Published online Dec 6, 2021. doi: 10.12998/wjcc.v9.i34.10671
Peer-review started: April 6, 2021
First decision: July 6, 2021
Revised: July 14, 2021
Accepted: October 20, 2021
Article in press: October 20, 2021
Published online: December 6, 2021
Processing time: 237 Days and 17.9 Hours
Fibrous dysplasia (FD) is a developmental hamartomatous bone disease characterized by a blend of fibrous and osseous entities. Though rarely malignant, the tumor can vary from being small and asymptomatic, to a fairly large sized lesion, progressing gradually, compromising occlusion and facial esthetics. Treatment approach depends on the stage of skeletal maturity. It primarily involves surgical management for stabilizing the disease process. Post-surgical comprehensive dental treatment is necessary for restoring form and function of the jaws and teeth. This article describes comprehensive orthodontic management of severe malocclusion in a surgically operated case of FD maxilla.
A 19-year female presented with a chief complaint of excessive gingival display when smiling. Dental history included swelling of gums around the upper right front teeth, diagnosed at the age of 15 as FD of the right anterior maxillary segment and treated with surgical recontouring of the dysplastic bone. The clinical and radiological examinations showed adequate post-surgical healing. The surgically treated dysplastic area presented with right canting of the maxillary anterior occlusal plane. The maxillary teeth were torqued palatally, with the root of the right maxillary canine exposed clinically. We discuss sequential management of the associated malocclusion with comprehensive fixed orthodontics, along with special precautions taken to prevent reactivation of the quiescent and healed lesion.
The adequate healing of fibro-dysplastic bone post-surgery must be allowed before initiating orthodontic tooth movement in the dysplastic bone. Periodic follow-ups are needed to monitor stability of occlusion and any relapse of the lesion.
Core Tip: This article discusses comprehensive management of severe malocclusion in a surgically treated case of maxillary fibrous dysplasia. Adequate healing of the fibro-dysplastic bone post-surgery must be allowed before initiating orthodontic tooth movement. Orthodontic treatment in such patients should mainly focus on improving function and esthetics. Special precautions must be taken to prevent reactivation/relap
- Citation: Kaur H, Mohanty S, Kochhar GK, Iqbal S, Verma A, Bhasin R, Kochhar AS. Comprehensive management of malocclusion in maxillary fibrous dysplasia: A case report. World J Clin Cases 2021; 9(34): 10671-10680
- URL: https://www.wjgnet.com/2307-8960/full/v9/i34/10671.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i34.10671
Fibrous dysplasia (FD) is a rare slow-growing disorder of the bone characterized histologically by excessive cellular fibrous connective tissue interspersed with irregular bony trabeculae[1,2]. Lichtenstein and Jaffe first identified and named this pathological bone deformity in 1938. The etiology is still unclear, although certain studies highlight mutations in the alpha-subunit of the stimulatory G protein encoded by the gene GNAS[3]. This rare clinical entity presents in three forms- monostotic, polyostotic, and polyostotic with endocrinopathies with hyperpigmentation (café-au-lait macules) known as McCune Albright syndrome[4]. Generalized FD involving the face and skull and appearing prominently in the middle third of the face is known as "Leontiasis ossea"[5]. Monostotic forms are less severe, most commonly involving the zygomatic-maxillary complex. In monostotic forms involving the jaw, the symptoms may vary depending on the location, resulting in malocclusions, asymmetry, facial deformity, nasal obstruction, visual changes, pain and/or paresthesia. Either crowding or spacing may be seen, because teeth positions can change following the contours of the bony deformity. Polyostotic FD presents as multiple lesions involving adjacent bone. Skeletal deformities in the extremities may be seen, due to repeated fractures in the affected bone[4]. The most common dental anomalies associated with FD include tooth rotation, oligodontia, displacement, enamel hypoplasia, enamel hypomineralization, taurodontism, retained deciduous teeth and attrition[6]. The differential diagnosis for FD includes ossifying fibroma, hyperparathyroidism, chronic osteomyelitis, Paget's disease, osteosarcoma and various other bony lesions. These entities should be excluded by taking a detailed history, evaluating the pattern of growth of the lesion, clinical examination, radiographs and histological analysis[6-8].
Management of FD depends upon the severity and rate of progression of the lesion. There are no accepted medical treatments for curing or stopping the progression of the disease. Bisphosphonates may be used for pain management, although they have shown no significant effect on disease progression[9]. Monoclonal antibodies to the receptor activator of nuclear factor kappa-Β ligand and interleukin-6 have also been explored as a medical treatment for FD, resulting in reduction in bone pain, tumor growth, and bone turnover markers[10,11]. Most FD lesions require surgical management, mostly involving a conservative recontouring of the dysplastic bone to restore the normal bone shape. However, the need for re-surgery is high with this type of conservative surgical treatment. Reconstruction may be necessary for larger lesions[12]. The correction of concomitant malocclusion is also necessary, with the main focus on improving function and esthetics.
A thorough search revealed little mention of fibrous dysplasia in the orthodontic literature, and it is probably rarely seen in the typical orthodontic practice. There is limited information regarding protocols and precautions for orthodontic management of such lesions[13]. The case report follows and adheres to the CARE guidelines[14]. In the present article, we shall describe sequential dental and orthodontic management of malocclusion in a case of surgically treated FD of the maxilla.
A 19-year-old Indian female presented with a chief complaint of excessive display of gums when smiling.
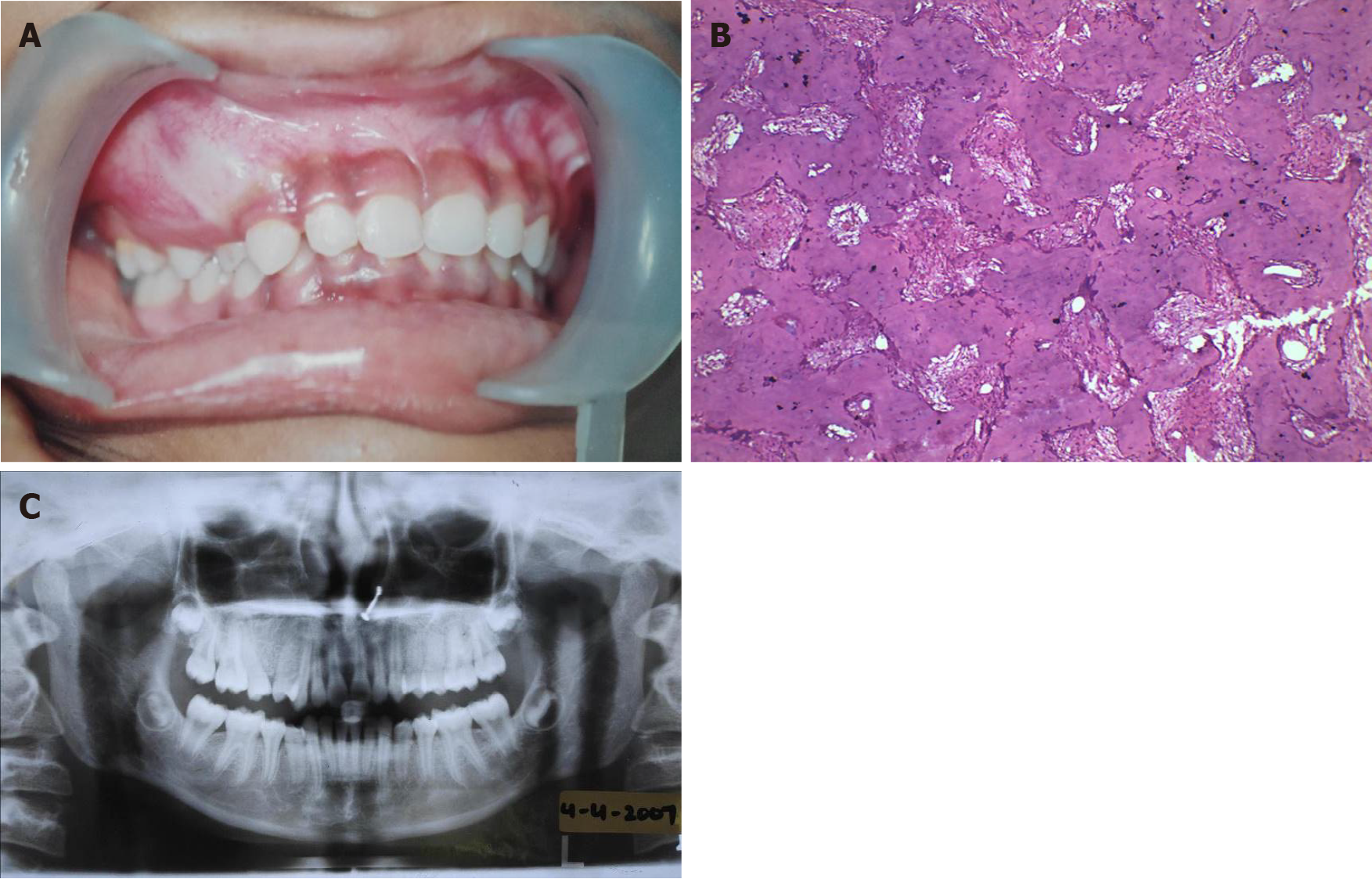
Dental history included a hard, non-tender swelling of gums around the upper right canine-premolar teeth, first noted at 15 years of age. Orthopantomogram (OPG) X-ray revealed a mixed radiolucent/radiopaque lesion with ground-glass appearance, blending into the adjacent normal bone. There was loss of lamina dura of the associated teeth. Biopsy revealed trabeculae of mature bone with osteocytes in lacunae and rimmed by osteoid. The connective tissue was cellular and vascular, suggestive of a hamartomatous fibro-osseous lesion. The case was thus diagnosed as FD of the maxillary right anterior segment (Figure 1).
There was no significant medical, family and psychosocial history.
There was no special personal and family history.
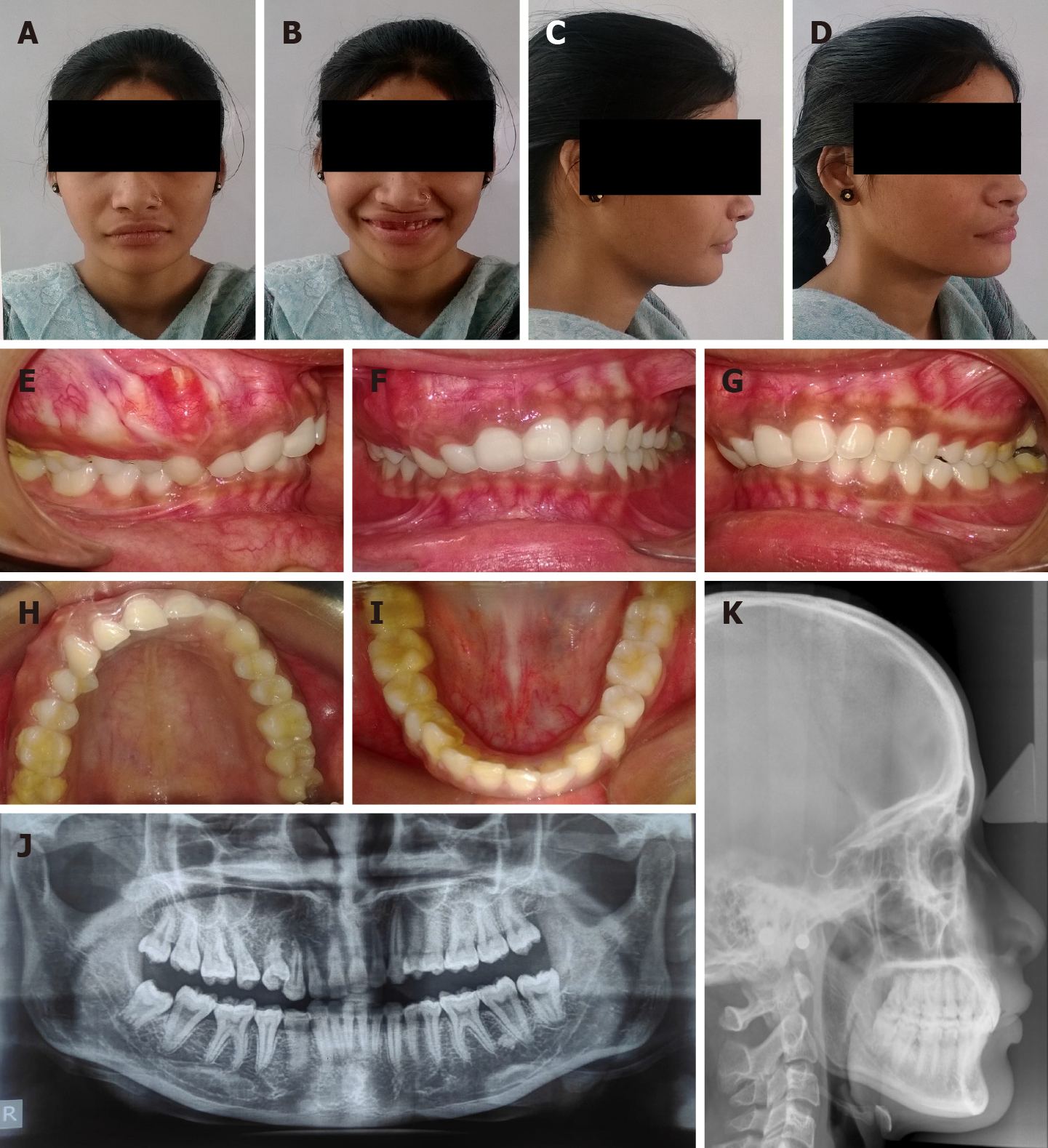
OPG X-ray revealed that the bone around the right maxillary canine-premolar teeth was less dense than in other areas, yet the bone pattern was regular. These findings suggested normal healing post-surgical resection. The lateral cephalometric analysis confirmed the aforementioned clinical diagnosis-Class II skeletal pattern, retrognathic mandible, retroclined maxillary anterior teeth and a normal growth pattern (Figure 2).
The patient presented with symmetrical mesoprosopic face, competent lips, everted upper lip on right side, mild class II skeletal pattern with retrusive mandible and deep mentolabial sulcus. On smiling, inadequate display of incisor teeth with excessive gingival display on the right side was noted (Figure 2). Photographic analysis revealed canting of the inter-commissural line with respect to the inter-pupillary line, indicating an altered lip posture secondary to dysplasia and its surgical treatment (Figures 2 and 3A). Also, the photographs revealed no tooth display in the affected quadrant when smiling (Figure 3C).
Intra-oral examination showed that the bony alveolus in the right maxillary canine-premolar region was markedly enlarged. The crowns of anterior maxillary teeth in this area were torqued lingually, with the root of the right maxillary canine (tooth #13) being exposed clinically. The maxillary anterior occlusal plane was canted towards the right side, resulting in asymmetric anterior arch form. Mandibular teeth were well aligned and upright on basal bone. Both left and right buccal segments had Class I occlusion.
In the first phase of treatment, surgical recontouring of the dysplastic area was performed was done by the oral surgeons. Four years after surgery, when the lesion was resolved and adequate bone healing was achieved, the case was referred for second phase treatment involving correction of the residual malocclusion and restoration of smile esthetics.
This phase involved a comprehensive orthodontic treatment and was commenced after thorough clinical and radiographic examination.
FD of the maxillary right anterior segment.
The treatment objectives included endodontic management of the clinically exposed root apex of right maxillary canine #13 (Federation Dentaire Internationale notation), followed by orthodontic correction of the following- the palatal root torque of teeth in the right maxillary anterior segment; the cant of the maxillary anterior occlusal plane towards the right side; the excessive gingival display on the right side; and the excess overbite. The radiographic findings suggested adequate healing of the lesion four years after surgery, therefore we decided to initiate tooth movement of the displaced teeth.
The treatment commenced with non-surgical endodontic treatment of the right maxillary canine #13, followed by apicoectomy of the clinically exposed root apex. Three months later, after confirming adequate healing, the orthodontic treatment was started using .022X.028" slot, conventional straight-wire mechanics. (Figure 4). Following alignment of the maxillary arch, .019X.025" stainless steel wire was placed with anterior differential palatal root torque (Figure 4A). Additional trans-palatal arch allowed cross-arch stabilization. After desired up righting of teeth was achieved, the remaining mandibular arch was bonded for alignment along with an asymmetric anterior intrusion in the upper arch using a unilateral intrusion arch made from .018" A.J. Wilcock archwire (Figure 4B). Then, a separate canine intrusion spring (again made from .018" A.J. Wilcock archwire) and continued asymmetric anterior intrusion were used to further correct the occlusal cant and anterior deep bite (Figure 4C). After adequate bite opening and levelling of the occlusal cant, post-intrusion finishing and detailing was done using .019X.025" stainless steel wire with artistic positioning bends (Figure 4D). OPG X-rays were taken periodically throughout the active tooth movement phase to monitor for any changes in bone morphology. The case was debonded after 41 mo of active treatment (Figure 5). A maxillary Essix retainer and mandibular bonded lingual retainer were placed to maintain the achieved dental corrections.
Periodic follow-ups were done every 6-mo for monitoring the stability of occlusion and any progression of the lesion. At the 3-year follow up, the patient's occlusion was stable and treatment results were well maintained without any signs and/or symptoms of an active lesion, despite discontinuing the maxillary retainer after two years (Figure 6).
FD is a type of bone disorder mostly involving craniofacial bones. Lesions are twice as common in the posterior maxilla as compared to the mandible[15]. Maxillary FD is associated with metabolic dysfunction and disordered bone architecture, which in turn affects tooth development and eruption.
The most common dental anomalies associated with FD include tooth rotation, oligodontia, displacement, enamel hypoplasia, enamel hypomineralization, impacted teeth and/or severe malocclusion[16]. The patient in the current report presented for esthetic reasons with excessive gingival display and malocclusion following surgically corrected/recontoured FD of the right maxilla in the canine-premolar area. The lesion resulted in crowding, rotations and displacement of teeth in the same quadrant, along with excessive palatal crown torque/buccal root torque of teeth, exposed root of the right maxillary canine tooth #13 and a canted occlusion plane. Deposition of dysplastic bone caused expansion of the buccal cortical plate, and surgical recontouring of the lesion caused exposure of the maxillary right canine root apex. It was treated by root canal treatment and apicoectomy. Our ultimate goal was to correct malocclusion by movement of teeth in the affected area.
FD in the craniofacial skeleton and related structures results in significant dysmorphic features like facial asymmetry and deformity. In the present case, characteristic features of FD were apparent on pre-surgical panoramic radiographs, described as a mixed radiolucent/radiopaque lesion with ground glass appearance[1-4]. Few articles have reported adequate healing of fibro-dysplastic bone following orthognathic surgery[17,18]. There is also very limited information regarding orthodontic tooth movement in dysplastic bone, and the long-term prognosis of such treatment. A case report describing orthodontic repositioning of an impacted cuspid in fibro-dysplastic maxillary bone of a 12-year-old girl suggests a normal response of dysplastic bone to orthodontic forces[19]. Lee et al[3] and Akintoye et al[20] suggest delaying orthodontic therapy until after the age of skeletal maturity, based on the individual patient’s needs and findings from an initial orthodontic evaluation. The advantage of such delay is that FD disease activity tends to decrease after skeletal maturity, which is reflected in a decline in bone turnover markers, a decrease in the number of mutated skeletal stem/progenitor cells, and a tendency of FD histology to improve over time[21]. Orthodontic treatment for the patient in the current report was initiated after completion of the pubertal growth spurt. Furthermore, four years post-surgery, there were no signs and/or symptoms of an active lesion. The OPG X-ray revealed less osseous density but predominantly regular woven bone in the area of the lesion, indicative of successful healing.
A position correlation between increase in c-fos gene and FD was described by Marie et al[22]. Increase in c-fos gene has been related to post-traumatic FD in a couple of case reports[23,24]. Therefore, to avoid the risk of transforming a quiescent lesion into an aggressively growing lesion, we planned to proceed with sequential orthodontic tooth movement, using light forces, without applying any direct forces to the bone (through micro-implants) and to monitor the lesion periodically. There were no signs of reactivation of the FD lesion during the active orthodontic treatment period of 41 mo, as evident on post-operative photographs and radiographs (Figure 5), which may be attributed to the following special precautions taken in this case: Delaying orthodontic treatment until adequate healing of the surgically treated bone was confirmed, as well as skeletal maturity was attained[21]; Sequential orthodontic mechanics: Initial torquing and up righting of the teeth was followed by segmental intrusion of anterior teeth to correct the cant of the occlusal plane; Use of light forces: To correct the anterior cant of the occlusal plane, a unilateral cantilever intrusion arch was used for unilateral intrusion of the right maxillary incisors. The forces were kept light, below 20gms, and 0.018" A.J Wilcock wire was used instead of conventional 0.017X0.25" TMA wires. Additionally, we did a separate intrusion for the right maxillary canine; Avoid direct forces to the healed bone: We avoided using micro-implants for supported intrusion, to prevent any immediate trigger for reactivation of the lesion.
The total duration of active treatment was 41 mo. This is in accordance with previous studies showing that orthodontic treatment duration is increased in FD cases[3,20]. Using light forces over longer duration also minimizes the possibility of relapse after orthodontic treatment. There is limited data on long-term outcomes of orthodontic treatment and the effectiveness of retention in FD cases[3,13]. Therefore, we proposed long-term retention in the present case. Maxillary Essix retainer and mandibular bonded lingual retainer were given to maintain the achieved dental corrections. Periodic follow-ups were done every 6-mo. The 3-year follow-up records showed relatively stable occlusion and minimal relapse, despite discontinuing the maxillary retainer after two years. However, the authors believe that results from this case report may not be applicable to all patients with FD and further characterization of orthodontic management should be decided by more precise, prospective clinical studies.
In this report, FD of the maxilla was successfully treated with surgical recontouring and orthodontic treatment. The goal of orthodontic treatment in FD affecting the maxillary region is to focus on improving function and esthetics, while avoiding reactivation of the quiescent/healed lesion. Adequate healing of fibro-dysplastic bone post-surgery must be allowed before commencement of orthodontic tooth movement, as inferred from a good outcome in this case. Special precautions must be taken, such as sequential orthodontic tooth movement, use of lighter forces and avoidance of direct orthodontic forces to the latent bone. Periodic follow-ups are necessary to monitor the stability of occlusion and any relapse of the lesion.
We acknowledge the patient and her parents for providing us with consent to perform the treatment, being cooperative throughout the treatment and follow-ups, and giving us permission to submit and publish the records for this article. We also acknowledge Dr. Verma P (DDS, MS, FAGD, Diplomate, American Board of Endodontics) for the prompt professional guidance and expertise to polish the manuscript further.
Provenance and peer review: Invited article; Externally peer reviewed.
Specialty type: Oncology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kaku M S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
| 1. | Costanzi MA, Velasco e Cruz AA. Envolvimento orbitário difuso por dysplasia fibrosa na síndrome de McCune Albright: Relato de caso. Arq Bras Oftalmol. 2007;70:1021-1023. |
| 2. | Neville BW, Damm DD, Allen CW, Bouquot JR. Patologia Oral & Maxilofacial. 2nd ed. Rio de Janeiro: Guanabara Koogan, 2004. |
| 3. | Lee JS, FitzGibbon EJ, Chen YR, Kim HJ, Lustig LR, Akintoye SO, Collins MT, Kaban LB. Clinical guidelines for the management of craniofacial fibrous dysplasia. Orphanet J Rare Dis. 2012;7 Suppl 1:S2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 166] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 4. | MacDonald-Jankowski D. Fibrous dysplasia: a systematic review. Dentomaxillofac Radiol. 2009;38:196-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Mansilla-Lory J, Amezcua-Guerra LM, Vargas-Rodríguez A, Fernández-Tapia S, Leboreiro I, Resnick D, Martínez-Lavín M, Villanueva M, Gaytan E, Pineda C. Leontiasis ossea: a paleopathologic case report. J Clin Rheumatol. 2007;13:269-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Akintoye SO, Boyce AM, Collins MT. Dental perspectives in fibrous dysplasia and McCune-Albright syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e149-e155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Burke AB, Collins MT, Boyce AM. Fibrous dysplasia of bone: craniofacial and dental implications. Oral Dis. 2017;23:697-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 89] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 8. | Unal Erzurumlu Z, Celenk P, Bulut E, Barıs YS. CT Imaging of Craniofacial Fibrous Dysplasia. Case Rep Dent. 2015;2015:134123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Plotkin H, Rauch F, Zeitlin L, Munns C, Travers R, Glorieux FH. Effect of pamidronate treatment in children with polyostotic fibrous dysplasia of bone. J Clin Endocrinol Metab. 2003;88:4569-4575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 117] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Boyce AM, Chong WH, Yao J, Gafni RI, Kelly MH, Chamberlain CE, Bassim C, Cherman N, Ellsworth M, Kasa-Vubu JZ, Farley FA, Molinolo AA, Bhattacharyya N, Collins MT. Denosumab treatment for fibrous dysplasia. J Bone Miner Res. 2012;27:1462-1470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 171] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 11. | de Boysson H, Johnson A, Hablani N, Hajlaoui W, Auzary C, Geffray L. Tocilizumab in the treatment of a polyostotic variant of fibrous dysplasia of bone. Rheumatology (Oxford). 2015;54:1747-1749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Zeng HF, Lu JJ, Teng L, Jin XL, Xu JJ, Zhang C, Xu MB, Xie F, Tian T, Xu R, Wu HH. Surgical treatment of craniomaxillofacial fibrous dysplasia: functionally or aesthetically? J Craniofac Surg. 2013;24:758-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Subramani K, Lee V, Krisko A, Huja S. Orthodontic treatment of patient with maxillofacial fibrous dysplasia: A case report. J Clin Exp Dent. 2019;11:e296-e302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, Kiene H, Helfand M, Altman DG, Sox H, Werthmann PG, Moher D, Rison RA, Shamseer L, Koch CA, Sun GH, Hanaway P, Sudak NL, Kaszkin-Bettag M, Carpenter JE, Gagnier JJ. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 741] [Cited by in RCA: 1014] [Article Influence: 126.8] [Reference Citation Analysis (0)] |
| 15. | Menon S, Venkatswamy S, Ramu V, Banu K, Ehtaih S, Kashyap VM. Craniofacial fibrous dysplasia: Surgery and literature review. Ann Maxillofac Surg. 2013;3:66-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Catena DL, Glick GL. Monostotic fibrous dysplasia with dental anomalies. Report of a case. Oral Surg Oral Med Oral Pathol. 1971;32:136-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (1)] |
| 17. | Samman N, Piette E, Cheung LK, Tideman H. Feasibility of osteotomies in fibrous dysplasia of the jaws. Int J Oral Maxillofac Surg. 1991;20:353-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Yeow VK, Chen YR. Orthognathic surgery in craniomaxillofacial fibrous dysplasia. J Craniofac Surg. 1999;10:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Colella G, Itro A, Perillo L, Cannavale R. Orthodontic movement of impacted cuspid in fibrodysplastic bone: a case report. Bone. 2010;46:248-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Akintoye SO, Lee JS, Feimster T, Booher S, Brahim J, Kingman A, Riminucci M, Robey PG, Collins MT. Dental characteristics of fibrous dysplasia and McCune-Albright syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:275-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 56] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Davies ML, Macpherson P. Fibrous dysplasia of the skull: disease activity in relation to age. Br J Radiol. 1991;64:576-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Marie PJ, de Pollak C, Chanson P, Lomri A. Increased proliferation of osteoblastic cells expressing the activating Gs alpha mutation in monostotic and polyostotic fibrous dysplasia. Am J Pathol. 1997;150:1059-1069. [PubMed] |
| 23. | Tomiyama A, Aoki K, Nakayama H, Izukura H, Kimura H, Harashina J, Ito K, Hayashi M, Saito N, Sakurai T, Oharaseki T, Terada H, Iwabuchi S. Posttraumatic cranial cystic fibrous dysplasia. Case Rep Med. 2011;2011:680401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Umerani MS, Bakhshi SK, Abbas A, Sharif S, Arshad S. Post-traumatic fibrous dysplasia of the parietal bone: A rare entity. Asian J Neurosurg. 2017;12:547-550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |