Published online Jan 26, 2021. doi: 10.12998/wjcc.v9.i3.672
Peer-review started: September 5, 2020
First decision: November 14, 2020
Revised: November 22, 2020
Accepted: December 6, 2020
Article in press: December 6, 2020
Published online: January 26, 2021
Processing time: 136 Days and 21.1 Hours
Abnormalities of the inferior vena cava (IVC) are uncommon, and in many cases they are asymptomatic. Even so, it is vital that clinicians be aware of such anomalies prior to surgery in affected individuals. In the present report, we describe a rare anatomical variation of the IVC.
A 66-year-old male was admitted to the hospital due to deep vein thrombosis of the right lower extremity. Upon contrast-enhanced computed tomography imaging, we found that this patient presented with a case of left-sided IVC draining into the hemiazygos vein, while his hepatic vein was directly draining into the atrium.
Cases of left-sided IVC can increase patient susceptibility to thromboembolism owing to the resultant changes in blood flow and/or associated vascular compression.
Core Tip: We found that one patient with deep venous thrombosis had left-sided inferior vena cava draining into the hemiazygos vein, while his hepatic vein was directly draining into the atrium. It is vital that clinicians be aware of such anomalies prior to surgery in affected individuals.
- Citation: Zhang L, Guan WK. Deep vein thrombosis in patient with left-sided inferior vena cava draining into the hemiazygos vein: A case report. World J Clin Cases 2021; 9(3): 672-676
- URL: https://www.wjgnet.com/2307-8960/full/v9/i3/672.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i3.672
As noninvasive vascular imaging technologies have become increasingly advanced, a number of different anatomic variations in the structure of the inferior vena cava (IVC) have been observed in clinical practice. The development of the IVC is complex and relies upon the formation of connections between three paired embryonic veins, resulting in multiple potential variations in the overall venous architecture. It is important that medical professionals understand these variations and their clinical implications so that they can properly diagnose and treat patients affected by conditions such as deep vein thrombosis (DVT).
A 66-year-old male presented with pain and edema of the right leg for 2 d.
Pain and edema of the right leg for 2 d prior to hospital admission, no fever, chest pain, or dyspnea.
Multiple soft tissue injuries caused by falls 12 d before admission.
The patient had no remarkable personal or family history.
Swelling of the right lower extremity with palpable pitting edema, normal skin temperature, and a good arterial pulse within this extremity.
At the time of admission, the patient had a D-dimer level of 2789 ng/mL (NG, 0-500 ng/mL).
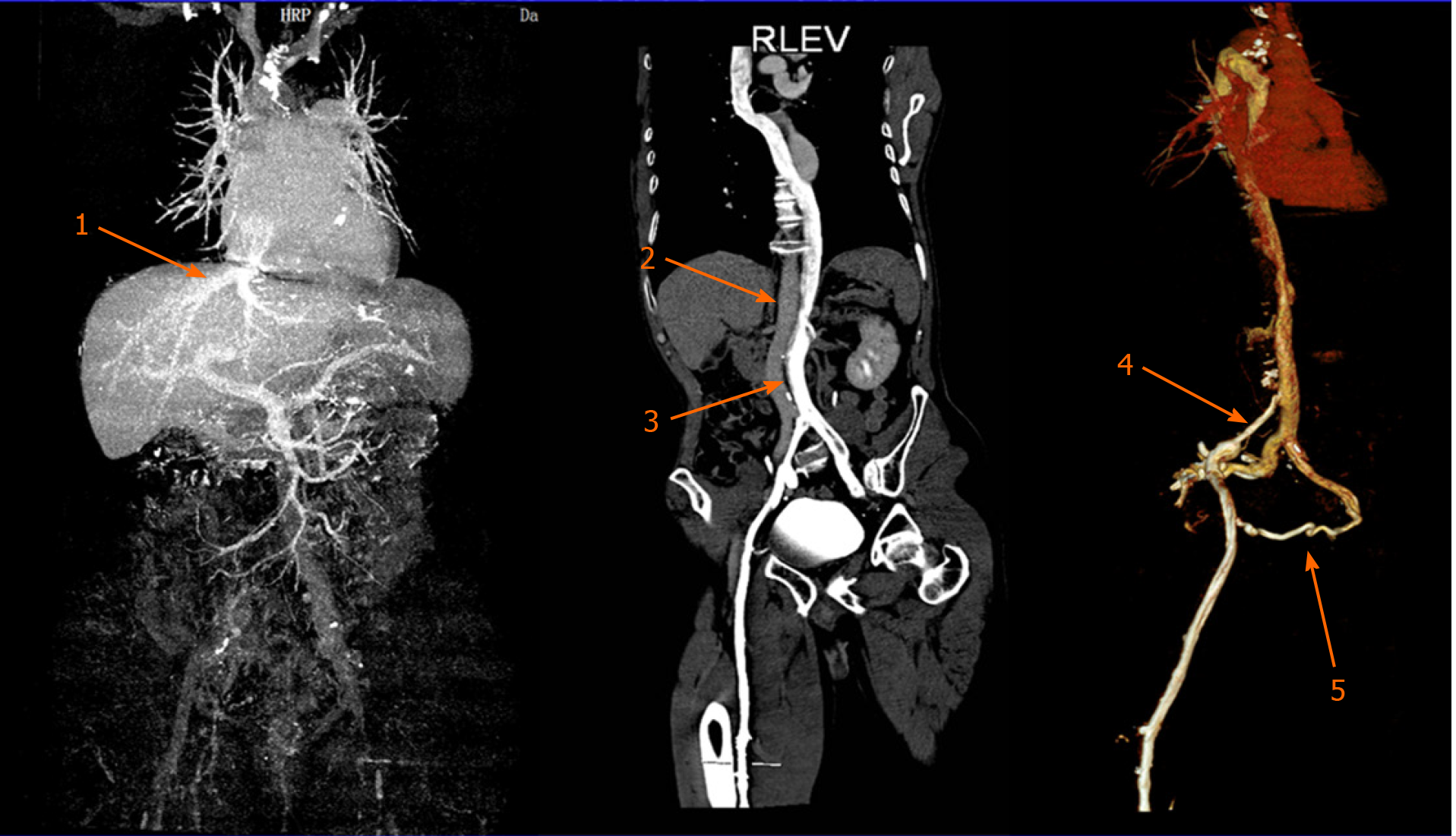
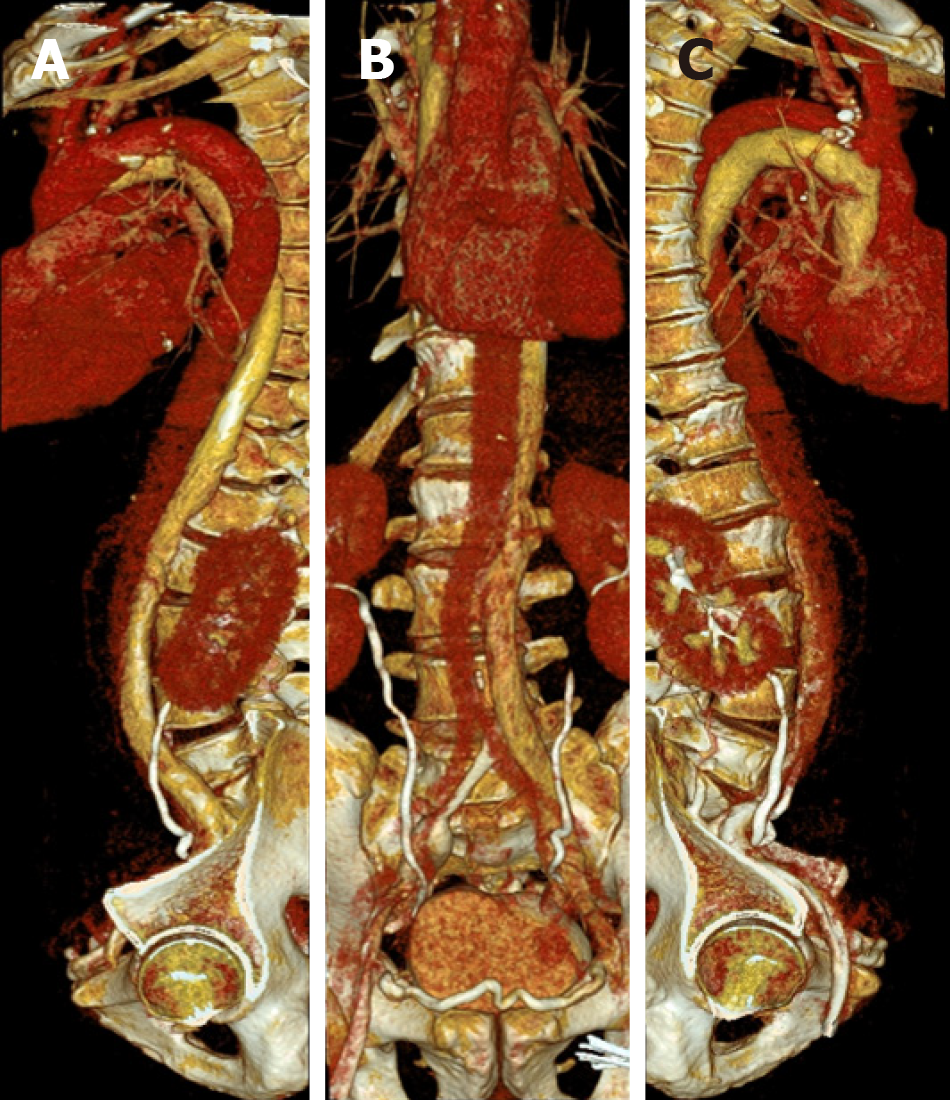
At the time of admission, color Doppler ultrasonography revealed right iliac-femoral vein thrombosis with decreased distal blood flow velocity. In order to accurately assess the anatomy of the retroperitoneal venous system in this patient, contrast-enhanced computed tomography was conducted after the thrombolysis procedure, which revealed that the right common iliac vein was located behind the left common iliac artery and was clearly compressed and stenotic. Many collateral vessels had formed in the pelvic cavity, and the left iliac vein was significantly wider than that on the right side. Abnormal left-sided IVC drainage was the result of the union of the two common iliac veins at the level of the 4th lumbar vertebra. It ascended vertically to the left side of the abdominal aorta where it connected with the left and right renal vein at the levels of the 2nd and 3rd lumbar vertebrae, respectively. The right renal vein additionally crossed posteriorly to the abdominal aorta. The left-sided IVC continued to ascend and intersected with the hemiazygos vein at the level of the 2nd lumbar vertebra, after which it crossed posteriorly to the left diaphragm crura and entered the thorax. It then ascended through the posterior mediastinum to the left of the four inferior thoracic vertebrae, crossing posteriorly to the thoracic aorta and the azygos vein at the level of 8th thoracic vertebra, arching over the root of the right lung and joining the right superior vena cava at the level of the 5th thoracic vertebra. There was no retrohepatic IVC or right IVC in this patient, and the hepatic vein drained directly into the right atrium (Figures 1 and 2). No other anatomic anomalies were detected in this patient, and echocardiographic findings were normal.
DVT of right lower extremity, variation of IVC, multiple soft tissue injuries.
When the patient underwent phlebography, a rare anatomical variation in the structure of the IVC was detected. Specifically, the patient exhibited a case of left-sided IVC draining into the hemiazygos vein. The renal vein drained into the left-sided IVC below its typical anatomic position. The patient was treated for DVT of the lower right extremity via catheter-directed thrombolysis and experienced significant symptom improvement after 4 d. Subsequent phlebography revealed right iliac vein stenosis with collateral vessel formation. As the primary symptoms associated with this case of DVT had been alleviated, no further treatment of iliac vein stenosis was administered other than warfarin anticoagulant therapy.
The swelling of the right lower extremity disappeared, and the limbs were not swollen after exercise. Color Doppler ultrasound examination showed that the right lower extremity vein was unobstructed, and there was no recurrence of thrombus.
There have been several previous reports of anatomic IVC variability[1]. Azygos continuation of the IVC has, in previous reports, been described as the absence of the hepatic segment of the IVC with azygos continuation. Overall, this anatomic variation has a 0.6% prevalence and is thought to arise due to a failure of right subcardinal-hepatic anastomosis during embryonic development, which ultimately causes the right subcardinal vein to atrophy. There have been even fewer reports of hemiazygos continuation of left-sided IVC[2]. In most cases, IVC anomalies present from birth are asymptomatic and are only discovered incidentally when patients are undergoing abdominal surgery or imaging evaluations[3-5]. As such, the true prevalence of IVC anomalies is likely higher than current estimates. These anomalies have been diagnosed and studied using a range of techniques, with helical computed tomography being an efficient and reliable modality that is commonly used for such evaluations[6].
Hemiazygous IVC continuation can result in dilatation that may be misinterpreted as a mediastinal or paracardiac mass upon radiographic assessment. Patients with this continuation are additionally at risk of accidental ligation of the IVC during thoracic surgery[7]. It is therefore essential that such anatomic variations be preoperatively identified using appropriate imaging techniques in order to minimize the risk of surgical complications in affected individuals.
In the present case, phlebography led to the diagnosis of DVT of the right leg as well as the presence of a rare anatomical variation wherein the patient exhibited left-sided IVC draining into the hemiazygos vein. Contrast-enhanced computed tomography imaging revealed that the right common iliac vein was behind the left common iliac artery with clear evidence of stenosis and compression. In addition, several collateral vessels were evident within the pelvic cavity, and the left iliac vein was significantly wider than that on the right side. Cases of left-sided IVC can increase patient susceptibility to thromboembolism owing to the resultant changes in blood flow and/or associated vascular compression.
There have been few prior reports of left-sided IVC draining into the hemiazygos vein, suggesting that this is a relatively rare anatomical variation. This structural anomaly may be clinically relevant to the development, treatment and prevention of venous thromboembolic events in affected individuals.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hashimoto N, Sirin G, Teramoto-Matsubara OT S-Editor: Huang P L-Editor: Filipodia P-Editor: Li JH
| 1. | Ang WC, Doyle T, Stringer MD. Left-sided and duplicate inferior vena cava: a case series and review. Clin Anat. 2013;26:990-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Berry CA. Oblique Lumbar Interbody Fusion in Patient with Persistent Left-Sided Inferior Vena Cava: Case Report and Review of Literature. World Neurosurg. 2019;132:58-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Dilli A, Ayaz UY, Kaplanoğlu H, Saltas H, Hekimoglu B. Evaluation of the left renal vein variations and inferior vena cava variations by means of helical computed tomography. Clin Imaging. 2013;37:530-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Gandhi SP, Modi P, Sutariya H, Patel K. Rare Anatomical Variation of Dual IVC with Left Sided IVC Draining into Hemiazygous Vein- A Case Report. J Clin Diagn Res. 2016;10:TD14-TD15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Hong PS, Cornett CA. Left-sided inferior vena cava in anterior lumbar spine surgery. Spine J. 2015;15:1674-1675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Spratt JD. Inferior vena cava, portal and hepatic venous systems. In: Tubbs RS, Shoja MM, Loukas M. Bergman's Comprehensive Encyclopedia of Human Anatomic Variation. John Wiley & Sons, Inc. 2016; 877-889. [DOI] [Full Text] |
| 7. | Rajabnejad Y, Aliakbarian M, Rajabnejad A, Motie MR. Left-Sided Inferior Vena Cava Encountered During Organ Retrieval Surgery: Report of Two Cases. Int J Organ Transplant Med. 2016;7:229-232. [PubMed] |