Published online Jan 26, 2021. doi: 10.12998/wjcc.v9.i3.644
Peer-review started: August 30, 2020
First decision: November 8, 2020
Revised: November 18, 2020
Accepted: December 6, 2020
Article in press: December 6, 2020
Published online: January 26, 2021
Processing time: 140 Days and 21.9 Hours
Cervical spondylectomy for the treatment of cervical tumors is traumatic, causes bleeding, and is risky. This study reports on the experience with minimally invasive cervical spondylectomy for a cervical metastasis and reviewed the literature on cervical spondylectomy. The purpose was to reduce the risk and trauma of spondylectomy.
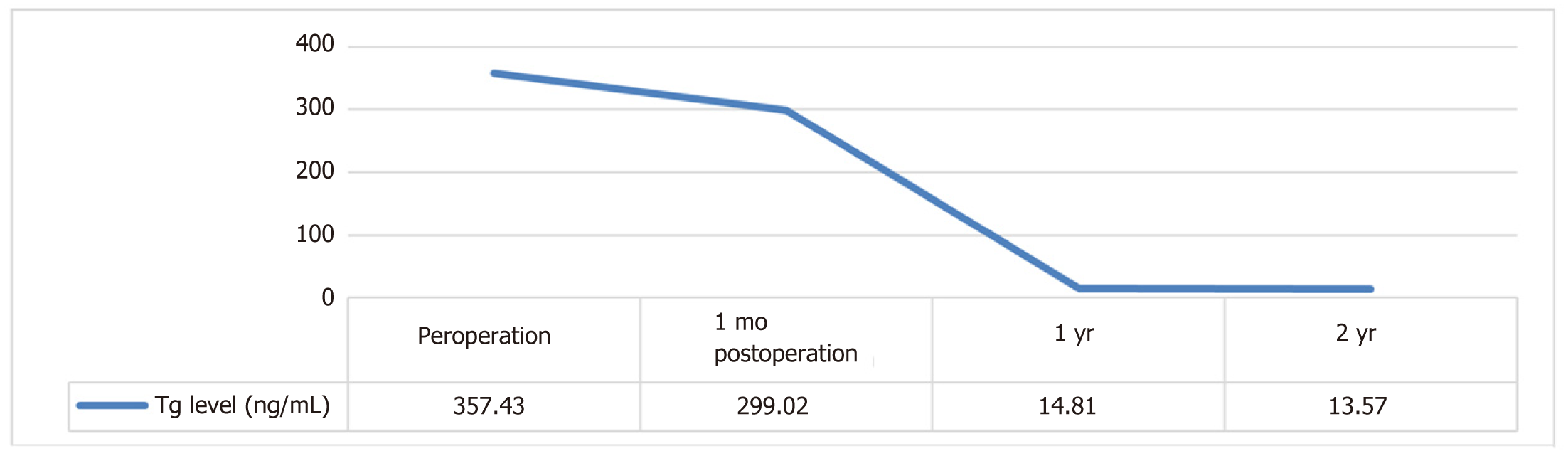
A 60-year-old woman presented with cervical pain and radiating pain in the left upper limb for more than 2 mo. Preoperative diagnosis was C4 metastasis of thyroid cancer. Preoperative visual analogue scale score was 5. American Spinal Cord Injury Association (ASIA) grade was E. Tomita classification was 7. Weinstein-Boriani-Biagini (WBB) classification was A-D, 3-9. Tomita score was 5. Modified Tokuhashi score was 9. Spinal instability neoplastic score (SINS) was 13. The patient underwent minimally invasive cervical spondylectomy on September 28, 2017. The operative time was 200 min; the estimated blood loss was 1200 mL. The operation was successful, without complications. The postoperative visual analogue scale score was 0. The patient remained classified as ASIA grade E at the last follow-up. She accepted regular iodine-131 therapy postoperatively. The serum thyroglobulin (Tg) level of this patient was 299.02 ng/mL at 1 mo after the operation and was 13.57 ng/mL at the last follow-up. There was no local recurrence at the 25-mo follow-up, according to images, single-photon emission computed tomography, and serum Tg levels. Obvious ossification and solid fusion of C3-C5 were found at the last follow-up.
Minimally invasive cervical spondylectomy with tubular retractor could minimize soft tissue trauma, intraoperative traction injury, and paraspinal muscle injury, accelerating postoperative recovery. This technique requires a rich experience in cervical spine surgery with tubular retractors, so that surgeons can visualize the anatomical structure in a small field.
Core Tip: Cervical spondylectomy for the treatment of cervical tumors is traumatic, causes bleeding, and is risky. We report a case of 60-year-old woman with C4 metastasis of thyroid carcinoma after thyroidectomy. The patient underwent minimally invasive spondylectomy through tubular retractors. The purpose of the procedure was to reduce surgical trauma and risks. After the operation, the patient was treated with iodine-131. There was no local recurrence, and achievement of solid fusion was detected at last follow-up. This study shows that minimally invasive spondylectomy is feasible in patients who are not candidates for total en bloc spondylectomy, and could reduce the surgical trauma and risks.
- Citation: He LM, Ma X, Chen C, Zhang HY. Treatment of cervical spine metastasis with minimally invasive cervical spondylectomy: A case report and literature review . World J Clin Cases 2021; 9(3): 644-650
- URL: https://www.wjgnet.com/2307-8960/full/v9/i3/644.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i3.644
Following the lung and liver, the skeletal system is the third most common site of metastases. Within the skeletal system, the spine is the most common site of metastases[1,2]. The metastatic spinal level is reportedly 32.76%-71.6% at the thoracic vertebra, 25.17%-60% at the lumbar spine, 8.10%-22.9% at the cervical spine[3,4]. Surgical intervention is indicated for metastatic lesions causing neurologic compression, instability, and rapid deterioration of function. There are many surgical methods for cervical metastasis.
Wright et al[5] reported a total of 2148 patients with spinal metastases. The extent of surgical resection resulted in the following: Cementoplasty (1.9%), palliative decompression (49.3%), piecemeal debulking (27.6%), piecemeal vertebrectomy (6.3%), en bloc intralesional resection (7.0%), and en bloc extralesional resection (7.8%). The spinal instability neoplastic score (commonly known as SINS) score, Tokuhashi scores, and Tomita scores serve as useful guides for evaluating prognostic factors and helping formulate an appropriate plan[6-8]. A comprehensive multimodal approach designed for different individuals will prove to be the best strategy for the surgical management of cervical spine malignancies[9].
Tubular retractors have been used in the facetectomy or transpedicular corpectomy with reconstruction for the treatment of lumbar or thoracic spine metastasis[10-13]. Reports of such, however, described only palliative treatments for the tumor. Here, we report our experience with the surgical method of minimally invasive cervical spondylectomy in a case presenting with neurologic symptoms progression due to a C4 metastatic tumor.
A 60-year-old woman presented with complaint of cervical pain and radiating pain in the left upper limb lasting for more than 2 mo.
The patient was found to have a C4 tumor upon performance of radiography of the cervical spine on July 24, 2017. A computed tomography (CT)-guided biopsy confirmed the diagnosis of follicular thyroid carcinoma-spinal metastasis on July 29, 2017. Thyroid carcinoma was diagnosed by ultrasound on August 2, 2017. Then, the patient was treated with thyroidectomy on August 14, 2018. The patient was transferred to our hospital after the operation.
The patient had been diagnosed with right eye hemangioma 2 years prior and back lipoma 5 years prior. She had no history of other illnesses. She had no known allergies.
The patient had no pertinent family history.
The patient had radiating pain in the right upper limb. The rest of the limbs were normal. Pathological signs were negative. Preoperative visual analogue scale (VAS) score was 5. American Spinal Cord Injury Association (ASIA) grade was E.
Findings of all routine laboratory tests were within normal range.
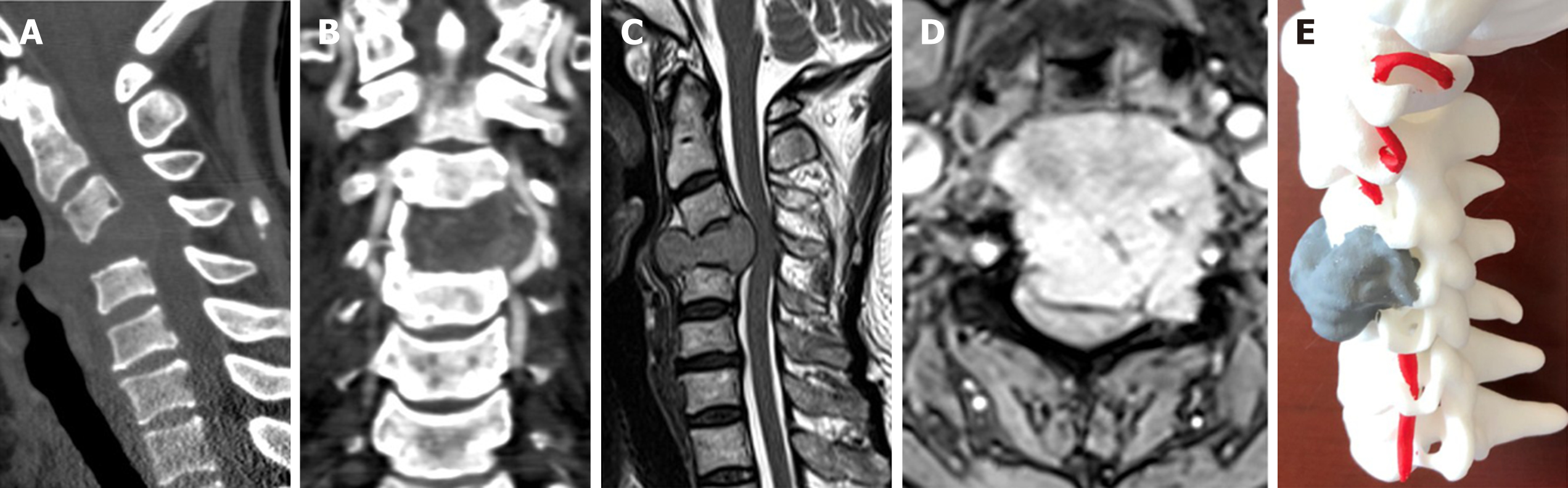
Radiography of the cervical spine showed disappearance of the C4 vertebral body. CT showed an osteolytic lesion at the C4 vertebral body and a left mass (Figure 1A). The right vertebral artery (VA) was severely compressed (Figure 1B). Magnetic resonance imaging (MRI) showed a tumor with an identical signal at the C4 vertebral body and left mass. The lesion protruded into the spinal canal and caused spinal cord compression at the C4 segment (Figure 1C and D). Three-dimensional (3D) cervical modeling based on CT images revealed the lesion and allowed for a surgical plan to be made (Figure 1E).
Single-photon emission computed tomography showed a C4 metastatic tumor and multiple punctate calcifications in the right lung. Tomita classification was 7. Weinstein-Boriani-Biagini (WBB) classification was A-D, 3-9. Tomita score was 5. Modified Tokuhashi score was 9. Spinal instability neoplastic score (SINS) was 13.
C4 metastasis of thyroid carcinoma due to the outcome of a cervical biopsy.
The C4 metastasis of thyroid carcinoma had reduced the stability of the cervical spine and compressed the nerves. There was a risk of further damage to the spinal cord without operation. Therefore, we decided to perform a minimally invasive spondylectomy to remove the tumor, relieve neurological symptoms, and rebuild cervical spine stability.
The patient was placed in a supine position with the neck slightly extended. The levels of C3-C5 were marked via intra-operative lateral C-arm radiography. A right-sided approach with a 5-cm transverse incision was implemented. The front of the C4 vertebral body was exposed through blunt dissection between the trachea and carotid. The initial dilator was inserted into the wound between the fingers to palpate the bony anatomy, and fluoroscopy was used to identify the position. Following sequential dilation, a tubular retractor was introduced and docked at the level of C4. Then, the retractor was locked in place with the flexible arm anchored to the operating table’s side rail. Once the proper placement of the tubular retractor was confirmed with fluoroscopy, the blades were retracted in the vertical axis. Then, the sliding rivet retractor was deployed to open up the deep blades and obtain an adequate field of view.
Two screws, which were used to fix the tubular retractor, were inserted into the C3-C5 vertebral bodies through the lateral hole of the retractor. The trachea, gullet, and carotid were protected with additional retractors. The C4 vertebral body and bilateral mass were resected in a piecemeal fashion. The bilateral VA and dural sac were exposed and protected. A 3D-printed artificial vertebral body was fitted into the site of the C4 vertebral body and checked. An anterior plate was fixed with four bicortical screws. This resulted in a rigid and stable lordotic construction.
The posterior procedure was performed through a midline incision in line with the C3-C5 spinous processes. The incision was 3 cm in length, to accommodate the diameter of the tubular retractors. The fascial incision was equivalent in length and placed at the midline. The spinous processes were exposed through the midline incision. Then, the paraspinal muscles were bluntly dissected to the outer edge of the facet joints. The tubular-like anterior method was deployed and confirmed with fluoroscopy. The dilator was placed at different angles to facilitate proper access for the posterior elements. Piezosurgery and an osteotome were used to cut the posterior element into approximately four to five blocks. These posterior elements were removed one by one. Navigation-assisted lateral mass screw fixation was performed on C3-C5. Intraoperative specimens were sent for pathological examination.
The operative time was 260 min; the estimated blood loss was 1800 mL. The patient was allowed to get up 3 d after operation under the protection of a cervical collar. She accepted regular iodine-131 therapy after the operation.
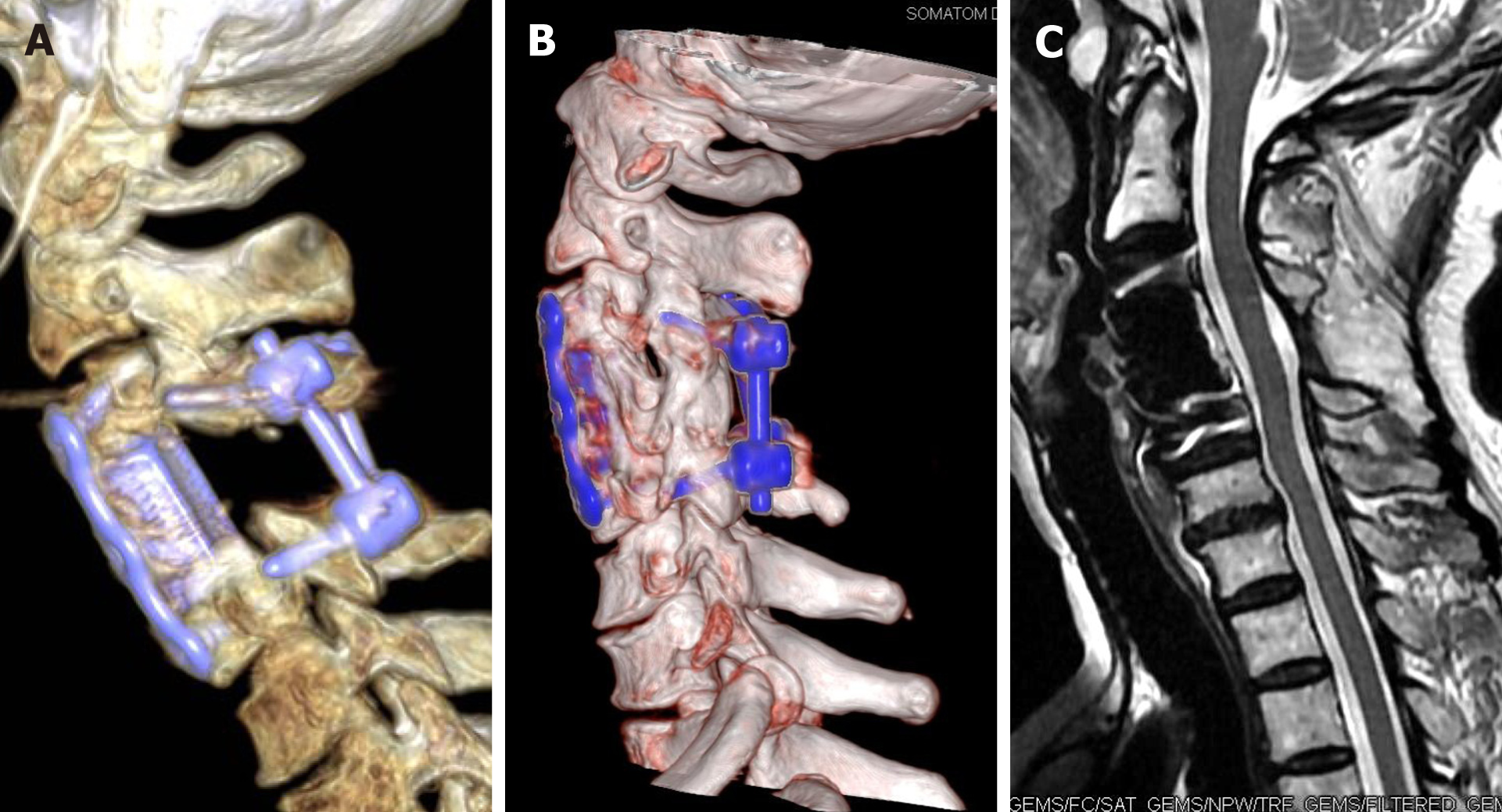
The operation was successful, without complications. The pathological diagnosis was metastatic thyroid carcinoma. Postoperative fluoroscopy, CT, and MRI showed that the tumor and C4 vertebra had been wholly resected (Figure 2A). The physiological curvature and stability of the cervical spine were satisfactory. Postoperative VAS score was 0. The patient remained classified as ASIA grade E at the latest follow-up and achieved pain relief and normal activity. Obvious ossification around the artificial vertebra was shown on postoperative CT, and solid fusion of C3-C5 was found to have been obtained at 25-mo follow-up (Figure 2B). MRI showed no compression of the spinal cord (Figure 2C). Increased serum thyroglobulin (Tg) levels are a sign of differentiated thyroid cancer recurrence or metastasis[14]. The serum Tg levels of this patient are shown in Figure 3.
Generally, surgical resection with a wide margin in accordance with Enneking’s principles of musculoskeletal tumor resection is the most appropriate management for cervical tumors[15]. Tomita et al[16,17] described total en bloc spondylectomy (TES) for malignant vertebral tumors in 1997. TES demanded removal of the tumor in its entirety in one piece, together with a layer of healthy tissue. The method required that the tumor be confined to the vertebral body. This method is still technically challenging in the cervical spine and has high incidence of complications[18]. Several reports have described experiences with TES for cervical lesions, most of which have been case reports.
Currier et al[19] reported a case of C5 chordoma treated successfully with TES, preserving the vertebral arteries and neural structures. Many surgeons believe that this was not true TES because the entire tumor was destroyed when the VA was preserved. Rhines et al[20] presented a case of an extensive upper cervical chordoma treated with TES, reconstruction, and long-segment stabilization. They sacrificed the right C2-C4 nerve roots and the right VA to perform TES. Hoshino et al[21] retrospectively analyzed 15 patients with cervical tumors. All of them underwent unilateral VA ligation during surgery, and none of them experienced complications. Wang et al[22] presented 4 patients with multilevel cervical chordomas who underwent parasagittal osteotomies and en bloc resection. Cervical nerve roots were sacrificed in 2 patients, and unilateral VA ligation and sacrifice were performed in 3 patients. They reported that if VA sacrifice is to be performed, cerebral angiography and temporary balloon occlusion tests are recommended to evaluate the dominant VA and the posterior cranial circulation. The C1-C4 nerve roots can generally be ligated without significant morbidity or weakness. When possible, the nerve roots of C5 and below should be preserved to maintain the deltoid and biceps[23].
Boriani et al[24] reported a retrospective study of 134 patients. The rate of complications was 34.3%. Local recurrence was recorded in 15.7%. Igarashi et al[25], limited their study to only metastatic spinal tumors and showed that the local recurrence rate after frozen autograft TES was 11.0%. A history of radiotherapy was the only risk factor for local recurrence. The primary cancer type was considered the most important factor that affects prognosis. Kato et al[26] reported that patients in the complete excision group survived significantly longer than those in the incomplete excision group. Yang et al[27] reported the overall local recurrence rate was 17.3%. The perioperative mortality rate was 0.9%. The complication-related mortality rate was 1.8%. The rates of overall complications and major complications were 41.8% and 20.9%. Wright et al[5] reported the overall survival rates after surgery were 53% at 1 year, 31% at 2 years, and 10% at 5 years after surgery. There was longer survival in patients who underwent surgery in 2011-2016 compared with those who underwent surgery in earlier periods. In conclusion, total spondylectomy, early treatment, and chemoradiotherapy were beneficial for reducing local recurrence and prolonging survival. Reducing operative trauma and time was beneficial for reducing complications.
Tubular surgery has the advantages of reducing invasion, blood loss, cervical paraspinal muscle injury, perioperative pain, and length of hospital stay. There have been few reports published on the use of tubular retractors in cervical spine surgeries. Mikhael et al[28] reported that multilevel foraminotomy and instrumented fusion using lateral mass screw fixation could be safely accomplished with tubular retraction systems. Uehara et al[29] reported mini-open foraminotomy for cervical radiculopathy by using either large tubular or TrimLine retractors, which is minimally invasive and effective. It could also reduce operative risks associated with anterior exposure, including the recurrent laryngeal nerve injury, trachea injury, esophagus injury, carotid sheath injury, and thoracic duct injury. Kulkarni et al[30] reported minimally invasive anterior cervical discectomy fusion and anterior cervical corpectomy fusion with a tubular retractor using a single incision.
The patient in the present case was treated with total piecemeal spondylectomy because the tumor was not confined in the vertebra and invaded the neural foramen and spinal canal. The minimally invasive operation not only relieved the symptoms but also shortened the hospital stay and bedridden time.
Minimally invasive cervical spondylectomy with tubular retractor could minimize soft tissue trauma, intraoperative traction injury, and paraspinal muscle injury. As such, it accelerates postoperative recovery and reduces complications. This technique requires a rich experience in cervical spine surgery with tubular retractors, so that surgeons can visualize the anatomical structure in a small field. With the development of microscopy and endoscopy technology, minimally invasive cervical spondylectomy will be more useful and safer.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Vagholkar K S-Editor: Huang P L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Brihaye J, Ectors P, Lemort M, Van Houtte P. The management of spinal epidural metastases. Adv Tech Stand Neurosurg. 1988;16:121-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 44] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Constans JP, de Divitiis E, Donzelli R, Spaziante R, Meder JF, Haye C. Spinal metastases with neurological manifestations. Review of 600 cases. J Neurosurg. 1983;59:111-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 272] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | Amelot A, Terrier LM, Cristini J, LeNail LR, Buffenoir K, Pascal-Moussellard H, Bonaccorsi R, Mathon B. Approaching spinal metastases spread profile. Surg Oncol. 2019;31:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Yang L, Wang F, Zhang H, Yang XG, Zhang HR, Li JK, Qiao RQ, Zhang GC, Hu YC. Patient Characteristics Following Surgery for Spinal Metastases: A Multicenter Retrospective Study. Orthop Surg. 2019;11:1039-1047. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Wright E, Ricciardi F, Arts M, Buchowski JM, Chung CK, Coppes M, Crockard A, Depreitere B, Fehlings M, Kawahara N, Lee CS, Leung Y, Martin-Benlloch A, Massicotte E, Mazel C, Oner C, Peul W, Quraishi N, Tokuhashi Y, Tomita K, Ulbricht C, Verlaan JJ, Wang M, Choi D. Metastatic Spine Tumor Epidemiology: Comparison of Trends in Surgery Across Two Decades and Three Continents. World Neurosurg. 2018;114:e809-e817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 6. | Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 2001;26:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 973] [Cited by in RCA: 951] [Article Influence: 39.6] [Reference Citation Analysis (0)] |
| 7. | Papastefanou S, Alpantaki K, Akra G, Katonis P. Predictive value of Tokuhashi and Tomita scores in patients with metastatic spine disease. Acta Orthop Traumatol Turc. 2012;46:50-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, Harrop JS, Fehlings MG, Boriani S, Chou D, Schmidt MH, Polly DW, Biagini R, Burch S, Dekutoski MB, Ganju A, Gerszten PC, Gokaslan ZL, Groff MW, Liebsch NJ, Mendel E, Okuno SH, Patel S, Rhines LD, Rose PS, Sciubba DM, Sundaresan N, Tomita K, Varga PP, Vialle LR, Vrionis FD, Yamada Y, Fourney DR. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010;35:E1221-E1229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 996] [Cited by in RCA: 778] [Article Influence: 51.9] [Reference Citation Analysis (0)] |
| 9. | Mesfin A, Buchowski JM, Gokaslan ZL, Bird JE. Management of metastatic cervical spine tumors. J Am Acad Orthop Surg. 2015;23:38-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Venkatesh R, Tandon V, Patel N, Chhabra HS. Solitary plasmacytoma of L3 vertebral body treated by minimal access surgery: Common problem different solution! J Clin Orthop Trauma. 2015;6:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Zairi F, Troux C, Sunna T, Karnoub MA, Boubez G, Shedid D. Minimally invasive resection of large dumbbell tumors of the lumbar spine: Advantages and pitfalls. Clin Neurol Neurosurg. 2018;168:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Barzilai O, McLaughlin L, Amato MK, Reiner AS, Ogilvie SQ, Lis E, Yamada Y, Bilsky MH, Laufer I. Minimal Access Surgery for Spinal Metastases: Prospective Evaluation of a Treatment Algorithm Using Patient-Reported Outcomes. World Neurosurg. 2018;120:e889-e901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 13. | Serak J, Vanni S, Levi AD. The extreme lateral approach for treatment of thoracic and lumbar vertebral body metastases. J Neurosurg Sci. 2019;63:473-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Ramadan S, Ugas MA, Berwick RJ, Notay M, Cho H, Jerjes W, Giannoudis PV. Spinal metastasis in thyroid cancer. Head Neck Oncol. 2012;4:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Enneking WF. A system of staging musculoskeletal neoplasms. Clin Orthop Relat Res. 1986;9-24. [PubMed] |
| 16. | Tomita K, Kawahara N. The threadwire saw: a new device for cutting bone. J Bone Joint Surg Am. 1996;78:1915-1917. [PubMed] |
| 17. | Tomita K, Kawahara N, Baba H, Tsuchiya H, Fujita T, Toribatake Y. Total en bloc spondylectomy. A new surgical technique for primary malignant vertebral tumors. Spine (Phila Pa 1976). 1997;22:324-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 407] [Cited by in RCA: 386] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 18. | Charest-Morin R, Flexman AM, Srinivas S, Fisher CG, Street JT, Boyd MC, Ailon T, Dvorak MF, Kwon BK, Paquette SJ, Dea N. Perioperative adverse events following surgery for primary bone tumors of the spine and en bloc resection for metastases. J Neurosurg Spine. 2019;1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Currier BL, Papagelopoulos PJ, Krauss WE, Unni KK, Yaszemski MJ. Total en bloc spondylectomy of C5 vertebra for chordoma. Spine (Phila Pa 1976). 2007;32:E294-E299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Rhines LD, Fourney DR, Siadati A, Suk I, Gokaslan ZL. En bloc resection of multilevel cervical chordoma with C-2 involvement. Case report and description of operative technique. J Neurosurg Spine. 2005;2:199-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 99] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 21. | Hoshino Y, Kurokawa T, Nakamura K, Seichi A, Mamada T, Saita K, Miyoshi K. A report on the safety of unilateral vertebral artery ligation during cervical spine surgery. Spine (Phila Pa 1976). 1996;21:1454-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Wang X, Eichbaum E, Jian F, Chou D. Two-Stage En Bloc Resection of Multilevel Cervical Chordomas With Vertebral Artery Preservation: Operative Technique. Oper Neurosurg (Hagerstown). 2018;14:538-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Hsieh PC, Gallia GL, Sciubba DM, Bydon A, Marco RA, Rhines L, Wolinsky JP, Gokaslan ZL. En bloc excisions of chordomas in the cervical spine: review of five consecutive cases with more than 4-year follow-up. Spine (Phila Pa 1976). 2011;36:E1581-E1587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Boriani S, Bandiera S, Donthineni R, Amendola L, Cappuccio M, De Iure F, Gasbarrini A. Morbidity of en bloc resections in the spine. Eur Spine J. 2010;19:231-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 148] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 25. | Igarashi T, Murakami H, Demura S, Kato S, Yoshioka K, Yokogawa N, Tsuchiya H. Risk factors for local recurrence after total en bloc spondylectomy for metastatic spinal tumors: A retrospective study. J Orthop Sci. 2018;23:459-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Kato S, Murakami H, Demura S, Fujimaki Y, Yoshioka K, Yokogawa N, Tsuchiya H. The impact of complete surgical resection of spinal metastases on the survival of patients with thyroid cancer. Cancer Med. 2016;5:2343-2349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 27. | Yang W, Jiang L, Liu X, Wei F, Yu M, Wu F, Dang L, Zhou H, Zhang H, Liu Z. Surgical complications of extraspinal tumors in the cervical spine: a report of 110 cases and literature review. Eur Spine J. 2018;27:882-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Mikhael MM, Celestre PC, Wolf CF, Mroz TE, Wang JC. Minimally invasive cervical spine foraminotomy and lateral mass screw placement. Spine (Phila Pa 1976). 2012;37:E318-E322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Uehara M, Takahashi J, Kuraishi S, Shimizu M, Ikegami S, Futatsugi T, Aoki K, Mukaiyama K, Ogihara N, Hashidate H, Hirabayashi H, Kato H. Mini Open Foraminotomy for Cervical Radiculopathy: A Comparison of Large Tubular and TrimLine Retractors. Asian Spine J. 2015;9:548-552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Kulkarni AG, Patel A, Ankith NV. A technical case report on use of tubular retractors for anterior cervical spine surgery. Eur Spine J. 2018;27:1454-1459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |