Published online Nov 6, 2021. doi: 10.12998/wjcc.v9.i31.9617
Peer-review started: June 21, 2021
First decision: July 14, 2021
Revised: July 27, 2021
Accepted: September 19, 2021
Article in press: September 19, 2021
Published online: November 6, 2021
Processing time: 129 Days and 23 Hours
Gallbladder polyps are one indication for cholecystectomy, but this procedure carries some disadvantages, including the potential for severe injury and high risk of post-operative complications. Laparoscopy combined with endoscopic surgery is a minimally invasive treatment option. We herein report a young patient with a gallbladder polyp who was successfully discharged from the hospital after laparoscopic-assisted endoscopy. This procedure may offer an alternative in the management of such lesions.
A 24-year-old female patient was hospitalized primarily for a gallbladder polyp. Due to the surgical risk associated with cholecystectomy and the low post-operative quality of life, the woman underwent laparoscopic-assisted transumbilical gastroscopy for gallbladder-preserving polypectomy under endotracheal intubation and general anaesthesia. The operation went smoothly.
We conclude laparoscopic-assisted transumbilical gastroscopy for gallbladder-preserving polypectomy is a safe and effective technique for the treatment of gallbladder polyps.
Core Tip: Cholecystectomy is currently the standard of care for gallbladder polyps. However, resection techniques not only cause great injury and carry high risk but may also lead to various postoperative complications. We present a successful case of radical resection after laparoscopic-assisted transumbilical gastroscopy for gallbladder-preserving polypectomy without severe postoperative complications.
- Citation: Zheng Q, Zhang G, Yu XH, Zhao ZF, Lu L, Han J, Zhang JZ, Zhang JK, Xiong Y. Perfect pair, scopes unite — laparoscopic-assisted transumbilical gastroscopy for gallbladder-preserving polypectomy: A case report. World J Clin Cases 2021; 9(31): 9617-9622
- URL: https://www.wjgnet.com/2307-8960/full/v9/i31/9617.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i31.9617
Laparoscopic-assisted endoscopy has been increasingly used in clinical settings. It results in relatively little trauma to surrounding tissues, is low risk and offers a quick recovery[1-5].
Laparoscopic-assisted transumbilical gastroscopy for gallbladder-preserving polypectomy was used in place of traditional laparoscopic cholecystectomy to remove a gallbladder polyp safely, effectively and with minimal invasiveness from the gallbladder of this young patient. This method provides a new option for the treatment of gallbladder polyps. We report a case of laparoscopic-assisted endoscopic excision of a gallbladder polyp and evaluate the safety and efficacy of this approach.
A 24-year-old woman presented in this case with a gallbladder polyp requiring treatment.
The patient was hospitalized for a gallbladder polyp discovered more than 3 years prior. The patient’s gallbladder polyp, approximately 0.7 cm × 0.6 cm in size, was found by physical examination 3 years ago, and it was not treated at that time.
She had no specific past illness.
The patient didn’t have a history of smoking or drinking alcohol. And she has no remarkable family medical history.
No significant abnormalities on physical examination. Her temperature was 36.5°C, pulse rate was 72 beats/min, and blood pressure was 124/86 mmHg.
Blood analysis showed a normal complete blood count, liver function and C-reactive protein.
Colour ultrasound examination of the upper abdomen showed a medium-strong echo intensity on the capsule wall, with a size of approximately 1.3 cm × 0.9 cm. There was no obvious sound or shadow behind it, and it did not move with a change in posture (Figure 1).
The patient was diagnosed with gallbladder polyp with no dysplasia.
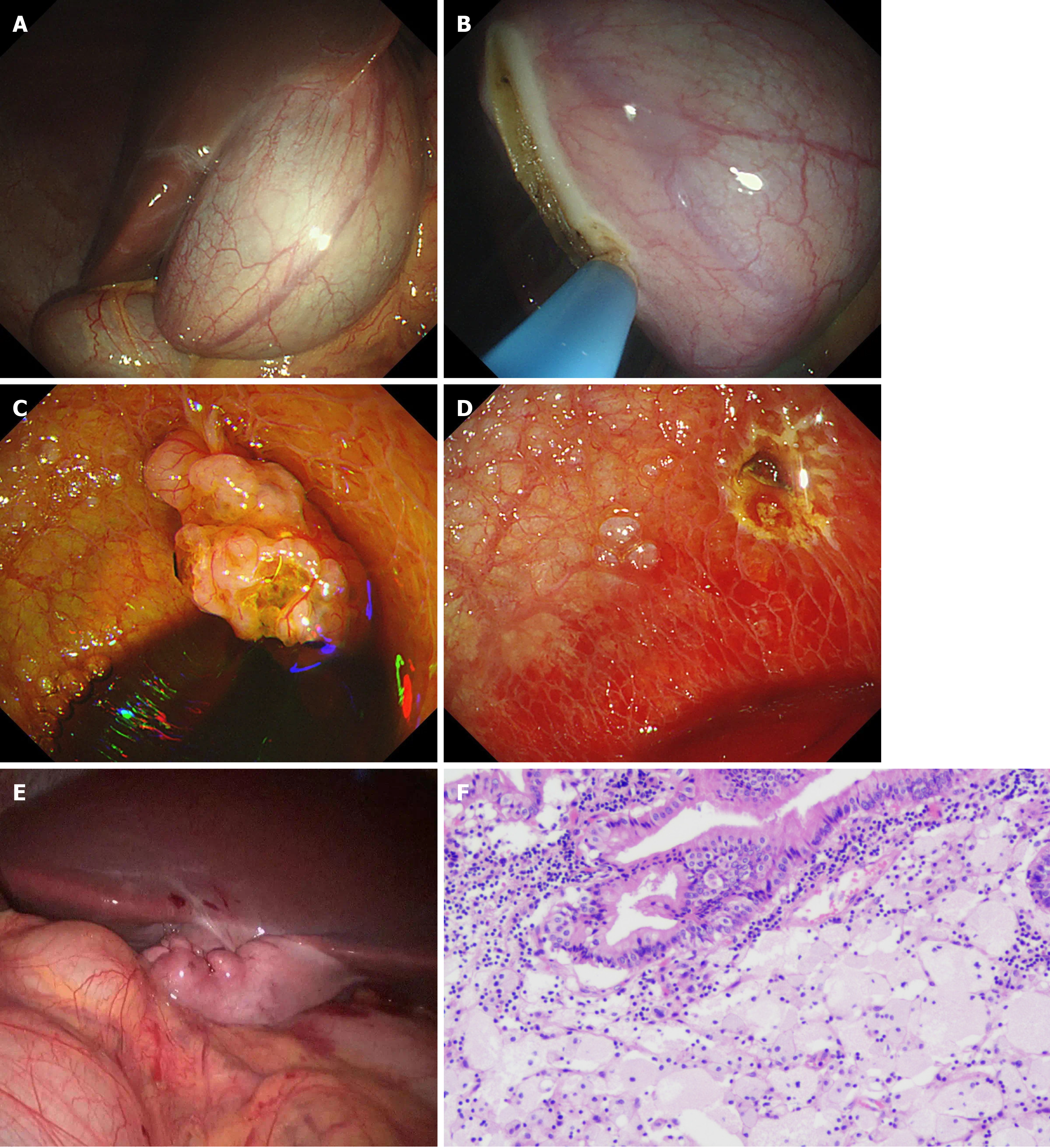
Laparoscopic-assisted transumbilical gastroscopy for gallbladder-preserving polypectomy was performed (Figure 2). The patient was placed in the supine position under general anaesthesia. Pneumoperitoneum was established using direct trocar insertion in an umbilical location. A right subcostal 12-mm port was then placed. The gastroscope entered the abdominal cavity through the umbilical trocar. The gallbladder was located with the assistance of laparoscopy, and an approximately 2-cm incision in the gallbladder wall was made longitudinally at the bottom of the gallbladder (Figure 2A and B). The procedure was smooth, and no significant bleeding was observed. Endoscopy entering the gallbladder showed a pedicled polyp with a grape cluster appearance (Figure 2C). The lesion was resected by high-frequency electroresection; active bleeding could be seen at the base, and haemostasis was achieved by electrocoagulation with haemostatic forceps (Figure 2D). The specimen was removed and fixed for pathological examination. The gastroscope was withdrawn from the abdominal cavity, and laparoscopic suture of the gallbladder incision was performed, followed by full flushing of the abdominal pelvic cavity and suture of the abdominal incision (Figure 2E). The specimen was found to be a cholesterol polyp. The total operative time was 96 min, and the blood loss was 10 mL.
The patient was cured after the operation, and the specimen was found to be a cholesterol polyp (Figure 2F). Her vital signs were stable, and no obvious abnormality was found in cardiopulmonary or abdominal specialist examinations.
The patient was a 24-year-old woman. Routine cholecystectomy to remove the gallbladder not only causes great injury and carries high risk but may also lead to various postoperative complications. Recently reported complications have mainly included postoperative bleeding, bile leakage, biliary peritonitis, subhepatic effusion or subphrenic abscess, postoperative jaundice, postoperative pancreatitis, and gastrointestinal fistula. Long-term complications include bile duct stricture, recurrent choledocholithiasis, biliary bleeding, post-cholecystectomy syndrome, cystic duct residual syndrome, and an increased incidence of colon cancer, among others. These complications can greatly impact the future quality of life of these patients[6,7]. Under this premise, gallbladder-preserving polypectomy was the most minimally invasive and safest treatment for this patient, which also reflects that surgery today needs to consider the concept of minimally invasive and humanized polypectomy.
Laparoscopic-assisted transumbilical gastroscopy for gallbladder-preserving polypectomy gives full play to the respective advantages of laparoscopy and gastroscopy. The advantages of laparoscopy are as follows: (1) It can directly monitor the location of abdominal organs and can provide an intraoperative visual field for endoscopy; and (2) Laparoscopy can be used to suture the gallbladder after the operation and reduce the incidence of biliary fistula and removes the need for metal clips to remain in the body. The advantages of the gastroscope are as follows: (1) It is a “soft lens” with a good degree of freedom. Gastroscopy can remove polyps under direct vision of the gallbladder and can locate small polyps that cannot be detected by ultrasound and other simultaneous auxiliary examinations; and (2) Tissue staining combined with electronic endoscopy (NBI, BLI, etc.) can improve the diagnosis rate of early cancer. Therefore, the complementary advantages of gastroscopy and laparoscopy provide the best solution for gallbladder-preserving polypectomy.
Laparoscopic-assisted endoscopic techniques are increasingly being used[8], including laparoscopic-assisted endoscopic retrograde cholangiopancreatography (LA-ERCP) and laparoscopic-assisted endoscopic ultrasound (LA-EUS)[9,10]. In a dual-centre study reported by Bowman et al[11] these surgical approaches were used for patients who underwent Roux-en-Y gastric bypass and developed pancreatobiliary issues after surgery. Bowman et al[11] argued in this study that LA-ERCP and combined LA-EUS plus LA-ERCP are safe and highly successful diagnostic and therapeutic modalities for patients. The advantages of laparoscopic-assisted transumbilical gastroscopy for gallbladder-preserving polypectomy over these laparoscopic-assisted peroral gastroscopy procedures are as follows: The gastroscope does not enter the abdominal cavity through a window in the stomach wall through the oral cavity but through the umbilicus, a natural cavity, which is clearly safer and minimally invasive, as the stomach incision does not need to be sutured when removing the scope. By minimizing the operation of the laparoscope during surgery, the laparoscope is only responsible for observing the position of the gallbladder and suturing the gallbladder incision, which shortens the operative time and reduces the risk associated with surgery.
This operation reflects the organic combination of laparoscopy and endoscopy, giving full play to their respective advantages. With the concept of minimally invasive therapy deeply rooted in the hearts of people and the continuously increasing demand for improvements in post-surgical aesthetics, the combination of laparoscopy and endoscopy is bound to become the direction of development for minimally invasive therapy[12,13]. This combination meets not only the aesthetic requirement of “no scar” surgery but also the inevitable trend toward more accurate and minimally invasive medical surgery in the 21st century.
To our knowledge, this is the first report of laparoscopic-assisted transumbilical gastroscopy for gallbladder-preserving polypectomy. We encountered no complications in the case. Our results suggest that this new method is safe and effective in the treatment of gallbladder polyps when cholecystectomy is not possible or available.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and Hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Saraiva MM S-Editor: Chang KL L-Editor: A P-Editor: Xing YX
| 1. | Ceppa FA, Gagné DJ, Papasavas PK, Caushaj PF. Laparoscopic transgastric endoscopy after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2007;3:21-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 70] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Nguyen NT, Hinojosa MW, Slone J, Lee J, Khiatani V, Wilson SE. Laparoscopic transgastric access to the biliary tree after Roux-en-Y gastric bypass. Obes Surg. 2007;17: 416-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Martinez J, Guerrero L, Byers P, Lopez P, Scagnelli T, Azuaje R, Dunkin B. Endoscopic retrograde cholangiopancreatography and gastroduodenoscopy after Roux-en-Y gastric bypass. Surg Endosc. 2006;20:1548-1550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 80] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Pimentel RR, Mehran A, Szomstein S, Rosenthal R. Laparoscopy-assisted transgastrostomy ERCP after bariatric surgery: case report of a novel approach. Gastrointest Endosc. 2004;59:325-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Roberts KE, Duffy AJ, Bell RL. Laparoscopic transgastric repair of a gastrogastric fistula after gastric bypass: a novel technique. Surg Innov. 2007;14:18-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Strasberg SM. Laparoscopic biliary surgery. Gastroenterol Clin North Am. 1999;28:117-132, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Maydeo A, Dhir V. The gallbladder polyp conundrum: a riddler on the wall. Gastrointest Endosc. 2013;78:494-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Roberts KE, Panait L, Duffy AJ, Jamidar PA, Bell RL. Laparoscopic-assisted transgastric endoscopy: current indications and future implications. JSLS. 2008;12:30-36. [PubMed] |
| 9. | Lopes TL, Clements RH, Wilcox CM. Laparoscopy-assisted ERCP: experience of a high-volume bariatric surgery center (with video). Gastrointest Endosc. 2009;70:1254-1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Bertin PM, Singh K, Arregui ME. Laparoscopic transgastric endoscopic retrograde cholangiopancreatography (ERCP) after gastric bypass: case series and a description of technique. Surg Endosc. 2011;25:2592-2596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Bowman E, Greenberg J, Garren M, Guda N, Rajca B, Benson M, Pfau P, Soni A, Walker A, Gopal D. Laparoscopic-assisted ERCP and EUS in patients with prior Roux-en-Y gastric bypass surgery: a dual-center case series experience. Surg Endosc. 2016;30:4647-4652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Cho WY, Kim YJ, Cho JY, Bok GH, Jin SY, Lee TH, Kim HG, Kim JO, Lee JS. Hybrid natural orifice transluminal endoscopic surgery: endoscopic full-thickness resection of early gastric cancer and laparoscopic regional lymph node dissection--14 human cases. Endoscopy. 2011;43:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Hammad H, Esmadi M, Ahmad D, Reicks M, Rawlings A. Laparoscopic and hand-assisted deep enteroscopy with polypectomy in Peutz-Jeghers syndrome. Gastrointest Endosc. 2014;79:26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |