Published online Nov 6, 2021. doi: 10.12998/wjcc.v9.i31.9592
Peer-review started: April 24, 2021
First decision: May 24, 2021
Revised: June 20, 2021
Accepted: October 11, 2021
Article in press: October 11, 2021
Published online: November 6, 2021
Processing time: 187 Days and 22.8 Hours
Acquired hemophilia is rare. In some cases, the bleeding in muscle causes compartment syndrome. However, it is not clear whether fasciotomy should be performed for the compartment syndrome caused by acquired hemophilia because of the risk of bleeding and the unknown functional results.
A 75-year-old woman was admitted with severe pain of the right forearm with no preceding traumatic event. The right forearm was obviously swollen, and stretch pain was observed. Subcutaneous hematomas were suspected in various parts of the body. Compartment pressure was 110 mmHg on the volar side. Activated partial thromboplastin time (aPTT) was prolonged to 54.9 s. Fasciotomy was performed, and hematoma was observed in the volar compartment. Postoperative laboratory examinations revealed a low level of factor VIII (FVIII) activity (12.5%) and a high level of FVIII inhibitor (15.2 bethesda units/mL). Acquired hemophilia A was diagnosed. Though recombinant clotting factors were administered, transfusion of red blood cells reached 46 units (140 mL/unit). Hemostasis was achieved 9 d after fasciotomy. The total cost of the clotting factor concentrates administered reached 28834600 yen. With prednisolone, FVIII activity and aPTT recovered gradually. Final function of the hand was good in the index finger and excellent in the others.
Fasciotomy resulted in good function of the hand in a case of non-traumatic compartment syndrome caused by acquired hemophilia, but life-threatening bleeding occurred, and the cost of clotting factor treatment was high. Preparation of sufficient blood transfusion, preoperative administration of recombinant activated clotting factor VII, and prompt fasciotomy could be ideal for such cases.
Core Tip: Whether we should perform fasciotomy for compartment syndrome caused by acquired hemophilia is unclear. A 75-year-old woman admitted with severe pain of the right forearm was diagnosed as having compartment syndrome, and fasciotomy was performed. Laboratory data showed acquired hemophilia A. Though recombinant activated clotting factor VII (rFVIIa) was administered, transfused red blood cells reached 46 units, and the cost of the clotting factor was 28834600 yen. Final hand function was good, but life-threatening bleeding and the high cost of treatment were serious problems. Preparation for sufficient blood transfusion, preoperative administration of rFVIIa, and prompt fasciotomy could be ideal.
- Citation: Kameda T, Yokota T, Ejiri S, Konno SI. Forearm compartment syndrome due to acquired hemophilia that required massive blood transfusions after fasciotomy: A case report. World J Clin Cases 2021; 9(31): 9592-9597
- URL: https://www.wjgnet.com/2307-8960/full/v9/i31/9592.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i31.9592
Acquired hemophilia is a rare disease with a reported incidence of 1.48 per million per year[1]. An antibody to factor VIII (FVIII) causes FVIII deficiency and results in the primary symptoms of subcutaneous and/or muscle bleeding. In some cases, the bleeding in muscle causes compartment syndrome. Compartment syndrome is an urgent condition, because fasciotomy must be performed within 4-6 h, and the natural course is known to have a terrible functional result.
However, whether we should perform fasciotomy for the compartment syndrome caused by acquired hemophilia is unclear because of the risk of bleeding and the unknown functional result. A case of non-traumatic compartment syndrome caused by acquired hemophilia in which fasciotomy resulted in good function of the hand, but life-threatening bleeding occurred, is presented.
A 75-year-old woman was admitted to Iwaki Medical Center complaining of severe pain of the right forearm.
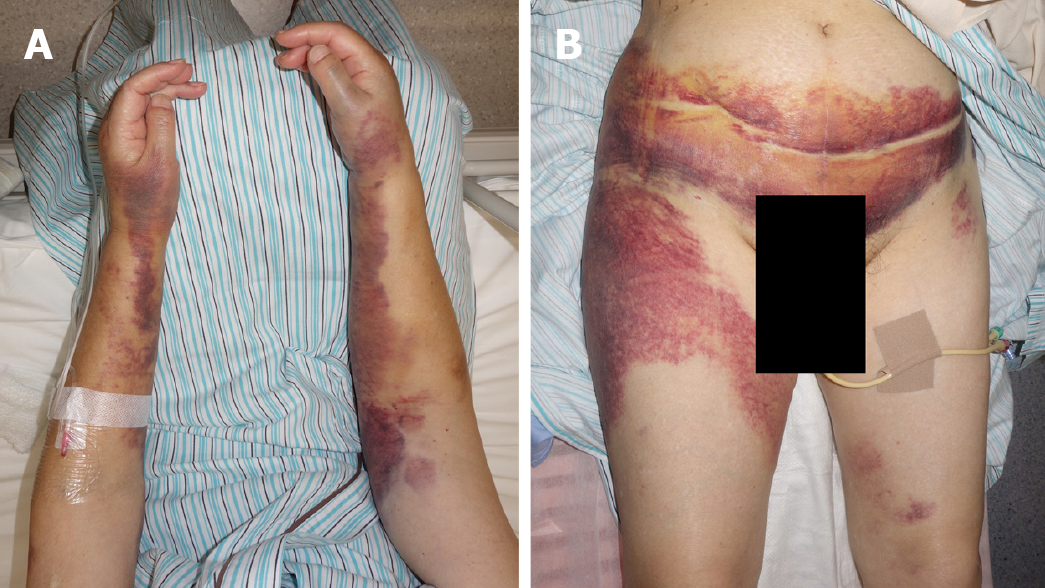
A few weeks before the first visit, she felt that her skin was easily bruised. One day before the visit, her right forearm became gradually painful without any traumatic event. At the initial examination, the right forearm was obviously swollen (Figure 1), and subcutaneous hematoma was suspected because of the purple skin. Her left forearm, lower abdomen, and right proximal thigh were the same color without swelling or pain (Figure 1).
When the patient was 73 years old, she underwent surgery for left breast cancer.
She also had hypertension since she was 70 years old.
Tenderness was mainly observed on the volar side of the forearm, and severe stretch pain was evident. Compartment pressure was measured. The pressure of volar compartment was 110 mmHg, that of the dorsal compartment was 38 mmHg and that of the mobile wad compartment was 20 mmHg, while the blood pressure was 203/102 mmHg (mean: 136 mmHg).
Activated partial thromboplastin time (aPTT) was prolonged to 54.9 s, though prothrombin time was normal (100 s). At this point, her blood hemoglobin level was 7.7 g/dL.
A right forearm X-ray showed no fracture. Contrast-enhanced computed tomography (CT) did not show obvious arterial extravasation.
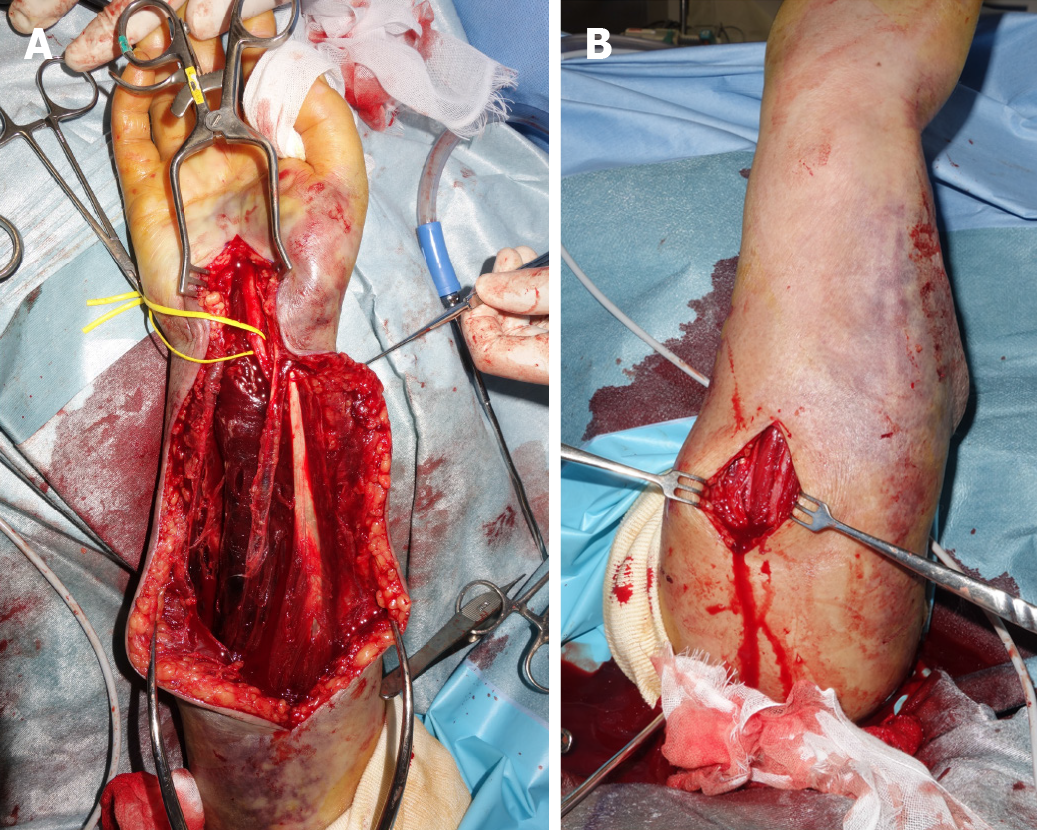
Based on the physical examination, compartment syndrome of the right forearm was diagnosed. Though aPTT was prolonged, fasciotomy was performed as soon as possible. During surgery, hematoma was observed in the muscle of the volar compartment (Figure 2). Though release of compartment pressure was confirmed, continuous oozing was observed. The surgical site was covered by artificial dermis because the swollen muscle made primary closure difficult. After the operation, the severe resting pain decreased, and the stretch pain disappeared.
After consulting a hematologist, additional laboratory examinations showed a low level of FVIII activity (12.5%) and a high level of FVIII inhibitor [15.2 bethesda units (BU)/mL]. Based on these results, which were available 3 d after the surgery, acquired hemophilia A was diagnosed.
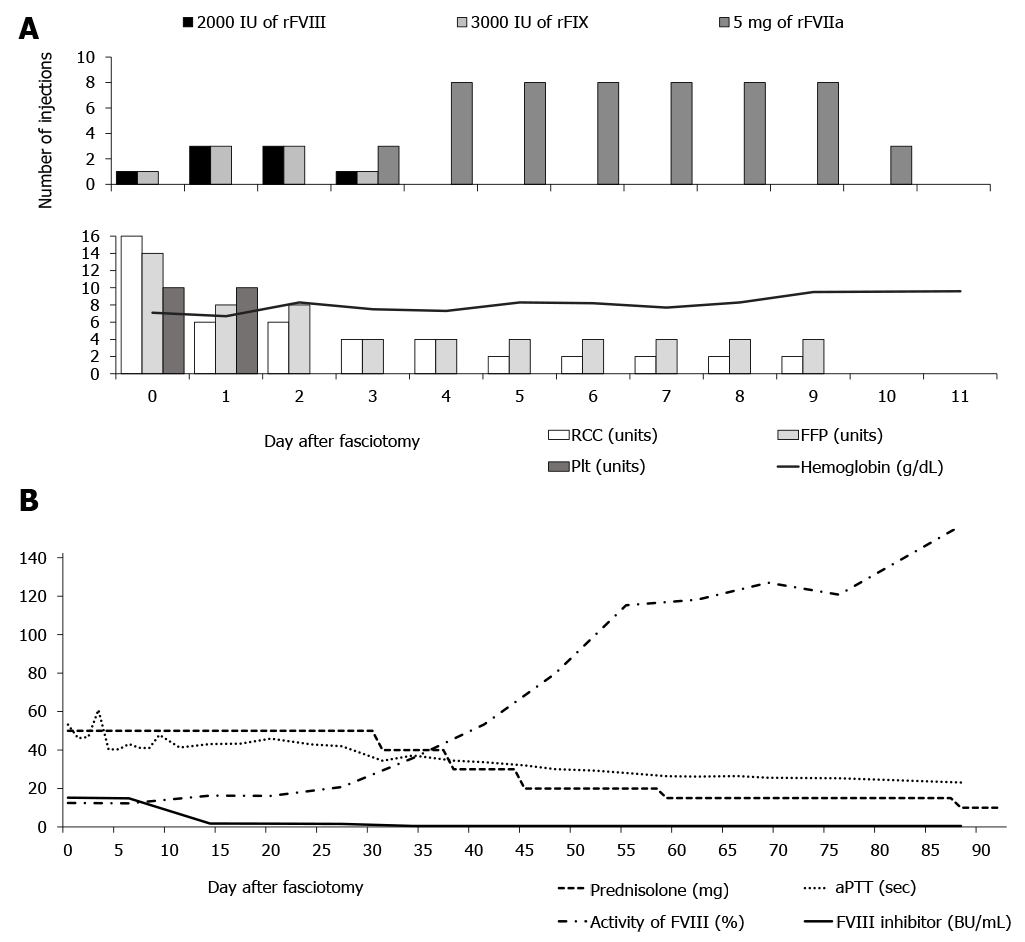
After the operation, Eloctate, a recombinant factor VIII, and Alprolix, a recombinant factor IX, were administered before the coagulation factor results were available. The effectiveness of bandage compression was limited. The oozing from the surgical site continued. Prednisolone sodium succinate was also administered for the treatment of acquired hemophilia. On day three after surgery, acquired hemophilia A was diagnosed, and NovoSeven, recombinant activated clotting factor VII (rFVIIa), was started. By that point, the amount of red blood cell concentrate (RCC) transfused was 28 units (140 mL/unit in Japan), that of fresh frozen plasma (FFP) was 30 units (120 mL/unit), and that of platelet concentrate was 20 units (20 mL/unit), but oozing continued. On day nine after surgery, bleeding finally stopped. The total amount transfused was 46 units of RCC, 58 units of FFP, and 20 units of platelets. The total cost of the clotting factor concentrates was 28834600 yen.
The time courses of aPTT, FVIII activity, FVIII inhibitor, and the dose of prednisolone are shown in Figure 3. On day 31 after surgery, since aPTT returned to within the normal range, the dose of prednisolone was gradually decreased. On day 34 after surgery, the FVIII inhibitor decreased to under 1.0, and on day 48, FVIII activity increased to the normal range.
On day 25 after surgery, Acinetobacter baumannii (A. baumannii), which was resistant to ciprofloxacin, was detected from the surgical site. Administration of amikacin and daily wound treatment healed the infection. On day 69 after surgery, split thickness skin grafting from the left thigh was performed for the skin defect of the right forearm. The wound had completely healed by day 78. Finally, though slight restriction of active flexion of the right index finger remained (% total active motion was 78%: good)[2], the patient had no other impaired function after 4 mo.
In this report, a case of non-traumatic compartment syndrome caused by acquired hemophilia was presented. Fasciotomy resulted in good function of the hand. However, it caused life-threatening bleeding, and the continuous bleeding required a large amount of clotting factor concentrates, at a very high cost.
Compartment syndrome is an urgent condition. It is well known that the fasciotomy followed by compartment pressure measurement should be performed promptly because of the terrible functional result in the natural course. Even 3 h of ischemia can cause necrosis or cellular deterioration[3,4]. However, with respect to cases caused by congenital hemophilia, an algorithm showed slightly different indications for fasciotomy[5] considering the risk of bleeding. According to this algorithm, factor replacement should be performed before measuring compartment pressure. Next, if delta pressure (difference between mean blood pressure and compartment pressure) is under 30, and if the onset of symptoms was within 2 h, we should wait and observe the compartment pressure continuously. If we applied this algorithm to the present case, the administration of rFVIIa or activated prothrombin complex concentrate (aPCC) replacement, called a bypassing agent, should have been performed before fasciotomy. In acquired hemophilia A, rFVIIa and aPCC have been shown to have very high rates of controlling bleeding that were essentially equal (93.0% vs 93.0%) in a multicenter, prospective study[6]. In the present case, another problem was the time lag between the diagnosis of compartment syndrome and that of acquired hemophilia. Even though the decision for fasciotomy should be made promptly, the results for clotting factor and inhibitor activities, which are necessary for the definitive diagnosis of acquired hemophilia, were only available a few days after the fasciotomy. Therefore, if non-traumatic compartment syndrome is diagnosed with a prolonged aPTT and normal PT, we may need to consider a bypassing agent and subsequent fasciotomy before making the definitive diagnosis of acquired hemophilia. To help provide such prompt management, a novel algorithm for non-traumatic compartment syndrome with aPTT prolongation is needed. This requires study of more cases of compartment syndrome caused by acquired hemophilia.
The present case required a large amount of clotting factor concentrates at a very high cost. Based on the normal protocol for compartment syndrome, prompt fasciotomy should be performed. However, it can cause life-threatening bleeding in cases of acquired hemophilia. Additionally, the evidence for agents that provide adequate hemostasis for surgical procedures with acquired hemophilia is inadequate. Ma reported that rFVIIa administration before and after the surgical procedure provided adequate hemostasis[7]. In that report, the total number of injections was from one to 77 (n = 24), whereas it was 54 in the present case, at a cost of 21941000 yen. Additionally, inappropriate administration of recombinant factors VIII and IX resulted in further cost in the present case. The patient should be informed of this cost issue before starting the treatment, though delay of fasciotomy must be avoided. Suitable and prompt administration of rFVIIa, including preoperative treatment, may result in early hemostasis, reduce the total amount of bleeding, and decrease extra costs.
Fasciotomy in acquired hemophilia also has a risk of surgical site infection (SSI). Immunosuppressive therapy, as typified by prednisolone or cyclophosphamide, is the standard treatment for acquired hemophilia, but it can lead to the risk of SSI[8]. However, this should be performed in parallel with wound care after fasciotomy. Since aPTT recovery takes time, and additional surgical treatments can lead to further bleeding, it produces a compromised host with an open wound. This condition easily leads to SSI. Fortunately, the A. baumannii in the present case was not the multidrug-resistant type. If so, the final functional result would have been worse. From this perspective, establishing an adequate algorithm for non-traumatic compartment syndrome with acquired hemophilia would be important.
Fasciotomy can provide good function of the hand, but it could result in life-threatening bleeding in non-traumatic compartment syndrome caused by acquired hemophilia. Continuous bleeding after fasciotomy could incur a high cost for clotting factors for hemostasis. To manage life-threatening bleeding and reduce costs, sufficient preparation for blood transfusion, preoperative administration of rFVIIa, and prompt fasciotomy could be ideal. Confirming the adequacy of this response and achieving a smooth treatment protocol will require the integration of many cases and the establishment of an algorithm for non-traumatic compartment syndrome with prolonged aPTT.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yang TY S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Collins PW, Hirsch S, Baglin TP, Dolan G, Hanley J, Makris M, Keeling DM, Liesner R, Brown SA, Hay CR; UK Haemophilia Centre Doctors' Organisation. Acquired hemophilia A in the United Kingdom: a 2-year national surveillance study by the United Kingdom Haemophilia Centre Doctors' Organisation. Blood. 2007;109:1870-1877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 453] [Cited by in RCA: 500] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 3. | Heppenstall RB, Scott R, Sapega A, Park YS, Chance B. A comparative study of the tolerance of skeletal muscle to ischemia. Tourniquet application compared with acute compartment syndrome. J Bone Joint Surg Am. 1986;68:820-828. [PubMed] |
| 4. | Vaillancourt C, Shrier I, Vandal A, Falk M, Rossignol M, Vernec A, Somogyi D. Acute compartment syndrome: how long before muscle necrosis occurs? CJEM. 2004;6:147-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 5. | Naranja RJ Jr, Chan PS, High K, Esterhai JL Jr, Heppenstall RB. Treatment of considerations in patients with compartment syndrome and an inherited bleeding disorder. Orthopedics. 1997;20:706-9; quiz 710. [PubMed] |
| 6. | Baudo F, Collins P, Huth-Kühne A, Lévesque H, Marco P, Nemes L, Pellegrini F, Tengborn L, Knoebl P; EACH2 registry contributors. Management of bleeding in acquired hemophilia A: results from the European Acquired Haemophilia (EACH2) Registry. Blood. 2012;120:39-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 273] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 7. | Ma AD, Kessler CM, Al-Mondhiry HA, Gut RZ, Cooper DL. US experience with recombinant factor VIIa for surgery and other invasive procedures in acquired haemophilia: analysis from the Hemostasis and Thrombosis Research Society Registry. Haemophilia. 2016;22:e18-e24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, Reinke CE, Morgan S, Solomkin JS, Mazuski JE, Dellinger EP, Itani KMF, Berbari EF, Segreti J, Parvizi J, Blanchard J, Allen G, Kluytmans JAJW, Donlan R, Schecter WP; Healthcare Infection Control Practices Advisory Committee. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017;152:784-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1394] [Cited by in RCA: 2037] [Article Influence: 254.6] [Reference Citation Analysis (0)] |