Published online Nov 6, 2021. doi: 10.12998/wjcc.v9.i31.9686
Peer-review started: June 28, 2021
First decision: July 26, 2021
Revised: July 27, 2021
Accepted: September 19, 2021
Article in press: September 19, 2021
Published online: November 6, 2021
Processing time: 123 Days and 5.6 Hours
Only a few cases of giant pseudomeningoceles have been reported in the literature. Herein, we report a giant pseudomeningocele of the cervical spine that was found after cervical laminectomy for an epidural hematoma following epidural blockade.
A 47-year-old man presented with recurrent neck pain and posterior neck swelling after spinal surgery. Magnetic resonance imaging of the cervical spine revealed fluid collection (5.6 cm × 6.6 cm × 11.2 cm) at the C3-6 level; this proved to be a pseudomeningocele. Symptoms related to the pseudomeningocele resolved following dural repair and fat graft transplantation.
Although rare, pseudomeningocele is a possibility in patients with recurrent back pain, radicular pain, or a persistent headache following spinal surgery. Continuous attention should be paid throughout the spinal procedure, whether conservative or non-conservative.
Core Tip: Only a few cases of giant pseudomeningoceles have been reported in the literature. Here we present a rare case of a giant pseudomeningocele of the cervical spine identified after cervical laminectomy for an epidural hematoma after epidural blockade. The patient presented with recurrent neck pain and posterior neck swelling after spinal surgery. Magnetic resonance imaging of the cervical spine revealed fluid collection at the C3-6 level that proved to be a pseudomeningocele. This case highlights that, despite its rarity, giant pseudomeningocele must be taken in consideration in patients who report recurrent back pain, radicular pain, or a persistent headache after spinal surgery.
- Citation: Kim KW, Cho JH. Iatrogenic giant pseudomeningocele of the cervical spine: A case report. World J Clin Cases 2021; 9(31): 9686-9690
- URL: https://www.wjgnet.com/2307-8960/full/v9/i31/9686.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i31.9686
A pseudomeningocele forms when the dura is torn and the leptomeninges and subarachnoid space protrude through the dural defect[1]. Three types of pseudomeningocele (congenital, iatrogenic, and traumatic) have been reported[2,3]. An iatrogenic pseudomeningocele usually occurs as a postoperative complication following lumbar spinal laminectomy[4]. Giant pseudomeningoceles have rarely been reported[2,5,6]. Only a few cases of giant cervical pseudomeningoceles have been reported in the literature, and most were associated with brachial plexus injury[5,6].
The current report describes a 47-year-old man with a giant pseudomeningocele after cervical laminectomy for an epidural hematoma following epidural block. To our knowledge, no cases of iatrogenic giant pseudomeningoceles of the cervical spine have been reported. In the current case, in which a large dead space existed in the pseudomeningocele, a dural repair, local epidural fat graft transplantation, and additional abdominal subcutaneous vascularized fat graft transplantation successfully closed the dead space.
A 47-year-old man was admitted for pain in the left posterior nuchal and shoulder regions and left-sided weakness and numbness.
Three hours prior to admission, he had received a cervical epidural block for head and neck pain. One hour after this block, he felt severe neck pain followed by left-sided weakness.
The patient had diabetes and had recently received medication (Amaryl M 2/500 mg). He had experienced a traffic accident six months prior to admission and since then had taken intermittent conservative treatments for persistent head and neck pain from another local hospital. The patient reported that he did not undergo magnetic resonance imaging (MRI) and that X-ray scanning had revealed no significant abnormalities.
The patient had a free personal and family history.
Upon admission, a neurological examination revealed global weakness on the left side (hand grasping (V/II), elbow extension (V/III), elbow flexion (V/III), knee flexion (V/III), knee extension (V/III), hip flexion (V/III), and hip extension (V/III)). Sensory testing revealed painful numbness (allodynia) on the lateral side of the left upper arm. The anal sphincter tone was intact.
Laboratory findings were normal.
Emergency MRI revealed an epidural hemorrhage at the C2-T6 level causing central spinal canal stenosis and cord compression at the C3-T1 level (Figure 1).
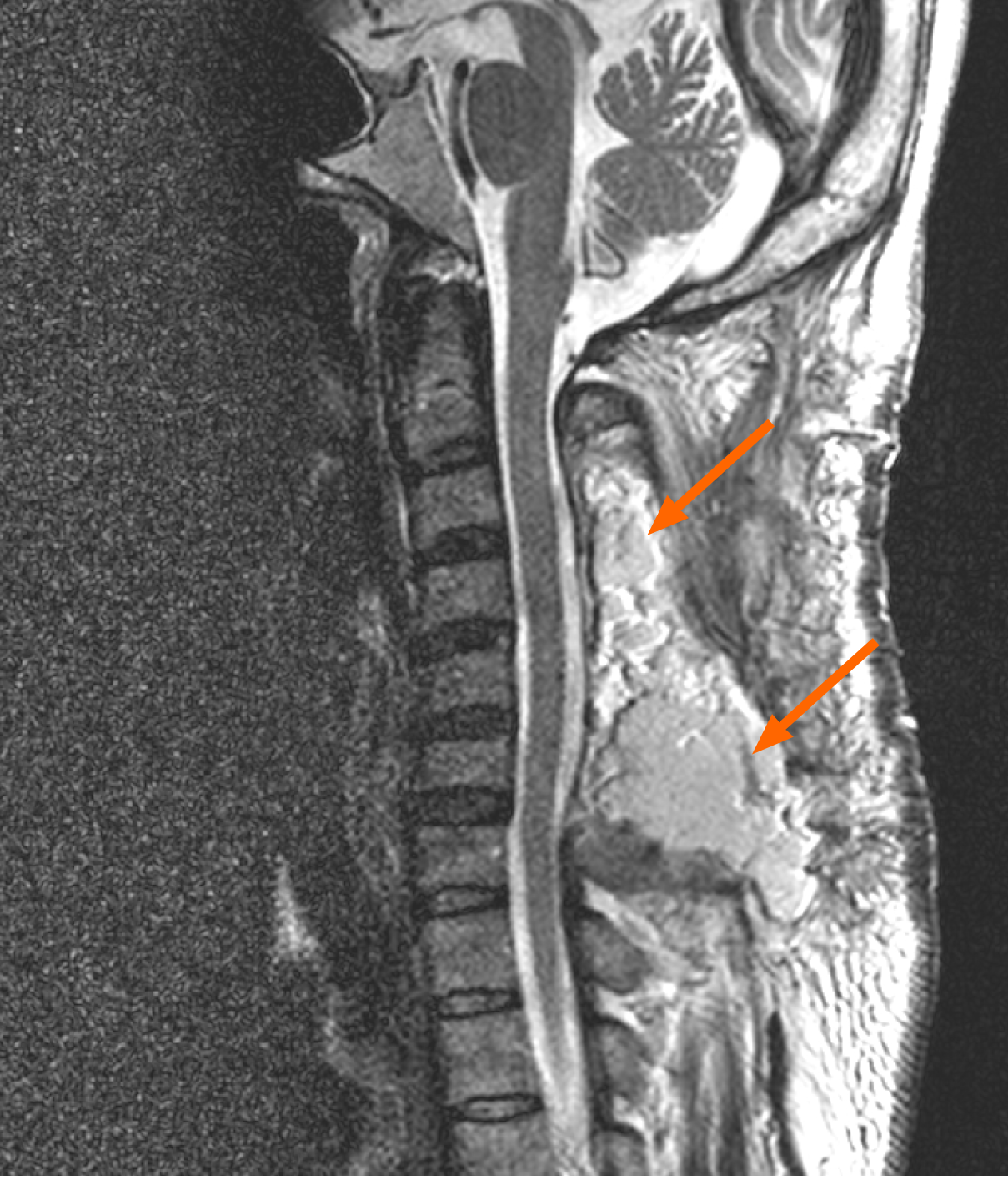
Following the diagnosis of a cervical epidural hematoma, the patient was transferred to the Neurosurgery Department for continued care. A total C3-6 laminectomy with a partial laminectomy at the C2 level (dome-like enlargement) and the upper lamina at the C7 level, with hematoma removal and lateral mass screw fixation at C3-6, as well as posterior fusion were performed. Postoperatively, neurologic recovery was initially observed, but five days later, the patient’s neck pain worsened severely. Continuous oozing was seen at the hemovac removal site and swelling was observed in the posterior nuchal area. A follow-up MRI demonstrated fluid collection (5.6 cm × 6.6 cm × 11.2 cm) at the posterior operative site at the C3-6 level (Figure 2).
The final diagnosis of the presented case was a giant pseudomeningocele of the cervical spine identified after cervical laminectomy for an epidural hematoma following epidural blockade.
As severe neck pain aggravated by the Valsalva maneuver was sustained, the decision was made to proceed with surgery. Intraoperatively, a 3-4 mm dural opening was observed at the left C5-6 laminectomy site from which cerebrospinal fluid (CSF) was leaking. The dural opening was closed with local fat graft transplantation, and an abdominal subcutaneous vascularized fat graft transplantation was used to close the large dead space. Thereafter, no active CSF leakage was observed.
Postoperatively, the patient’s neck pain resolved, and he was ambulatory and able to return to work at the time of discharge. No significant fluid collection or posterior epidural hematoma, observed on the previous MRI, was found (Figure 3).
In the current report, we described a giant pseudomeningocele of the cervical spine following cervical laminectomy for an epidural hematoma following an epidural block. The surgical dural repair of the pseudomeningocele was successful without any recurrence in clinical symptoms or radiologic abnormalities.
A pseudomeningocele is an abnormal extradural collection of CSF in the soft tissue of the back that occurs due to a dural tear[2,7]. Three types of pseudomeningoceles (congenital, iatrogenic, and traumatic) were reported by Miller et al[3] in 1968. The pseudomeningocele in the current case had two possible pathogeneses. The first is iatrogenic dural micropuncture during the cervical block. It is essential to ensure the integrity of the dura to prevent leaks regardless of spinal level. However, the surgeon may not have noticed a fine dural tear during the operation, which may have led to pseudomeningocele formation. The second is that a pseudomeningocele may have resulted from a dural tear that went unnoticed during the laminectomy and may have been left open during the surgical procedure. Either possibility could be categorized as an iatrogenic pseudomeningocele, which stresses the importance of suitably training spine surgeons to appropriately handle intraoperative CSF leaks.
In the current case, the patient’s posterior neck muscles were thin due to persistent neck pain after the whiplash injury. Secondarily, the surgeons used additional abdominal vascularized fat graft transplantation to close the large amount of dead space, a common plastic surgery technique. However, this technique may be controversial, and comparisons between treatment options should be performed in future studies.
Continuous attention should be paid throughout spinal treatment procedures, whether conservative or non-conservative in nature, and pseudomeningoceles should be considered the causative etiology for patients with recurrent back and neck pain, radicular pain, or a persistent headache after spinal surgery.
Herein, we presented a rare case of giant pseudomeningocele at the cervical level after cervical laminectomy for an epidural hematoma following an epidural block that was successfully repaired with a local fat graft and additional abdominal vascularized fat transplantation. Our findings suggest that pseudomeningoceles should be carefully considered a reason for recurrent back and neck pain following spinal surgery.
We would like to appreciate our patient for consenting to have his case presented and published.
Manuscript source: Unsolicited manuscript
Specialty type: Clinical neurology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dye DC S-Editor: Wu YXJ L-Editor: A P-Editor: Xing YX
| 1. | Agrawal D, Mishra S. Post-traumatic intradiploic pseudomeningocele. Indian Pediatr. 2010;47:271-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Weng YJ, Cheng CC, Li YY, Huang TJ, Hsu RW. Management of giant pseudomeningoceles after spinal surgery. BMC Musculoskelet Disord. 2010;11:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Miller PR, Elder FW Jr. Meningeal pseudocysts (meningocele spurius) following laminectomy. Report of ten cases. J Bone Joint Surg Am. 1968;50:268-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 65] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Lee KS, Hardy IM 2nd. Postlaminectomy lumbar pseudomeningocele: report of four cases. Neurosurgery. 1992;30:111-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Hader WJ, Fairholm D. Giant intraspinal pseudomeningoceles cause delayed neurological dysfunction after brachial plexus injury: report of three cases. Neurosurgery. 2000;46:1245-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Kotani Y, Abumi K, Ito M, Terae S, Hisada Y, Minami A. Neurological recovery after surgical treatment of giant cervical pseudomeningoceles extending to lumbar spine associated with previous brachial plexus injury. Eur Spine J. 2010;19 Suppl 2:S206-S210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Pau A. Postoperative "meningocele spurius." Report of two cases. J Neurosurg Sci. 1974;18:150-152. [PubMed] |