Published online Dec 6, 2021. doi: 10.12998/wjcc.v9.i34.10733
Peer-review started: August 2, 2021
First decision: September 1, 2021
Revised: September 9, 2021
Accepted: October 18, 2021
Article in press: October 18, 2021
Published online: December 6, 2021
Processing time: 119 Days and 21 Hours
Penetrating neck injuries require prompt recognition, diagnosis and management of critical airways. This case demonstrates an emergent situation that a “medical negligence” was avoided with the aid of end-tidal carbon dioxide (ETCO2) waveform.
We report a case of malposition of the endotracheal tube into the right hemithoracic cavity for cervical knife trauma, resulting in pneumothorax. Tube placement was not confirmed during emergency airway management, and the patient was directly transferred to the emergency operation room. Assisted by ETCO2 and imaging examinations, the anesthetist timely noticed the absence of ETCO2 waveform and resolved this urgent situation before anesthesia induction.
This case emphasizes the necessity of ETCO2 waveform and/or X-ray confirma
Core Tip: We report a case of malposition of the endotracheal tube into the right hemithoracic cavity for cervical knife trauma, resulting in pneumothorax. Fortunately, the anesthetist timely noticed the absence of end-tidal carbon dioxide (ETCO2) waveform and reviewed the thoracic computed tomography scanning just before anesthesia induction. This case highlights the role of ETCO2 waveform and/or chest radiography in confirmation of emergency endotracheal intubation, especially for junior doctors and emergency physicians.
- Citation: Li KX, Luo YT, Zhou L, Huang JP, Liang P. Tracheal tube misplacement in the thoracic cavity: A case report. World J Clin Cases 2021; 9(34): 10733-10737
- URL: https://www.wjgnet.com/2307-8960/full/v9/i34/10733.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i34.10733
Penetrating neck injuries (PNI) are neck injuries penetrating the platysma and represent 5% to 10% of all traumatic events with a high mortality rate due to unprotected airway and proximity to vital vascular structures and trachea[1,2]. PNI requires anesthesiologists and surgeons to maintain vigilance on timely recognition, diagnosis, and management[2-4]. Challenging airway management is inevitable[5]. End-tidal carbon dioxide (ETCO2) monitoring non-invasively detects the concentration of CO2 at the end of expiration[6]. And the appearance of ETCO2 waveform is regarded as the golden standard for proper intubations. However, intubation without confirmation tends to happen, especially in urgent situations, such as PNI. Here we report a rare case of misplaced endotracheal tube into the thoracic cavity.
A 28-year-old female patient was admitted to the emergency department with knife injury to the neck for 12 h.
The patient was found to have tracheal injury 1cm below the thyroid cartilage with severe pain, active bleeding (the specific amount of blood loss was unknown) dyspnea, chest distress, shortness of breath and dysphonia. She was managed with compression packing at a local hospital and was transferred to our hospital for further manage
The patient had a disease-free personal and family history.
The patient had not the special personal or family history.
On admission, the patient was awake with stable vital signs: temperature 36.6 ℃, pulse rate 98 bpm, respiratory rate 22/min and blood pressure 118/70 mmHg. Tissue deficits were identified on the left sternocleidomastoid muscles. Breath sounds were slightly diminished, and dry and moist rales were noticed on both upper lobes.
Leucocyte count was 12.79 × 109/L, where neutrophils accounted for 86.8%. And other examinations were all normal, such as hematocrit and hemoglobin count. Urine analysis was also normal. Prothrombin, partial thromboplastin times, and d-dimers were within normal ranges. Electrocardiogram showed a sinus rhythm.
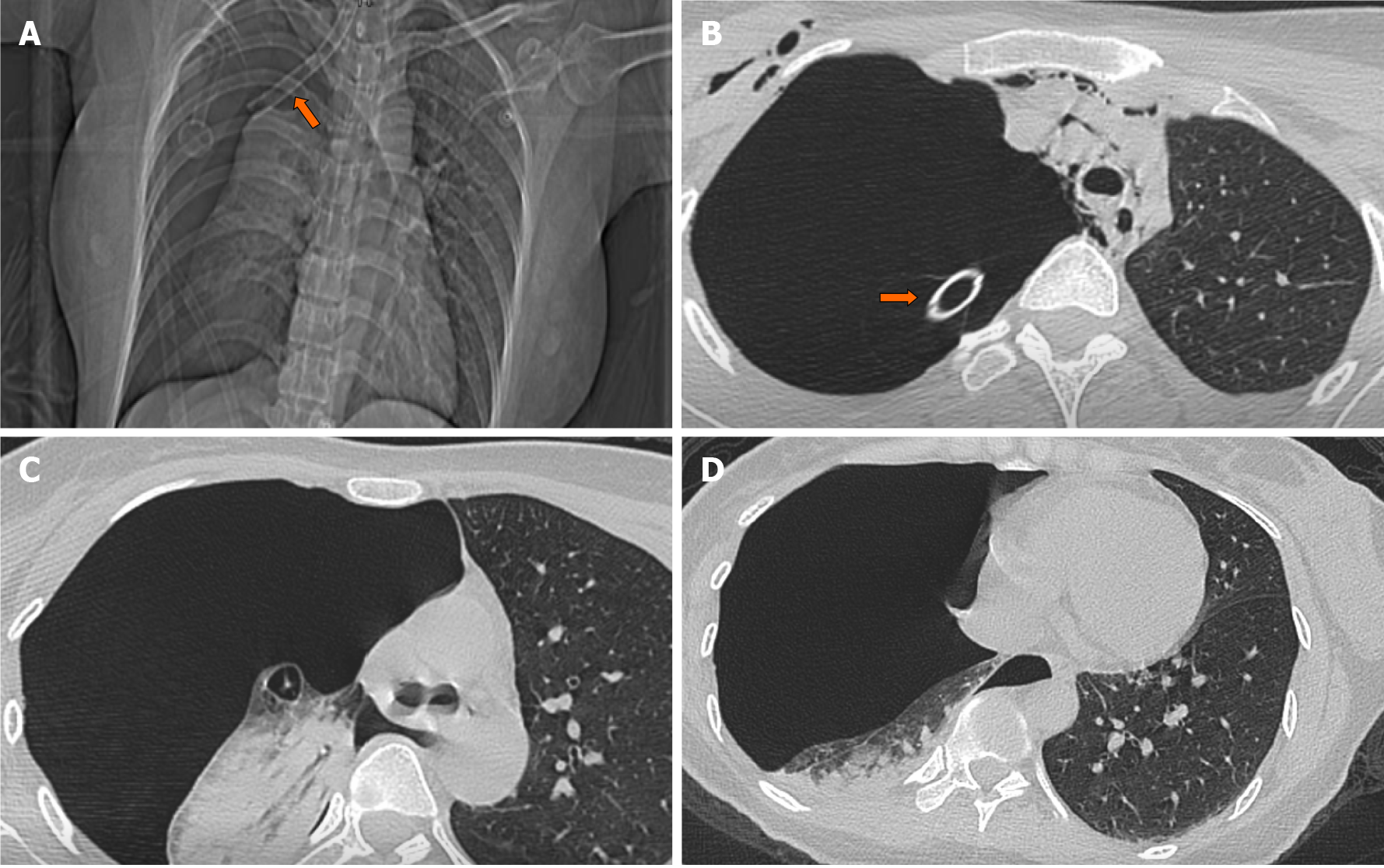
After the endotracheal tube was inserted, the patient underwent urgent imaging examinations for operation preparation. Computed tomographic angiography (CTA) showed that there was no leakage, occlusion or expansion of cervical blood vessels and branches. Emergent cervical computed tomography (CT) scan revealed extensive gas accumulation in the mediastinum and underneath the cervical tissue, and continuous interruption in the anterior part of trachea. Chest CT scan demonstrated that the right hemithoracic cavity with limited pleural effusion was collapsed by 70% approximately. The patchy lesions and shadows suggested slight infection in the right hemithorax.
The patient was diagnosed with cervical knife trauma and tracheal injuries, which should be managed by emergency operation.
The emergency medicine physician inserted a 6.5# endotracheal tube into the wound, and inflated the cuff to prevent bleeding from the lumen into the ruptured trachea. Right chest tube was placed for preventing suspected pneumothorax. The patient was immediately transferred to the operating room for exploration after CT scan was performed, but without final reading and confirmation.
The anesthetist was informed that the airway was secured without aspiration risks. However, the patient was agitated and in respiratory distress with 85% pulse oxygenation on room air. After the tracheal tube was connected with anesthesia circuit, the breathing bag of the anesthesia machine was expanding and shrinking during patient’s spontaneous breathing (25/min). However, ETCO2 waveform was absent. CT scan was reviewed immediately and revealed that the endotracheal tube entered into the right hemithoracic cavity and the right lung was collapsed by 70% approximately due to extensive pneumothorax (Figure 1).
The anesthesiologist and otolaryngologist immediately reinserted the tracheal tube, connecting it to the ETCO2 monitor. The tube placement was confirmed carefully before final fixation. Next, the patient underwent open neck exploration, tracheal end-to-end anastomosis, recurrent laryngeal nerve reconstruction and tracheotomy thereafter. The subsequent clinical course was uneventful, the patient was transferred into intensive care unit and discharged after two-week hospitalization.
We presented a case of tracheal tube misplacement into the thoracic cavity for neck injury. Although the emergency medicine physicians promptly evaluated and attempted to manage the airway with an awake endotracheal intubation, the tube was inserted into the thoracic cavity and produced pneumothorax. Because the patient was on spontaneous breathing and a chest tube was placed on the same side, breath sounds were heard bilaterally. The patient was sent immediately to the operating room assuming successful airway establishment. Successful airway management should have been confirmed with clinical evaluation, chest radiography, and ETCO2 detection[4].
Iatrogenic tracheobronchial injuries by intubation have been reported[6-8], including tracheal laceration[9,10] and subcutaneous emphysema[11-13]. Incorrect tube sizes and reintubation may contribute to iatrogenic injuries with direct laryngoscopy after endotracheal intubation[14]. Therefore, some studies recommended awake intubation, flexible fiberoptic bronchoscopy, or direct ultrasound visualization to avoid false passage and tracheal injury[15-18]. When dealing with tracheal trauma from PNI, confirmation of the endotracheal tube placement by ETCO2 waveform and/or X-ray/CT scan is mandatory.
Airway establishment is the priority option for tracheal injuries, which was an extremely urgent situation for PNI. Emergent evaluation and treatment are challenging. Negligence is inevitable, especially in emergency situations. This case highlights the role of ETCO2 waveform and/or chest radiography in confirmation of emergent endotracheal intubation after emergent intubation, especially for junior doctors and emergent physicians.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Beşler MS, Masaki S S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Shiroff AM, Gale SC, Martin ND, Marchalik D, Petrov D, Ahmed HM, Rotondo MF, Gracias VH. Penetrating neck trauma: a review of management strategies and discussion of the 'No Zone' approach. Am Surg. 2013;79:23-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 75] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 2. | Sgardello SD, Christodoulou M, Abbassi Z. Anatomy of a Suicide: A Case Report. Am J Case Rep. 2019;20:1801-1804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Triggiani E, Belsey R. Oesophageal trauma: incidence, diagnosis, and management. Thorax. 1977;32:241-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 84] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Mandavia DP, Qualls S, Rokos I. Emergency airway management in penetrating neck injury. Ann Emerg Med. 2000;35:221-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 55] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Hiraoka C, Ikuta Y, Yamamoto T. [A Case of Penetrating Injury of the Neck in Which It Was Difficult to Secure the Airway]. Masui. 2015;64:1052-1055. [PubMed] |
| 6. | Siobal MS. Monitoring Exhaled Carbon Dioxide. Respir Care. 2016;61:1397-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 7. | Schneider T, Storz K, Dienemann H, Hoffmann H. Management of iatrogenic tracheobronchial injuries: a retrospective analysis of 29 cases. Ann Thorac Surg. 2007;83:1960-1964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 99] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Regragui IA, Fagan AM, Natrajan KM. Tracheal rupture after tracheal intubation. Br J Anaesth. 1994;72:705-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Borasio P, Ardissone F, Chiampo G. Post-intubation tracheal rupture. A report on ten cases. Eur J Cardiothorac Surg. 1997;12:98-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 100] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Ross HM, Grant FJ, Wilson RS, Burt ME. Nonoperative management of tracheal laceration during endotracheal intubation. Ann Thorac Surg. 1997;63:240-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 51] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Cunningham LC, Jatana KR, Grischkan JM. Conservative management of iatrogenic membranous tracheal wall injury: a discussion of 2 successful pediatric cases. JAMA Otolaryngol Head Neck Surg. 2013;139:405-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Watters KF, Lacy PD, Walsh RM. Massive subcutaneous emphysema following routine endotracheal intubation. J Laryngol Otol. 2003;117:899-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Harris R, Joseph A. Acute tracheal rupture related to endotracheal intubation: case report. J Emerg Med. 2000;18:35-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Doherty KM, Tabaee A, Castillo M, Cherukupally SR. Neonatal tracheal rupture complicating endotracheal intubation: a case report and indications for conservative management. Int J Pediatr Otorhinolaryngol. 2005;69:111-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Wood JW, Thornton B, Brown CS, McLevy JD, Thompson JW. Traumatic tracheal injury in children: a case series supporting conservative management. Int J Pediatr Otorhinolaryngol. 2015;79:716-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Mercer SJ, Jones CP, Bridge M, Clitheroe E, Morton B, Groom P. Systematic review of the anaesthetic management of non-iatrogenic acute adult airway trauma. Br J Anaesth. 2016;117 Suppl 1:i49-i59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Turbitt L, Nawaz Y, Sharpe E. Mediastinal intubation following complete tracheal transection secondary to blunt trauma. Anaesth Intensive Care. 2011;39:137-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Horton CL, Brown CA 3rd, Raja AS. Trauma airway management. J Emerg Med. 2014;46:814-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |