Published online Jan 26, 2021. doi: 10.12998/wjcc.v9.i3.722
Peer-review started: November 6, 2020
First decision: November 20, 2020
Revised: November 23, 2020
Accepted: December 6, 2020
Article in press: December 6, 2020
Published online: January 26, 2021
Processing time: 75 Days and 9.2 Hours
Bimaxillary protrusion is a clinically common dentofacial deformity, particularly among Chinese patients. This kind of malformation can severely affect facial esthetics and, even in mild cases, is difficult to correct without surgery. Unfortunately, many patients abandon treatment because of fear of surgery. Here, we describe a case of severe skeletal bimaxillary protrusion treated with nonsurgical orthodontic treatments, highlighting an alternative treatment option.
A 31-year-old woman wished to address a severe protrusion profile (approximately 8 mm overbite) and gummy smile. Cephalometric analysis and superimposition showed a severe skeletal class II pattern with a mandibular retrusion, and proclined and protrusive mandibular incisors. Panoramic radiograph showed a missing mandibular right third molar. A diagnosis of severe bimaxillary dentoalveolar protrusion was made. Taking into account the patient’s fear of orthognathic surgery, she accepted the proposed alternative treatment using micro-implants and a self-made four-curvature torquing auxiliary. The treatment allowed for maximal en masse anterior tooth retraction, proper relocation of incisors, and alleviation of the skeletal class II pattern. Esthetically, the patient’s lip protrusion was significantly decreased as was the overjet (from 10.5 mm to 1.8 mm), and the results remained stable throughout the 2-year follow-up.
Nonsurgical treatment using micro-implants and a four-curvature torquing auxiliary may benefit severe cases of skeletal bimaxillary protrusion in adults.
Core Tip: Nonsurgical orthodontic treatments can benefit cases of severe skeletal bimaxillary protrusion in adults who fear the traditional orthognathic surgical procedures. Success of such nonsurgical alternatives will depend on control of four key factors, namely, maximal en masse anterior tooth retraction, proper relocation of the incisors, ultimate alleviation of the skeletal class II pattern, and sufficient treatment time. Using such an approach, with micro-implants and a self-made four-curvature torquing auxiliary, we significantly decreased a patient’s severe lip protrusion and overjet, with results remaining stable through the 2-year follow-up.
- Citation: Liu R, Hou WB, Yang PZ, Zhu L, Zhou YQ, Yu X, Wen XJ. Severe skeletal bimaxillary protrusion treated with micro-implants and a self-made four-curvature torquing auxiliary: A case report. World J Clin Cases 2021; 9(3): 722-735
- URL: https://www.wjgnet.com/2307-8960/full/v9/i3/722.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i3.722
Bimaxillary protrusion is a common dentofacial deformity encountered in clinical practice, particularly in Chinese patients. This kind of malformation not only results in functional problems but also severely affects facial esthetics and, consequently, the self-esteem of the afflicted individual. The presence of bimaxillary protrusion is generally associated with a strong desire to change the facial profile that is perceived as unattractive. However, it is difficult for orthodontists to completely correct severe bimaxillary dentoalveolar protrusion without surgery, especially in cases that also present chin retraction or skeletal class II profile.
Currently, a combination approach of orthodontics and orthognathic surgery is the most efficient treatment option for improving the facial profile of patients with severe bimaxillary dentoalveolar protrusion. Although, many patients fear the surgery and deny or drop out of the treatment process. Micro-implants are widely considered the best tools to provide absolute anchorage for orthodontics. Application of micro-implants has proven to be a convenient method to achieve maximal retraction of protrusive anterior teeth, representing an alternative to surgery for patients with severe skeletal bimaxillary protrusion who are unwilling to undergo surgery[1,2]. Micro-implants have also been shown to provide stable and efficient anchorage, thereby protecting against mesial movement of the molars[3,4]. It has also been reported that micro-implants can facilitate whole arch distalization[1,5]. Indeed, more and more orthodontic procedures that benefit patients with severe bimaxillary protrusion may be carried out with micro-implants, bypassing the need for surgery[3-5].
Despite the successful applications of micro-implants in bimaxillary protrusion patients (i.e., significantly increasing the retraction of anterior teeth), a new challenge arose in incisor torque control. The long-distance retraction, unfortunately, results in linguoclination of the incisors, negating the improvement in facial esthetics. Herein, we report the nonsurgical treatment of an adult female patient with severe dentoalveolar protrusion, using micro-implants and a self-made four-curvature torquing auxiliary, respectively, to control the molars’ anchorage and incisors’ torque. Ultimately, the patient’s lip protrusion was significantly improved and an ideal lateral profile was obtained, highlighting the potential benefit that this alternative nonsurgical option may provide for individuals with this type of dentofacial deformity.
A Chinese woman, aged 31 years and 1 mo, presented to our clinic on July 1, 2013 with the chief complaints of a severe protrusion profile and gummy smile.
The patient reported having recently noticed her protrusion profile, citing a negative effect on her self-esteem and a strong desire to correct her facial profile.
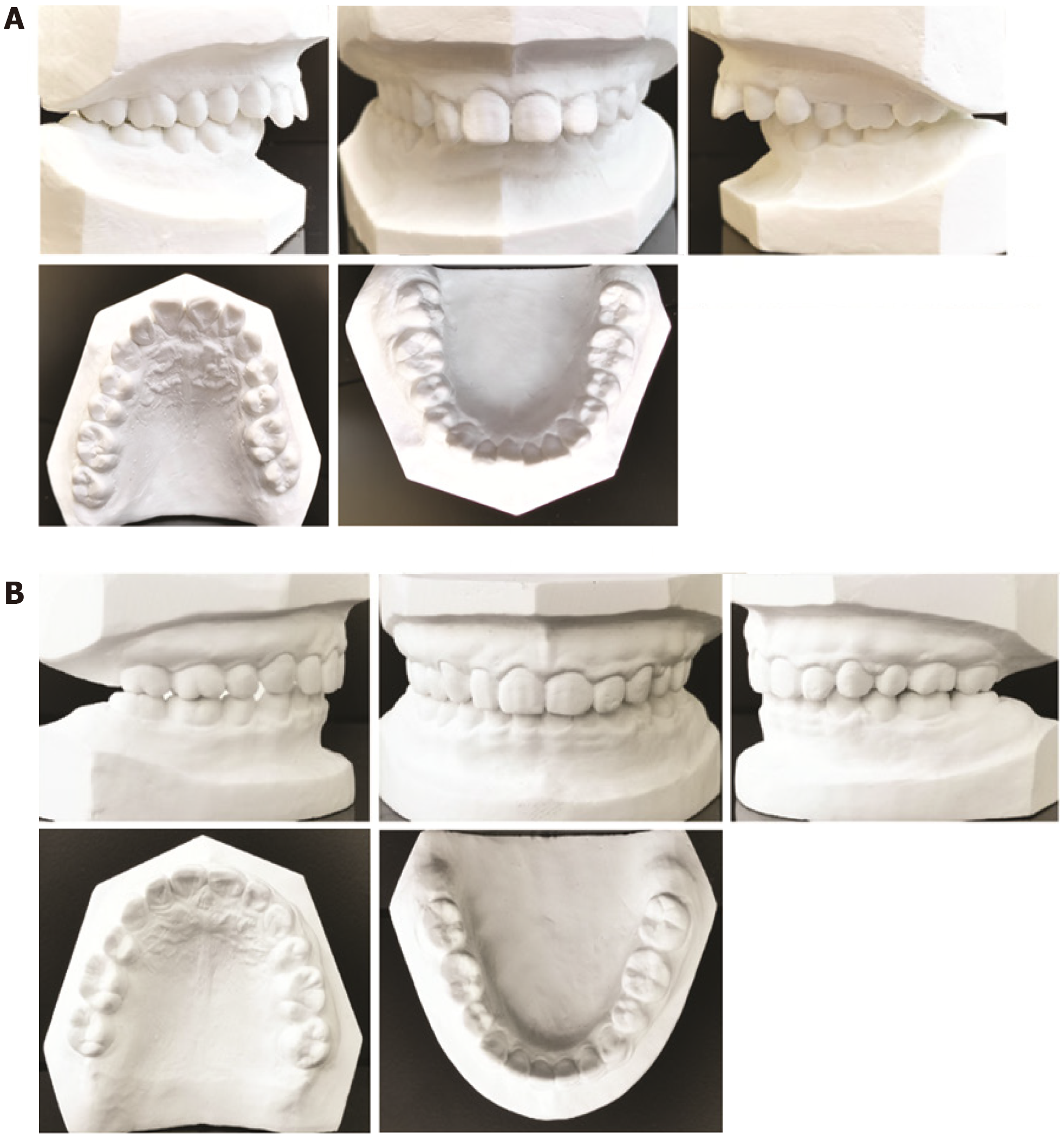
Clinical examination revealed the presence of dentoalveolar protrusion and full class II molar relationships, with an overjet of 10.5 mm (Figures 1 and 2). A deep overbite (approximately 8 mm) was also found. The left first premolar and second molar had positive crossbite. There was almost no crowding in either arch and no obvious temporomandibular joint disease was found.
Model analysis and imaging examinations: Model analysis showed arch length discrepancies of 0.0 mm on the maxillary arch and -1.5 mm on the mandibular arch (Figure 2A). Bolton’s indexes were 76.90% for the anterior ratio and 89.56% for the overall ratio, both of which were slightly lower than the normal reference range (78.80% ± 1.72% and 91.50% ± 1.51%, respectively). The Spee’s curve was 5.0 mm in the mandibular arch.
The cephalometric analysis and superimposition were performed with Uceph software (Online version 3.1.1, build 508; Sichuan University, Chengdu, China). The data (summarized in Table 1) indicated a severe skeletal class II pattern with a mandibular retrusion, proclined and protrusive mandibular incisors, and protrusive upper and lower lips. Panoramic radiography showed the mandibular right third molar to be missing (Figure 1).
| Measurement | Norm ± SD | Pretreatment (July 2013) | Leveling and aligning (June 2014) | Progress I (Oct, 2015) | Progress II (Sep, 2016) | Posttreatment (Jun, 2017) | Retention (Mar, 2019) |
| SNA | 82.8 ± 4.0 | 82.5 | 82.0 | 81.0 | 81.0 | 80.5 | 80.5 |
| SNB | 80.1 ± 3.9 | 71.0 | 76.0 | 72.5 | 72.5 | 72.5 | 72.6 |
| ANB | 2.7 ± 2.0 | 11.5 | 6.0 | 8.5 | 8.5 | 8.0 | 7.9 |
| SND | 77.3 ± 3.8 | 70.0 | 73.0 | 70.0 | 71.0 | 71.0 | 71.3 |
| U1-NA (mm) | 5.1 ± 2.4 | 5.0 | 6.8 | -0.7 | 1.8 | 2.0 | 1.8 |
| U1-NA | 22.8 ± 5.7 | 25.7 | 31.1 | 6.0 | 8.0 | 10.0 | 9.5 |
| L1-NB (mm) | 6.7 ± 2.1 | 10.0 | 13.6 | 6.4 | 7.2 | 6.5 | 6.0 |
| L1-NB | 30.3 ± 5.8 | 30.7 | 42.5 | 29.0 | 24.5 | 24.0 | 24.5 |
| U1-L1 | 124.2 ± 8.2 | 116.0 | 95.5 | 136.0 | 139.0 | 135.0 | 137.9 |
| GoGn-SN | 32.5 ± 5.2 | 33.4 | 33.8 | 33.1 | 33.7 | 33.0 | 33.3 |
| SE | 20.2 ± 2.6 | 17.9 | 17.1 | 20.0 | 17.0 | 17.0 | 16.5 |
| SL | 52.1 ± 5.4 | 44.3 | 40.1 | 38.6 | 36.0 | 36.0 | 36.5 |
| FMA | 31.3 ± 5.0 | 31.0 | 31.6 | 31.1 | 30.5 | 30.3 | 30.5 |
| FMIA | 54.9 ± 6.1 | 46.0 | 34.0 | 45.0 | 52.0 | 52.0 | 53.2 |
| IMPA | 93.9 ± 6.2 | 103.0 | 114.0 | 102.0 | 98.0 | 98.0 | 96.5 |
| UL-EP (mm) | 1.0 ± 2.0 | 7.0 | 6.8 | 2.4 | 0.2 | -0.7 | -0.7 |
| LL-EP (mm) | -1.0 ± 1.0 | 4.0 | 2.1 | 0.5 | -0.8 | -1.2 | -1.3 |
| Pog-Pog′ (mm) | 9.9 ± 2.1 | 14.2 | 14.6 | 16.8 | 16.4 | 16.7 | 17.1 |
| Gn-Gn′ (mm) | 6.0 ± 2.2 | 4.5 | 6.0 | 6.6 | 7.3 | 7.7 | 8.3 |
| Me-Me′ (mm) | 6.5 ± 2.1 | 6.5 | 6.3 | 7.1 | 6.3 | 6.6 | 6.8 |
Dental and skeletal class II bimaxillary protrusion; gummy smile; severe deep overjet and overbite; mandibular retrusion; tooth midline inconsistency; left first premolar and second molar positive crossbite.
The following four treatment alternatives were devised and proposed to the patient.
The first treatment option was the most traditional, involving a combination of orthodontics and orthognathic surgery to improve the facial profile. Alignment and leveling would first be achieved by orthodontic appliances, after which an anterior segmental osteotomy combined with two upper first premolar extractions would be performed in the single maxilla. The orthodontic treatment would then resume to achieve a functional intercuspal occlusion and sustainable full class II relationships for the bilateral molars.
The second treatment option also used the traditional approach of combined orthodontics and orthognathic surgery to improve the facial profile. The only difference was that both jaws would undergo an anterior segmental osteotomy combined with extraction of the four first premolars and simultaneous bilateral sagittal split ramus osteotomy (the latter to advance the mandible). Ultimately, the skeletal class II and full class II molar relationships would be corrected to class I.
The third treatment option excluded the traditional surgical approach and relied on orthodontics with extraction of the two upper first premolars. Two micro-implants would be used to avoid molar mesialization and maximize the retraction of the upper anterior teeth. By this option, the bilateral full class II molar relationships would be maintained and class I canine relationships would be established.
The fourth treatment option excluded the traditional surgical approach, similar to option 3, relying on orthodontics but with extraction of the four first premolars. Four micro-implants would be used to provide an absolute anchorage and to maximize the retraction of both upper and lower anterior teeth, especially in the maxillary arch. In this approach, advancement of the mandibular arch and distalization of the upper whole arch would also be required to reduce the anteroposterior skeletal discrepancy and establish the class I molar relationship.
The patient cited her fear of orthognathic surgery in her selection of treatment option 4.
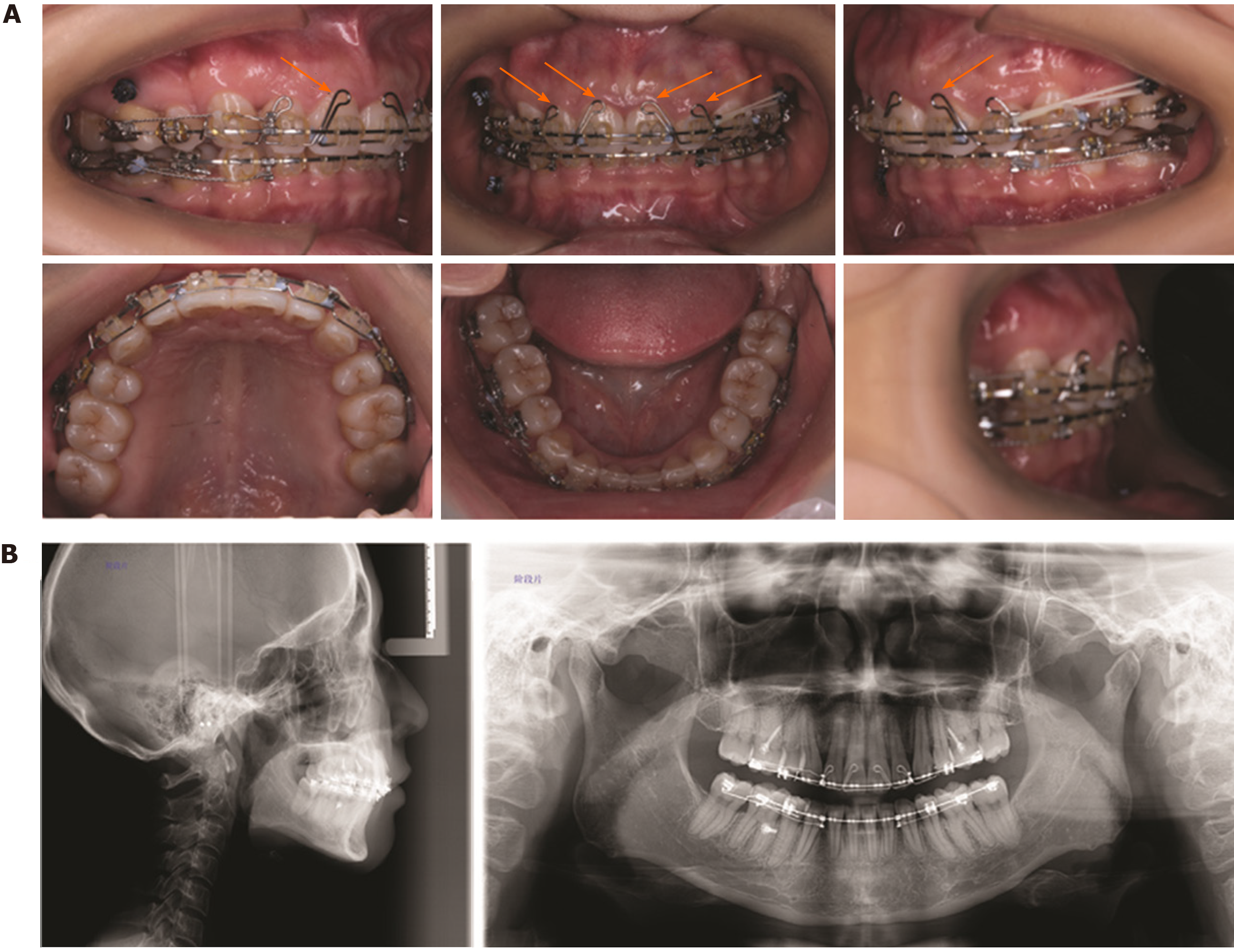
Before the orthodontic treatment portion began, three third molars were extracted. The 0.022-inch preadjusted brackets were bonded to the maxillary teeth, excluding the second molars. A series of superelastic nickel-titanium alloy archwires (0.012-inch, 0.016-inch, 0.016-inch × 0.022-inch) were used for the initial leveling and aligning. At 6 mo later, a removable anterior inclined plane was used to advance the mandible and release the bite lock of the positive crossbite of the left first premolars and second molars. At the same time, the 0.022-inch preadjusted brackets were bonded to the mandibular teeth, including the left second molar. Another 6 mo later, use of the anterior inclined plane was stopped, when both arches had achieved leveling by 0.019 × 0.025-inch stainless steel wires (Figure 3). At this time, the positive crossbites of the left first premolars and second molars were corrected and the deep overbite and overjet were significantly improved.
In the 14th month of treatment, the patient was referred for extraction of the four first premolars. At 1 mo post-extraction, four micro-implants (1.4 mm × 8 mm; Ormco, Orange, CA, United States) were placed between the second premolars and first molars in each quadrant. Another 1 mo later, the en masse retraction of the anterior teeth was initiated with 3.5-ounce orthodontic rubber bands (5/16) being applied from the micro-implants to short hooks fixed on the wire between the lateral incisor and the canine in each quadrant. Bilateral class II elastics were used simultaneously to continue advancement of the mandible and help establish the class I molar relationship.
In the 27th month of treatment, the extraction spaces had closed by about 3/4 (Figure 4). However, the maxillary incisors were found to be seriously up-righted. In order to prevent the up-righted maxillary incisors becoming worse, a self-made four-curvature torquing auxiliary was used in the following treatment of en masse retraction. The following 11 mo of treatment ended with all the extraction spaces becoming closed (Figure 5).
The total treatment duration was 48 mo. After removal of all the fixed appliances (Figures 2B and 6), a Hawley retainer was prescribed for 24 h/d use for 6 mo followed by nightly use for about 2 years.
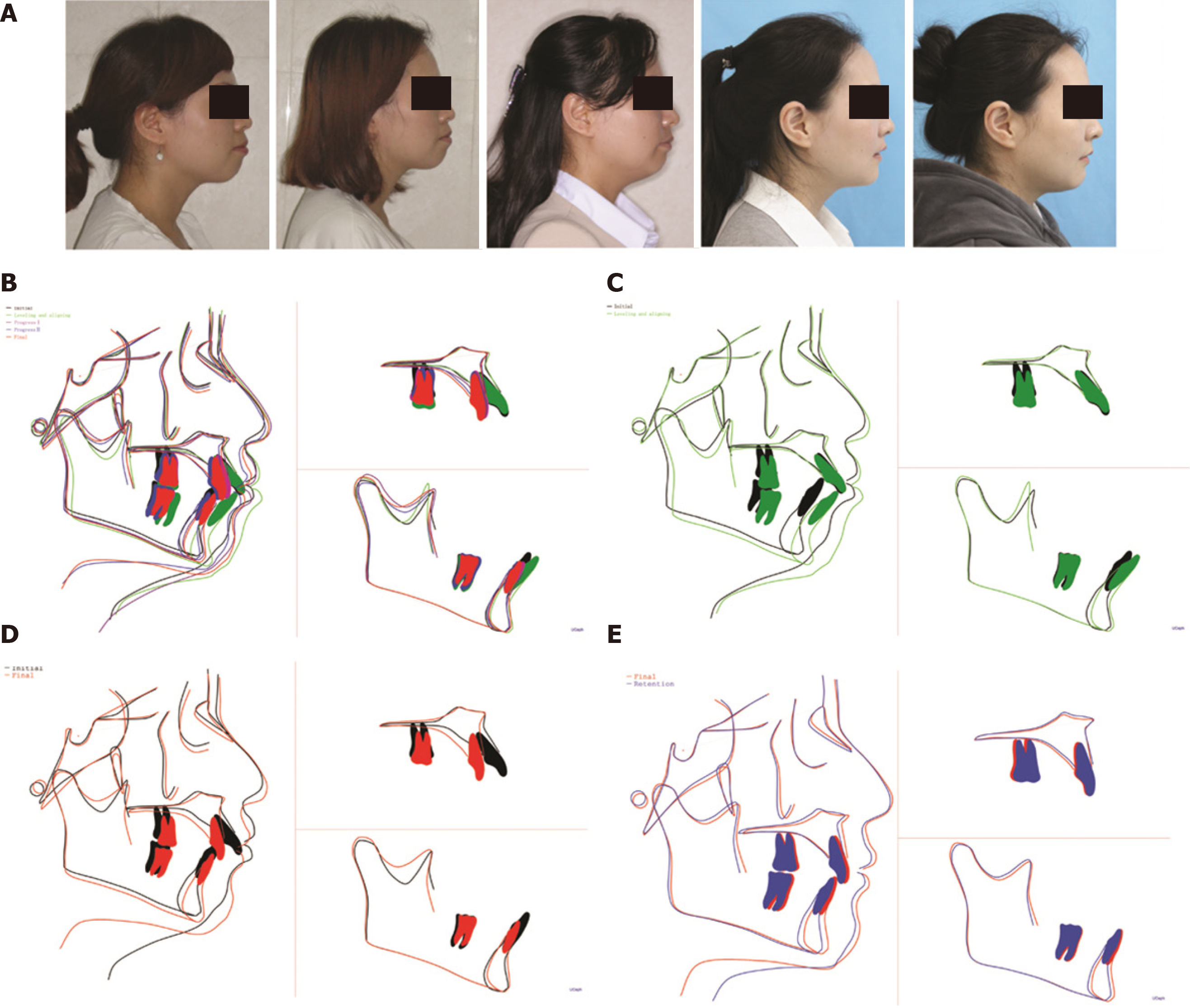
In the retention stage, the patient attended follow-up visits once every 3 mo; the results at the end of 2 years of follow-up are shown in Figure 7. The patient reported being “very satisfied” with her post-treatment lateral profile, with the lip protrusion being significantly decreased (Figures 6 and 8A). The appearance was similar to that achieved by traditional orthognathic surgery. The final overjet decrease was substantial, from 10.5 mm to 1.8 mm (Figure 2B). The canines and molars achieved class I relationships on the left. In contrast, however, the class II relationships on the right were not completely corrected, and midlines retained an approximately 1.5 mm discrepancy.
The soft tissue profile changes achieved by the orthodontic treatment were remarkable (Figures 1 and 6). An ideal chin contour was obtained, as the upper lip to E-line distance was significantly decreased as was the lower lip to E-line distance (Table 1). The soft tissue thickness of the chin was also increased (Figure 8B and D, and Table 1).
The incisor protrusion and torque varied greatly throughout the treatment period, as shown by the cephalometric measurements (Table 1) and the superimposition modeling (Figure 8B-E). The incisor protrusion and torque were increased at the initial stage of the teeth alignment and leveling. With the four premolars extracted and anterior teeth en masse retracted, the nasion to point A and nasion to point B measurements for the upper incisor and lower incisor were dramatically decreased at the progress I stage (Figure 4 and Table 1). In contrast, the up-righted result of the maxillary incisors was undesirable. In order to deal with this problem, a self-made four-curvature torquing auxiliary was used over the following 22 mo, resulting in a great improvement, even in the anterior teeth retraction stage. The cephalometric superimposition (Figure 8D) showed that the sagittal anchorage was well controlled, with only slight mesial movement detected in the mandibular molars.
Skeletal changes were also achieved. The skeletal class II correlation was greatly improved, with the point A-nasion-point B (ANB) angle sufficiently decreased (Table 1). The ANB angle remarkably decreased at the beginning stage of leveling and aligning because of the use of a removable anterior inclined plane, stabilizing at approximately 8.0°. The Sella-nasion-point B (SNB) angle increased initially, then decreased and stabilized at approximately 72.5°. The underlying reason for this outcome likely involved the forward movement of the mandibular position (achieved by the removable anterior inclined plane) being instable and partly relapsing. The mandibular plane angle, however, was well maintained, as the angle between the SN planes and mandibular plane (known as GoGn-SN) and the Frankfort to mandibular plane angle (commonly referred to as FMA) remained stable throughout the entire treatment (Table 1).
The latest follow-up visit occurred at 2-year post-treatment (Figure 7) and the results were found to be stable (Figure 8E). The collective data from this case presentation through treatment follow-up (i.e. photographs, cephalometric analysis, and superimposition) showed that the combination approach of micro-implants and a self-made four-curvature torquing auxiliary is efficient and a feasible alternative option for patients who fear surgery but seek to correct their skeletal bimaxillary protrusion.
Esthetic correction of facial profile is a common desire expressed by patients with bimaxillary protrusion. Lip protrusion, chin morphology, and mentolabial sulcus depth are considered the key parameters correlated to facial esthetics[6]. In our case report, the patient initially presented a complaint of inaesthetic appearance, due to large lip protrusion, severe chin retraction, and deep overjet. After nonsurgical treatment using micro-implants and a self-made four-curvature torquing auxiliary, the protrusion of the upper and lower lips was significantly retracted. An ideal chin morphology and excellent facial balance were also achieved. In evaluating the measurable changes of hard and soft tissues before and after treatment, we identified four factors of importance to the final outcome.
The first factor was the absolute anchorage facilitated by the micro-implants. As we know, preventing the mesial movement of molars is crucial in treatment of severe skeletal bimaxillary protrusion; it is necessary that the whole extraction space can be used for the maximal retraction of anterior incisors. In the past, it was difficult to obtain absolute anchorage with the various conventional anchorage devices that were applied in clinic. The advent of temporary skeletal anchorage devices, such as mini-implants and mini-screws, has overcome this problem[7]. In our patient, the sagittal anchorage was well controlled, as evidenced by the cephalometric superimpositions and the no or little mesial movement that was detected in the molars of both jaws. Almost the entirety of each extraction space was used for the anterior teeth retraction. The outcomes of our case further confirm that micro-implants are a reliable anchorage tool. With the help of micro-implants, more and more clinicians can devise and implement effective nonsurgical orthodontic treatment of patients with severe skeletal bimaxillary protrusion. It is important to note here that obtaining absolute anchorage is not the be-all-end-all aim of nonsurgical treatment of severe skeletal bimaxillary protrusion.
Proper relocation of the incisor position is the second crucial factor to obtain a good lateral profile; this is because the function of the upper and lower lips mainly depends on incisor position, especially the upper incisor position[6]. Incisor relocation and the subsequent lip retraction may have remarkable influence on the subjective facial esthetics of bimaxillary protrusion patients[8,9]. Although the maximal retraction of anterior teeth becomes easier, and even the whole arch distalization could be achieved with micro-implants, it is still perplexing to orthodontists why some patients obtain a good lateral profile while others do not[10,11]. It is possible that the improper relocation of maxillary and mandibular incisors is the answer that the perplexed orthodontists should focus on. In our patient, the anterior incisors were greatly retracted in the initial stage of space-closing, as four micro-implants were used. Undesirably, however, the maxillary incisors were seriously up-righted, which proved an obstacle to further improvement of the lateral profile. The presence of up-righted maxillary incisors, namely, the clockwise rotation of the incisor axis itself, meant that the roots of the teeth would eventually become more protrusive, preventing adequate upper lip retraction. Moreover, this compelled the lower jaw to shift further back and the chin morphology to become worse. We solved this problem by the subsequent use of a self-made four-curvature torquing auxiliary, which proved an efficient tool to reverse the up-righted maxillary incisors during the en masse retraction stage. Compared with some torque control methods reported previously[12,13] (such as high-torque appliances, reverse-curve arch, and positive or negative torque pre-adjusted in stainless steel rectangular wire), the self-made four-curvature torquing auxiliary used in this case report has a much longer arm of force that significantly facilitates the incisor torque expression. Besides, it could meet the different incisor torque expression needs of individual patients by changing its force sizes and treatment time.
The third factor important for improvement of facial esthetics is alleviation of the skeletal class II relationship. It has been reported that patients with bimaxillary protrusion generally display a mild class II skeletal pattern[14,15]. The retrusive chin makes the lip protrusion more visibly obvious, further worsening the lateral profile. In our patient, the ANB angle was 11.5° before treatment, displaying a serious skeletal class II pattern. This increased the difficulty of correction without orthognathic surgery. Our treating orthodontists recognized that a maximal incisor retraction was needed in conjunction with good incisor torque control. Without such, the long distance of retraction could easily result in maxillary incisor up-right or lingual inclination, which would compel the lower jaw to draw back and worsen the skeletal class II pattern. This phenomenon has been reported by Mukaida et al[16], whose patient achieved a 1° increase in ANB angle (from 4.5° to 5.5°) and 28° decrease in U1-Frankfort horizontal (referred to as FH) angle (from 128° to 100°) by the end of treatment. Similar results were reported by both Kook et al[5], whose patient achieved a 2° increase in ANB angle (from 3.5° to 5.5°) and 35° decrease in U1-FH angle (from 135° to 100°), and Chung et al[17] , whose patient achieved a 1° increase in ANB angle (from 4.3° to 5.3°) and 18.1° decrease in the angle between the long axis of the maxillary central incisor and the nasion point (referred to as Mx1-NA) (from 17.3° to -0.8°). This undesired result greatly offsets the lateral profile improvement that would otherwise have resulted from the anterior incisors’ retraction. In our case, the ANB angle was not only increased but remarkably decreased (by 3.5°), contributing to the perfect lateral profile at post-treatment. Alleviation of the skeletal class II relationship would be better if the self-made four-curvature torquing auxiliary was used at the beginning of the extraction space-closing. Thus, the decrease of the upper incisor-nasion angle would be smaller and leave more space for the lower jaw to move forward. Besides, the decrease of the ANB angle was partly due to the reconstruction of point A (the SNA angle: From 82.5° at pretreatment to 80.5° at post-treatment) resulting from the maximal en masse retraction of anterior teeth. Of course, further studies are needed to reveal the mechanism that underlies the alleviation of skeletal class II relationship in adult patients.
The fourth factor involves having sufficient time in which the treatment can achieve alveolar bone remodeling, which we believe was essential for our patient to obtain the satisfactory lateral profile. If the speed of incisor retraction is too fast, the labial alveolar bone remodeling will fail to keep with the upper lip, hindering retraction of the latter. In a report by Mimura et al[4], the active treatment time was about 20 mo. Their patient’s upper anterior teeth were well intruded and retracted but the maxillary alveolar process failed to remodel and leave behind a prominent labial ridge of bone, which prevented decrease of the upper lip protrusion. An alveoloplasty had to be carried out at the end of orthodontic treatment, to recontour the labial bone and the incisive fossae. This kind of unusual bony change in the maxillary alveolar process during orthodontic treatment has also been reported by others[4]. For our case, the active treatment time was 48 mo, which provided sufficient time for the alveolar bone to remodel. Therefore, there was no labial bone ridge or unusual bony outgrowth in our patient.
A surgery was avoided and an excellent lateral profile was obtained in our adult patient with severe bimaxillary protrusion, skeletal class II, and chin retraction. The overall case data indicated that the combination of micro-implants and our self-made four-curvature torquing auxiliary provided an alternative feasible option for cases of severe bimaxillary protrusion in patients who fear surgery. If the four key factors are well controlled—namely, maximal en masse anterior tooth retraction, proper relocation of incisors, alleviation of skeletal class II pattern, and sufficient treatment time—we can devise and implement more nonsurgical orthodontic treatments for adult patients with severe skeletal bimaxillary protrusion.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Chinese Orthodontic Society of Chinese Stomatological Association.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Grippaudo C S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Jiang C, Liu Y, Cheng Q, He W, Fang S, Lan T, Wang J. Chin remodeling in a patient with bimaxillary protrusion and open bite by using mini-implants for temporary anchorage. Am J Orthod Dentofacial Orthop. 2018;153:436-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 2. | Antoszewska-Smith J, Sarul M, Łyczek J, Konopka T, Kawala B. Effectiveness of orthodontic miniscrew implants in anchorage reinforcement during en-masse retraction: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2017;151:440-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 3. | Ishida Y, Ono T. Nonsurgical treatment of an adult with a skeletal Class II gummy smile using zygomatic temporary anchorage devices and improved superelastic nickel-titanium alloy wires. Am J Orthod Dentofacial Orthop. 2017;152:693-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Mimura H. Treatment of severe bimaxillary protrusion with miniscrew anchorage: treatment and complications. Aust Orthod J. 2008;24:156-163. [PubMed] |
| 5. | Kook YA, Park JH, Bayome M, Sa'aed NL. Correction of severe bimaxillary protrusion with first premolar extractions and total arch distalization with palatal anchorage plates. Am J Orthod Dentofacial Orthop. 2015;148:310-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 6. | Huang YP, Li WR. Correlation between objective and subjective evaluation of profile in bimaxillary protrusion patients after orthodontic treatment. Angle Orthod. 2015;85:690-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Kyung HM, Park HS, Bae SM, Sung JH, Kim IB. Development of orthodontic micro-implants for intraoral anchorage. J Clin Orthod. 2003;37:321-8; quiz 314. [PubMed] |
| 8. | Saxby PJ, Freer TJ. Dentoskeletal determinants of soft tissue morphology. Angle Orthod. 1985;55:147-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Arnett GW, Jelic JS, Kim J, Cummings DR, Beress A, Worley CM Jr, Chung B, Bergman R. Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofacial Orthop. 1999;116:239-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 202] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 10. | Sung EH, Kim SJ, Chun YS, Park YC, Yu HS, Lee KJ. Distalization pattern of whole maxillary dentition according to force application points. Korean J Orthod. 2015;45:20-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Chen K, Cao Y. Class III malocclusion treated with distalization of the mandibular dentition with miniscrew anchorage: A 2-year follow-up. Am J Orthod Dentofacial Orthop. 2015;148:1043-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Archambault A, Lacoursiere R, Badawi H, Major PW, Carey J, Flores-Mir C. Torque expression in stainless steel orthodontic brackets. A systematic review. Angle Orthod. 2010;80:201-210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Sfondrini MF, Gandini P, Castroflorio T, Garino F, Mergati L, D'Anca K, Trovati F, Scribante A. Buccolingual Inclination Control of Upper Central Incisors of Aligners: A Comparison with Conventional and Self-Ligating Brackets. Biomed Res Int. 2018;2018:9341821. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Keating PJ. Bimaxillary protrusion in the Caucasian: a cephalometric study of the morphological features. Br J Orthod. 1985;12:193-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Zhang J, Qiao M. [Cephalometric analysis of the patients with bimaxillary protrusion in south China]. Hua Xi Kou Qiang Yi Xue Za Zhi. 2001;19:32-34. [PubMed] |
| 16. | Mukaida K, Mayahara K, Sanuki-Suzuki R, Tamura T, Shimizu N. Treatment of bimaxillary protrusion with temporary anchorage devices. J Oral Sci. 2018;60:316-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Chung KR, Choo H, Lee JH, Kim SH. Atypical orthodontic extraction pattern managed by differential en-masse retraction against a temporary skeletal anchorage device in the treatment of bimaxillary protrusion. Am J Orthod Dentofacial Orthop. 2011;140:423-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |