Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.10909
Peer-review started: July 11, 2021
First decision: August 18, 2021
Revised: August 22, 2021
Accepted: October 27, 2021
Article in press: October 27, 2021
Published online: December 16, 2021
Processing time: 151 Days and 21.3 Hours
Thumb polydactyly is one of the most common congenital hand deformities, and the Bilhaut-Cloquet procedure or a modified one is often used. However, controversy remains over the rare instances in which both thumbs are not of similar length or far apart in distance.
To evaluate the clinical outcomes of pedicle complex tissue flap transfer in the treatment of duplicated thumbs with unequal size.
From January 2014 to December 2020, 15 patients underwent duplicated thumb reconstruction by pedicle complex tissue flap transfer at our hand surgery center. The technique was used when it was necessary to combine different tissues from both severed and preserved thumbs that were not of similar length or far apart in distance. Subjective parents’ evaluations and functional outcomes (ALURRA and TATA criteria) were obtained. The alignment deviation, instability, range of motion (percent of opposite thumb) of the interphalangeal and metacarpophalangeal joints, and the aesthetic aspects, including circumference, length, nail size, and nail deformity, were used to assess the clinical outcomes.
The average age of patients at the time of surgery was 13 mo, and the mean final follow-up occurred at 42 mo. An appropriate volume with a stable joint and good appearance was obtained in 14 reconstructed thumbs. An unstable inter
Harvesting a pedicle flap from a severed thumb is a safe and reliable procedure. Defects of the preserved thumb, such as the skin, nail, and bone, can be effectively restored using the complex tissue flap.
Core Tip: We found that an appropriate volume with a stable joint and good appearance was obtained in 14 reconstructed thumbs. An unstable interphalangeal joint occurred in one thumb. The mean ALURRA score was 21.8 (range: 20-24), and the Tada score was 6.9 (range: 5-8). Compared with the non-operated side, the length of the operated thumb was approximately 95%, the girth was 89%, and the nail width was 82.9%. The mean ranges of motion were 62.1% of that of the unaffected thumb in the interphalangeal joint and 78.3% in the metacarpophalangeal joint. Therefore, harvesting a pedicle flap from a severed thumb is a safe and reliable procedure. Defects of the preserved thumb, such as the skin, nail, and bone, can be effectively restored using the complex tissue flap.
- Citation: Wang DH, Zhang GP, Wang ZT, Wang M, Han QY, Liu FX. Pedicle complex tissue flap transfer for reconstruction of duplicated thumbs with unequal size. World J Clin Cases 2021; 9(35): 10909-10918
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/10909.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.10909
Thumb polydactyly is the most prevalent duplication in Caucasian and Asian populations, occurring in approximately 0.8 to 1.4 per 1000 births[1-4], impacting not only the appearance of the affected hand but also the function of thumb flexion and extension and grasping and pinching movements[5-7]. To better restore the function of the thumb, reconstruction surgery for thumb deformities should be performed early in the first year of life[8], which could help children to obtain a thumb similar to normal thumb anatomy with less growth impairment and to reconstruct thumb function during their growth and development.
The surgical strategy should be formulated according to the specific thumb deformity because thumb deformities are different for various children. There are many clinical diagnostic classifications of complex thumb deformity. At present, the Wassel classification is the most commonly used, which divides complex thumb deformity into seven types based on its type and grade of phalangeal division[9]. Currently, for a clear distinction between primary and redundant thumbs, a surgical strategy including resection of the redundant finger and reconstruction of the main thumb is generally adopted when the primary thumb is well developed. The Bilhaut-Cloquet procedure and its modified operation are often used to reconstruct symmetrical or essentially symmetrical thumb polydactyly with the same size as the supernumerary finger[7,10]. However, reconstruction of thumb polydactyly correction is often associated with several problems, such as a slender and short reserved thumb, unstable joints, nail lateral deviation deformity, and a narrow skin defect in the first web space, which is a challenge for clinicians.
Thumb polydactyly is one of the most common congenital hand deformities; surgery for most conditions usually involves removal of the more hypoplastic thumb and reconstruction of the better thumb. When neither thumb is obviously dominant in all aspects or when a combination of the two thumbs is a better choice, the Bilhaut-Cloquet procedure or a modified one can be used. There are rare instances in which both thumbs are not of similar length or far apart in distance, in which case the Bilhaut-Cloquet procedure or a modified procedure is difficult to implement. In such cases, a useful procedure is to transfer a complex tissue flap on a neurovascular pedicle raised from the severed thumb to overcome the defect in length or distance.
Therefore, the purpose of this article is to deliver our experience on this kind of reconstruction and to report the follow-up outcomes in our series of patients.
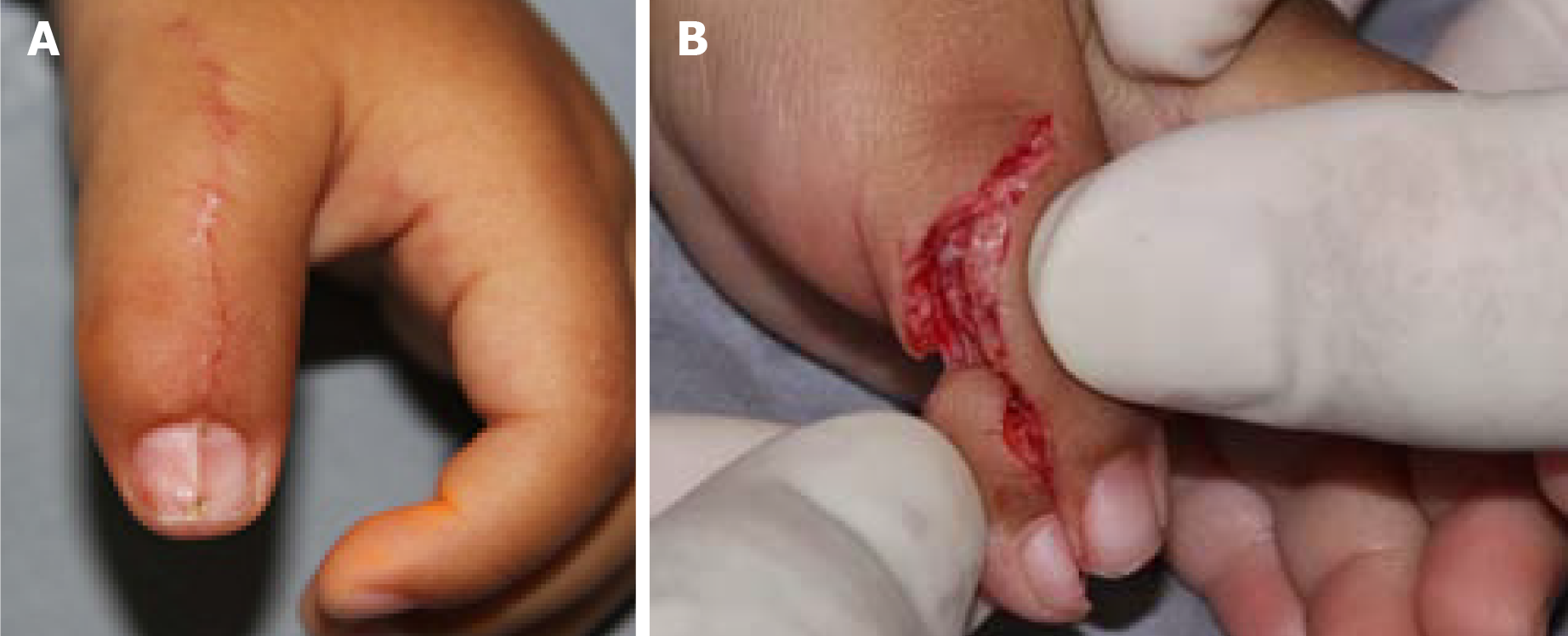
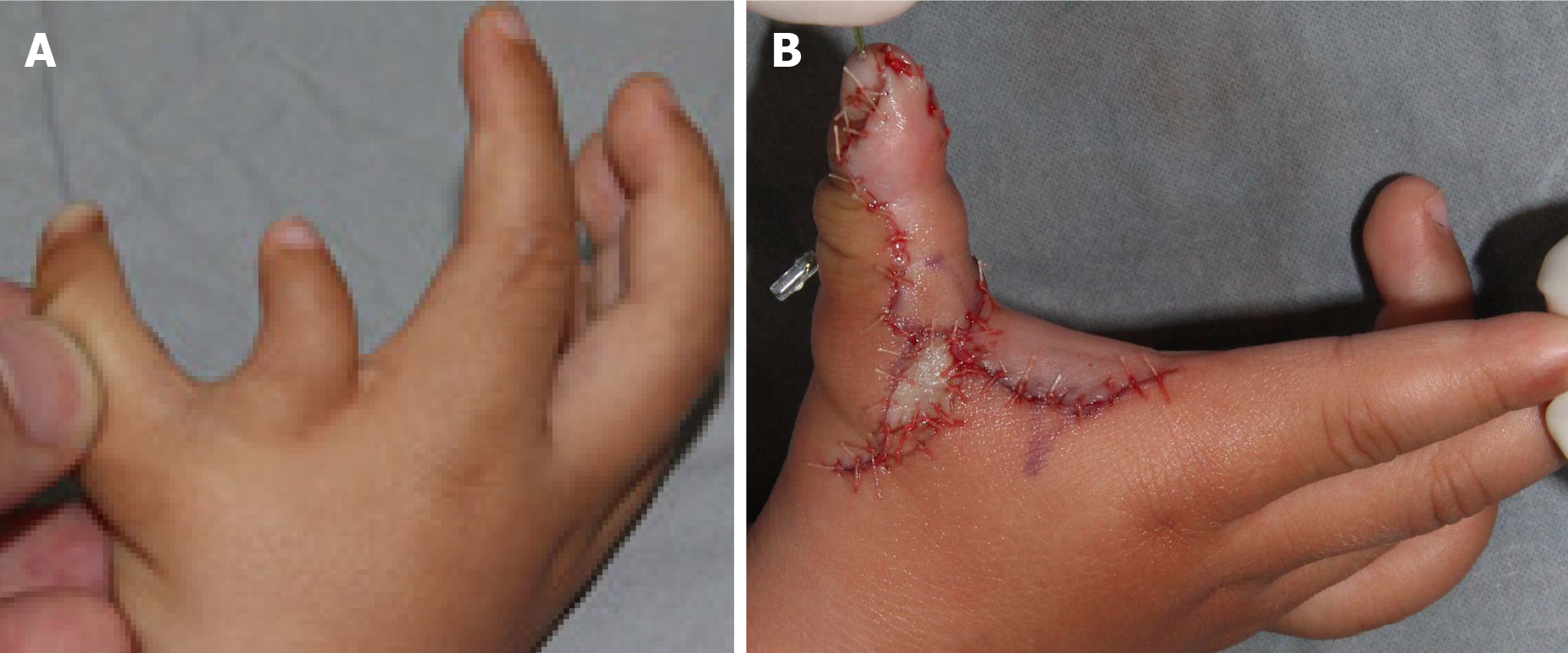
This retrospective study included patients who underwent duplicated thumb reconstruction by pedicle complex tissue flap transfer at the Shandong Provincial Hospital Affiliated to Shandong First Medical University from January 2014 to December 2020. The technique was used when it was necessary to combine different tissues from both severed and preserved thumbs that were not of similar length or far apart in distance. The patients had at least one of the following symptoms: There was a skin defect in the preserved thumb (Figure 1A); neither thumb was obviously dominant in all aspects, and there was a difference in length between the two thumbs that were intended to be combined together (Figure 1B); and there was a distance in space between the two thumbs that also had different defects, such as short and slender bulks, unstable joints, and nail deformities (Figure 1C).
Detailed clinical assessments and radiological examinations are essential for hand surgeons to design an ideal reconstruction plan for duplicated thumbs. The clinical assessment addresses the soft tissue bulk and shape, the integrity of the nail folds, and the stability and the range and motion (ROM) in both interphalangeal joints (IPJs) and metacarpophalangeal joints (MCPJs). An X-ray of the opposite thumb is beneficial, especially when accompanied by the findings of the clinical examination to obtain as accurate information as possible. Ultrasound may assist in the assessment of neurovascular conditions of the thumbs but is not employed routinely.
The surgery was performed under general anesthesia and tourniquet control. Generally, the procedures are divided into three steps. First, preoperative assessments must determine which digit will provide the best thumb with an essentially stable osteoarticular structure, especially an adequate carpometacarpal joint. Second, tense skin relaxation and first web space broadening, partial cutoff of the deformed nail, diverse transverse or longitudinal osteotomy of metacarpal or phalangeal bones, and K-wire internal fixation are performed on the chosen thumb (Figures 2-4). Then, the defects are evaluated in all aspects. Finally, pedicle complex tissue flaps, according to the defects in all aspects, are carefully designed and elevated from the abandoned thumb to reconstruct the chosen thumb. Clinical manifestations, operating methods, and follow-up results are discussed by way of typical case reports in the following report.
Spasmolysis and blood circulation-promoting drugs were routinely applied after the operation, and the digit was bandaged with external brace fixation. Six weeks after surgery, the internal fixation K-wires and external fixation were removed. Rehabilitation activities were allowed, including active and passive functional exercises of the operated digit.
The survival of pedicled tissue flaps was observed after the operation. The length and diameter of the reconstructed thumb and the contralateral healthy thumb, the finger strength line, the stability and mobility of the MCPJ and IPJ, and the appearance of the nail were observed and recorded. These objective indexes were evaluated by the Horri Tata score system (Table 1) and the ALURRA score system[11] (Table 2). Meanwhile, the satisfaction of the parents of the children with the reconstruction of thumb appearance (aesthetic) and function was recorded.
| Score | 2 | 1 | 0 |
| Range of motion1 | > 70% | 50%-70% | < 50% |
| Instability | - | No instability | Instability |
| Deformity | < 10° | 10°-20° | > 20° |
| Cosmetic | Acceptable | Moderate deformity | Substantial deformity |
| Criteria | Score | ||
| 2 | 1 | 0 | |
| Alignment | < 10° | 10°-20° | > 20° |
| IP joint deviation (radial/ulnar) | |||
| MP joint deviation (radial/ulnar) | < 10° | 10°-20° | > 20° |
| Ulnar instability | |||
| IP joint | < 5° | 5°-15° | > 15° |
| MCP joint | < 20° | 20°-40° | > 40° |
| Radial instability | |||
| IP joint | < 5° | 5°-15° | > 15° |
| MCP joint | < 20° | 20°-40° | > 40° |
| Range of motion | |||
| IP joint | > 70° | 50°-70° | < 50° |
| MCP joint (% of opposite thumb) | > 70° | 50°-70° | < 50° |
| Aesthetical aspects | |||
| Circumference (% of opposite thumb) | 75-100 | 50-75 | < 50 |
| Length | 75-100 | 50-75 | < 50 |
| Nail size | 75-100 | 50-75 | < 50 |
| Nail deformities | None | Small ridge | Severe deformation |
All patients with thumb duplication were treated by pedicle complex tissue flap transfer. Sex distribution, weight, types of duplicated thumb, and nail deformity information were provided. Parametric data, including age, follow-up, range of motion and alignment deviation of the IPJ and MCPJ, aesthetic aspects including circumference, length, nail size, and nail deformities, ALURRA score, and Tata score are described as the mean ± SD.
In total, 15 patients involving eight males and seven females, were included in this study, with an average age at surgery of 13 mo (range: 10 mo to 2 years old). All 15 patients were followed from 20 to 60 mo, with a mean of 42 mo (Table 3). Due to the absence of cooperation, outcomes were measured using appearance, parent satisfaction, and ROM.
| Case | Sex | Term birth | Age (mo) | Weight (kg) | Wassel type | Follow-up | ALURRA criteria | Score | TATA criteria | Score | ||||||||||||||
| Alignment (deviation) | Instability | ROM1 | Aesthetical aspects1 | ROM1 | Instability | Deformity | Cometic | |||||||||||||||||
| IPJ | MCPJ | IPJ (ulnar) | MCPJ (radial) | IPJ | MCPJ | Circumference | Length | Nail size | Nail deformities | |||||||||||||||
| 1 | M | Yes | 12 | 10 | III | 60 | < 5 | 0 | < 5 | 15 | < 5 | 10 | 45 | 90 | 90 | 92 | 85 | None | 22 | 65 | Yes | < 10° | Ac | 6 |
| 2 | F | No | 13 | 10.5 | IV | 20 | < 5 | 5 | < 5 | 10 | < 5 | 15 | 60 | 75 | 120 | 89 | 95 | None | 22 | 65 | Yes | < 10° | Ac | 6 |
| 3 | F | Yes | 11 | 9.5 | IV | 50 | < 5 | 5 | < 5 | 10 | 25 | 15 | 60 | 70 | 90 | 95 | 88 | None | 20 | 65 | No | < 10° | Ac | 5 |
| 4 | M | No | 12 | 10 | V | 34 | < 5 | 5 | < 5 | 12 | < 5 | 10 | 65 | 75 | 74 | 80 | 70 | None | 21 | 70 | Yes | < 10° | Ac | 6 |
| 5 | M | Yes | 10 | 9 | V | 22 | < 5 | 5 | < 5 | 10 | < 5 | 5 | 60 | 75 | 130 | 78 | 90 | Small ridge | 21 | 68 | Yes | < 10° | Md | 5 |
| 6 | F | Yes | 17 | 12 | IV | 46 | < 5 | 6 | < 5 | 10 | < 5 | 10 | 75 | 85 | 80 | 75 | 80 | None | 24 | 80 | Yes | < 10° | Ac | 7 |
| 7 | M | Yes | 13 | 11 | IV | 49 | < 5 | 4 | < 5 | 14 | < 5 | 8 | 80 | 78 | 85 | 80 | 74 | None | 23 | 80 | Yes | < 10° | Ac | 7 |
| 8 | M | No | 11 | 9 | V | 43 | < 5 | 0 | < 5 | 13 | < 5 | 10 | 55 | 77 | 86 | 82 | 97 | Small ridge | 21 | 65 | Yes | < 10° | Ac | 6 |
| 9 | M | Yes | 24 | 15 | V | 53 | < 5 | 0 | < 5 | 10 | < 5 | 5 | 75 | 85 | 118 | 85 | 94 | None | 23 | 80 | Yes | < 10° | Ac | 7 |
| 10 | F | No | 12 | 10.5 | VI | 56 | < 5 | 8 | < 5 | 10 | < 5 | 15 | 55 | 60 | 80 | 86 | 72 | None | 20 | 55 | Yes | < 10° | Ac | 6 |
| 11 | F | Yes | 11 | 9 | V | 52 | < 5 | 3 | < 5 | 12 | < 5 | 10 | 65 | 85 | 78 | 90 | 96 | Small ridge | 22 | 75 | Yes | < 10° | Md | 6 |
| 12 | M | No | 13 | 11 | VI | 46 | < 5 | 4 | < 5 | 15 | < 5 | 10 | 50 | 70 | 79 | 78 | 81 | None | 23 | 60 | Yes | < 10° | Ac | 6 |
| 13 | F | Yes | 14 | 11 | V | 28 | < 5 | 5 | < 5 | 15 | < 5 | 13 | 72 | 75 | 90 | 79 | 90 | Small ridge | 23 | 70 | Yes | < 10° | Md | 5 |
| 14 | M | Yes | 12 | 12 | VI | 27 | < 5 | 6 | < 5 | 15 | < 5 | 8 | 55 | 80 | 79 | 84 | 70 | None | 21 | 66 | Yes | < 10° | Ac | 6 |
| 15 | F | Yes | 10 | 10 | III | 44 | < 5 | 3 | < 5 | 10 | < 5 | 10 | 60 | 95 | 82 | 70 | 68 | None | 21 | 70 | Yes | < 10° | Ac | 6 |
| mean | 13 | 10.6 | 42 | 3.9 | 12.1 | 10.3 | 62.1 | 78.3 | 90.7 | 82.9 | 83.3 | 21.8 | 68.9 | 6 | ||||||||||
| SD | 3.4 | 1.5 | 12.3 | 2.3 | 2.1 | 3.1 | 9.6 | 8.5 | 16.8 | 6.5 | 10.1 | 1.2 | 7.1 | 0.6 | ||||||||||
All pedicle complex tissue flaps survived well after the operation with no arteriovenous crises. The reconstructed thumbs in 14 patients obtained a good longitudinal axis, with appropriate length and girth matching the healthy contralateral thumbs. The reconstructed thumb girth of one child was larger than the contralateral thumb, which was further improved upon treatment by plastic surgery during the surgery for removing the internal fixation. The appearance of the nail was good, though there were various degrees of ridging of the nail after operation of the two halves in some patients (Figure 3). All the MCPJs and IPJs except for one joint of one thumb remained stable after the primary surgery. One case required revision due to IPJ radial collateral instability. The active and passive mobility levels of the MCPJs were good, the mobility of the interphalangeal joints was diminished, and the active mobility was significantly diminished. Compared with the non-operated side, the length of the operated thumb was approximately 82.9%, the girth was 90.7%, and the nail width was 83.3%. The mean ROMs were 62.1% of the unaffected thumb in the IPJ and 78.3% in the MCPJ. MCPJ malalignment showed statistically significant negative correlations with the Tada, and ALURRA scores. Most of the parents were satisfied with the cosmetic and functional results of the reconstructed thumb. The mean ALURRA score was 21.8 (range: 20-24), and the Tada score was 6.9 (range: 5-8).
The basic goals of reconstruction surgery for thumb duplication are to obtain good appearance and function[12,13]. There are many important factors to be considered in the process of reconstruction surgery, including good finger line, sufficient circumference and length of finger, stable metacarpophalangeal and interphalangeal joints, adequate blood circulation, and keen sense function[14,15]. In the case of the poor development of the preserved thumb or even the poor development of both thumbs, it is necessary to cut a part of the tissue structure from the resected thumb to make up for the defects of the preserved thumb.
The Bilhaut-Cloquet procedure and its modified operation provided a sound solution to these situations involving symmetrical or essentially symmetrical compound thumbs, slender little finger bodies, joint deflection and instability, lateral deviation of the nail, and skin defects[16-19]. If the distance between the two thumbs is far or if they are different in length, BC and its modified operation have difficulty achieving good thumb results. Therefore, according to the condition of retaining the tissue defect of the thumb, a tissue flap pedicled with the neurovascular bundle of the finger can be designed and cut from the resected finger for long-distance transfer, which can effectively solve the above problems. Our study included 15 cases with a long distance between or different lengths of the two thumbs. We used the above method for surgical treatment, and good clinical outcomes were achieved during the follow-up.
When the two thumbs had different lengths (Figure 1B), we usually used the shorter thumb with pedicle extension and then combined it with the other thumb to keep the thumb length as long as possible (Figure 3B). The case presented in this study demonstrated that the pedicle can effectively extend to the distal end up to 1 cm, which is enough to compensate for the difference in length between the two thumbs. The skin defect of the proximal pedicle caused by the extension of the thumb to the distal end can be effectively covered by local skin.
When the distance between the two thumbs was relatively far, especially when combined with a narrow mouth in the thumb web (Figure 4A), a tissue flap pedicled with the digital nerve and vascular bundle for a longer distance transfer was used to achieve the combination of the two thumbs (Figure 4B). To achieve the distant transfer of pedicled tissue flaps, the vascular pedicle often needs to be free to the proximal end to reach the level of the metacarpal base. If the tissue mass is large, it can be transferred with a piece of dorsal reflux vein. A transverse design should be avoided in the incision at the thumb web to prevent contracture scarring
In the process of bone joint splicing, especially the IPJ, epiphyseal plate butt joint and joint face joint connections were often contradictory. To preserve the growth potential of the phalanges, the epiphyseal plate butt joint had priority in handling and subsequently repairing the surface of the joint. In the follow-up cases, although the active and passive ranges of motion of the interphalangeal joint decreased, the joint was stable with a good holding function.
Nail splicing is an important step in the process of correcting compound thumb deformities. Tien et al[20] and Wang et al[21] performed an in-depth follow-up investigation and formulated the evaluation criteria in detail. To achieve enough width and good radians of regenerated nails and to prevent the occurrence of longitudinal ridges in the middle of nails, longitudinal oblique osteotomy of the distal phalanx can achieve a good arc fit of the nail bed. If the original nail is too narrow, we usually butt sutures after removing the nail and peeling off the nail bed from the upper part of the phalanx on the basis of the abovementioned treatment. In the follow-up, the regenerated nails achieved a good appearance. In conclusion, distal transfer of pedicled composite tissue flaps from thumb resection can effectively compensate for a variety of tissue defects of the thumb to achieve good therapeutic effects.
Harvesting a pedicle flap from the severed thumb is a safe and reliable procedure. Defects of the preserved thumb, such as the skin, nail, and bone, can be effectively restored with the complex tissue flap.
Thumb polydactyly is one of the most common congenital hand deformities, and the Bilhaut-Cloquet procedure or a modified one is often used. However, controversy remains over the rare instances in which both thumbs are not of similar length or far apart in distance.
Bilhaut-Cloquet procedure or a modified one is often used for thumb polydactyly. However, controversy remains over the rare instances in which both thumbs are not of similar length or far apart in distance.
To evaluate the clinical outcomes of pedicle complex tissue flap transfer in the treatment of duplicated thumbs with unequal size.
We performed a cross-sectional study of patients who underwent duplicated thumb reconstruction by pedicle complex tissue flap transfer from January 2014 to December 2020.
An appropriate volume with a stable joint and good appearance was obtained in 14 reconstructed thumbs. The mean ALURRA score was 21.8 (range: 20-24), and the Tada score was 6.9 (range: 5-8). Compared with the non-operated side, the length of the operated thumb was approximately 95%, the girth was 89%, and the nail width was 82.9%. The mean ranges of motion were 62.1% of that of the unaffected thumb in the interphalangeal joint and 78.3% in the metacarpophalangeal joint.
Harvesting a pedicle flap from a severed thumb is a safe and reliable procedure. Defects of the preserved thumb, such as the skin, nail, and bone, can be effectively restored using the complex tissue flap.
Pedicle complex tissue flap transfer should be the initial management strategy for patients with duplicated thumbs with unequal size. In the future, more controlled studies with multicenter samples will be needed to confirm this finding.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Committee Member of Traumatology and Orthopedics of Shandong Pain Medical Association; European Orthopaedic Research Society; President of German and Chinese Association of Physicians and Medical Research.
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abulsoud MI S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Yan JP
| 1. | Van Wyhe RD, Trost JG, Koshy JC, Pederson WC. The Duplicated Thumb: A Review. Semin Plast Surg. 2016;30:181-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Comer GC, Potter M, Ladd AL. Polydactyly of the Hand. J Am Acad Orthop Surg. 2018;26:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Thomas BP, Pallapati S. Congenital thumb differences- current concepts. J Clin Orthop Trauma. 2020;11:580-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Dobyns JH, Lipscomb PR, Cooney WP. Management of thumb duplication. Clin Orthop Relat Res. 1985;26-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Ogino T, Ishii S, Takahata S, Kato H. Long-term results of surgical treatment of thumb polydactyly. J Hand Surg Am. 1996;21:478-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 89] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Yeung CM, Choi AKY, Tong JWS, Fok W, Chan YF, Chow YY. Long-Term Results of Surgically Treated Radial Polydactyly - An Outcome Correlation Study. J Hand Surg Asian Pac Vol. 2019;24:264-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Chang CF, Chen IC, Tsai YC, Lai CS, Chen YW, Lu CT, Yen JH. Transposition of Duplicated Thumb for Reconstruction of Asymmetric Radial Polydactyly. Ann Plast Surg. 2019;82:S13-S17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Tada K, Yonenobu K, Tsuyuguchi Y, Kawai H, Egawa T. Duplication of the thumb. A retrospective review of two hundred and thirty-seven cases. J Bone Joint Surg Am. 1983;65:584-598. [PubMed] [DOI] [Full Text] |
| 9. | Wassel HD. The results of surgery for polydactyly of the thumb. A review. Clin Orthop Relat Res. 1969;64:175-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Hu CH, Thompson ER, Agel J, Bauer AS, Moeller AT, Novotny SA, Van Heest AE, Bohn DC; CoULD Registry Study Group. A Comparative Analysis of 150 Thumb Polydactyly Cases from the CoULD Registry Using the Wassel-Flatt, Rotterdam, and Chung Classifications. J Hand Surg Am. 2021;46:17-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Lim YB, Seul JH, Nam HJ, Woo SH. Extended Indications of Bilhaut-Cloquet Procedure for Type III and IV of Duplicated Thumb. J Korean Soc Plast Reconstr Surg. 2011;38:821-828. |
| 12. | Tonkin MA. Thumb duplication: concepts and techniques. Clin Orthop Surg. 2012;4:1-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Cabrera González M, Pérez López LM, Martínez Soto G, Gutiérrez de la Iglesia D. Prognostic value of age and Wassel classification in the reconstruction of thumb duplication. J Child Orthop. 2013;7:551-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Tonkin MA, Bulstrode NW. The Bilhaut-Cloquet procedure for Wassel types III, IV and VII thumb duplication. J Hand Surg Eur Vol. 2007;32:684-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Al-Qattan MM, Kattan AE, Al-Lazzam A, Gelidan AG. A Modified Bilhaut-Cloquet Procedure for Zigzag Thumb Polydactyly Types III and IV. Plast Reconstr Surg Glob Open. 2017;5:e1589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Baek GH, Gong HS, Chung MS, Oh JH, Lee YH, Lee SK. Modified Bilhaut-Cloquet procedure for Wassel type-II and III polydactyly of the thumb. J Bone Joint Surg Am. 2007;89:534-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Baek GH, Gong HS, Chung MS, Oh JH, Lee YH, Lee SK. Modified Bilhaut-Cloquet procedure for Wassel type-II and III polydactyly of the thumb. Surgical technique. J Bone Joint Surg Am. 2008;90 Suppl 2 Pt 1:74-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Dautel G, Perrin P. Use of an Axial Flap to Increase the Girth of Wassel IV Thumb Reconstructions. J Hand Surg Am. 2015;40:1327-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Abid A, Accadbled F, Knorr G, Darodes P, Cahuzac JP, Sales de Gauzy J. Type IV-D thumb duplication: A new reconstruction method. Orthop Traumatol Surg Res. 2010;96:521-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Tien YC, Chih TT, Wang TL, Fu YC, Chen JC. Soft tissue reconstruction for type IV-D duplicated thumb: a new surgical technique. J Pediatr Orthop. 2007;27:462-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Wang AY, Gao WY, Wu LM, Li ZJ, Chen XL, Li XY. Nail Fusion Plasty: Nail Cosmetic Results and Assessment Criteria of Nail Reconstruction. Ann Plast Surg. 2015;75:290-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |