surgery were included in the final database (Figure 1).
From the patient archives, information was gathered about medical history, time of CP diagnosis, etiology of CP, previous CP treatments, type of current surgical therapy, postoperative complications, possible reoperations, and exocrine and endocrine pancreatic insufficiency. The date of death was recorded on September 22, 2017.
QLQ-C30, PAN-26[24] and AUDIT questionnaires and a nonstandardized questionnaire about pain before and after surgery were sent to the patients.
A previously reported Finnish general CP cohort from 2014-2015 was used as a control for the AUDIT, QLQ-C30 and PAN26 questionnaires[25]. In the control cohort, the median age was 58 (26-95) years, 67% were male and median time after diagnosis was 4 (1-42) years. Around 68% and 58% of patients had alcohol and smoking, respectively, as a risk factor for CP. Calcifications were found in 66% of the patients and ductal lesions were present in half of the patients. Endoscopic procedures were performed on 27% of patients and 9% underwent surgery.
The study was approved by the Ethics Committee of Tampere University Hospital, Finland (ETL code R16153). The data from the HILMO register was provided by the Finnish National Institute for Health and Welfare with a license/permission (THL/1854/5.05.00/2012)
Data are presented as median (range). The statistical analyses were performed using Pearson’s χ2 or Fisher’s exact test. For analysis of the QLQ-C30 and PAN26 questionnaires, the Mann-Whitney U test was used. The EORTEC scoring manual was used for the QLQ-C30 and PAN26 questionnaires, and the responses were scored as 0-100. A higher score on QoL/functioning indicated better QoL and a lower score on symptoms (e.g., pain or insomnia) represented better QoL. P < 0.05 was considered statistically significant.
Thirty patients underwent pancreatic surgery for CP in Finland during the period 2000-2008 and formed the final study cohort.
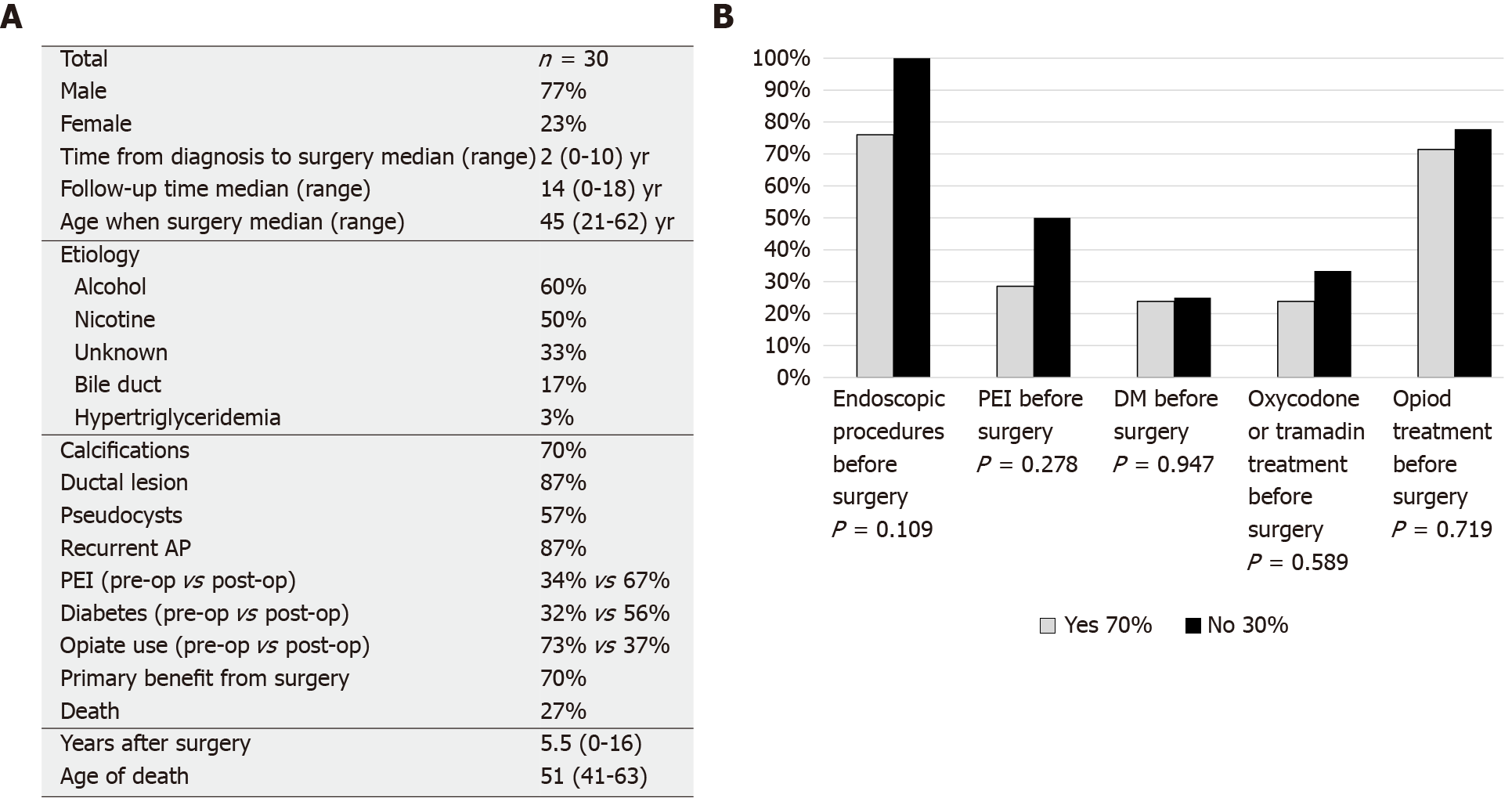
Surgery was performed in 13 different hospitals; median two (range 1-7) per hospital. Of the patients 77% were men and the median age was 45 (21-62) years. Surgery was performed a median 2 (0-10) years after diagnosis of CP. During the 16 (10-26) years of follow-up, eight patients died, a median 4.5 (0-16) years after surgery. The etiology of CP was alcohol in 60%, while 47% had idiopathic disease. Eighty-seven percent had recurrent episodes of acute pancreatitis (AP).
Half of the patients smoked. All of the smoking patients were on opioids before surgery, compared to 42% in the non-smoking group (P = 0.0004).
Out of the 30 operations performed in the course of 9 years, one was a drainage procedure (Puestow), nine combined resection and drainage, and there were 20 pancreatic resections (16 distal and 4 pylorus-preserving PD/PDs). Fifteen included splenectomies (Figure 2). Out of the combined pancreatic resection and drainages, four were Frey´s procedure, two were Beger´s procedure and three were Puestow´s drainage combined with caudal resection (Figure 3).
Eighty-three percent (n = 25) of the patients had no postoperative complications, 17% (n = 5) developed complications: two had Clavien-Dindo (CD) grade 1 complications; two had CD grade 2 complications and one had CD grade 3b complications. One patient died within 3 wk of surgery; this patient had undergone four prior laparotomies and had intraoperative hemorrhage during surgery for CP.
Seventy percent of the patients had reported primary pain relief after the surgery and 64% of those who had undergone previous endoscopic procedures had experienced primary pain relief and all those with no previous endoscopic procedures had experienced primary pain relief, but the nonendoscopic group was so small that the difference was not significant (P = 0.10). No correlation was seen in time after diagnosis and primary pain relief (P = 0.43) (Figure 2).
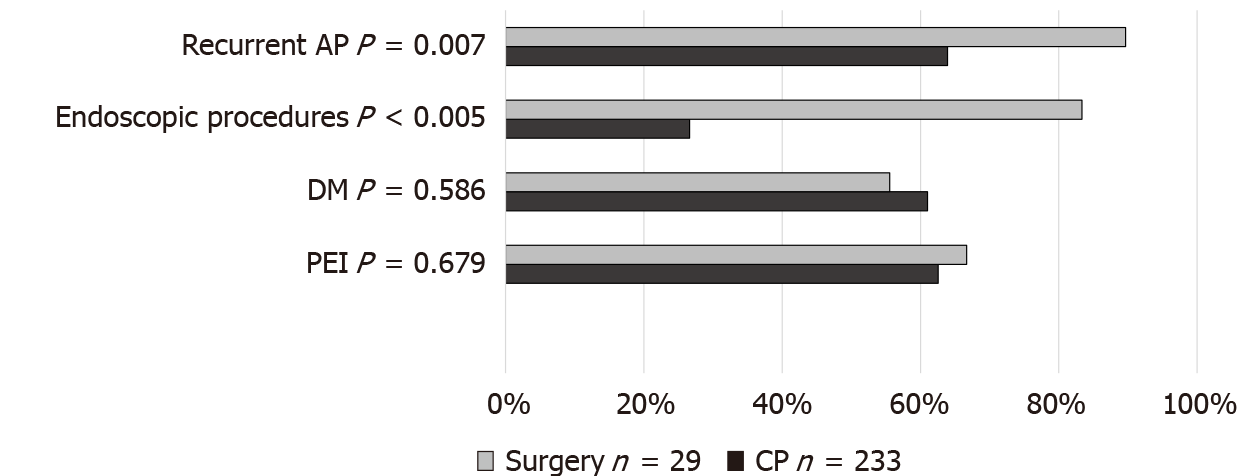
Pancreatic exocrine insufficiency (PEI) was present in 34% of the patients preoperatively and in 67% postoperatively. Diabetes was seen in 32% of the patients preoperatively and in 56% postoperatively. When comparing CP patients who had surgery (n = 25) to the Finnish general CP cohort who did not have pancreatic surgery (n = 195) and had a median time after diagnosis of 5-43 years, the frequency of PEI was similar (surgery group 67% vs nonsurgical group 63%, P = 0.679). Also, the frequency of diabetes was the same in CP patients not undergoing pancreatic surgery (61%) as in patients undergoing surgery (56%; P = 0.586). Seventy-three percent of the patients were on opioids before surgery and 37% after surgery (P = 0.004). Opioid use for the control group was not recorded (Figure 4).
Endoscopic retrograde cholangiopancreatography was performed on 83% of the patients prior to surgery. Twenty percent had already undergone prior pancreatic surgery for pancreatic pseudocyst complications. When comparing these parameters to the Finnish general CP cohort, significantly more endoscopic procedures (83% vs 27%, P < 0.0001) and recurrent AP (87% vs 67%, P = 0.007) were seen in these surgically treated CP patients than in the overall CP patients in the control group (Figure 4).
Out of the 21 patients asked to complete the questionnaires, eight (38%) returned the QoL questionnaires (QLQ-C30 and Pan-26) and the AUDIT questionnaire. There was no significant difference between the responders and nonresponders in gender, pancreatic calcifications, PEI, recurrent AP or alcohol-related etiology. All the patients who responded had a history of smoking and 63% continued smoking compared to 35% among the nonrespondent patients (P = 0.003).
Of the CP patients who responded, 88% reported that the surgery helped their pain and 63% were almost or entirely pain-free 14 (10-18) years after surgery. The AUDIT questionnaire median was 4 (0-28) points, and in the control CP population, the AUDIT score median was 3 (0-39) points (P = 0.764).
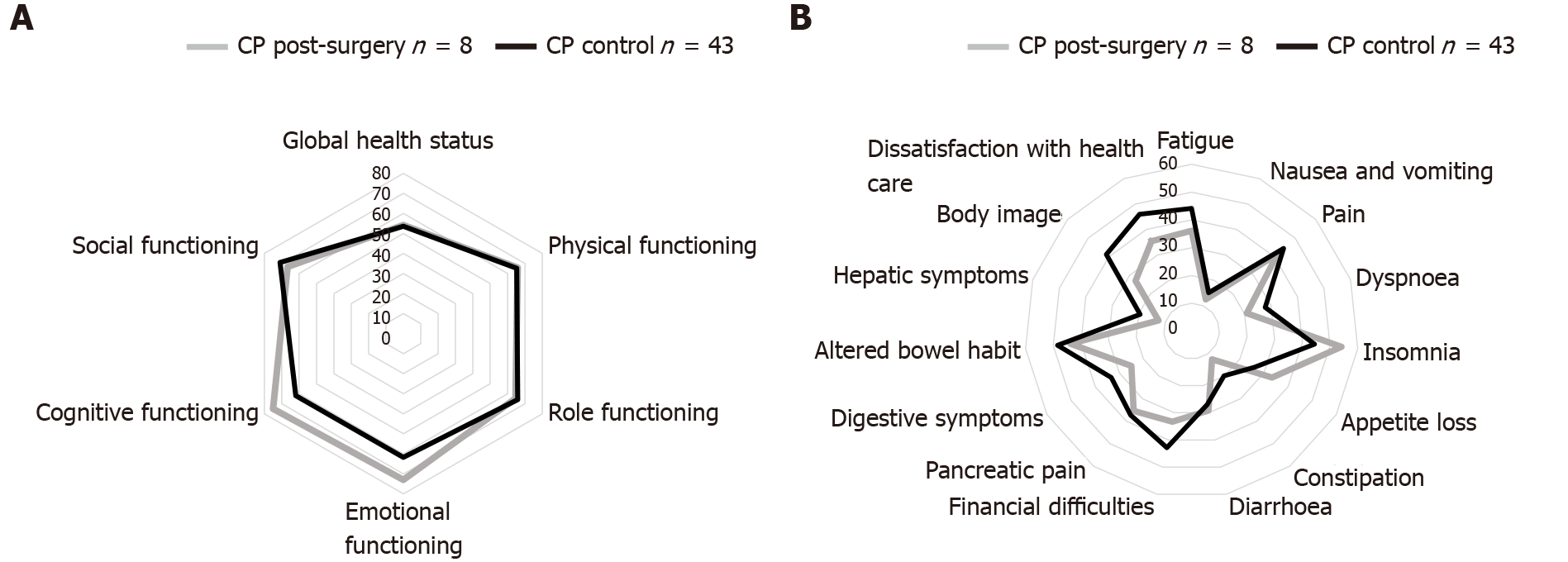
When comparing the QLQ-C30 and PAN26 responses to the Finnish general CP cohort (Figure 5) the nonsurgery group had more pain, pancreatic pain and hepatic symptoms but this was not significant (P = 0.869, P = 0.970 and P = 0.379). Since all the responding CP patients undergoing surgery were smokers, we compared them to those in the Finnish general CP cohort who had been smoking.
Surgery for CP is rare and no nationwide data with long-term follow-up after surgery are available. Our aim was to find out how common CP surgery is and what the long-term effects on CP patients are. We found that surgery for CP is rare but seems to give long-term pain relief in CP and reduces opiate use.
Approximately three operations for CP pain were performed per year in the whole of Finland. We estimate that 0.6%-0.8% of CP patients undergo surgery for CP pain. Most of the surgical interventions in CP are for treatment of complications (such as pseudocyst infections, hemorrhage and bowel obstruction), or due to suspicion of malignancy. Overall, pancreatic surgery for CP is rare in Northern Europe: < 10%, compared to studies from North America and Hungary, reporting 20% pancreatic surgery in the CP population[26-28]. Most patients had already undergone endoscopic procedures; some of them multiple times. In our study, patients with no previous endoscopic procedures had better pain relief (64% vs 100%) even though the difference was not significant due to the number patients with no previous endoscopies. It seems that in Finland surgical procedures are only considered after endoscopic means have been already tried. Thirty-four percent already had preoperative PEI, indicating advanced CP. Retrospective studies have shown that pancreatic surgery for pancreatic duct decompression is more cost-effective than endoscopy[29,30].
During the time of the study, CP pancreatic surgery was spread over many hospitals in Finland, 13 in total — compared to five centers at present. Most of the patients underwent endoscopic procedures before the operation. The procedures performed were also heterogeneous. In our study there was no correlation in the timing of the surgery and primary pain relief but most of the operations were performed within 3 years of diagnosis (74%). A few retrospective studies have reported that earlier CP surgery (< 3 years after diagnosis) improves the outcome and is also safe. In a prospective, multicenter randomized controlled trial (ESCAPE trial), surgery was reported to produce better outcomes when performed early enough before endoscopic procedures. In CP, the pancreas tends to be harder due to fibrosis, which can lead to fewer postoperative pancreatic fistulas than in a soft normal pancreas. Compared to reports in Europe and North America, the low percentage of CP surgery in Finland suggests that CP patients are operated on too seldom in Finland, which could be due to advances in endoscopic procedures or to a high threshold for performing pancreatic surgery on a benign disease[31-35].
Most of the patients in our study used opioids before surgery, and surgery reduced the need for opioids. Perhaps when opioids are needed surgery should be considered. Thirty-six percent of the patients had opioids after surgery and this could be due to opioid tolerance and addiction. Preoperative opioid use, persistent pain (3 mo) and previous surgery have been shown to be risk factors for postoperative pain in abdominal surgery. Chronic use of opioids in abdominal pain such as in CP can cause hyperalgesia in which abdominal pain paradoxically may become more severe[36-39].
Half of the CP patients undergoing surgery were smokers and they took significantly more opioids before surgery. Smoking has been reported to impair the outcome of pancreatic surgery and QoL[40]. Cessation of smoking and opioid use should be considered before pancreatic surgery for CP.
There was no significant difference in PEI, diabetes or QLQ responses between CP patients undergoing surgery and a Finnish control CP group, even though it seems that the CP patients who underwent pancreatic surgery were a selected patient group with more severe pancreatitis, since they had significantly more endoscopic procedures (83% vs 27%, P < 0.0001) and recurrent AP (87% vs 67%, P = 0.023) than the control CP group. Nonoperated and operated CP patients had approximately the same amount of PEI. Surprisingly, diabetes is more common in CP patients without pancreatic surgery. This could be due the decompressing surgery influencing the progression of pancreatitis and slowing pancreatic insufficiency[41,42].
The rate of idiopathic pancreatitis is high in patients who have surgery. In some cases, it could be due to the difficulty in differencing benign pancreatic masses and malignant tumors, which could affect the decision for surgery[43-45].
The strength of our study is that it involved all the CP patients in Finland. We made a broad selection and only included patients with CP diagnosis and surgery performed for CP pain. To the best of our knowledge, no national study on CP surgery had been published earlier. In spite of the small population, our study provides a valuable description of CP patients who undergo surgery for CP.
The limitations of this study were the small patient number and low response rate of 38%, which is approximately the same as in an earlier study[25]. We gathered the medical histories retrospectively, and one was lost because the patient was deceased, and the record had been deleted. Smoking and alcohol consumption were not always recorded accurately, so presumably these may have been more common.
Surgery for CP is rare in Finland, but seems to produce good long-term results. Opiate usage was reduced after surgery. Most of the patients had undergone endoscopic procedures before surgery. Complications after CP surgery were rare. More studies are needed on the timing of CP surgery to ensure maximum benefit for patients.
Chronic pancreatitis (CP) may need invasive surgical interventions. There is no current knowledge of long-term outcomes and prevalence of surgery for CP.
We wanted to investigate the current state of pancreatic surgery in Finland for CP.
Our objective was to find long-term outcomes of patients who have pancreatic surgery for CP pain in Finland.
We gathered all CP patients who had pancreatic surgery in Finland in 2000-2008 via the Finnish National Institute for Health and Welfare registry. We gathered information about the time of CP diagnosis, etiology of CP, previous CP treatments, type of current surgical therapy, postoperative complications, possible reoperations, and exocrine and endocrine pancreatic insufficiency.
We found that surgery for CP is rare in Finland but most patients (70%) are pain free after surgery. Opiate usage was less after surgery.
CP surgery is rare and produces good long-term results in CP patients.
Our study was limited because of the small number of patients but we provide a long 16-year follow-up and our study contains all of CP patients in Finland who had pancreatic surgery.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Corresponding Author's Membership in Professional Societies: Finnish Society of Gastroenterology; Finnish Digestive Surgeons.
Specialty type: Medicine, research and experimental
Country/Territory of origin: Finland
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): E
P-Reviewer: İnal V, Li CP, Patel D, Uhlmann D, Xu ZL S-Editor: Gao CC L-Editor: Kerr C P-Editor: Gao CC
| 1. | Agarwal S, Sharma S, Gunjan D, Singh N, Kaushal K, Poudel S, Anand A, Gopi S, Mohta S, Sonika U, Saraya A. Natural course of chronic pancreatitis and predictors of its progression. Pancreatology. 2020;20:347-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Lévy P, Domínguez-Muñoz E, Imrie C, Löhr M, Maisonneuve P. Epidemiology of chronic pancreatitis: burden of the disease and consequences. United European Gastroenterol J. 2014;2:345-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 135] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 3. | Singh VK, Yadav D, Garg PK. Diagnosis and Management of Chronic Pancreatitis: A Review. JAMA. 2019;322:2422-2434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 301] [Article Influence: 50.2] [Reference Citation Analysis (0)] |
| 4. | Barry K. Chronic Pancreatitis: Diagnosis and Treatment. Am Fam Physician. 2018;97:385-393. [PubMed] |
| 5. | Schneider A, Hirth M. Pain Management in Chronic Pancreatitis: Summary of Clinical Practice, Current Challenges and Potential Contribution of the M-ANNHEIM Classification. Drugs. 2021;81:533-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Mohta S, Singh N, Gunjan D, Kumar A, Saraya A. Systematic review and meta-analysis: Is there any role for antioxidant therapy for pain in chronic pancreatitis. JGH Open. 2021;5:329-336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Sureshkumar S, Omang A, Anandhi A, Rajesh BS, Abdulbasith KM, Vijayakumar C, Palanivel C, Pazhanivel M, Kate V. Efficacy of Pregabalin and Antioxidants Combination in Reducing Pain in Chronic Pancreatitis: A Double Blind Randomized Trial. Dig Dis Sci. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Valente R, Waldthaler A, Scandavini CM, Vujasinovic M, Del Chiaro M, Arnelo U, Löhr JM. Conservative Treatment of Chronic Pancreatitis: A Practical Approach. Scand J Surg. 2020;109:59-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Sand J, Nordback I. Kroonisen haimatulehduksen aiheuttama kipu: katsaus. Lääketieteellinen Aikakauskirja Duodecim. 2011;127:995-1001. |
| 10. | Hartwig W, Werner J, Ryschich E, Mayer H, Schmidt J, Gebhard MM, Herfarth C, Klar E. Cigarette smoke enhances ethanol-induced pancreatic injury. Pancreas. 2000;21:272-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Drewes AM, Kempeneers MA, Andersen DK, Arendt-Nielsen L, Besselink MG, Boermeester MA, Bouwense S, Bruno M, Freeman M, Gress TM, van Hooft JE, Morlion B, Olesen SS, van Santvoort H, Singh V, Windsor J. Controversies on the endoscopic and surgical management of pain in patients with chronic pancreatitis: pros and cons! Gut. 2019;68:1343-1351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 12. | Seicean A, Vultur S. Endoscopic therapy in chronic pancreatitis: current perspectives. Clin Exp Gastroenterol. 2015;8:1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Nabi Z, Lakhtakia S. Endoscopic management of chronic pancreatitis. Dig Endosc. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Mendieta PJO, Sagae VMT, Ribeiro IB, de Moura DTH, Scatimburgo MVCV, Hirsch BS, Rocha RSP, Visconti TAC, Sánchez-Luna SA, Bernardo WM, de Moura EGH. Pain relief in chronic pancreatitis: endoscopic or surgical treatment? Surg Endosc. 2021;35:4085-4094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 15. | Adler JM, Gardner TB. Endoscopic Therapies for Chronic Pancreatitis. Dig Dis Sci. 2017;62:1729-1737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Yin Z, Sun J, Yin D, Wang J. Surgical treatment strategies in chronic pancreatitis: a meta-analysis. Arch Surg. 2012;147:961-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Bachmann K, Tomkoetter L, Kutup A, Erbes J, Vashist Y, Mann O, Bockhorn M, Izbicki JR. Is the Whipple procedure harmful for long-term outcome in treatment of chronic pancreatitis? Ann Surg. 2013;258:815-20; discussion 820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 18. | Iqbal N, Lovegrove RE, Tilney HS, Abraham AT, Bhattacharya S, Tekkis PP, Kocher HM. A comparison of pancreaticoduodenectomy with pylorus preserving pancreaticoduodenectomy: a meta-analysis of 2822 patients. Eur J Surg Oncol. 2008;34:1237-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Tillou JD, Tatum JA, Jolissaint JS, Strand DS, Wang AY, Zaydfudim V, Adams RB, Brayman KL. Operative management of chronic pancreatitis: A review. Am J Surg. 2017;214:347-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Puestow CB, Gillesby WJ. Retrograde surgical drainage of pancreas for chronic relapsing pancreatitis. AMA Arch Surg. 1958;76:898-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 193] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Roch A, Teyssedou J, Mutter D, Marescaux J, Pessaux P. Chronic pancreatitis: A surgical disease? World J Gastrointest Surg. 2014;6:129-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Frey CF, Smith GJ. Description and rationale of a new operation for chronic pancreatitis. Pancreas. 1987;2:701-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 267] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 23. | Ni Q, Yun L, Roy M, Shang D. Advances in surgical treatment of chronic pancreatitis. World J Surg Oncol. 2015;13:34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Mihaljevic AL, Kleeff J, Friess H. Beger's operation and the Berne modification: origin and current results. J Hepatobiliary Pancreat Sci. 2010;17:735-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Fitzsimmons D, Kahl S, Butturini G, van Wyk M, Bornman P, Bassi C, Malfertheiner P, George SL, Johnson CD. Symptoms and quality of life in chronic pancreatitis assessed by structured interview and the EORTC QLQ-C30 and QLQ-PAN26. Am J Gastroenterol. 2005;100:918-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 133] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 26. | Parhiala M, Sand J, Laukkarinen J. A population-based study of chronic pancreatitis in Finland: Effects on quality of life. Pancreatology. 2020;20:338-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Olesen SS, Poulsen JL, Drewes AM, Frøkjær JB, Laukkarinen J, Parhiala M, Rix I, Novovic S, Lindkvist B, Bexander L, Dimcevski G, Engjom T, Erchinger F, Haldorsen IS, Pukitis A, Ozola-Zālīte I, Haas S, Vujasinovic M, Löhr JM, Gulbinas A, Jensen NM, Jørgensen MT, Nøjgaard C; Scandinavian Baltic Pancreatic Club (SBPC). The Scandinavian baltic pancreatic club (SBPC) database: design, rationale and characterisation of the study cohort. Scand J Gastroenterol. 2017;52:909-915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 28. | Machicado JD, Amann ST, Anderson MA, Abberbock J, Sherman S, Conwell DL, Cote GA, Singh VK, Lewis MD, Alkaade S, Sandhu BS, Guda NM, Muniraj T, Tang G, Baillie J, Brand RE, Gardner TB, Gelrud A, Forsmark CE, Banks PA, Slivka A, Wilcox CM, Whitcomb DC, Yadav D. Quality of Life in Chronic Pancreatitis is Determined by Constant Pain, Disability/Unemployment, Current Smoking, and Associated Co-Morbidities. Am J Gastroenterol. 2017;112:633-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 146] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 29. | Szücs Á, Marjai T, Szentesi A, Farkas N, Párniczky A, Nagy G, Kui B, Takács T, Czakó L, Szepes Z, Németh BC, Vincze Á, Pár G, Szabó I, Sarlós P, Illés A, Gódi S, Izbéki F, Gervain J, Halász A, Farkas G, Leindler L, Kelemen D, Papp R, Szmola R, Varga M, Hamvas J, Novák J, Bod B, Sahin-Tóth M, Hegyi P; Hungarian Pancreatic Study Group. Chronic pancreatitis: Multicentre prospective data collection and analysis by the Hungarian Pancreatic Study Group. PLoS One. 2017;12:e0171420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 30. | Łaski D, Hać S, Marek I, Kobiela J, Kostro J, Adrych K, Śledziński Z. Cost-effectiveness of benign Wirsung duct strictures treatment in chronic pancreatitis. Wideochir Inne Tech Maloinwazyjne. 2018;13:17-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 31. | Kawashima Y, Kawaguchi Y, Kawanishi A, Ogawa M, Hirabayashi K, Nakagohri T, Mine T. Comparison between Endoscopic Treatment and Surgical Drainage of the Pancreatic Duct in Chronic Pancreatitis. Tokai J Exp Clin Med. 2018;43:117-121. [PubMed] |
| 32. | Ke N, Jia D, Huang W, Nunes QM, Windsor JA, Liu X, Sutton R. Earlier surgery improves outcomes from painful chronic pancreatitis. Medicine (Baltimore). 2018;97:e0651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 33. | Willner A, Bogner A, Müssle B, Teske C, Hempel S, Kahlert C, Distler M, Weitz J, Welsch T. Disease duration before surgical resection for chronic pancreatitis impacts long-term outcome. Medicine (Baltimore). 2020;99:e22896. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 34. | Bordaçahar B, Couvelard A, Vullierme MP, Bucchini L, Sauvanet A, Dokmak S, Ruszniewski P, Lévy P, Rebours V. Predicting the efficacy of surgery for pain relief in patients with alcoholic chronic pancreatitis. Surgery. 2018;164:1064-1070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Issa Y, Kempeneers MA, Bruno MJ, Fockens P, Poley JW, Ahmed Ali U, Bollen TL, Busch OR, Dejong CH, van Duijvendijk P, van Dullemen HM, van Eijck CH, van Goor H, Hadithi M, Haveman JW, Keulemans Y, Nieuwenhuijs VB, Poen AC, Rauws EA, Tan AC, Thijs W, Timmer R, Witteman BJ, Besselink MG, van Hooft JE, van Santvoort HC, Dijkgraaf MG, Boermeester MA; Dutch Pancreatitis Study Group. Effect of Early Surgery vs Endoscopy-First Approach on Pain in Patients With Chronic Pancreatitis: The ESCAPE Randomized Clinical Trial. JAMA. 2020;323:237-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 162] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 36. | Lapshyn H, Petruch N, Thomaschewski M, Sondermann S, May K, Frohneberg L, Petrova E, Zemskov S, Honselmann KC, Braun R, Keck T, Wellner UF, Bolm L. A simple preoperative stratification tool predicting the risk of postoperative pancreatic fistula after pancreatoduodenectomy. Pancreatology. 2021;21:957-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 37. | opioid analgesics. Codeine, dihydrocodeine and tramadol: no less risky than morphine. Prescrire Int. 2016;25:45-50. [PubMed] |
| 38. | Keefer L, Drossman DA, Guthrie E, Simrén M, Tillisch K, Olden K, Whorwell PJ. Centrally Mediated Disorders of Gastrointestinal Pain. Gastroenterology. 2016;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 39. | Ewald N, Hardt PD. Diagnosis and treatment of diabetes mellitus in chronic pancreatitis. World J Gastroenterol. 2013;19:7276-7281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 132] [Cited by in RCA: 125] [Article Influence: 10.4] [Reference Citation Analysis (3)] |
| 40. | Strik C, van den Beukel B, van Rijckevorsel D, Stommel MWJ, Ten Broek RPG, van Goor H. Risk of Pain and Gastrointestinal Complaints at 6Months After Elective Abdominal Surgery. J Pain. 2019;20:38-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 41. | Maartense S, Ledeboer M, Bemelman WA, Ringers J, Frolich M, Masclee AA. Effect of surgery for chronic pancreatitis on pancreatic function: pancreatico-jejunostomy and duodenum-preserving resection of the head of the pancreas. Surgery. 2004;135:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 42. | Yang CJ, Bliss LA, Schapira EF, Freedman SD, Ng SC, Windsor JA, Tseng JF. Systematic review of early surgery for chronic pancreatitis: impact on pain, pancreatic function, and re-intervention. J Gastrointest Surg. 2014;18:1863-1869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 43. | Kleeff J, Stöß C, Mayerle J, Stecher L, Maak M, Simon P, Nitsche U, Friess H. Evidence-Based Surgical Treatments for Chronic Pancreatitis. Dtsch Arztebl Int. 2016;113:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 44. | Sun GF, Zuo CJ, Shao CW, Wang JH, Zhang J. Focal autoimmune pancreatitis: radiological characteristics help to distinguish from pancreatic cancer. World J Gastroenterol. 2013;19:3634-3641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 45. | Wang Y, Chen X, Wang J, Cui W, Wang C, Wang Z. Differentiation between non-hypervascular pancreatic neuroendocrine tumors and mass-forming pancreatitis using contrast-enhanced computed tomography. Acta Radiol. 2021;62:190-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |