Published online Nov 6, 2021. doi: 10.12998/wjcc.v9.i31.9635
Peer-review started: May 11, 2021
First decision: August 18, 2021
Revised: August 24, 2021
Accepted: September 26, 2021
Article in press: September 26, 2021
Published online: November 6, 2021
Processing time: 170 Days and 21.8 Hours
Thread rhinoplasty can trigger a reaction to thread material, which is a foreign body. We compared clinical features induced by absorbable and non-absorbable threads following thread rhinoplasty.
Two patients who underwent different thread materials showed different clinical courses and different Hounsfield unit (HU) values in computed tomography. Patients with absorbable thread showed high HU values similar to a metallic material, and the HU value of inflammation was similar to vascular tissues with a lot of water (250). In the intraoperative field, absorbable thread materials and micro-abscesses were observed. In contrast, in the case of a non-absorbable thread, an object presumed to be thread was seen on the computed tomography (CT), and the HU value of inflammatory tissues was less than 100. In both patients, post-operative HU decreased to less than 100 and the clinical course improved. In both cases, histopathologic findings revealed foreign body granuloma associated with inflammation.
Absorbable threads were more aggressive and are more easily detected on CT.
Core Tip: In this study, we observed that different clinical features appeared according to the physical difference of thread material used in thread rhinoplasty. The difference in Hounsfield unit (HU) values on computed tomography was confirmed and objectively verified. Because of their hydrophilicity in the absorbable thread, they showed more severe inflammatory results and higher HU values. It will be very helpful in treatment if this is used for patients who show complication after thread rhinoplasty in the future.
- Citation: Lee DW, Ryu H, Jang SH, Kim JH. Clinical features and literature review related to the material differences in thread rhinoplasty: Two case reports. World J Clin Cases 2021; 9(31): 9635-9644
- URL: https://www.wjgnet.com/2307-8960/full/v9/i31/9635.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i31.9635
Minimally invasive procedures for plastic surgery have become more popular, and rhinoplasty is no exception. There is increasing interest in thread rhinoplasty that is simpler and requires less surgical time than incisional rhinoplasty. Threads are divided into those using absorbable components and those using non-absorbable polypropylene components. Polydioxanone (PDO) is an absorbable material that has been increasingly used for face thread lifting. Lerwick first reported the efficacy and safety of PDO thread lifting in 1983 and the formation of fibrous encapsulation tissue around the PDO thread were detected histopathologically[1]. In oriental traditional medicine, in recent years, the procedure of thread embedding acupuncture called “maesun” in Korean was performed indiscriminately to remove facial wrinkles, correct laxity, and even facilitate rhinoplasty[2]. However, the indiscriminate “maesun” thread treatment by untrained oriental medical practitioners was associated with multiple complications such as permanent scarring, extrusion of thread, infection, and thread malposition. In severe cases, complications such as alopecia, facial asymmetry, and parotid gland injury may also occur[3]. The risk of complications increases with the increase in the number of threads[4]. The use of PDO thread in oriental traditional medicine entails the insertion of 20-40 threads from the nasal tip to the dorsum and from the tip to the columella for nasal tip projection and dorsal augmentation. In Korea, approximately 30% of patients who underwent thread acupuncture at an oriental medicine clinic complained of side effects such as cosmetic dissatisfaction or soft tissue infection[5]. Despite the complications related to PDO thread, non-absorbable threads are extremely rare cases of thread-related complications. Therefore, we compared different clinical features associated with the use of absorbable and non-absorbable threads.
Hounsfield unit (HU) density is the basic principle in implementing computed tomography (CT). All substances have unique HU values, and it is useful to compare HU for lesions with similar gross findings on CT[6]. This study was also conducted to demonstrate the advantage of HU for the comparison of inflammation associated with two different threads by evaluating the difference in HU values of absorbable and non-absorbable threads.
The CT scans wound bacterial culture tests and laboratory examinations of the blood such as white blood cell count and high-sensitivity C-reactive protein (hs-CRP) were performed in two patients who showed skin perforation after thread rhinoplasty. All treatments were performed by the same plastic surgeon. The contrast-enhanced, high-resolution, multi-slice CT examination (GE Medical System, Milwaukee, WI) was performed before and after surgery to compare changes in HU values. The HU was measured at the suspected inflammatory tissue. The size of the region of interest was 1.2 mm2 or approximately the size of a slightly larger ballpoint pen size. All HU measurements were performed by two different physicians who were blinded to the patients' data at the same CT setting status. In addition, the HU values of three axial slices (1 slice that contained the suspected lesion, and an adjacent upper and lower slice) at a distance of 3 mm intervals were measured, and the lowest measured HU was used for analysis.
Case 1: A 63-year-old woman was admitted with a perforating skin defect of the nasal dorsum.
Case 2: A 31-year-old man was visited our hospital with a perforating skin defect of the nasal tip.
Case 1: She continued swelling and induration of nasal dorsum for several months and developed a perforated skin defect of nasal dorsum 1 mo ago.
Case 2: He presented swelling with induration, not a palpable nodule or mass-like lesion on the nasal tip one month before the formation of the abscess, and was treated according to cellulitis, but did not improve and developed into abscess formation.
Case 1: She underwent PDO (absorbable) thread rhinoplasty at an oriental traditional medicine clinic 4 mo before the outpatient visit. The patient explained that nearly 10 threads were injected at the nasal dorsum. There was no other medical or trauma history related to wound formation.
Case 2: He underwent rhinoplasty with polypropylene non-absorbable threads at another plastic surgery clinic ten years ago. He also had no medical past history or trauma history related to skin defect.
Case 1: No one in the family had a medical or traumatic history associated with wound formations.
Case 2: His family also had no significant medical past history or trauma history of abscess formation.
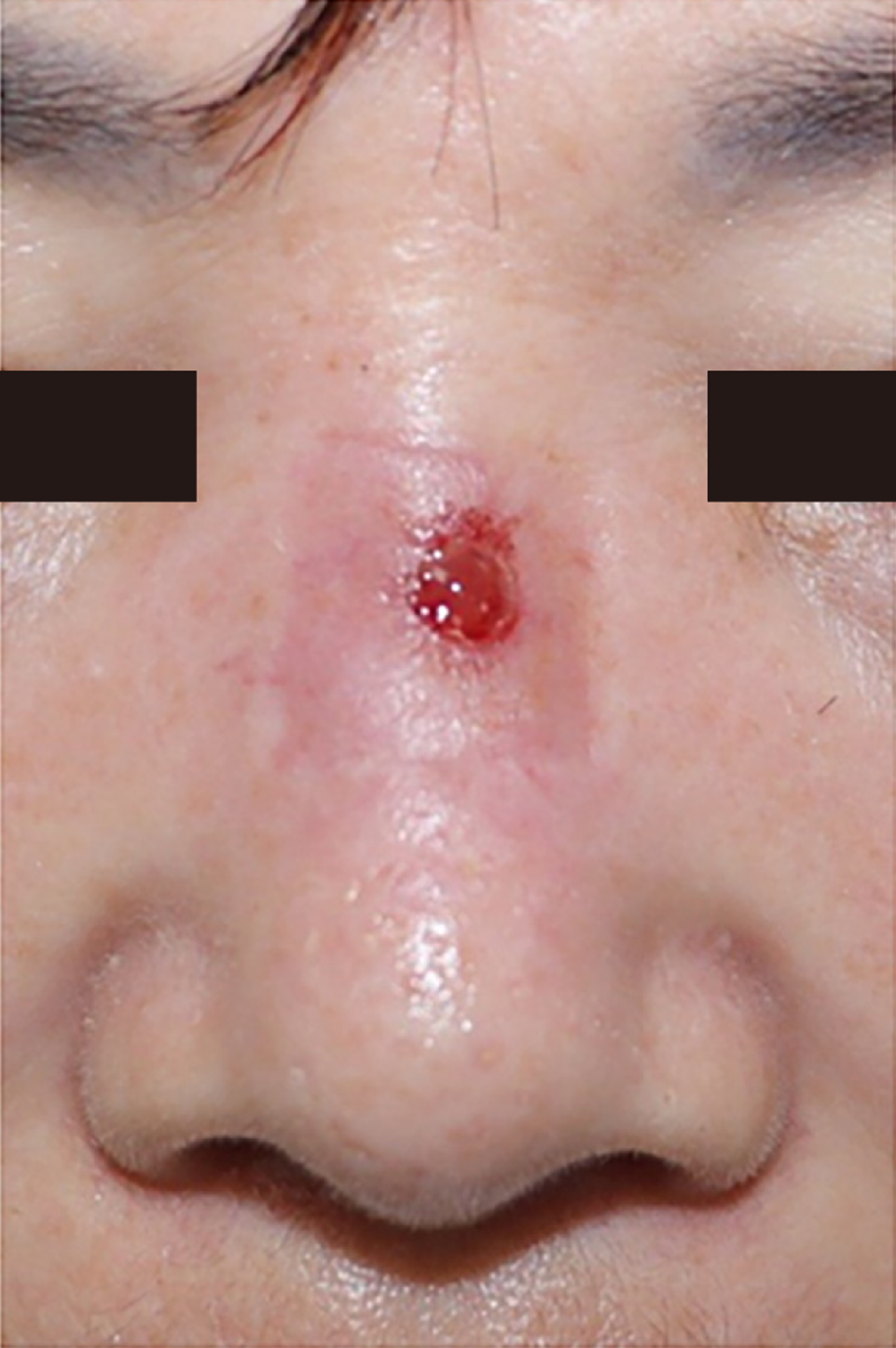
Case 1: Erythema and pus drainage through the nasal dorsal defect (Figure 1). She complained of induration and severe tenderness around the nasal dorsal skin defect.
Case 2: Overgranulation tissue accompanied by ulceration was observed on the nasal tip, and he complained of mild tenderness (Figure 2).
Case 1: The laboratory findings of whole blood count, serum electrolytes, liver function tests, and C-reactive protein were normal. Methicillin-sensitive Staphylococcus aureus was identified in the wound bacterial culture.
Case 2: He also showed no abnormal findings in laboratory findings, as did case 1. MSSA was also identified in the bacterial culture.
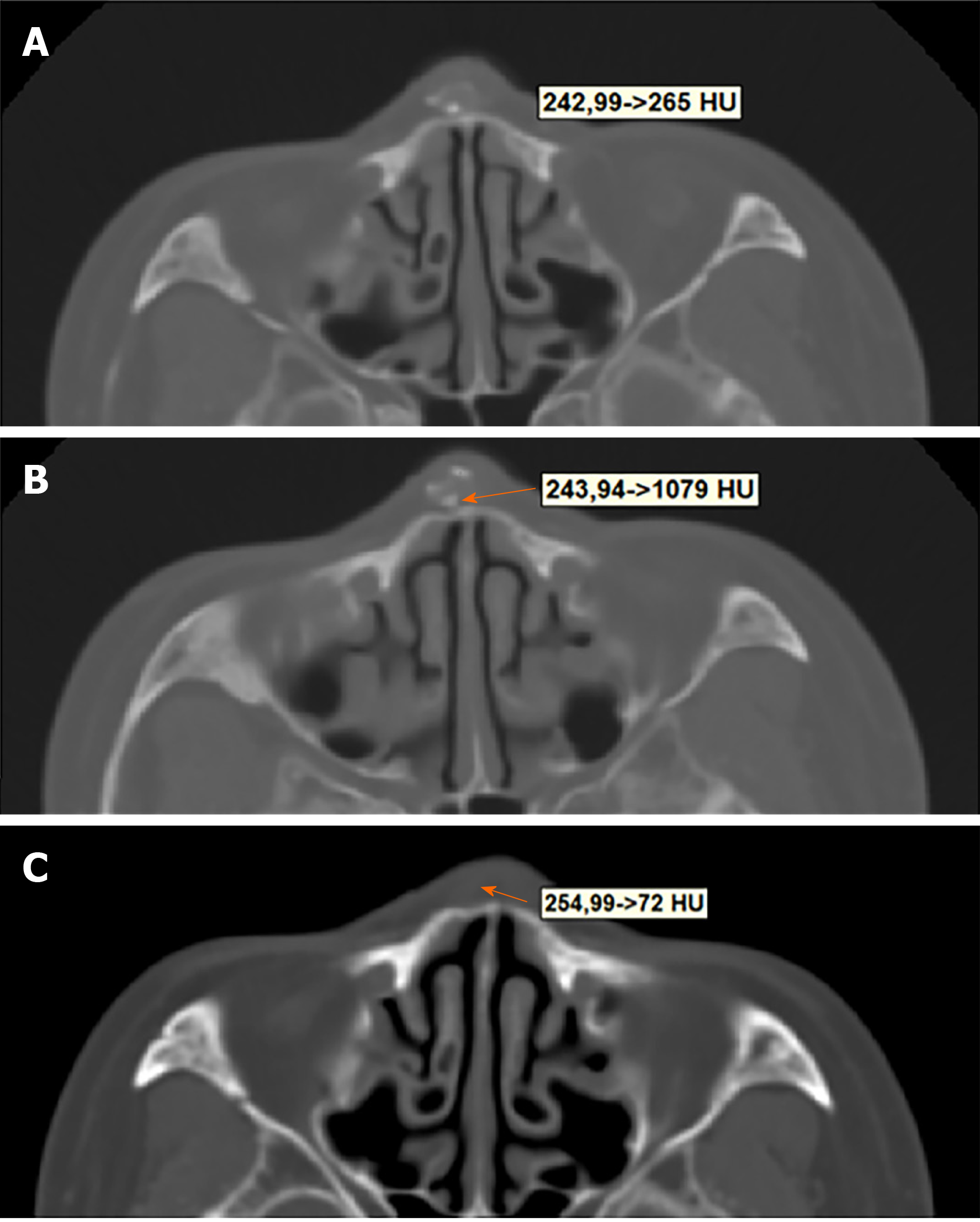
Case 1: The CT scan revealed a specific foreign body and surrounding inflammatory tissue. The HU of inflammatory tissue was approximately 250 in the post-contrast phase (Figure 3A). Additionally, fragmented PDO fragments similar to brightly calcified lesions were observed. The HU of the calcified lesion estimated as PDO was about 1000, which was similar to that of crystal or glass (Figure 3B).
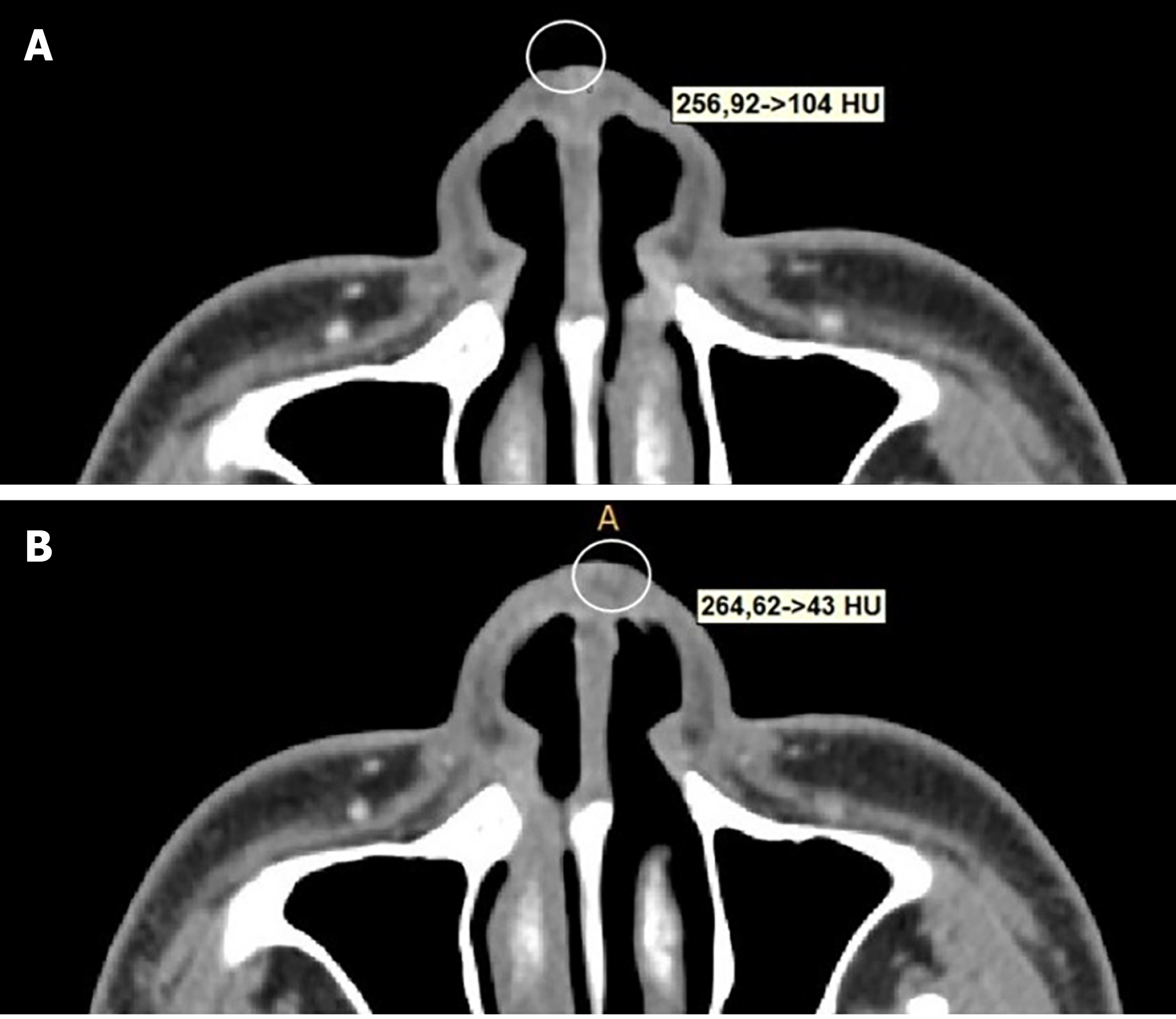
Case 2: CT scan revealed soft tissue swelling and inflammatory tissue enhanced in both alar areas. The HU value of inflammatory tissue was less than that of patient 1 by about 100, which is similar to that of normal soft tissue (Figure 4A). The HU of the foreign body (polypropylene thread) was about 140, which was also lower than in patient 1.
Cases 1 and 2: According to the clinical features and radiological findings, the patients were diagnosed with complications caused by a thread after rhinoplasty with necrosis in the skin and subcutaneous tissue.
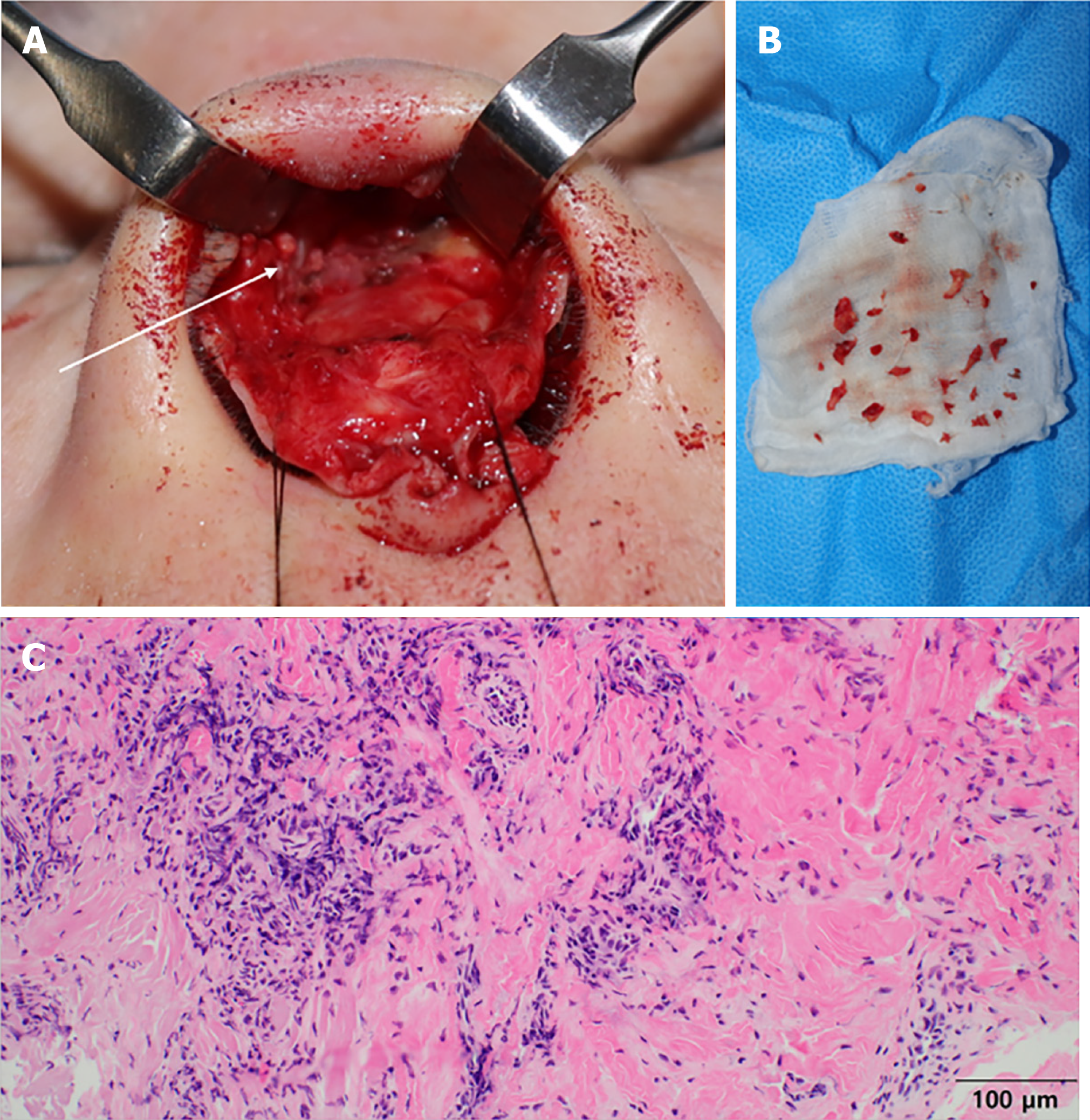
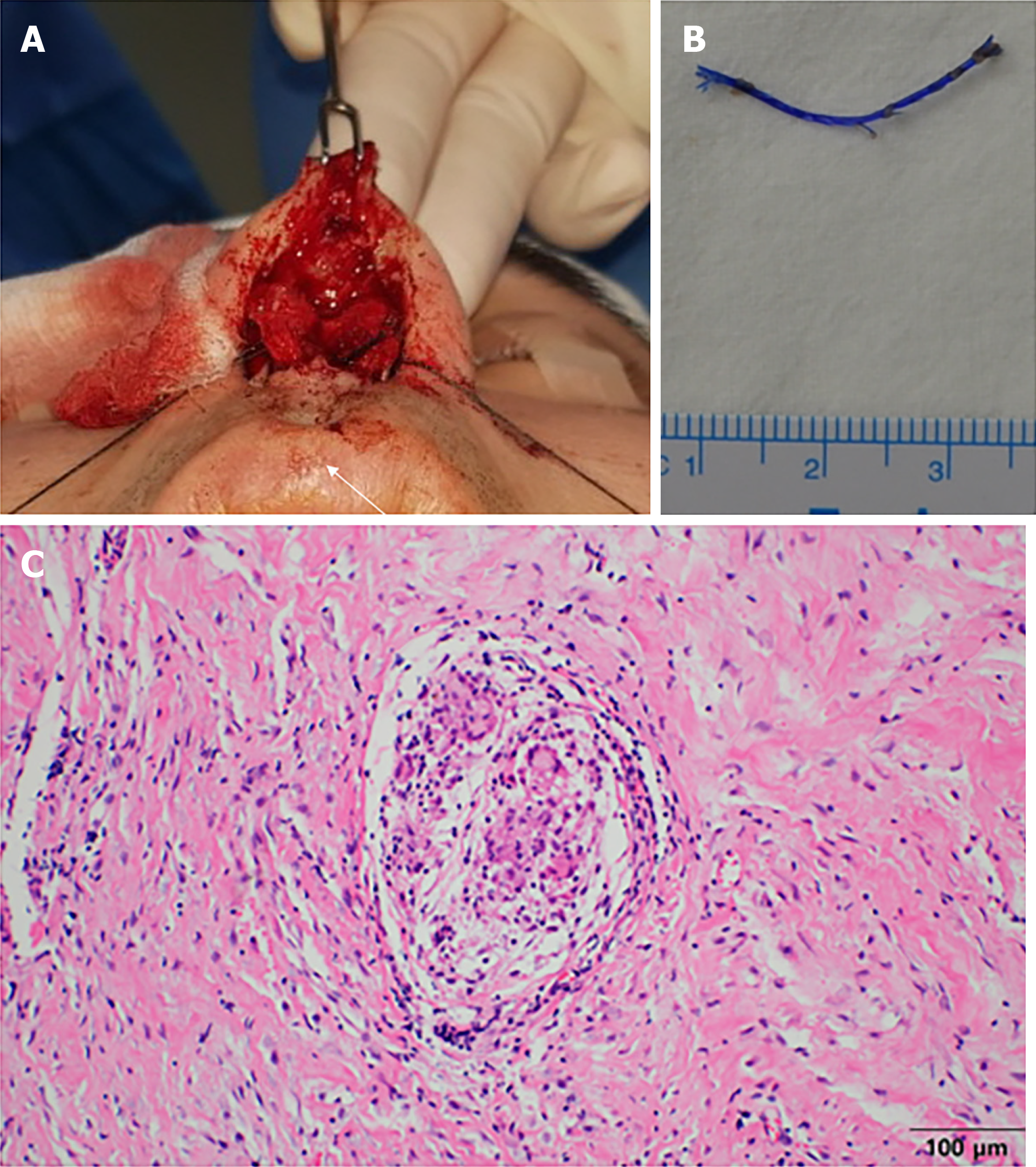
Case 1: Intraoperative findings, tissues carrying hard fibrous capsules, and overgranulation tissue was observed in the superficial musculoaponeurotic system layer. Multiple PDO fragments in the nasal dorsum area around the keystone area were observed, which barely adhered to the surrounding tissue and upper lateral cartilage (Figure 5A). The PDO was dissolved and decomposed into dozens of pieces (Figure 5B). Histopathological findings revealed severe, patchy inflammatory infiltrates of neutrophils, histiocytes, lymphocytes, and plasma cells, in the inflamed granulation tissue. Some foreign-body-type giant cells were noted in the fibrotic areas (Figure 5C).
Case 2: In operation, three polypropylene threads with a barbed pattern located between the medial crura of the lower lateral cartilage were removed (Figure 6A and B). No tissues such as infected granuloma were detected around the thread, and the tissues were relatively clean without debris. The histopathological reports of the skin showed moderate, patchy infiltrates of inflammatory cells including neutrophils and plasma cells interlacing the collagenous dermal stroma (Figure 6C).
Case 1: A follow-up CT scan was performed on a postoperative day (POD) 5. Under similar CT settings, the HU values of the inflammatory tissue at the nasal dorsal area decreased to 80, whereas the size of preoperative inflammatory tissue was decreased, and the PDO showing calcified change was also removed. HU around the PDO, which increased to 800 in the preoperative period, also decreased to about 80 following the removal of PDO (Figure 3C). During the postoperative follow-up period, she had persistent erythema in the nasal dorsum and a moderate contracted scar at the first monthly visit after the operation. The patient also complained of pain at the operation site. At 2 mo after the operation, inflammation such as erythema subsides. After that, the improvement of symptoms such as pain was expressed only after 3 mo, and after that, the treatment was finished after monthly follow-up for an additional 3 mo.
Case 2: Follow-up CT was performed on POD 8, and the HU value in the alar area was 40, which was not significantly different compared with preoperative CT (Figure 4B). In addition, compared with pre-surgical value, no foreign body was observed, and the soft tissue swelling in the alar area and the size of the inflammatory enhancing tissue were also reduced. During postoperative follow-up, he did not complain of pain in the nasal tip 1 mo after the operation, and the tip color also returned to normal. The characteristic comparison features of patients 1 and 2 are mentioned in Table 1.
| PDO thread | Prolene thread | ||
| Duration of symptom onset | 4 months | 10 yr | |
| Culture | MSSA | MSSA | |
| HU of Abscess | Preoperative | 250 | 100 |
| Postoperative | 50 | 40 | |
| HU of Foreign body | Preoperative | 1000 | 140 |
| Postoperative | 50-80 | No foreign body exists | |
| Histopathological findings | Severe, patchy inflammatory infiltrates of neutrophils | Moderate, patchy infiltrates of variable inflammatory cells | |
The injection of PDO thread acts as a powerful stimulant of collagen formation. The immediate effect of thread insertion is tissue lift due to the mechanical effect[3,7]. Yoon et al[7] reported that the PDO thread induces fibrous connective tissue formation, an increase in the number of nearby capillary vessels, and a reduction in the thickness of the fat layer due to fat cell denaturation. The PDO begins to disassemble after 3 mo of thread insertion and disappears by 6 mo[8]. Even after the loss of PDO, the collagen-inducing effect of PDO threads persisted for more than 10 mo[7].
In standard plastic surgery, usually, eight or fewer PDO threads act as tissue scaffolds, and the rest of the volume is supplemented with micronized fat graft or hyaluronic acid filler injections. Thread extrusion and asymmetry are the most frequent complications associated with this procedure when the operator is less experienced in standard plastic surgery. In contrast, in oriental traditional medicine, several 20-40 PDO threads are buried into the dermis of the fat layer for skin tightness and augmentation. No additional volume supplementation procedures such as filler injections or fat grafts are used, but only the number of PDO threads is increased to fill the insufficient volume. This procedure is very dangerous and increases the risk of infection and skin perforation. In standard plastic surgery, thorough sterile preparation is essential prior to invasive procedures, unlike oriental medicine. Kim et al also reported that there were too many threads, and the resulting repetitive inflammation with nasal mucosa pathogens was the cause of the increase in PDO thread infection in oriental medicine[4]. The other studies suggested that repetitive trauma and micro-movements between the barbs of the sutures and the surrounding capsule induce chronic inflammation in the soft tissues [9].
On the other hand, since polypropylene threads do not decompose, these side effects are less. Polypropylene thread is composed of isotactic crystal stereoisomers, a synthetic linear polyolefin. A review of the literature reveals fewer complications following rhinoplasty using non-absorbable thread compared with that of PDO. Teymoortash et al reported a case of skin abscess after polypropylene thread rhinoplasty, but the patient showed adverse cutaneous skin reaction to polypropylene, which is difficult to regard as a complication associated with non-absorbable thread rhinoplasty[10]. In our case of polypropylene thread, infection occurred 10 years after the polypropylene thread insertion, so it was initially difficult to attribute the infection to non-absorbable polypropylene thread. However, the lesion in patient 2 did not respond to various conservative treatments, and skin perforation was healed after the polypropylene thread was removed, suggesting that the wound was caused by the polypropylene thread.
There are several differences in the clinical progress of the two patients. In the PDO thread, symptoms such as skin perforation lasted shorter than polypropylene thread. In fact, the progress was faster. The clinical progression was also worse. Further, the CT of the PDO thread patient revealed a wider pocket. On the other hand, the polypropylene thread induced skin perforation much later than the PDO and alleviated inflammation via a rapid decrease in hs-CRP levels after the thread removal. The degree of post-operative contracture was also less severe. Histopathological findings comparing the severity of inflammatory reactions between the two patients revealed more severe, patchy inflammatory infiltrates of neutrophils in the inflamed granulation tissue associated with PDO thread. Overall, it can be seen that PDO shows a more severe inflammatory reaction.
Starting from a previously published review, we searched PubMed, Google Scholar, and Embase to collect all studies reporting complications. Table 2 summarizes the results found based on various searches. We extensively analyzed the overall literature related to thread rhinoplasty and only the complications associated with thread infection were investigated by the published studies. We excluded cases where the original article could not be searched, or where enough information was not available from reviews and analysis. Nine patients were selected and all the patients showed severe infections such as skin abscess. Eight of these patients developed an early phase within a few months due to PDO-related complications, and one patient with polypropylene developed in the late phase after 2 years. The lesions of all patients healed when the PDO thread was removed. Another patient with skin abscess caused by polypropylene thread showed symptom alleviation after thread removal. Similar to our study, other studies reported that PDO patients had a faster progression of infectious lesions.
| Authors | Journal | Sex | Age | Thread material | Location | Culture | Duration of symptom onset (mo) |
| KIM et al[5] | Aesth Plast Surg | M | 37 | PDO | Supratip | MRSA | 2 |
| - | - | M | 33 | PDO | Tip | Staphylococcusaureus | 6 |
| - | - | M | 27 | PDO | Tip | None | 7 |
| - | - | F | 29 | PDO | Supratip | None | 2.5 |
| - | - | F | 33 | PDO | Tip | None | 12 |
| - | - | F | 51 | PDO | Tip | None | 1 |
| - | - | F | 47 | PDO | Tip | Enterobacteraerogenes, | 2 |
| Teymoortash et al[10] | J Laryngol and Otol | F | 26 | Prolene | Tip | Strepto-cocci group C | 24 |
| Jaafar et al[11] | J Cosmetic Med | F | 45 | PDO | Tip | Propionibacterium acnes | 4 |
The HU is a fundamental parameter generated from CT. This is the original linear attenuation of the linear decay coefficient and is often used to analyze the density and water content distribution in biological tissues. HU decreases as the density decreases. The HU value of pure water is 0, and that of air is -1000, and that of metals in the body ranges from thousands to tens of thousands[12]. Therefore, HU measurements of inflammatory lesions and similar clinical features or findings on CT provide a more accurate differential diagnosis. Trojanowska et al[13] reported increased HU values associated with inflammatory tissues. In this study, a higher HU value of absorbable PDO threads revealed a severe clinical course, because the PDO thread generates more carbon dioxide and water during the decomposition and results in a more severe inflammatory reaction. The postoperative follow-up CT showed a greater decrease in HU in patients with PDO thread than in those carrying the polypropylene thread. In addition, the HU value associated with the PDO thread fragment was very high, about 800, which is attributed to the crystalline PDO material. The HU measurements facilitate distinguishing the severity of inflammatory lesions.
In this study, chronic inflammatory reactions were reported rarely compared to absorbable and non-absorbable threads, although the clinical characteristics (skin perforation and erythema) were similar, the measured values of HU showed many differences. And this study is the first study to reveal the relationship between thread characteristics and HU value.
This study has several limitations. The single patient with thread insertion was a statistical limitation for the analysis of different characteristics. In addition, no prospective studies were conducted and only retrospective studies were conducted, resulting in unwanted bias. In addition, polypropylene thread is different from PDO since the onset of complications occurs 10 years after thread insertion. Finally, there is a limitation in that it is not possible to accurately distinguish whether the clinical features of polypropylene thread complication, which are different from PDO threads, are due to the characteristics of the thread material itself or the characteristics of early or late complication.
In our study, the patients’ clinical course varied depending on the type of thread material. Compared with polypropylene thread, the PDO thread can cause severe infections such as abscess formation with an open wound and show a measure of higher HU values. Therefore, it is thought that the absorbable thread can cause more serious complications despite other limitations in the time of complications. The surgeons must be reminded that the procedure is associated with various early or late complications like as demonstrated in our studies. Therefore, identifying the thread material associated with specific complications can shorten the patient's clinical treatment.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bassetto F S-Editor: Wang LL L-Editor: A P-Editor: Yu HG
| 1. | Lerwick E. Studies on the efficacy and safety of polydioxanone monofilament absorbable suture. Surg Gynecol Obstet. 1983;156:51-55. [PubMed] |
| 2. | Yun YH, Leem JT, Ahn JH, Lee JH, Choi YY, Shin JM. A Case Report of facial wrinkles and folds improved by using the Thread Embedding Acupuncture (TEA). J Korean Med Ophthalmol Otolaryngol Dermatol. 2018;31:97-106. [DOI] [Full Text] |
| 3. | Ahn SK, Choi HJ. Complication After PDO Threads Lift. J Craniofac Surg. 2019;30:e467-e469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Rachel JD, Lack EB, Larson B. Incidence of complications and early recurrence in 29 patients after facial rejuvenation with barbed suture lifting. Dermatol Surg. 2010;36:348-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Kim HJ, Lee SJ, Lee JH, Kim SH, Suh IS, Jeong HS. Clinical Features of Skin Infection After Rhinoplasty with Only Absorbable Thread (Polydioxanone) in Oriental Traditional Medicine: A Case Series Study. Aesthetic Plast Surg. 2020;44:139-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (2)] |
| 6. | Park MH, Rah YC, Kim YH, Kim JH. Usefulness of computed tomography Hounsfield unit density in preoperative detection of cholesteatoma in mastoid ad antrum. Am J Otolaryngol. 2011;32:194-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Kim CM, Kim BY, Hye Suh D, Lee SJ, Moon HR, Ryu HJ. The efficacy of powdered polydioxanone in terms of collagen production compared with poly-L-lactic acid in a murine model. J Cosmet Dermatol. 2019;18:1893-1898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Molea G, Schonauer F, Bifulco G, D'Angelo D. Comparative study on biocompatibility and absorption times of three absorbable monofilament suture materials (Polydioxanone, Poliglecaprone 25, Glycomer 631). Br J Plast Surg. 2000;53:137-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 92] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Sulamanidze M, Sulamanidze G, Vozdvizhensky I, Sulamanidze C. Avoiding complications with Aptos sutures. Aesthet Surg J. 2011;31:863-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Teymoortash A, Fasunla JA, Pfützner W, Steinbach-Hundt S. Nasal tip abscess due to adverse skin reaction to Prolene: an unusual long term complication of rhinoplasty. J Laryngol Otol. 2013;127:76-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Jaafar AFL. Nose abscess after thread rhinoplasty: a case report. J Cosmetic Medicine. 2018;46-51. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Phelps ME, Hoffman EJ, Ter-Pogossian MM. Attenuation coefficients of various body tissues, fluids, and lesions at photon energies of 18 to 136 keV. Radiology. 1975;117:573-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 80] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Trojanowska A, Trojanowski P, Olszanski W, Klatka J, Drop A. Differentiation between cholesteatoma and inflammatory process of the middle ear, based on contrast-enhanced computed tomography imaging. J Laryngol Otol. 2007;121:444-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |