Published online Nov 6, 2021. doi: 10.12998/wjcc.v9.i31.9584
Peer-review started: March 29, 2021
First decision: April 28, 2021
Revised: May 12, 2021
Accepted: September 19, 2021
Article in press: September 19, 2021
Published online: November 6, 2021
Processing time: 214 Days and 8.6 Hours
Drainage tube removal is difficult when the greater omentum becomes incarcerated in the drainage tube through the side holes. Currently, known removal methods are either ineffective or will cause additional damage to the patient in a secondary operation. Ureteroscopy and the holmium laser have been used in various surgical techniques in urology, and in theory, they are expected to be a good strategy for solving the problem of tissue incarceration.
Four patients diagnosed with difficult removal of an abdominal drainage tube following abdominal surgery are reported. All patients underwent surgery to remove the incarcerated greater omentum in the drainage tube using a holmium laser and a ureteroscope, and a new 16-F drain was then placed in the abdominal or pelvic cavity. The efficacy of this technique was evaluated by intraoperative conditions, success rate, and operating time; safety was evaluated by perioperative conditions and the probability of postoperative complications. All four operations went smoothly, and the drains were successfully removed in all patients. The average operating time was 24.5 min. Intraoperatively, the average irrigation volume was 892.0 mL, the average drainage volume was 638.5 mL, and no bleeding or damage to surrounding tissues was observed. Postoperatively, the average drainage volume was 32.8 mL and the new drains were removed within 36 h. All patients were able to get out of bed and move around within 12 h. Their visual analogue pain scores were all below 3. The average follow-up duration was 12.5 mo and no complications such as fever or bleeding were noted.
Ureteroscopic holmium laser surgery is an effective, safe and minimally invasive technique for removing drains where the greater omentum is incarcerated in the abdominal drain.
Core Tip: Inability to remove an abdominal drainage tube is a complication of abdominal surgery, and one of the main reasons for this is that the greater omentum can become incarcerated in the drainage tube. We report four cases of difficult removal of an abdominal drainage tube treated with ureteroscopic holmium laser surgery to transect the greater omentum. This may be the first report of the use of this technique to successfully remove drainage tubes. All four patients recovered well after surgery and no complications were observed during follow-up. This strategy successfully decreased the risk of a secondary operation, additional hospitalization and minimized patient discomfort.
- Citation: Liu HM, Luo GH, Yang XF, Chu ZG, Ye T, Su ZY, Kai L, Yang XS, Wang Z. Ureteroscopic holmium laser to transect the greater omentum to remove an abdominal drain: Four case reports . World J Clin Cases 2021; 9(31): 9584-9591
- URL: https://www.wjgnet.com/2307-8960/full/v9/i31/9584.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i31.9584
Postoperative abdominal drainage is commonly used to observe and drain effusion in the surgical field. However, in approximately 0.067%–0.1% of patients the drain is difficult to remove[1]. The reasons for this may include: insufficient puncture hole of the drainage tube, incorrect methods of removing and suturing of the drainage tube, and the surrounding tissue wrapping the drainage tube. One of the most difficult situations is when the greater omentum is incarcerated in the drain through the side holes of the drainage tube. In such case, non-surgical methods, such as continuous traction, and perfusion of normal saline or paraffin oil into the drainage tube under strong pressure[2,3], are often ineffective and likely to cause bleeding and peripheral organ injury. Generally, laparoscopic and open exploratory laparotomy are the final option to remove the drainage tube[4,5]. However, additional surgery may cause secondary injury, and increase costs and hospital stay. We have previously managed a difficult case in which the drainage tube had inadvertently been trapped by a suture in the abdominal wall muscle layer. Based on our past experience of cutting the suture between the drain and tissue using a holmium laser and a ureteroscope to successfully remove the trapped drain[6,7], we used this minimally invasive method to transect the greater omentum incarcerated in the drain and then successfully removed the abdominal drain in four patients. We here report the procedure and discuss its safety and feasibility.
From March 2015 to June 2019, four patients, 2 males and 2 females aged 55 to 73 years underwent abdominal surgery in Guizhou Provincial People's Hospital. Postoperatively, the abdominal drainage tube could not be removed due to abdominal pain and discomfort when the surgeon attempted to remove the drainage tube.
The four patients underwent different abdominal surgeries. Postoperatively, the drainage volume decreased gradually with appropriate treatment, and then the abdominal drain was scheduled for removal. However, during the attempted drain removal, marked resistance was encountered, and the patients experienced obvious abdominal pain and discomfort.
The characteristics of the four patients are shown in Table 1. Case 1 had a history of laparoscopic radical resection of rectal cancer, case 2 and case 4 had a history of laparoscopic radical cystectomy for bladder carcinoma, respectively, and case 3 underwent laparoscopic resection of a recurrent left adrenal tumor. During surgery, a 24-F silicone or rubber drain was placed in the surgical field, the number of side holes in the drainage tube was 6-8, and the diameter of the side holes was 8.0 mm. The average operation time was approximately 4 h (range 1.8-6 h). Postoperatively, the drainage volume ranged from 40 to 1300 mL/d and drain indwelling time ranged from 13 to 63 d. Lymphatic fistulas accounted for prolonged drainage time, and the celiac test for abdominal drainage fluid was positive in cases 1 and 3. Methicillin-resistant Staphylococcus aureus was cultured from peritoneal drainage fluid in case 3. The mean postoperative serum albumin level (32.0 g/L) was significantly lower than that before surgery (40.1 g/L) in all four patients.
| Variable | Patients 1 | Patients 2 | Patients 3 | Patients 4 | Mean value |
| Age (yr) | 73 | 60 | 62 | 55 | 62.5 |
| Gender | Female | Male | Male | Female | — |
| Operation method | RR | RC | ATR | RC | — |
| Operation time (h) | 4 | 6 | 1.8 | 4.9 | 4.2 |
| Drain position | Left pelvic cavity | Left pelvic cavity | Left abdominal cavity | Right pelvic cavity | — |
| Drainage tube type | 24-F rubber tube | 24-F silicone tube | 24-F silicone tube | 24-F silicone tube | 24-F |
| Number of side holes of the drainage tube | 7 | 8 | 6 | 7 | 7.0 |
| Diameter of side holes of drainage tube (mm) | 8.0 | 8.0 | 8.0 | 8.0 | 8.0 |
| Preoperative mean serum albumin (g/L) | 37.9 (37.0-39.2) | 36.1 (35.2-37.7) | 45.5 (43.9-47.5) | 40.8 (39.7-41.9) | 40.1 |
| Postoperative mean serum albumin (g/L) | 30.9 (25.5-37.3) | 30.9 (24.7-35.6) | 33.6 (28.2-39.5) | 32.5 (25.8-37.8) | 32.0 |
| Postoperative mean drain volume (mL/ d) | 360 (110-1300) | 420 (125-950) | 150 (40-460) | 285 (75-1100) | 303.8 |
| The celiac test of the drainage fluid | Positive | Negative | Positive | Negative | — |
| Creatinine value of drainage fluid (mmol/L) | 56.3 | 73.2 | — | 62.6 | 64.0 |
| Drainage culture of bacteria | Negative | Negative | MRSA | Negative | — |
| Adjustment times of drainage tube position | 2 | 1 | 0 | 1 | 1 |
| Drain indwelling time (d) | 19 | 63 | 13 | 27 | 30.5 |
No notable personal or family history.
Pale-yellow clear fluid was seen in the abdominal drainage tube in all patients. The abdomen was soft, but tender with no rebound pain in all four patients.
Previous laboratory examinations in these four patients are shown in Table 1. At the time of this visit, all patients had normal laboratory examinations.
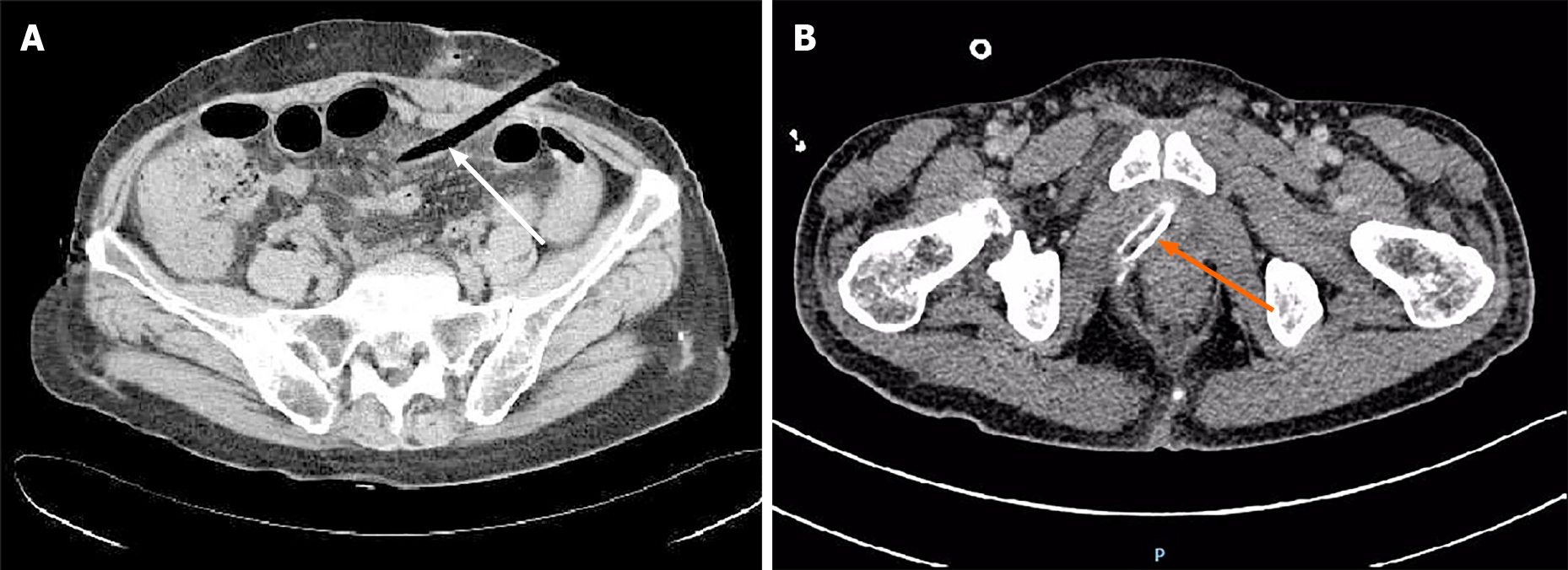
An imaging evaluation with abdominal computed tomography (CT), showed that the drainage tube passed through the abdominal cavity rigidly, and was at an angle to the abdominal wall, rather than parallel and close to the abdominal wall. The drainage tube was tightly enveloped by the surrounding tissue, with uneven density inside the tube. The greater omentum and other tissues were considered to be incarcerated in the peritoneal drains (Figure 1).
The diagnosis in all four patients was difficult removal of the abdominal drainage tube due to greater omentum incarceration in the drain. The diagnosis was further confirmed by intraoperative ureteroscopy.
Non-surgical methods such as continuous traction, and perfusion of normal saline or paraffin oil into the drainage tube under strong pressure failed. Considering that traditional methods, such as laparoscopic or open surgery, would cause greater trauma and slow postoperative recovery, we performed minimally invasive ureteroscopic holmium laser surgery. One patient with an indwelling drain in the upper abdominal cavity underwent general anesthesia for poor pain tolerance. The remaining three patients with indwelling pelvic drains received a 50–100 mg flurbiprofen axetil injection intraoperatively for analgesia, and pain was well tolerated.
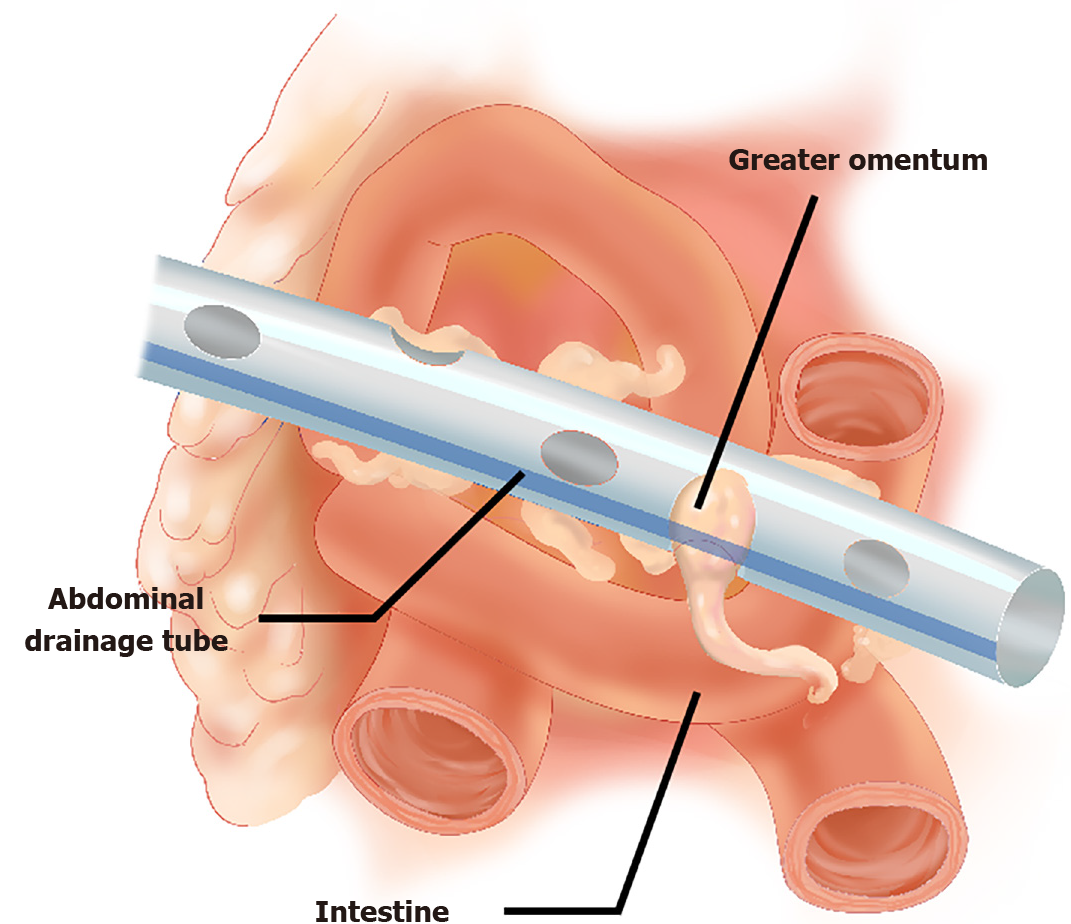
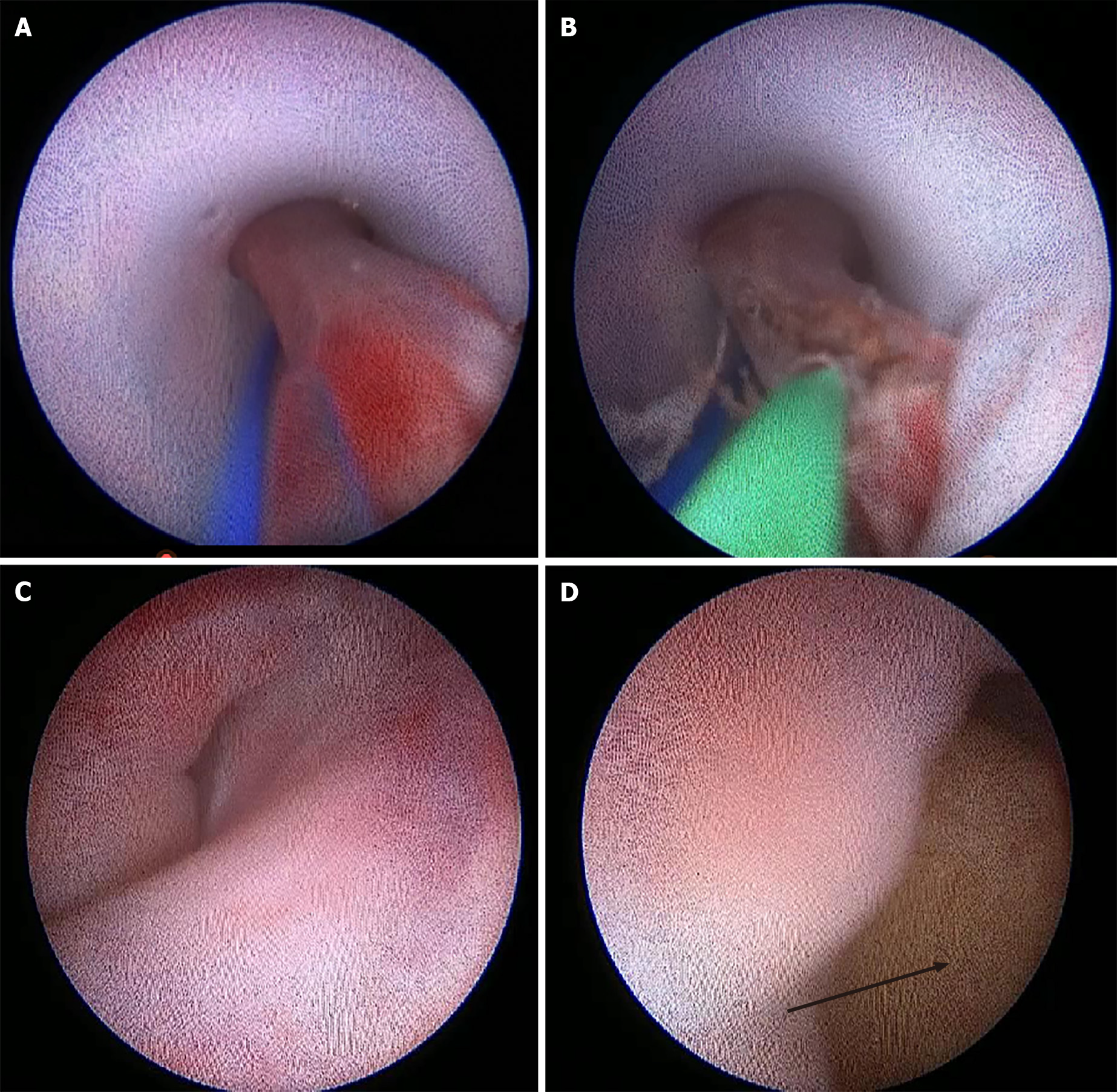
We transected the drain approximately 5 cm from the body surface and slowly placed a 7.8/9.5-F ureteroscope (Karl Storz SE & Co. KG, Tuttlingen, Germany) into the drain to inspect the inside of the drain under direct vision. We used foreign body forceps to clamp and remove cellulosic or necrotic tissues and other foreign material in the drain lumen, to maintain a clear field of vision. The greater omentum could then be seen which entered the drain through the side hole. The incarcerated greater omentum was edematous and blocked the drainage tube (Figure 2). In one patient, the greater omentum entered the drain through different side holes. The incarcerated tissues were carefully checked and the intestines were excluded. After confirming that the incarcerated tissue was the greater omentum, we used the holmium laser to cut the greater omentum (0.6 J, 30 Hz, 200-μm fiber; 60 W Holmium YAG Laser System; LISA Laser Products, Katlenburg, Germany) (Figure 3). Low-pressure flushing was required to maintain a clear visual field and observe bleeding in the greater omentum. Transection of the greater omentum should be performed gently and slowly to avoid the omentum rapidly retracting into the abdominal cavity as bleeding would not be observed. After transecting the greater omentum and confirming no hemorrhage, we rotated the drain gently and aspirated the infusion fluid. The drains were removed easily under direct vision of the ureteroscope. The integrity of the drains was confirmed, and a new 16-F drain was placed in the abdominal or pelvic cavity.
Using the ureteroscope, the greater omentum was found to be incarcerated in the drain through the side holes in all four patients. The operations in these patients went smoothly and the drains were successfully removed. The average operation time was 24.5 min (range: 20-30 min). Intraoperatively, the average infusion volume was 892 mL (range: 615–1285 mL), the average drainage volume was 638.5 mL (range: 453–845 mL), and no bleeding or damage to surrounding organs was observed. We noted that there were more side holes in the drain (6-8) and were larger (diameter: 8 mm) through which the omentum had become incarcerated. Postoperatively, the average drainage volume was 32.8 mL (range: 10-73 mL) and the new drains were removed within 36 h. Antibiotics were routinely given 30 min before and 24 h after surgery. The visual analogue pain score in these patients ranged from 1 to 3. All patients were able to get out of bed and move around within 12 h after surgery, and the anal exhaust time in all patients was within 12 h. Dietary intake and gastrointestinal function were not significantly affected. The average hospitalization time was 1.8 d (range: 1-3 d). The average follow-up duration was 12.5 mo. None of the patients developed complications during hospitalization such as bleeding, fever, abdominal pain, peritoneal effusion, abscess and hernia. One patient with rectal cancer died of metastasis, and the remaining three patients were still alive without long-term complications at the time of this report (Table 2).
| Variable | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Mean value |
| Intraoperative irrigation volume (mL) | 716 | 952 | 1285 | 615 | 892.0 |
| Intraoperative drainage volume (mL) | 500 | 756 | 845 | 453 | 638.5 |
| Operation time (min) | 25 | 30 | 23 | 20 | 24.5 |
| Intraoperative hemorrhage (mL) | No | No | No | No | — |
| Surrounding tissues damage | No | No | No | No | — |
| Successfully removed drain | Yes | Yes | Yes | Yes | — |
| Postoperative exhaust time (h) | 6.5 | 3.4 | 10.6 | 2.2 | 5.7 |
| Off-bed activity time (h) | 6.8 | 2 | 10 | 4.6 | 5.9 |
| Postoperative drainage volume (mL) | 16 | 10 | 73 | 32 | 32.8 |
| Postoperative VAS (score) | 3 | 1 | 1 | 2 | 1.8 |
| Postoperative fever | No | No | No | No | — |
| Postoperative bleeding | No | No | No | No | — |
| Follow-up time (mo) | 6 | 18 | 14 | 12 | 12.5 |
If an abdominal drainage tube has been in place for a long time, it is possible that granulation tissue, the greater omentum, intestine and other tissues may grow into the drainage tube through the side holes[8,9]. It is very difficult to remove the drain postoperatively when the greater omentum is incarcerated in the drainage tube (Figure 2). Non-surgical methods fail in most cases, and violent extubation may result in rupture of the drainage tube, which is a more difficult complication to manage[4,5]. In addition, severe bleeding may occur due to tearing of the vessels in the greater omentum if the drain is pulled out. Generally, open or laparoscopic laparotomy is the ultimate choice for drain removal. Although laparoscopic surgery can reduce the trauma to some extent, it is necessary to establish new methods for abdominal exploration under anesthesia. Ureteroscopic surgery can resolve these deficiencies, and is simpler, more convenient, and can minimize injury.
The ureteroscope (7.8/9.5-F) can easily enter 16-F or larger drainage tubes. Due to its accurate cutting ability and good hemostatic effect, the holmium laser has been widely used in different types of surgery, such as excising hyperplastic prostates, bladder tumors, and ureteral polyps[10,11]. The holmium laser has good directivity with less penetration, because 95% of the energy is absorbed quickly by the surrounding medium within a 5-mmcd low-energy continuous wave mode, especially when the frequency is > 20 Hz[12]. Therefore, we set our holmium laser energy to 0.6 J and frequency to 30 Hz. Additionally, the blood vessels supplying the omentum were trapped in the side holes of the drain for a long time in our patients; therefore, the blood supply to the incarcerated omental tissue was poor, and the risk of bleeding was low, intraoperatively. It was proved in these four patients that it is safe to cut the incarcerated greater omentum in the drain with the holmium laser under direct vision using the ureteroscope. The surgery can be completed easily within a short time. All the patients developed slight discomfort, but recovered quickly with no postoperative complications.
According to our experience, the following should be noted when using a holmium laser to remove incarcerated greater omentum in the drain under direct vision using a ureteroscope: (1) Non-steroidal analgesics (such as flurbiprofen axetil injection) are effective in relieving pain without general anesthesia. However, if the patient cannot tolerate pain and discomfort, general anesthesia can be used; (2) The ureteroscope is suitable for incarcerated greater omentum in the drain when the drain is kept approximately 5 cm away from the body surface; (3) The ureteroscope should enter the drain slowly and gently. Before the holmium laser is used, the nature of the incarcerated tissue should be determined to avoid bowel and other organ damage. In addition, the ureteroscope body or foreign body forceps can be used to remove loose tissue in the drain for clear vision; (4) When the holmium laser is used to cut the greater omentum, normal saline should be flushed to maintain clear vision and observe bleeding at all times; (5) When the greater omentum is transected and the residual omentum in the drain is removed, abdominal bleeding or other abnormalities should be observed under direct vision of the ureteroscope; and (6) To avoid secondary postoperative peritoneal effusion and infection, a new drainage tube can be placed to drain the perfusion fluid and removed within 48 h. If the infusion fluid is completely aspirated during the operation, it is not necessary to place a new drainage tube.
Omental incarceration in a drainage tube is a rare postoperative complication, which according to our clinical data is related to: (1) Prolonged drainage time which is a key point. Our four patients experienced lymphatic fistulas which is a common complication especially after radical tumor resection with lymph node dissection; (2) The size of the side holes in the drain is closely related to omental incarceration. In our four patients, the omentum was noted to enter the drain through the side holes of larger size; (3) Generally, the drain is placed along the abdominal and pelvic side wall; however, based on the postoperative CT scan, the drain moved in the abdominal cavity and was surrounded by the intestine and omentum. Incorrect position of the drain plays an important role in omental incarceration (Figure 2). When the drain is difficult to remove postoperatively, a CT scan may be helpful for the diagnosis of omentum incarceration (Figure 2). In our patients, when the diagnosis was suspected, we used a ureteroscope to confirm omentum incarceration; and (4) Hypoproteinemia may result in more ascites.
To avoid difficult drain removal postoperatively, the following points should be noted: (1) Unnecessary indwelling drains should be avoided. Some postoperative complications such as lymphatic fistulas, peritoneal infection, and hypoproteinemia should be controlled as soon as possible. It is necessary to evaluate daily whether the drain can be removed, and the drain should be removed in a timely fashion; (2) The side holes in the drain should not be too large or too many; (3) Avoid putting the drain in the abdominal cavity which can then be surrounded by the omentum and intestines; and (4) Rotating the drain gently every 2–3 d should be performed to avoid incarceration of the omentum. However, drainage may be required for a relatively long time due to some postoperative complications.
In summary, in the above cases, we used ureteroscopic holmium laser surgery to manage greater omentum incarceration in the drainage tube and successfully remove the abdominal drain through the existing cavity, reducing the risk of a secondary operation and shortening hospital stay. This new treatment strategy, which is a safe, feasible, easy to operate, and effective minimally invasive surgery, may be a better option than traditional surgical methods.
We sincerely thank Jane Charbonneau for editing the English text of a draft of this manuscript and polishing the English of this manuscript.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bains L S-Editor: Liu M L-Editor: A P-Editor: Guo X
| 1. | Jones SA. The foreign body problem after laparotomy. Personal experiences. Am J Surg. 1971;122:785-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | He XL, Liu W. Cause analysis and treatment of difficulty in abdominal drainage tube removal (report of 22 cases). Zhongguo Puwai Jichu Linchuang Zazhi. 2016;4:490-492. [DOI] [Full Text] |
| 3. | Zheng ZG. Diagnosis and treatment of 9 cases of difficult extubation caused by tissue insertion of abdominal drainage tube. Xinan Guofang Yiyao. 2002;12: 223-224. [DOI] [Full Text] |
| 4. | Carlomagno N, Santangelo M, Grassia S, La Tessa C, Renda A. Laparoscopic retrieval of retained intraperitoneal drain in the immediate postoperative period Report of two cases. Ann Ital Chir. 2012;2012. [PubMed] |
| 5. | Liao CS, Shieh MC. Laparoscopic retrieval of retained intraperitoneal drains in the immediate postoperative period. J Chin Med Assoc. 2011;74:138-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Luo GH, Xia SJ, Sun ZL. Holmium laser division of a suture causing entrapment of a drainage tube after laparoscopic nephrectomy. Int Urol Nephrol. 2013;45:355-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Gao X, Lu X, Ren S, Xu C, Sun Y. Ureteroscopic holmium laser cutting for inadvertently sutured drainage tube (report of five cases). Lasers Med Sci. 2008;23:337-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Zenni MK, Cooper CS, Hutcheson JC, Fenig DM, Snyder HM 3rd, Hawtrey CE. Intravesical Jackson-Pratt drain for urinary diversion after augmentation cystoplasty. J Urol. 2001;165:1233-1234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Poon CM, Leong HT. Abdominal drain causing early small bowel obstruction after laparoscopic colectomy. JSLS. 2009;13:625-627. [PubMed] |
| 10. | Planelles Gómez J, Olmos Sánchez L, Cardosa Benet JJ, Martínez López E, Vidal Moreno JF. Holmium YAG Photocoagulation: Safe and Economical Alternative to Transurethral Resection in Small Nonmuscle-Invasive Bladder Tumors. J Endourol. 2017;31:674-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Sheng L, Zhang ZY, Qian WQ, Zhang HJ, Sun ZQ. Treatment of Ureteral Fibroepithelial Polyp by Ureteroscopy Combined with Holmium Laser or Thulium Laser: A Retrospective Study. Photomed Laser Surg. 2016;34:456-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Minagawa S, Okada S, Morikawa H. Safety and Effectiveness of Holmium Laser Enucleation of the Prostate Using a Low-power Laser. Urology. 2017;110:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |