Published online Nov 6, 2021. doi: 10.12998/wjcc.v9.i31.9491
Peer-review started: February 4, 2021
First decision: March 31, 2021
Revised: April 15, 2021
Accepted: July 9, 2021
Article in press: July 9, 2021
Published online: November 6, 2021
Processing time: 266 Days and 22.2 Hours
Low vitamin D levels are associated with a more severe case of knee osteoarthritis (OA). However, there are few published reports concerning an association between vitamin D deficiency and functional status of individuals with OA and no reports about postural balance in this population.
To analyze the relationship between vitamin D deficiency and severity, functional status, and balance in elderly patients with OA.
In this cross-sectional study, 105 elderly patients with hip and knee OA were included. The severity was assessed by the Kellgren-Lawrence criteria. The functional status was assessed with the Lequesne index. Postural balance was assessed using a force platform, and center-of-pressure parameters (velocity at anteroposterior and mediolateral axis) were used as the balance outcomes. Serum 25(OH) vitamin D levels were measured using a chemiluminescence method.
Most of the patients (mean age: 70.6 ± 6.5 years) were female (n = 78, 74.3%). In the group with vitamin D deficiency, 43 patients (56.6%) had severe OA, while 33 patients (43.4%) had mild or moderate OA (χ2 test, P = 0.04). Patients with vitamin D deficiency showed a higher Lequesne index score (Mann-Whitney test, P = 0.04), indicating a worse functional impairment when compared to individuals with normal vitamin D levels. Additionally, patients with vitamin D deficiency had worse postural balance according to the Mann-Whitney test (P = 0.03).
Vitamin D deficiency is associated with worse severity, functional status, and postural balance in patients with OA.
Core Tip: This study investigated the association between vitamin D deficiency and disease severity, functional status, and postural balance in elderly patients with osteoarthritis. The severity of osteoarthritis was assessed by the Kellgren-Lawrence criteria, and the functional status was evaluated with the Lequesne index. Additionally, postural balance was evaluated using a force platform and center-of-pressure parameters. We found that vitamin D deficiency was associated with worse severity and functional status as well as worse postural balance in elderly patients with osteoarthritis.
- Citation: Montemor CN, Fernandes MTP, Marquez AS, Poli-Frederico RC, da Silva RA, Fernandes KBP. Vitamin D deficiency, functional status, and balance in older adults with osteoarthritis. World J Clin Cases 2021; 9(31): 9491-9499
- URL: https://www.wjgnet.com/2307-8960/full/v9/i31/9491.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i31.9491
Osteoarthritis (OA) is the most common degenerative disease of the osteoarticular system. Progression can affect functional status and health-related quality of life, especially in elderly patients[1,2]. It is estimated to affect about 40% of people over 70 years of age, representing a major cause of morbidity and disability worldwide[2]. It is characterized by synovial inflammation, followed by subchondral abnormalities resulting in bone reshaping[3,4]. Genetic factors as well as biomechanical stresses or changes in the articular joint and synovial membrane are important factors in the etiology of OA. Risk factors for OA are obesity, trauma, periarticular injury, and occupational factors[5-8].
Vitamin D plays an important role in calcium homeostasis and mineralization because it controls calcium and parathormone homeostasis with direct effects on bone remodeling[9]. Additionally, there is clear evidence of the benefits over different cellular functions, including muscle mass and strength. Vitamin D receptors have been identified in skeletal muscles. Vitamin D deficiency decreases receptor expression in skeletal muscles and loss of muscle mass in elderly patients[10]. Vitamin D supplementation improves quality of life and physical performance in individuals with OA[11]. On the other hand, vitamin D deficiency is a predictor of reduced muscle strength and mass as well as worse physical performance among men and women within 3 years[12].
There is evidence that vitamin D deficiency is associated with severe knee OA[13,14]. However, there are contrasting results about this topic in different populations, and the mechanisms between vitamin D and OA are not so clear[15]. Furthermore, there are only a few published reports suggesting a possible association between vitamin D deficiency and functional status of individuals with OA[16,17]. There is also a variety of methods to assess functional status. The Western Ontario and McMaster Universities (WOMAC) index and Lequesne index are the gold standards, but they are not always used. Of concern, there are no studies evaluating the association between vitamin D deficiency in patients with OA and postural balance. Therefore, this study analyzed the association between vitamin D deficiency and functional impairment and balance in elderly patients with OA.
This study was approved by the Research Ethics Committee of the University Pitagoras Unopar. Before any procedure was undertaken, patients received instruction on the nature of the work and signed a free and informed consent form in which they agreed to participate in the study.
One hundred and five elderly patients with OA from a subsample of a project on aging and longevity were included in this cross-sectional study. The project was developed in a mid-sized city in the south region of Brazil (Londrina, Paraná, Brazil), which aimed to examine the social and demographic conditions and health indicators of elderly individuals of this city. The total sample was 508 elderly patients, who were selected in a random and stratified manner from the records of the Basic Health Units from this city.
The criteria for inclusion were patients: (1) of both genders; (2) aged 60 years or older; (3) with a diagnosis of hip and/or knee OA; and (4) who had signed a free and informed consent form. The criteria for exclusion were individuals: (1) with full or partial prosthetics in any of the joints evaluated; (2) with a concomitant diagnosis of other musculoskeletal disorder, such as rheumatoid arthritis, fibromyalgia, systemic erythematosus lupus, and other rheumatic diseases; (3) with post-traumatic or postseptic arthritis; (4) with skeletal dysplasia; (5) who were human immunodeficiency virus-positive; (6) who use corticosteroids or immunosuppressive medications; and (7) who were submitted to arthroplasty (due to the impossibility of functional status assessment). Additionally, those who did not agree to sign the free and informed consent form were also excluded from the study.
A structured interview guide with questions about gender, age, weight, height, and race was used to characterize the profile of the elderly patients with OA. The formula weight (kg)/height2 (m2) was used to calculate the body mass index. Body mass index is classified as normal range (18-24.9 kg/m2), overweight (25-29.9 kg/m2), and obesity (≥ 30 kg/m2).
The Lequesne index was used to assess the functional status of these patients. This questionnaire was translated to and validated in Portuguese and is recommended by the European League of Rheumatology to evaluate OA functional status. It is comprised of 11 questions involving pain, discomfort, and functional limitation, specially related to functional status[8,18].
The diagnosis and severity of OA were based on the Kellgren-Lawrence criteria[19] by an experienced radiologist. The severity of OA was determined by the following radiographic findings scale: Grade 0, no radiographic changes; grade I, doubtful space narrowing and possible marginal osteophytes; grade II, possible joint space narrowing and defined osteophytes observed; grade III, defined joint space narrowing, moderate multiple osteophytes, subchondral sclerosis, and any possible deformity of bone contour; and grade IV, remarkable joint space narrowing, severe subchondral sclerosis, definite deformity of bone contour, and presence of large osteophytes.
Balance assessments were performed by the same trained examiner. It was quantified using a force platform (BIOMEC 400; EMG system do Brasil, SP, Ltda). The participants performed a one-legged stance on the preferred leg, barefoot with their arms at their sides parallel to their trunk and with eyes open, as described elsewhere[20]. The 95% confidence ellipse area of center of pressure (A-CoP in cm2) represents an ellipse area that includes 95% of all CoP positions during a trial. The mean CoP sway velocity (cm/s) in the anteroposterior direction was the parameter used to assess postural balance in this population[20].
Serum 25 (OH) vitamin D levels were measured using a chemiluminescence kit (Architect iSR2000; Abbott, Chicago, IL, United States). The serum 25 (OH) D level represents the storage form of vitamin D. The Brazilian Society of Endocrinology and Metabolism recommends the classification of vitamin D deficiency as serum 25
The Statistical Package for Social Sciences version 20.0 (IBM Corp., Armonk, NY, United States) was used for statistical data analyses. A CI of 95% and a significance level of 5% (P < 0.05) were used. The Mann-Whitney test was used to compare functional status and balance parameters of individuals with OA and insuffi
In this cross-sectional study, 105 elderly patients with OA were recruited. The study participants were mostly women (74.3%) with a mean age of 70.6 ± 6.5 years. The mean body mass index was 28.0 ± 4.7 kg/m2. Thirty-six individuals (34.3%) were smokers (Table 1).
| Variable | Mean | Standard deviation |
| Age; BMI | 70.6; 28.0 | 6.5; 4.7 |
| Gender; Male; Female; Total | Absolute frequency (n) ; 27; 78; 105 | Relative frequency (%); 25.7; 74.3; 100.0 |
| Tobacco use; Yes; No | Absolute frequency (n); 36; 69 | Relative frequency (%); 34.3; 65.7 |
We compared vitamin D levels and severity of OA based on the Kellgren-Lawrence criteria. The data were reorganized into mild to moderate radiographic changes (grades I and II) and severe radiographic changes (grades III and IV). There were significant differences in the prevalence of radiographic OA and vitamin D deficiency. There were more severe cases of OA (56.6%) in elderly patients with vitamin D insufficiency/deficiency (P = 0.04; Table 2).
| Vitamin D classification | Osteoarthritis severity | ||
| Mild or moderate | Severe | Total | |
| Deficiency/insufficiency | 33 (43.4) | 43 (56.6) | 76 (100.0) |
| Normal | 19 (65.6) | 10 (34.5) | 29 (100.0) |
| Total | 52 (49.5) | 53 (50.5) | 105 (100.0) |
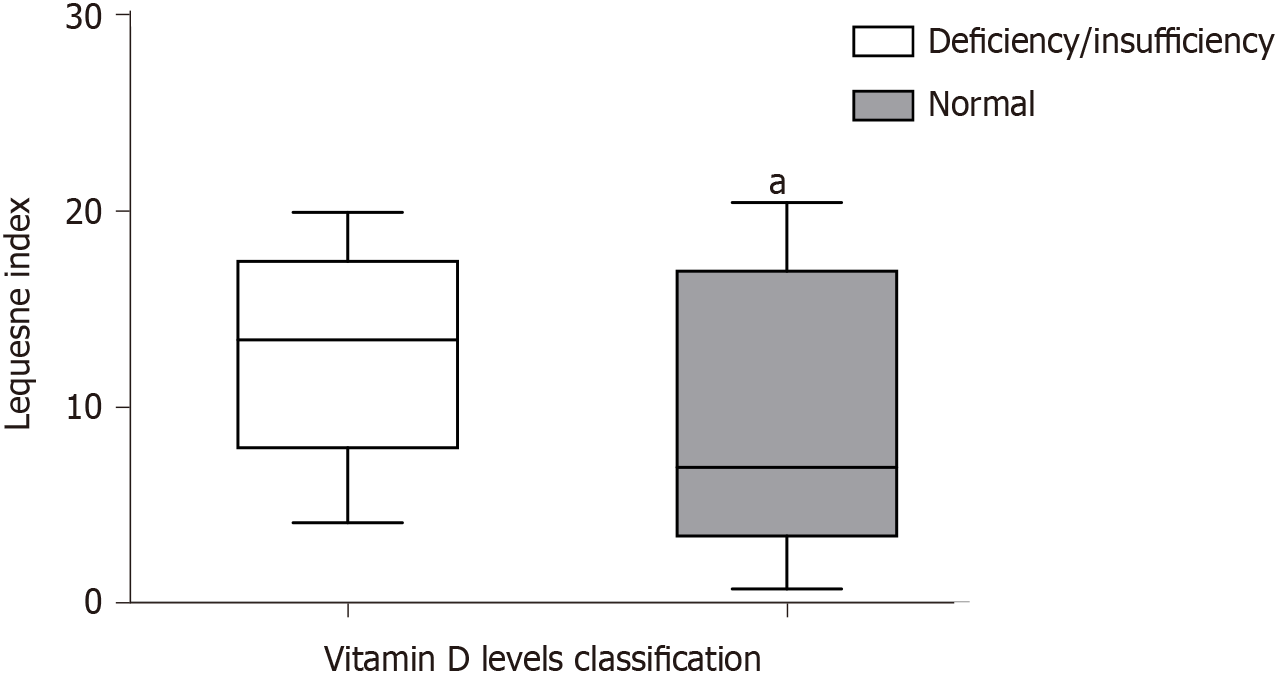
Individuals with vitamin D deficiency or insufficiency had a higher score on the Lequesne index (Mann-Whitney test, P = 0.04) when compared to patients with sufficient vitamin D levels (Figure 1). This indicated a worse functional impairment in patients with vitamin D deficiency or insufficiency.
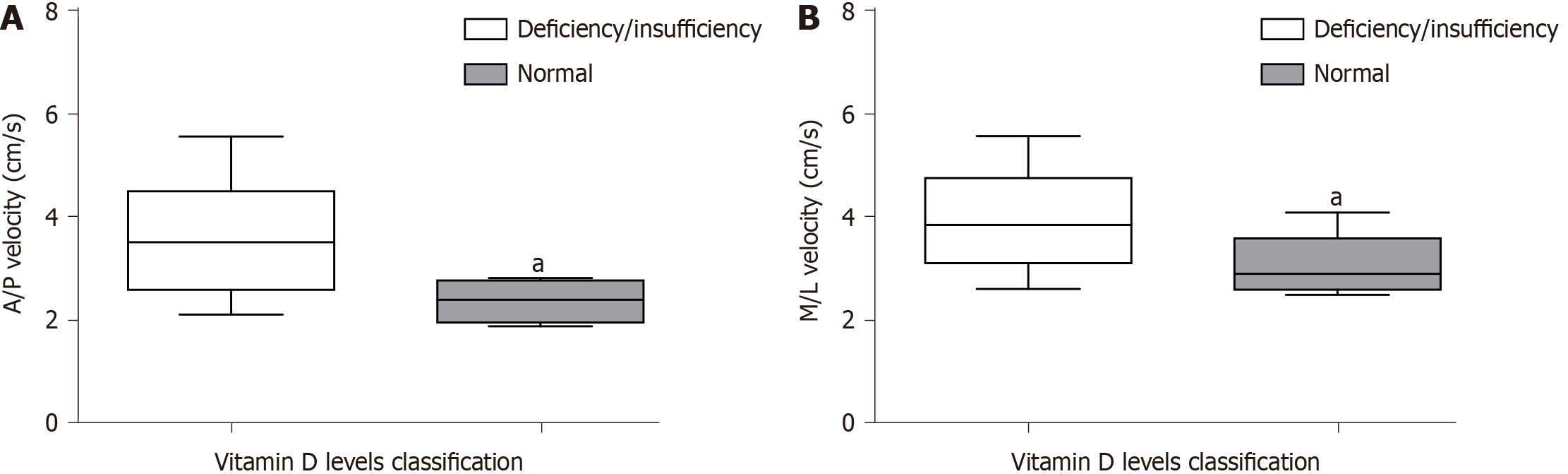
Patients with vitamin D deficiency or insufficiency had a significantly higher velocity value at the anteroposterior axis (median: 3.44 ± 1.79) when compared to patients with sufficient vitamin D levels (median: 2.18 ± 0.1; Mann-Whitney test, P = 0.03; Figure 2). Similar results were observed regarding the velocity at the mediolateral axis for patients with vitamin D deficiency or insufficiency (median: 3.86 ± 1.64) when compared to patients with sufficient vitamin D levels (median: 2.71 ± 0.10; Mann-Whitney test, P = 0.04; Figure 2).
The capacity of humans to produce vitamin D decreases in old age[16]. Furthermore, other risk factors, like malabsorptive diseases, medications that interfere with absorption, and less exposure to sunlight, increase the likelihood of vitamin D deficiency/insufficiency in the elderly population[22]. In this study, vitamin D deficiency/insufficiency impacted the severity of hip and/or knee OA. There were more severe cases in elderly patients with vitamin D deficiency/insufficiency. This data agrees with a previous report where vitamin D deficiency was associated with an advanced stage of knee OA[16]. Additionally, a case-control study found a correlation between the presence of knee osteophytes (indicating increased severity of OA) and a decrease of vitamin D[23].
A possible explanation for this observation is that vitamin D reduces the production of inflammatory cytokines[24,25]. Vitamin D influences cytokines in the synovial fluid that induce hyperalgesia and are related to the breakdown of cartilage. The major mediators are tumor necrosis factor-alpha and interleukin-1 beta, which are proinflammatory cytokines. They are produced by chondrocytes and stimulate the production of proteolytic enzymes, such as metalloproteinases. They also induce the production of other mediators, such as interleukin-6[26].
There are conflicting reports on the association between vitamin D deficiency and OA. A study of 805 Finnish patients with follow-up for 22 years found that vitamin D levels were not associated with the incidence of either knee or hip OA[24]. On the other hand, it was reported that vitamin D deficiency appeared to be associated with an increased risk of knee OA progression[27]. Additionally, the Osteoporosis Fractures in Men Study in the United States found a high prevalence of vitamin D deficiency in hip OA patients and found that these individuals were twice as likely to have hip OA[28]. The literature shows that vitamin D sufficiency can prevent the occurrence of osteoporosis of the femoral neck but not OA of the knee or lumbar spondylolysis[29].
Vitamin D deficiency or insufficiency was related to worse functional status when compared to normal levels in our patient population. Pain is the most prevalent symptom of OA that leads to functional disability. Studies comparing vitamin D levels and pain also have contrasting results[30]. In a trial of 103 knee OA patients that received oral vitamin D supplements (60000 IU per day for 10 d followed by 60000 IU once a month for 12 mo) had slightly higher pain and functional scores compared to those receiving placebos after a follow-up period of 1 year[31]. Joint function in OA is a good predictor of patient quality of life, and decreased joint function has a negative socioeconomic impact. In a study of patients with OA undergoing arthroplasty surgery, vitamin D deficiency was associated with decreased functional status scores. After the surgery, lower functional status scores were observed in patients with vitamin D deficiency, but the difference did not reach statistical significance[22].
The most novel finding of this study is that vitamin D deficiency was associated with balance impairment. CoP parameters from a force platform can directly analyze balance deficits related to proprioception and postural adjustments (feedback and feedforward) of the neuromuscular system[32]. Although the relationship between vitamin D deficiency and muscle weakness is well documented, there is almost no evidence regarding the effects of vitamin D on balance. Pfeifer et al[33] found that treatment with 800 IU of vitamin D3 per day reduced body sway in 242 elderly patients when compared with patients who received the placebo. This evidence agrees with our data. However, future studies regarding the optimal dose of vitamin D supplementation for the maximum effect with minimal side effects should be performed.
This study had some limitations. The small sample size and lack of longitudinal assessment were the main limitations of this study. This can increase the difficulty to generalize these findings for other populations and scenarios. Further multicenter studies are necessary to confirm our results as well as to elucidate the association between vitamin D deficiency and joint function and balance. More research to understand the mechanisms of vitamin D deficiency in disease development and progression will further our understanding of using vitamin D as a preventative or treatment.
Elderly patients with vitamin D deficiency and OA have worse disease severity, poor functional status, and balance deficit. Future studies with larger sample sizes are necessary to confirm these observations.
Vitamin D deficiency may be related to osteoarthritis (OA) severity and functional status. No previous studies have reported an association between vitamin D deficiency in patients with OA and postural balance.
Our study aimed to explore the severity, functional status, and postural balance in elderly patients with OA and their association with vitamin D levels. The differences might be helpful for proper evaluation and rehabilitation of these patients.
This study aimed to analyze if vitamin D deficiency/insufficiency is correlated to OA severity, functional status, and postural balance in elderly patients.
Elderly patients with hip and/or knee OA were included. Serum 25 (OH) vitamin D levels were measured using a chemiluminescence method. The severity was assessed by the Kellgren-Lawrence criteria. The functional status was evaluated with the Lequesne index. Postural balance was assessed using a force platform, and center-of-pressure parameters (velocity at anteroposterior and mediolateral axis) were used as the balance outcomes.
In this OA population, the patients with vitamin D deficiency had lower functional status than patients with sufficient vitamin D. Additionally, patients with vitamin D deficiency had worse postural balance.
Vitamin D deficiency is associated with worse severity and functional status. We found for the first time that individuals with OA and vitamin D deficiency have balance impairment.
We preliminarily explored the relationship between vitamin D levels and functional status and postural balance in elderly patients with OA. Further studies should expand the sample size and adopt a prospective study design to understand the role of vitamin D deficiency and joint function and balance.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Patel J S-Editor: Liu M L-Editor: Wang TQ P-Editor: Wang LYT
| 1. | Krasnokutsky S, Attur M, Palmer G, Samuels J, Abramson SB. Current concepts in the pathogenesis of osteoarthritis. Osteoarthritis Cartilage. 2008;16 Suppl 3:S1-S3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 131] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 2. | Sharma L, Kapoor D, Issa S. Epidemiology of osteoarthritis: an update. Curr Opin Rheumatol. 2006;18:147-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 196] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 3. | Johnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol. 2014;28:5-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 546] [Cited by in RCA: 678] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 4. | Goldring MB, Otero M, Tsuchimochi K, Ijiri K, Li Y. Defining the roles of inflammatory and anabolic cytokines in cartilage metabolism. Ann Rheum Dis. 2008;67 Suppl 3:iii75-iii82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 180] [Cited by in RCA: 175] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 5. | Harvey WF, Hunter DJ. Pharmacologic intervention for osteoarthritis in older adults. Clin Geriatr Med. 2010;26:503-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Vina ER, Kwoh CK. Epidemiology of osteoarthritis: literature update. Curr Opin Rheumatol. 2018;30:160-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 655] [Article Influence: 93.6] [Reference Citation Analysis (0)] |
| 7. | Martel-Pelletier J, Barr AJ, Cicuttini FM, Conaghan PG, Cooper C, Goldring MB, Goldring SR, Jones G, Teichtahl AJ, Pelletier JP. Osteoarthritis. Nat Rev Dis Primers. 2016;2:16072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 660] [Cited by in RCA: 1196] [Article Influence: 132.9] [Reference Citation Analysis (0)] |
| 8. | Marx FC, Oliveira LM, Bellini CG, Ribeiro MCC. Tradução e validação cultural do questionário algofuncional de Lequesne para osteoartrite de joelhos e quadris para a língua portuguesa. Rev Bras Reumatol. 2006;46:253-260. |
| 9. | Rizzoli R, Stevenson JC, Bauer JM, van Loon LJ, Walrand S, Kanis JA, Cooper C, Brandi ML, Diez-Perez A, Reginster JY; ESCEO Task Force. The role of dietary protein and vitamin D in maintaining musculoskeletal health in postmenopausal women: a consensus statement from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Maturitas. 2014;79:122-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 182] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 10. | Bischoff-Ferrari HA, Borchers M, Gudat F, Dürmüller U, Stähelin HB, Dick W. Vitamin D receptor expression in human muscle tissue decreases with age. J Bone Miner Res. 2004;19:265-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 369] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 11. | Manoy P, Yuktanandana P, Tanavalee A, Anomasiri W, Ngarmukos S, Tanpowpong T, Honsawek S. Vitamin D Supplementation Improves Quality of Life and Physical Performance in Osteoarthritis Patients. Nutrients. 2017;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 73] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 12. | Visser M, Deeg DJ, Lips P; Longitudinal Aging Study Amsterdam. Low vitamin D and high parathyroid hormone levels as determinants of loss of muscle strength and muscle mass (sarcopenia): the Longitudinal Aging Study Amsterdam. J Clin Endocrinol Metab. 2003;88:5766-5772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 797] [Cited by in RCA: 748] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 13. | Houston DK, Tooze JA, Neiberg RH, Hausman DB, Johnson MA, Cauley JA, Bauer DC, Cawthon PM, Shea MK, Schwartz GG, Williamson JD, Tylavsky FA, Visser M, Simonsick EM, Harris TB, Kritchevsky SB; Health ABC Study. 25-hydroxyvitamin D status and change in physical performance and strength in older adults: the Health, Aging, and Body Composition Study. Am J Epidemiol. 2012;176:1025-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 14. | Boland RL. VDR activation of intracellular signaling pathways in skeletal muscle. Mol Cell Endocrinol. 2011;347:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (1)] |
| 15. | Hussain S, Singh A, Akhtar M, Najmi AK. Vitamin D supplementation for the management of knee osteoarthritis: a systematic review of randomized controlled trials. Rheumatol Int. 2017;37:1489-1498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Jansen JA, Haddad FS. High prevalence of vitamin D deficiency in elderly patients with advanced osteoarthritis scheduled for total knee replacement associated with poorer preoperative functional state. Ann R Coll Surg Engl. 2013;95:569-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Mermerci Başkan B, Yurdakul FG, Aydın E, Sivas F, Bodur H. Effect of vitamin D levels on radiographic knee osteoarthritis and functional status. Turk J Phys Med Rehabil. 2018;64:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Lequesne MG. The algofunctional indices for hip and knee osteoarthritis. J Rheumatol. 1997;24:779-781. [PubMed] |
| 19. | Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9311] [Cited by in RCA: 8870] [Article Influence: 130.4] [Reference Citation Analysis (0)] |
| 20. | Oliveira MR, Vieira ER, Gil AWO, Fernandes KBP, Teixeira DC, Amorim CF, da Silva RA. One-legged stance sway of older adults with and without falls. PLoS One. 2018;13:e0203887. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Maeda SS, Saraiva GL, Kunii IS, Hayashi LF, Cendoroglo MS, Ramos LR, Lazaretti-Castro M. Factors affecting vitamin D status in different populations in the city of São Paulo, Brazil: the São PAulo vitamin D Evaluation Study (SPADES). BMC Endocr Disord. 2013;13:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Kupisz-Urbańska M, Płudowski P, Marcinowska-Suchowierska E. Vitamin D Deficiency in Older Patients-Problems of Sarcopenia, Drug Interactions, Management in Deficiency. Nutrients. 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 23. | Hunter DJ, Hart D, Snieder H, Bettica P, Swaminathan R, Spector TD. Evidence of altered bone turnover, vitamin D and calcium regulation with knee osteoarthritis in female twins. Rheumatology (Oxford). 2003;42:1311-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 87] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Barker T, Martins TB, Hill HR, Kjeldsberg CR, Dixon BM, Schneider ED, Henriksen VT, Weaver LK. Vitamin D sufficiency associates with an increase in anti-inflammatory cytokines after intense exercise in humans. Cytokine. 2014;65:134-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | Konstari S, Kaila-Kangas L, Jääskeläinen T, Heliövaara M, Rissanen H, Marniemi J, Knekt P, Arokoski J, Karppinen J. Serum 25-hydroxyvitamin D and the risk of knee and hip osteoarthritis leading to hospitalization: a cohort study of 5274 Finns. Rheumatology (Oxford). 2014;53:1778-1782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Goldring MB, Otero M. Inflammation in osteoarthritis. Curr Opin Rheumatol. 2011;23:471-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 857] [Cited by in RCA: 1052] [Article Influence: 75.1] [Reference Citation Analysis (0)] |
| 27. | McAlindon TE, Felson DT, Zhang Y, Hannan MT, Aliabadi P, Weissman B, Rush D, Wilson PW, Jacques P. Relation of dietary intake and serum levels of vitamin D to progression of osteoarthritis of the knee among participants in the Framingham Study. Ann Intern Med. 1996;125:353-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 263] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 28. | Chaganti RK, Parimi N, Cawthon P, Dam TL, Nevitt MC, Lane NE. Association of 25-hydroxyvitamin D with prevalent osteoarthritis of the hip in elderly men: the osteoporotic fractures in men study. Arthritis Rheum. 2010;62:511-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 29. | Yoshimura N, Muraki S, Oka H, Nakamura K, Kawaguchi H, Tanaka S, Akune T. Serum levels of 25-hydroxyvitamin D and the occurrence of musculoskeletal diseases: a 3-year follow-up to the road study. Osteoporos Int. 2015;26:151-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Mabey T, Honsawek S. Role of Vitamin D in Osteoarthritis: Molecular, Cellular, and Clinical Perspectives. Int J Endocrinol. 2015;2015:383918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 31. | Sanghi D, Mishra A, Sharma AC, Singh A, Natu SM, Agarwal S, Srivastava RN. Does vitamin D improve osteoarthritis of the knee: a randomized controlled pilot trial. Clin Orthop Relat Res. 2013;471:3556-3562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 105] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 32. | Winter DA. Human balance and posture control during standing and walking. Gait Posture. 1995;3:193-214. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1913] [Cited by in RCA: 1731] [Article Influence: 57.7] [Reference Citation Analysis (0)] |
| 33. | Pfeifer M, Begerow B, Minne HW, Suppan K, Fahrleitner-Pammer A, Dobnig H. Effects of a long-term vitamin D and calcium supplementation on falls and parameters of muscle function in community-dwelling older individuals. Osteoporos Int. 2009;20:315-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 330] [Cited by in RCA: 312] [Article Influence: 19.5] [Reference Citation Analysis (0)] |