Published online Jan 26, 2021. doi: 10.12998/wjcc.v9.i3.659
Peer-review started: September 2, 2020
First decision: November 8, 2020
Revised: November 21, 2020
Accepted: December 6, 2020
Article in press: December 6, 2020
Published online: January 26, 2021
Processing time: 139 Days and 22 Hours
Hepatic cystic echinococcosis (CE) is an infectious zoonotic parasitic disease, and the insidious onset and slow progression of hepatic CE usually contributes to delayed diagnosis and treatment. Hepatocellular carcinoma (HCC) is the fourth most common malignant tumor. Co-existence of CE and HCC is fairly rare in clinical settings and the association between the two is still not well recognized. We report a case of hepatic CE complicated with HCC which are radically resected and raise some questions worth thinking about.
A 70-year-old man presented with upper abdominal pain. On admission, laboratory data showed that, except for hepatitis B surface antigen positivity, other indicators were normal, including alpha-fetoprotein. Computed tomography of the abdomen revealed a huge polycystic lesion in left liver lobe, without reinforcement after enhanced scanning and sized about 16.9 cm × 12.2 cm, which was considered a type II hydatid cyst. Multiple small solid lesions were also found adjacent to it, and thus it was highly suspected as a malignant tumor. After a multidisciplinary team discussion, the diagnosis of co-occurrence of hepatic CE and HCC was made. According to Romic classification, the case belongs to type IIb, and radical left hemi-hepatectomy was performed. Postoperative pathological examination revealed CE co-existence with well-differentiated HCC, consistent with the preoperative diagnosis.
With the combination of hepatitis B and obvious extrusion by large hydatid, the HCC risk of a patient might be higher.
Core Tip: Hepatic cystic echinococcosis (CE) is an infectious zoonotic parasitic disease, hepatocellular carcinoma (HCC) is the fourth most common malignant tumor. Co-existence of CE and HCC is fairly rare in clinical settings and the association between the two is still not well recognized. We report a case of hepatic CE complicated with HCC which are radically resected, and present an opinion that with the combination of hepatitis B and obvious extrusion by large hydatid, the HCC risk of the patients might be higher.
- Citation: Kalifu B, Meng Y, Maimaitinijiati Y, Ma ZG, Tian GL, Wang JG, Chen X. Radical resection of hepatic polycystic echinococcosis complicated with hepatocellular carcinoma: A case report. World J Clin Cases 2021; 9(3): 659-665
- URL: https://www.wjgnet.com/2307-8960/full/v9/i3/659.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i3.659
Cystic echinococcosis (CE) is caused by Echinococcus granulosus (E. granulosus), an infectious parasitic disease. Liver is the most affected organ due to the special life cycle of E. granulosus[1,2]. In recent years, with the development of tourism and the movement of populations, hepatic CE has become a serious public health problem around the world. In endemic areas, the incidence of cystic hydatid disease is 1-200/100000 per year, and fatality rate has been reported as 2%-4%[3]. Hepatocellular carcinoma (HCC) is the most frequent primary liver cancer, accounting for more than 85%-90% of them, and is a leading cause of cancer-related mortality[4]. Although both are hepatic space-occupying diseases, it is rare to co-occur, due to their biological characteristics. There have been few reports concerning hepatic CE accompanied by HCC[5,6]. Whether hydatid infection impacts the occurrence and progression of HCC is still unclear.
Here, we share a case of huge hepatic CE lesion complicated with HCC, and present some controversial issues with detailed discussion.
A 70-year-old man presented to The Department of Hepatobiliary Surgery, People’s Hospital of Xinjiang Uygur Autonomous Region, with complaint of upper abdominal pain for 2 wk.
The patient had upper abdominal pain for 2 wk, and no another special discomfort symptom.
The patient had no significant past illness.
The patient had no significant personal and family history.
The physical examination was significant for pain in the right upper quadrant upon palpation.
All laboratory testing, including glutamic-pyruvic transaminase, glutamic-oxalacetic transaminase, gamma-glutamyl transpeptidase, and alpha-fetoprotein, was normal, except for positivity for hepatitis B surface antigen.
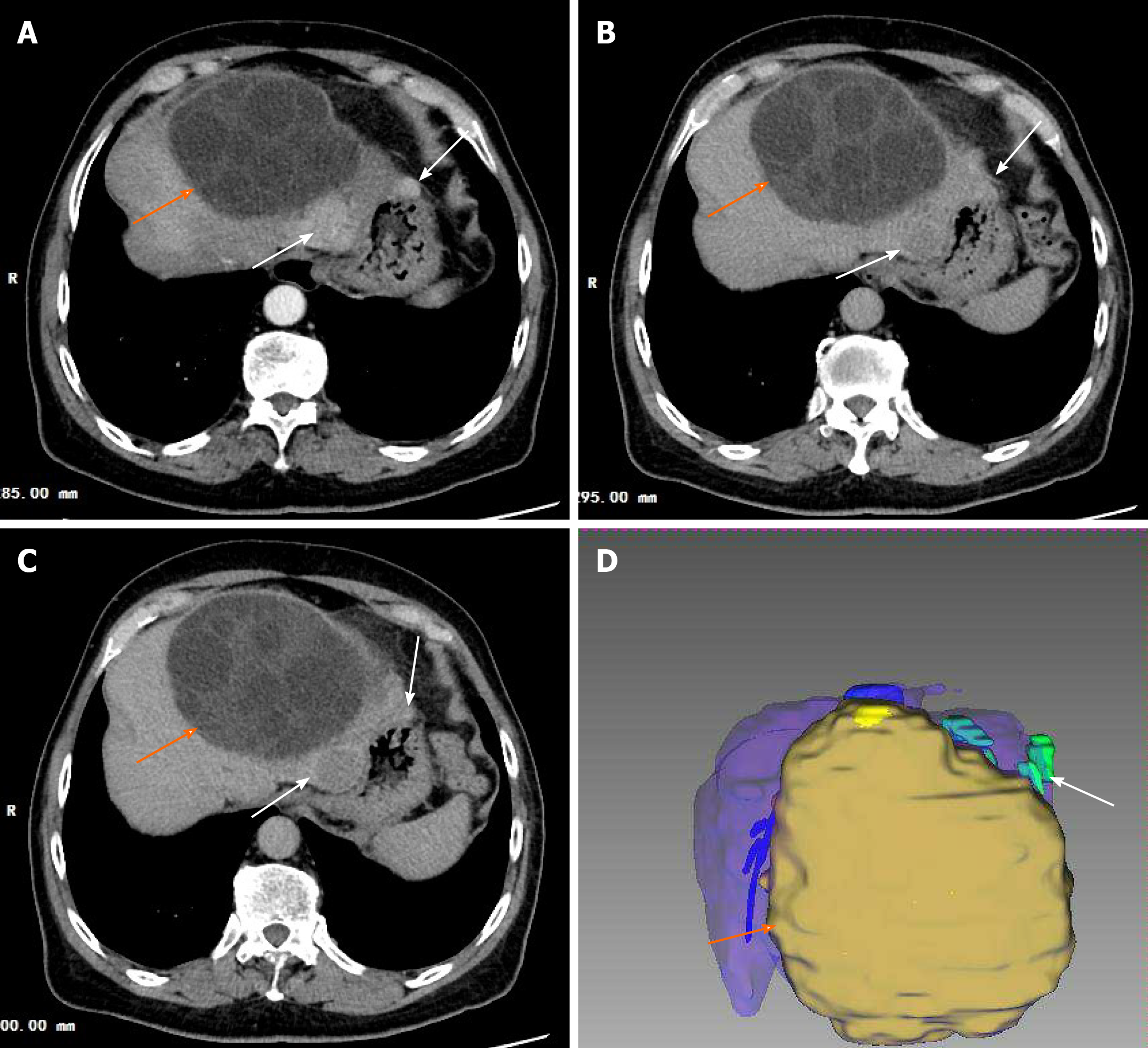
Computed tomography of the abdomen revealed a huge polycystic lesion in left liver lobe, without reinforcement after enhanced scanning, sized about 16.9 cm × 12.2 cm (Figure 1), which was considered a type II hydatid cyst[7]. Multiple small solid lesions were also found adjacent to it, and thus it was highly suspected as malignant tumor.
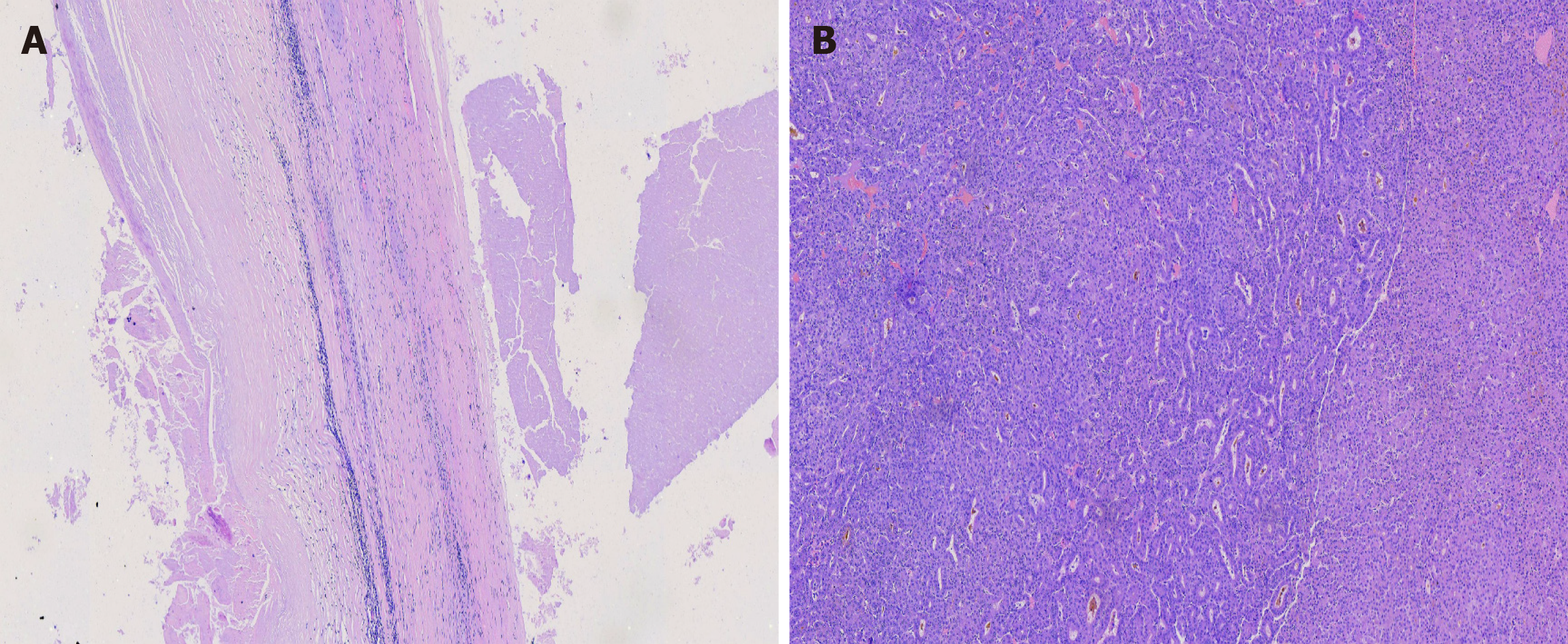
After a multidisciplinary team discussion, the preoperative diagnosis was made of co-occurrence of hepatic polycystic echinococcosis and HCC. According to Romic classification[8], the case was type IIb. The postoperative pathological examination revealed CE co-existence with well-differentiated HCC (Figure 2), consistent with the preoperative diagnosis.
Co-occurrence of hepatic polycystic echinococcosis and HCC.
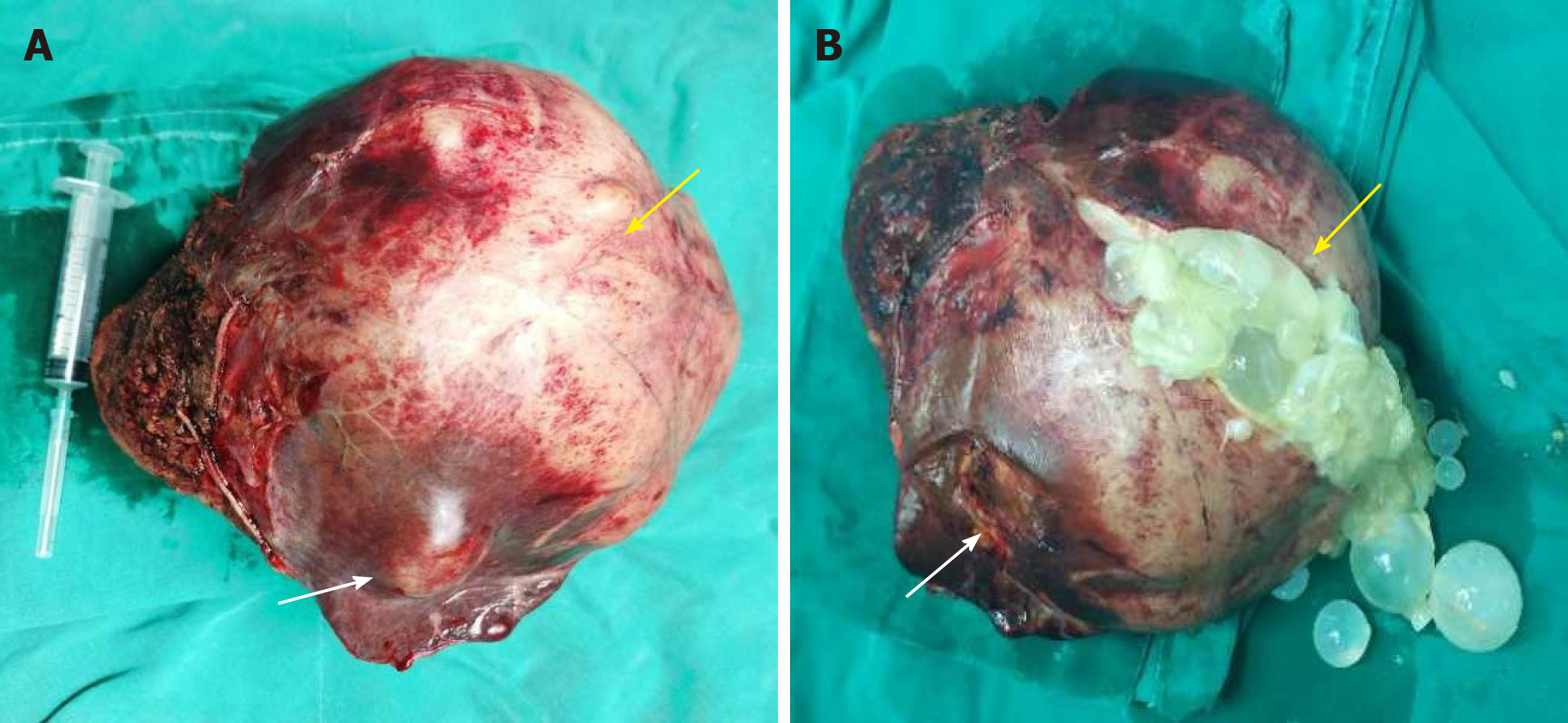
Radical left hemi-hepatectomy was performed (Figure 3).
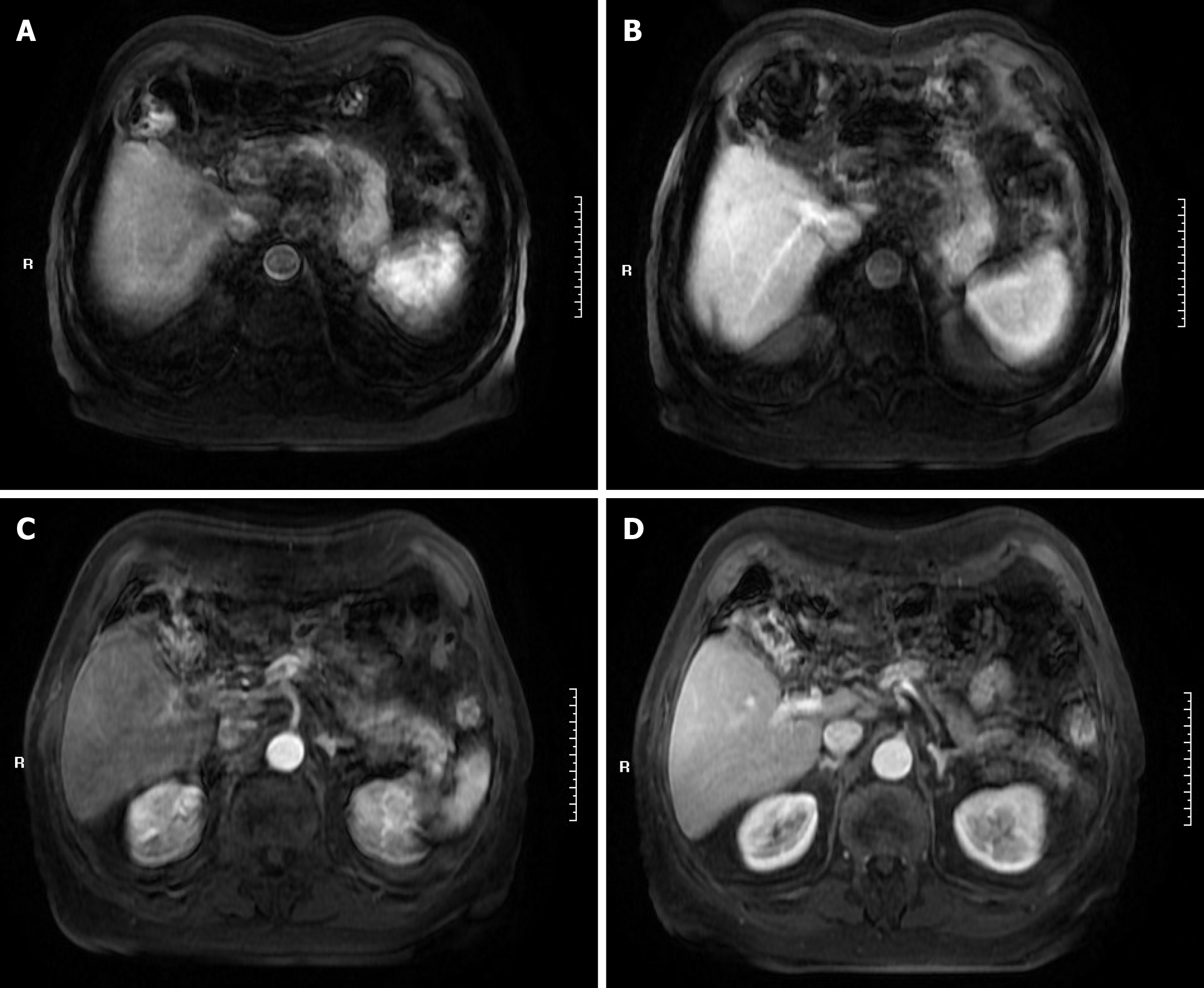
The patient recovered and was discharged on the eighth day after the operation and no treatment was received after discharge. The magnetic resonance imaging conducted at 3 mo after surgery showed no significant recurrence of the lesion (Figure 4).
Hepatic CE and HCC are both liver space-occupying diseases with high incidence, whereas the concomitant presence of hepatic CE and HCC is a fairly rare scenario, leaving evidence-based options of treatments unavailable worldwide. Based on the World Health Organization Informal Working Group on Echinococcosis (known as WHO-IWGE) international classification[7], the current case belongs to the type II hydatid cysts, for which radical resection is recommended to be performed in the guideline. The BCLC staging system is the method currently used to stage HCC and widely accepted as a therapeutic guidance. For the current patient, there were more than three tumors with the size of 35 mm, and the case was considered as intermediate-staged HCC (stage B); furthermore, the lesions were located in the same lobe of the liver. Hemihepatectomy is advised by the European Association for the Study of the Liver clinical practice guideline[9] and the American guideline (2018)[10] for such cases. By applying the guidelines for both diseases, the radical left hemihepatectomy was performed and albendazole therapy for CE and HCC adjuvant therapy were not recommended after surgery. In addition, entecavir was administered since the hepatitis B surface antigen test was positive.
To our knowledge, there are few studies on co-infection of CE and HCC and the association between the two is still not well recognized. There are 25 cases reported concerning concomitant HCC and echinococcal cysts in the scientific literature worldwide and 20 of them have provided sufficient data for review analysis. The patients represent 12 males and 8 females, aged from 27 years to 82 years, with an average age of 67. Fifteen of them had underlying chronic liver diseases. It has been reported that CE infection may lead to the development of liver carcinoma[11,12]. By contrast, van Knapen[13] put forward the hypothesis that echinococcus infection could suppress tumor growth. Recently, Bo et al[14] reported 13 patients with co-existence of hepatic CE and HCC, being the report with the largest number of cases at present. Those authors consider that E. granulosus may elicit a protective effect against the development and progression of HCC.
The most common cause of HCC is liver cirrhosis caused by hepatitis and other causes[15]. Although our case showed evidence of hepatitis B, there was no cirrhosis or elevation of alpha-fetoprotein. In addition, the tumors were located in the hydatid peripheral normal liver tissues, and there was no tumor in the right lobe of the liver. Therefore, we speculate that a chronic inflammatory reaction of liver tissue around the cyst, especially in the extruded area, may have led to increased risk of HCC development.
Based on the case and literature review described herein, the current knowledge may raise a hypothesis that human CE may induce the development of HCC, and increased cyst size and hepatitis B may increase the risk of such. When there is combination of hepatitis B and obvious extrusion by a large hydatid, the HCC risk of the patients might be higher. Nonetheless, further studies are needed to clarify the assumption.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: El-Hawary AK, Hashimoto N S-Editor: Huang P L-Editor: Filipodia P-Editor: Li JH
| 1. | Wen H, Vuitton L, Tuxun T, Li J, Vuitton DA, Zhang W, McManus DP. Echinococcosis: Advances in the 21st Century. Clin Microbiol Rev. 2019;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 421] [Cited by in RCA: 640] [Article Influence: 106.7] [Reference Citation Analysis (0)] |
| 2. | Kern P, Menezes da Silva A, Akhan O, Müllhaupt B, Vizcaychipi KA, Budke C, Vuitton DA. The Echinococcoses: Diagnosis, Clinical Management and Burden of Disease. Adv Parasitol. 2017;96:259-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 326] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 3. | Deplazes P, Rinaldi L, Alvarez Rojas CA, Torgerson PR, Harandi MF, Romig T, Antolova D, Schurer JM, Lahmar S, Cringoli G, Magambo J, Thompson RC, Jenkins EJ. Global Distribution of Alveolar and Cystic Echinococcosis. Adv Parasitol. 2017;95:315-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 640] [Article Influence: 80.0] [Reference Citation Analysis (0)] |
| 4. | Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, Hay RJ, Hunter-Merrill R, Huynh C, Hosgood HD, Johnson CO, Jonas JB, Khubchandani J, Kumar GA, Kutz M, Lan Q, Larson HJ, Liang X, Lim SS, Lopez AD, MacIntyre MF, Marczak L, Marquez N, Mokdad AH, Pinho C, Pourmalek F, Salomon JA, Sanabria JR, Sandar L, Sartorius B, Schwartz SM, Shackelford KA, Shibuya K, Stanaway J, Steiner C, Sun J, Takahashi K, Vollset SE, Vos T, Wagner JA, Wang H, Westerman R, Zeeb H, Zoeckler L, Abd-Allah F, Ahmed MB, Alabed S, Alam NK, Aldhahri SF, Alem G, Alemayohu MA, Ali R, Al-Raddadi R, Amare A, Amoako Y, Artaman A, Asayesh H, Atnafu N, Awasthi A, Saleem HB, Barac A, Bedi N, Bensenor I, Berhane A, Bernabé E, Betsu B, Binagwaho A, Boneya D, Campos-Nonato I, Castañeda-Orjuela C, Catalá-López F, Chiang P, Chibueze C, Chitheer A, Choi JY, Cowie B, Damtew S, das Neves J, Dey S, Dharmaratne S, Dhillon P, Ding E, Driscoll T, Ekwueme D, Endries AY, Farvid M, Farzadfar F, Fernandes J, Fischer F, G/Hiwot TT, Gebru A, Gopalani S, Hailu A, Horino M, Horita N, Husseini A, Huybrechts I, Inoue M, Islami F, Jakovljevic M, James S, Javanbakht M, Jee SH, Kasaeian A, Kedir MS, Khader YS, Khang YH, Kim D, Leigh J, Linn S, Lunevicius R, El Razek HMA, Malekzadeh R, Malta DC, Marcenes W, Markos D, Melaku YA, Meles KG, Mendoza W, Mengiste DT, Meretoja TJ, Miller TR, Mohammad KA, Mohammadi A, Mohammed S, Moradi-Lakeh M, Nagel G, Nand D, Le Nguyen Q, Nolte S, Ogbo FA, Oladimeji KE, Oren E, Pa M, Park EK, Pereira DM, Plass D, Qorbani M, Radfar A, Rafay A, Rahman M, Rana SM, Søreide K, Satpathy M, Sawhney M, Sepanlou SG, Shaikh MA, She J, Shiue I, Shore HR, Shrime MG, So S, Soneji S, Stathopoulou V, Stroumpoulis K, Sufiyan MB, Sykes BL, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tessema GA, Thakur JS, Tran BX, Ukwaja KN, Uzochukwu BSC, Vlassov VV, Weiderpass E, Wubshet Terefe M, Yebyo HG, Yimam HH, Yonemoto N, Younis MZ, Yu C, Zaidi Z, Zaki MES, Zenebe ZM, Murray CJL, Naghavi M. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3:524-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2838] [Cited by in RCA: 2962] [Article Influence: 370.3] [Reference Citation Analysis (0)] |
| 5. | Sygut A, Górski A, Dziki A. [A case of coexistence of primary cancer of the liver and hepatic echinococcosis]. Wiad Lek. 1987;40:826-828. [PubMed] |
| 6. | Kato T, Seino Y, Takada K, Maruya M, Okubo S, Nakamura H, Inoue Y, Meguro T, Horita S, Oshikiri T, Yamada H, Miyasaka Y, Fujita M, Morita T, Yoshida T, Chikai K. [A resectable case of hepatocellular carcinoma complicated with hepatic alveolar echinococcosis]. Nihon Shokakibyo Gakkai Zasshi. 2003;100:587-592. [PubMed] |
| 7. | WHO Informal Working Group. International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 2003;85:253-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 489] [Cited by in RCA: 501] [Article Influence: 22.8] [Reference Citation Analysis (1)] |
| 8. | Romic B, Romic I, Petrovic I, Romic M, Romic R, Romic M, Mance M, Pavlek G; -. A Synchronous Occurrence of Hepatocellular Carcinoma and Echinoccocal Liver Cyst - Can Parasite Promote Carcinogenesis? Chirurgia (Bucur). 2016;111:297-303. [PubMed] |
| 9. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5593] [Cited by in RCA: 6064] [Article Influence: 866.3] [Reference Citation Analysis (3)] |
| 10. | Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, Roberts LR, Heimbach JK. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68:723-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2121] [Cited by in RCA: 3243] [Article Influence: 463.3] [Reference Citation Analysis (1)] |
| 11. | Li H, Song T, Shao Y, Wen H. Cystic echinococcosis accompanied by hepatocellular carcinoma in a female herdsman. Int J Clin Exp Med. 2015;8:2985-2988. [PubMed] |
| 12. | Oikonomopoulou K, Yu H, Wang Z, Vasiliou SK, Brinc D, Christofi G, Theodorou M, Pavlou P, Hadjisavvas A, Demetriou CA, Kyriacou K, Diamandis EP. Association between Echinococcus granulosus infection and cancer risk - a pilot study in Cyprus. Clin Chem Lab Med. 2016;54:1955-1961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | van Knapen F. Echinococcus granulosus infection and malignancy. Br Med J. 1980;281:195-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Bo R, Yasen A, Shao Y, Zhang W, Lin R, Jiang T, Wen H, Xiao H, Aji T. Co-existence of hepatocellular carcinoma and cystic echinococcosis. Infect Agent Cancer. 2020;15:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2881] [Cited by in RCA: 3088] [Article Influence: 220.6] [Reference Citation Analysis (0)] |