Published online Dec 6, 2021. doi: 10.12998/wjcc.v9.i34.10723
Peer-review started: June 28, 2021
First decision: July 26, 2021
Revised: July 29, 2021
Accepted: October 8, 2021
Article in press: October 8, 2021
Published online: December 6, 2021
Processing time: 155 Days and 4.4 Hours
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is a safe and minimally invasive diagnostic tool for mediastinal and hilum evaluation. However, infectious complications may occur after EBUS-TBNA. Among these, mediastinitis and pericarditis are rare.
A 67-year-old woman was referred to our hospital due to paratracheal lymph node enlargement on chest computed tomography (CT). EBUS-TBNA was performed on the lymph node lesions, and prophylactic oral antibiotics were administered. Seven days after EBUS-TBNA, the patient visited the emergency room with a high fever and chest pain. Laboratory test results revealed leuko
Mediastinitis and pericarditis after EBUS-TBNA are rare but should be considered even after the use of prophylactic antibiotics.
Core Tip: Acute mediastinitis and pericarditis are rare complications of endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA). This case presented with acute mediastinitis and pericarditis that developed despite prophylactic antibiotic use after EBUS-TBNA and improved after antibiotic and surgical mana
- Citation: Koh JS, Kim YJ, Kang DH, Lee JE, Lee SI. Severe mediastinitis and pericarditis after endobronchial ultrasound-guided transbronchial needle aspiration: A case report. World J Clin Cases 2021; 9(34): 10723-10727
- URL: https://www.wjgnet.com/2307-8960/full/v9/i34/10723.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i34.10723
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is used to biopsy enlarged lymph nodes in the mediastinum and hilum to stage patients with lung cancer and to provide a definitive diagnosis of lymphadenopathy. Although EBUS-TBNA is a safer and less invasive procedure than mediastinoscopy, severe complications can occur; A major complication rate of 0.3% was found in one meta-analysis[1]. Complications such as massive bleeding, cardiac tamponade, hemomediastinum, pneumomediastinum and pneumothorax have been reported as a com
The patient presented with a high fever and chest pain. Seven days after EBUS-TBNA, she visited the emergency room.
A 67-year-old woman was referred to our hospital because of lymph node en
The patient had no comorbidities.
The patient and families were previously healthy.
On physical examination, the patient appeared acutely ill with a clear mental status. The patient was febrile (37.8°C) and had a stable blood pressure of 100/68 mmHg, pulse rate of 107 bpm, respiratory rate of 18/min, and body temperature of 37.8°C. The breath sounds on the left side of the chest were decreased.
Laboratory tests revealed leukocytosis with a left shift and the following results: White blood cell count: 14410/mm3; neutrophils: 81.3%; hemoglobin: 9.8 g/dL; platelet count: 198000/mm3. Blood chemistry showed elevated total bilirubin (1.40 mg/dL), aspartate aminotransferase (132 U/L), and alanine aminotransferase (137 U/L) levels in a normal renal panel. The cardiac enzyme level was normal, and the NT-proBNP level was slightly high (562.6 pg/mL). C-reactive protein level was elevated (25.7 mg/dL) and lactic acid level was within the normal range.
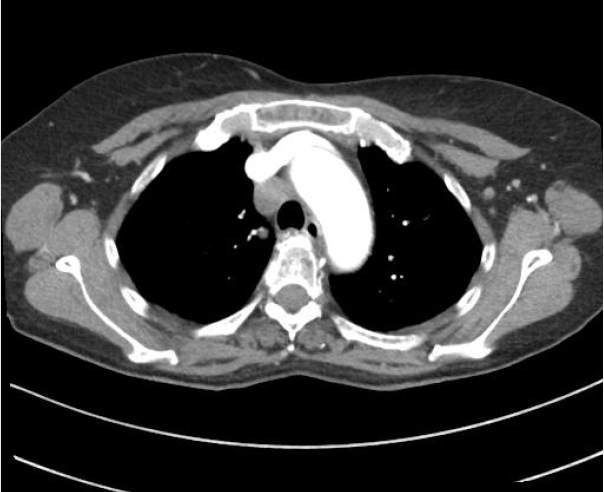
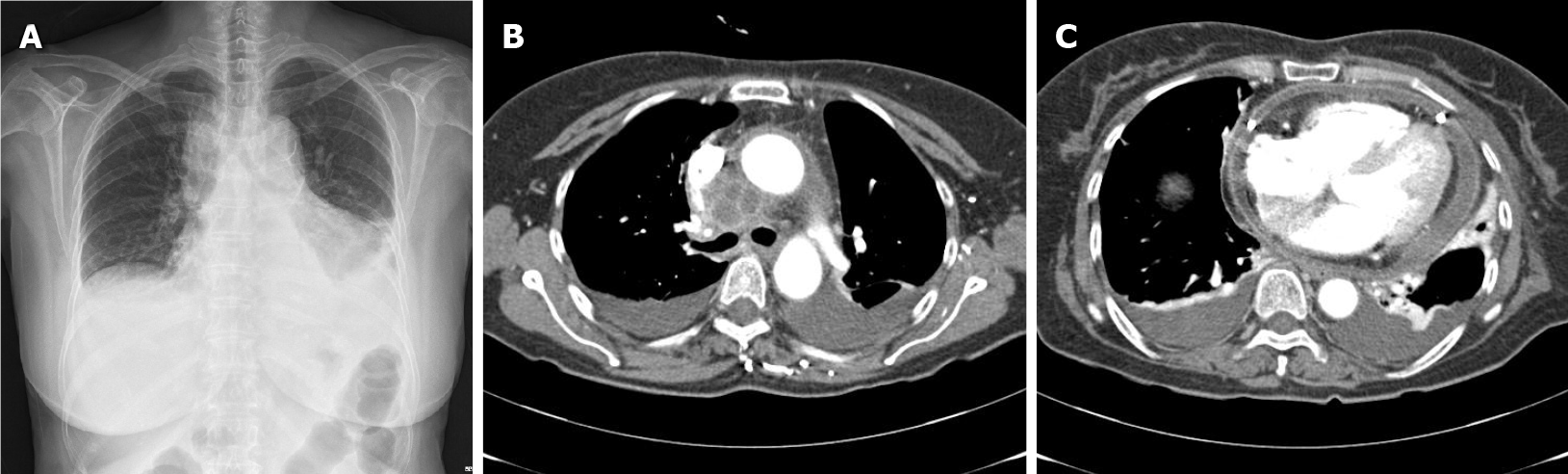
Chest radiography revealed left lung field haziness with pleural effusion and cardiomegaly (Figure 2). Emergency echocardiography revealed pericardial effusion of > 1 cm, and the blood pressure dropped (85/51 mmHg) after emergency echocardiography; cardiac drainage through the pericardiocentesis was performed. Chest CT showed a mediastinal abscess formation in the right paratracheal lymph node and pericardial and bilateral pleural effusions (Figure 2).
The final diagnosis in the present case was mediastinitis and pericarditis after EBUS-TBNA.
Intravenous antibiotic treatment was initiated. Exploratory thoracotomy was performed by consulting the thoracic and cardiovascular surgery department. Surgical observation revealed whole lung adhesions, mediastinal abscesses, and effusions in the lymph node area. Surgery was completed after adhesiolysis, irrigation, and drainage.
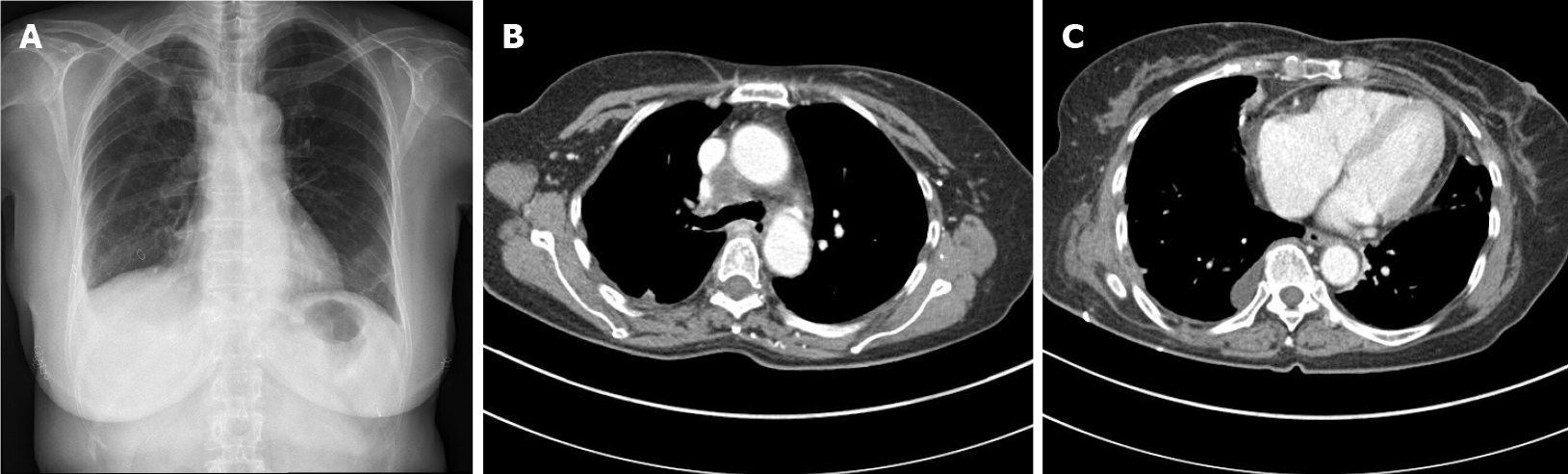
Postoperatively, laboratory findings and the patient’s general condition gradually improved. The cardiac drainage tube and chest drainage were removed 4 d and 16 d postoperatively, respectively (Figure 3). No bacterial pathogens were detected in the specimens obtained from the pericardial and abscess drainage.
The patient recovered favorably and was discharged 31 d after the operation. There was no evidence of recurrence within the 12 mo follow-up period.
Convex-probe EBUS-TBNA is a minimally invasive diagnostic technique for peritracheal and peribronchial areas[3]. EBUS-TBNA identifies the puncture site through real-time ultrasound guidance, allowing accurate sampling from lesions and cytological and histological diagnosis. The cumulative sensitivity of EUBS-TBNA is 88%-93% and the cumulative specificity is 100% in lymph node staging of lung cancer[4,5].
The overall major complication rate of this procedure was found to be 0.23%-1.23% in a previous meta-analysis[1,2]. Pneumothorax, hemopericardium, and infections such as mediastinitis, pericarditis, and abscesses are reportedly caused by EBUS-TBNA[1,2]. In 7345 EBUS-TBNA cases in Japan, hemorrhage was the most frequent complication (0.68%), followed by infection (0.19%, mediastinitis, n = 7; pneumonia, n = 4; pericarditis, n = 1; cyst infection, n = 1) and pneumothorax (0.03%)[2]. As such, the probability of mediastinitis and pericarditis occurring as a complication of EBUS-TBNA is very low. In addition, case reports revealing the occurrence of mediastinitis or pericarditis after EBUS-TBNA are rare[6-12].
Antibiotic prophylaxis is not used in most EBUS-TBNA cases. However, in this case, mediastinitis and pericarditis occurred even with the use of prophylactic antibiotics. Antibacterial precautions are not recommended for routine diagnostic bronchoscopy, unless there is a previous history of spleen removal, artificial heart valves, or endocarditis[13]. This patient with an enlarged, homogeneous right paratracheal lymph node underwent diagnostic EBUS-TBNA with a 22-gauge needle to obtain the tissue core. A total of 11 punctures were performed because of insufficient tissue cores. Multiple needle passes would have caused mediastinitis and pericarditis in this patient. There are no definitive guidelines regarding which prophylactic antibiotics should be used and for which patients. Despite the use of amoxicillin/clavulanate in this patient, infectious complications occurred; therefore, further research is needed to determine the optimal antibiotic course.
In this case, the patient recovered with the help of antibiotics, pericardial drainage, and surgery. Mediastinitis, with a mortality rate of approximately 50%, is a life-threatening condition that requires aggressive treatment with both broad-spectrum antibiotics and surgical intervention[14]. Appropriate antibiotic therapy and pericardial drainage may be helpful in treating infectious pericarditis. If vital signs are unstable, immediate pericardial drainage can help prevent pericardial tamponade in patients[15].
In conclusion, we reported a patient who developed mediastinitis and pericarditis as complications of EBUS-TBNA, even after the use of prophylactic antibiotics. Although EBUS-TBNA is a minimally invasive diagnostic and treatment option, the possibility of serious complications needs to be considered. Further research is needed to determine which type of prophylactic antibiotic should be used in at-risk patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Respiratory system
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fusaroli P S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Holty JE, Kuschner WG, Gould MK. Accuracy of transbronchial needle aspiration for mediastinal staging of non-small cell lung cancer: a meta-analysis. Thorax. 2005;60:949-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 159] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 2. | Asano F, Aoe M, Ohsaki Y, Okada Y, Sasada S, Sato S, Suzuki E, Semba H, Fukuoka K, Fujino S, Ohmori K. Complications associated with endobronchial ultrasound-guided transbronchial needle aspiration: a nationwide survey by the Japan Society for Respiratory Endoscopy. Respir Res. 2013;14:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 184] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 3. | Yasufuku K, Chiyo M, Sekine Y, Chhajed PN, Shibuya K, Iizasa T, Fujisawa T. Real-time endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest. 2004;126:122-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 450] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 4. | Gu P, Zhao YZ, Jiang LY, Zhang W, Xin Y, Han BH. Endobronchial ultrasound-guided transbronchial needle aspiration for staging of lung cancer: a systematic review and meta-analysis. Eur J Cancer. 2009;45:1389-1396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 400] [Cited by in RCA: 421] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 5. | Shen Y, Qin S, Jiang H. Endobronchial ultrasound-guided transbronchial needle aspiration combined with either endoscopic ultrasound-guided fine-needle aspiration or endoscopic ultrasound using the EBUS scope-guided fine-needle aspiration for diagnosing and staging mediastinal diseases: a systematic review and meta-analysis. Clinics (Sao Paulo). 2020;75:e1759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Inoue T, Nishikawa T, Kunimasa K, Tamiya M, Kuhara H, Nishino K, Fujiwara M, Fujita M, Imamura F, Kumagai T. Infectious pericarditis caused by Gemella sanguinis induced by Endobronchial Ultrasound-guided Transbronchial Needle Aspiration (EBUS-TBNA): A case report. Respir Med Case Rep. 2020;30:101057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Jahoor A, Ghamande S, Jones S, Boethel C, White HD. Mediastinitis Following Endobronchial Ultrasound-guided Transbronchial Needle Aspiration. J Bronchology Interv Pulmonol. 2017;24:323-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Jain A, Nayyar P, Chitkeshi V, Bahl A. An unusual complication after endobronchial ultrasound-guided transbronchial needle aspiration: Case report. Breathe (Sheff). 2018;14:e6-e11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Lee HY, Kim J, Jo YS, Park YS. Bacterial pericarditis as a fatal complication after endobronchial ultrasound-guided transbronchial needle aspiration. Eur J Cardiothorac Surg. 2015;48:630-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Liu W, Wang Y, Zhang W, Wu H, Liu Z. Pneumonia, pleurisy, mediastinitis, and mediastinal cyst infection secondary to endobronchial ultrasound-guided transbronchial needle aspiration: A case report. Medicine (Baltimore). 2021;100:e25973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Matsuoka K, Ito A, Murata Y, Sakane T, Watanabe R, Imanishi N, Matsuoka T, Nagai S, Ueda M, Miyamoto Y. Severe Mediastinitis and Pericarditis After Transbronchial Needle Aspiration. Ann Thorac Surg. 2015;100:1881-1883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Yokoyama Y, Nakagomi T, Shikata D, Higuchi R, Oyama T, Goto T. Surgical treatment for mediastinal abscess induced by endobronchial ultrasound-guided transbronchial needle aspiration: a case report and literature review. World J Surg Oncol. 2017;15:130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | British Thoracic Society Bronchoscopy Guidelines Committee; a Subcommittee of Standards of Care Committee of British Thoracic Society. British Thoracic Society guidelines on diagnostic flexible bronchoscopy. Thorax. 2001;56 Suppl 1:i1-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 151] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 14. | Prado-Calleros HM, Jiménez-Fuentes E, Jiménez-Escobar I. Descending necrotizing mediastinitis: Systematic review on its treatment in the last 6 years, 75 years after its description. Head Neck. 2016;38 Suppl 1:E2275-E2283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 74] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 15. | Imazio M, Gaita F, LeWinter M. Evaluation and Treatment of Pericarditis: A Systematic Review. JAMA. 2015;314:1498-1506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 259] [Article Influence: 25.9] [Reference Citation Analysis (0)] |