Published online Jan 26, 2021. doi: 10.12998/wjcc.v9.i3.602
Peer-review started: November 11, 2020
First decision: November 24, 2020
Revised: November 26, 2020
Accepted: December 6, 2020
Article in press: December 6, 2020
Published online: January 26, 2021
Processing time: 70 Days and 10.4 Hours
Peripherally inserted central catheters (PICCs) have been increasingly applied worldwide owing to many advantages. Even with these advantages, the related complications should not be ignored, especially in neonates. The available evidence about PICC-related thrombosis was manifold, but the cardiac tamponade, an emergency and life-threatening complication, has been rarely reported. Early recognized cardiac tamponade by ultrasound may reduce mortality.
A neonate weighting 2.8 kg was born at 40 wk of gestation. He was admitted to the Surgery Intensive Care Unit due to suspected congenital megacolon. A PICC line was inserted via the left antecubital fossa for the administration of total parenteral nutrition. Three days later, the patient was still on total parenteral nutrition. Cardiac tamponade caused by PICC was found on ultrasound. The patient recovered spontaneously after an emergency pericardiocentesis.
Proficiency in the use of point-of-care ultrasound may save the life of patients, since it enables clinicians to treat patients faster, more accurately, and in a non-invasive way at the point of care.
Core Tip: Physicians should be vigilant to delayed cardiac tamponade even if the patient had been using peripherally inserted central catheters for several days. Proficiency in the use of point-of-care ultrasound may save the life of the patients in intensive care unit, emergency department, as well as operation rooms, since it enables clinicians to treat patients faster, more accurately, and in a non-invasive way at the point of care.
- Citation: Cui Y, Liu K, Luan L, Liang P. Delayed cardiac tamponade diagnosed by point-of-care ultrasound in a neonate after peripherally inserted central catheter placement: A case report. World J Clin Cases 2021; 9(3): 602-606
- URL: https://www.wjgnet.com/2307-8960/full/v9/i3/602.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i3.602
In modern clinical practice, total parenteral nutrition (TPN) is widely utilized as parenteral supportive therapy, which is necessary in neonates with surgical complications and inflammatory diseases. Continuous intravenous catheter placement is needed due to prolonged TPN, blood product infusions, and drug administration. In recent years, the application of peripherally inserted central catheters (PICCs), which have many advantages, has gradually increased worldwide. PICCs are performed by nurses, which facilitates their use and accessibility in many settings[1]. In addition, PICCs can be well preserved as a parenteral supportive treatment lasting up to 6 mo[1]. Compared to other central venous catheters (CVCs), PICCs are believed to be safer because PICCs are associated with a lower incidence of mechanical injury[2] and central line-associated bloodstream infection[3].
Despite the above benefits, PICCs-related complications should not be ignored, especially in neonates. The available evidence about PICC-related thrombosis was manifold[4], but the emergency and life-threatening complication cardiac tamponade caused by PICCs has been rarely reported. Early recognized cardiac tamponade by ultrasound may reduce mortality. Point-of-care ultrasound (POCUS) refers to the practice of trained medical professionals using ultrasound to diagnose problems wherever a patient is being treated, which has become very popular in China in recent years. We report a case of a neonate who developed life-threatening cardiac tamponade induced by PICCs and was diagnosed by POCUS.
A neonate weighing 2.8 kg was born at 40 wk of gestation. The Apgar score was 8 and 8 at 1 min and 5 min, respectively. Breastfeeding was started at the day of life. However, after 3 d, the neonate developed vomiting and abdominal distension. After collecting a detailed personal history and physical examination, the neonate was admitted to the Surgery Intensive Care Unit due to suspected congenital megacolon. Then, on the same day, a PICC line was inserted via the left antecubital fossa for the administration of TPN. Three days later, the patient was still on TPN. Sudden desaturation (oxygen saturation could not be measured) and bradycardia (heart rates between 30-40 beats/min) were noticed.
No data were available.
No data were available.
No data were available.
The patient was unresponsive. Blood pressure could not be measured, and oxygen saturation in room air was 60%.
No data were available.
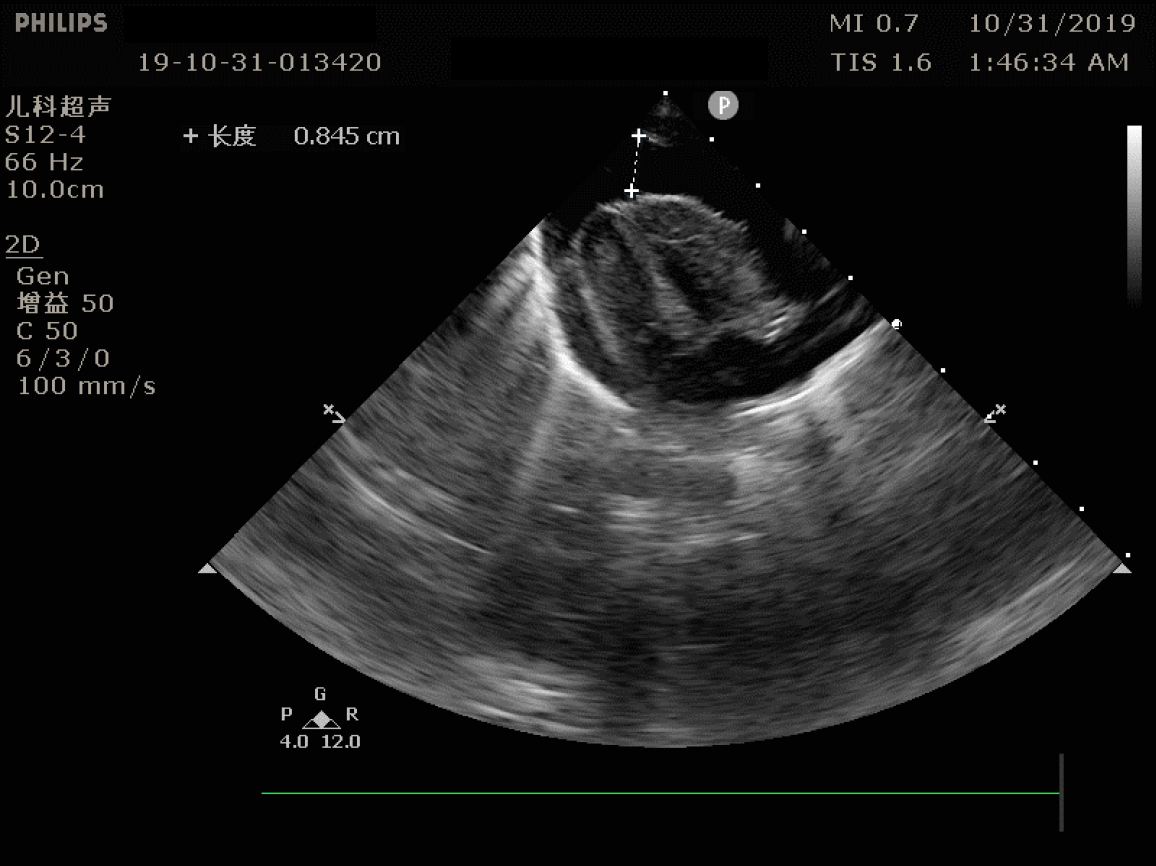
The urgent echocardiography demonstrated cardiac tamponade with more than 1 cm of deep fluid surrounding the heart (Figure 1).
Cardiac tamponade.
Cardiopulmonary resuscitation and emergency endotracheal intubation were conducted immediately. An emergency pericardiocentesis under the guide of ultrasound was conducted, and 15 mL creamy white fluid with a similar appearance of TPN was extracted. The patient improved spontaneously after the procedure. The heart rate increased to 150 beats/min, and oxygen saturation was up to 100%. The composition of the extracted creamy white fluid was detected to be TPN.
In fact, we reviewed the chest radiograph that was completed on post-PICC line placement. To our surprise, the tip of the PICC catheter was found in the right atrium. It was too deep, and hence the patient was more likely to be harmed (Figure 2); it had been unnoticed prior to this event.
Fortunately, the patient recovered and was discharged in a few days after appropriate treatments.
As an alternative for CVCs, PICCs are widely utilized in critically ill patients. However, the complications of thrombus and arrhythmia have been a concern of providers. Complications such as pericardial effusion and cardiac tamponade following PICC have been rarely reported, especially in neonates.
This is an interesting case as the PICCs-related cardiac tamponade was found by POCUS in a neonate. Because this incident was identified 3 d after the PICC placement, we believed that the PICC catheterization did not injure the heart during the procedure. We speculate that the cardiac tamponade may be caused by repeated motion friction at the tip of the PICC. The X-ray examination results after the PICC operation showed that the catheter tip entered the right atrium. Due to the small right atrium of neonates, thin atrial wall, and fast heart rate, continuous mechanical stimulation of the catheter tip might even puncture the atrium. In our case, the TPN was verified by detecting the composition of the extracted creamy white fluid, which confirmed our suspicions. In fact, a previous study had reported that tip location was one of independent risk factors of PICC-related complication. Therefore, it was essential to check the tip location of post-PICC placement and to review daily its function.
By reviewing the literature, we found that this was not the first case about PICCs-related cardiac tamponade. In 2016, Atmawidjaja and colleagues[5] reported a premature neonate with the PICCs-related cardiac tamponade, but they did not present the images of echocardiography and did not confirm that the intrapericardial fluid was TPN. The neonate died due to the acute life-threatening event that led to severe hypoxic-ischemic encephalopathy and multiple organs failure[5]. Furthermore, Atmawidjaja et al[5] reported a large pericardial effusion in a premature neonate who underwent 20 min active resuscitation before the bedside echocardiography. This might also be one of the reasons why their patient had a deteriorating prognosis. Compared to Atmawidjaja’s case, our patient had a better outcome following early diagnosis by POCUS and targeted treatments. When pericardial tamponade was diagnosed by POCUS, an emergency pericardiocentesis under the guide of ultrasound was conducted and the symptoms of cardiac compression were relieved immediately after the removal of tamponade.
In summary, the position of the catheter tip should be included in the checklist as part of routine clinical practice for post-PICC or CVCs placement. Proficiency in the use of POCUS may save the life of the patients in intensive care unit, emergency department, as well as operation rooms, since it enables clinicians to treat patients faster, more accurately, and in a non-invasive way at the point of care.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhang HJ S-Editor: Chen XF L-Editor: Filipodia P-Editor: Wang LL
| 1. | Campagna S, Gonella S, Berchialla P, Rigo C, Morano G, Zerla PA, Fuzzi R, Corona G, Storto S, Dimonte V, Mussa B. A retrospective study of the safety of over 100,000 peripherally-inserted central catheters days for parenteral supportive treatments. Res Nurs Health. 2019;42:198-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Zhao H, He Y, Wei Q, Ying Y. Medical Adhesive-Related Skin Injury Prevalence at the Peripherally Inserted Central Catheter Insertion Site: A Cross-sectional, Multiple-Center Study. J Wound Ostomy Continence Nurs. 2018;45:22-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 3. | Yamaguchi RS, Noritomi DT, Degaspare NV, Muñoz GOC, Porto APM, Costa SF, Ranzani OT. Peripherally inserted central catheters are associated with lower risk of bloodstream infection compared with central venous catheters in paediatric intensive care patients: a propensity-adjusted analysis. Intensive Care Med. 2017;43:1097-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 4. | Chopra V, Anand S, Hickner A, Buist M, Rogers MA, Saint S, Flanders SA. Risk of venous thromboembolism associated with peripherally inserted central catheters: a systematic review and meta-analysis. Lancet. 2013;382:311-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 431] [Cited by in RCA: 454] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 5. | Atmawidjaja RW, Azri M, Ismail IH. Cardiac tamponade: a rare but preventable complication of central venous catheter in neonates. Med J Malaysia. 2016;71:147-148. [PubMed] |