Published online Oct 6, 2021. doi: 10.12998/wjcc.v9.i28.8545
Peer-review started: May 18, 2021
First decision: June 24, 2021
Revised: June 27, 2021
Accepted: July 26, 2021
Article in press: July 26, 2021
Published online: October 6, 2021
Processing time: 132 Days and 22.3 Hours
Lumbar facet joint syndrome (LFJS) is a pain condition arising from lumbar facet joint diseases. Treatments of LFJS includes patient education, oral medication, bed rest, physical therapy, and procedural interventions. For some refractory cases that fail conservative therapies, dorsal ramus medial brunch radiofrequency ablation is warranted. However, as nerve fibers can regenerate, their efficacy is impermanent, and the recurrence rate is relatively high. Considering synovial impingement is a paramount pathogenesis of LFJS, in this case, we removed the culprit hyperplastic articular capsule and the articular process partially through a spinal endoscope. As the culprit hyperplastic joint capsule was excised, it is supposed to generate more prolonged efficacy and a lower recurrence rate than radiofrequency treatment.
A 40-year-old female patient was diagnosed with LFJS. She complained of low back pain and right buttock pain for half a year. The patient was placed in the prone position. After disinfection and draping, a 25-cm 18-gauge needle was inserted into the dorsal surface of the right L5 articular process. Subsequently, a guidewire, dilating tubes, and a working cannula was inserted successively. The spinal endoscope was positioned in the working cannula. Under the endoscope, the microvascular tissue, muscle tissue attached on the L5 inferior articular process and S1 superior articular process, as well as the capsule and minor portion of the inferior articular process were removed. After the joint space was clear and no bleeding points existed, the endoscope and working cannula were shifted, and the incision was sutured. After treatment, the symptoms were completely relieved. The patient was pain-free during the follow-up period of 6 mo.
The endoscopic partial joint capsule and articular process excision is an effective procedure for LFJS, especially for cases caused by synovial impingement.
Core Tip: For intractable lumbar facet joint syndrome (LFJS), medial branch radiofrequency ablation is a commonly used therapy. However, the recurrency rate of radiofrequency treatment is relatively high. In this case, we removed the lumbar facet joint capsule and articular process partially through the guidance of endoscope. The patient's symptoms were relieved for the next 6 mo. We assert that this treatment can generate long-lasting efficacy as this innovative treatment directly removes the hyperplastic joint capsule. It is supposed to be an effective treatment for LFJS caused by synovial impingement.
- Citation: Yuan HJ, Wang CY, Wang YF. Endoscopic joint capsule and articular process excision to treat lumbar facet joint syndrome: A case report. World J Clin Cases 2021; 9(28): 8545-8551
- URL: https://www.wjgnet.com/2307-8960/full/v9/i28/8545.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i28.8545
Lumbar facet joint syndrome (LFJS) is a pain condition arising from lumbar facet joint disease. As a common disease, LFJS accounts for about 15%-40% of low back pain patients[1,2]. The treatments of LFJS include patient education, oral medication, bed rest, physical therapy, and procedural interventions[3]. For patients refractory to preservative treatments, dorsal ramus medial brunch radiofrequency ablation is widely applied. However, as nerve fibers can regenerate, their efficacy is imper
A 40-year-old female patient complained of low back pain for half a year. The pain was located mainly at the right side of the lumbar back, and radiated to the right buttock. The pain was aggravated during lumbar dorsal extension and left lateral flexion. The patient felt obvious pain, especially during the cause of unbending the waist from the sitting position. The pain could be alleviated during lumbar anterior bending. She could walk and stand normally. A long time of standing and sitting did not aggravate pain. The VAS score was 4.
The patient was diagnosed with LFJS in other clinics and underwent oral medication, bed rest, facet joint steroid injection, etc. However, the symptoms could only be relieved slightly and temporarily.
No history of high blood pressure, diabetes mellitus, and no history of trauma existed.
No family history of chronic low back pain was reported.
Physical examination manifested tenderness on the paravertebral region on the L5-S1 level. The lower leg muscle force and sensory function were normal. The straight leg raising test was negative.
Complete blood count, erythrocyte sedimentation rate, and automated blood chemistry testing were within the normal range.
The lumbar spine magnetic resonance imaging (MRI) indicated degenerative changes in the L5-S1 disc and with no sign of spinal nerve compression (Figure 1). Plain radiography was standard. Lateral flexion and extension views showed no sign of lumbar instability.
The diagnosis was confirmed as LFJS, and the culprit’s joint was defined as right L5-S1.
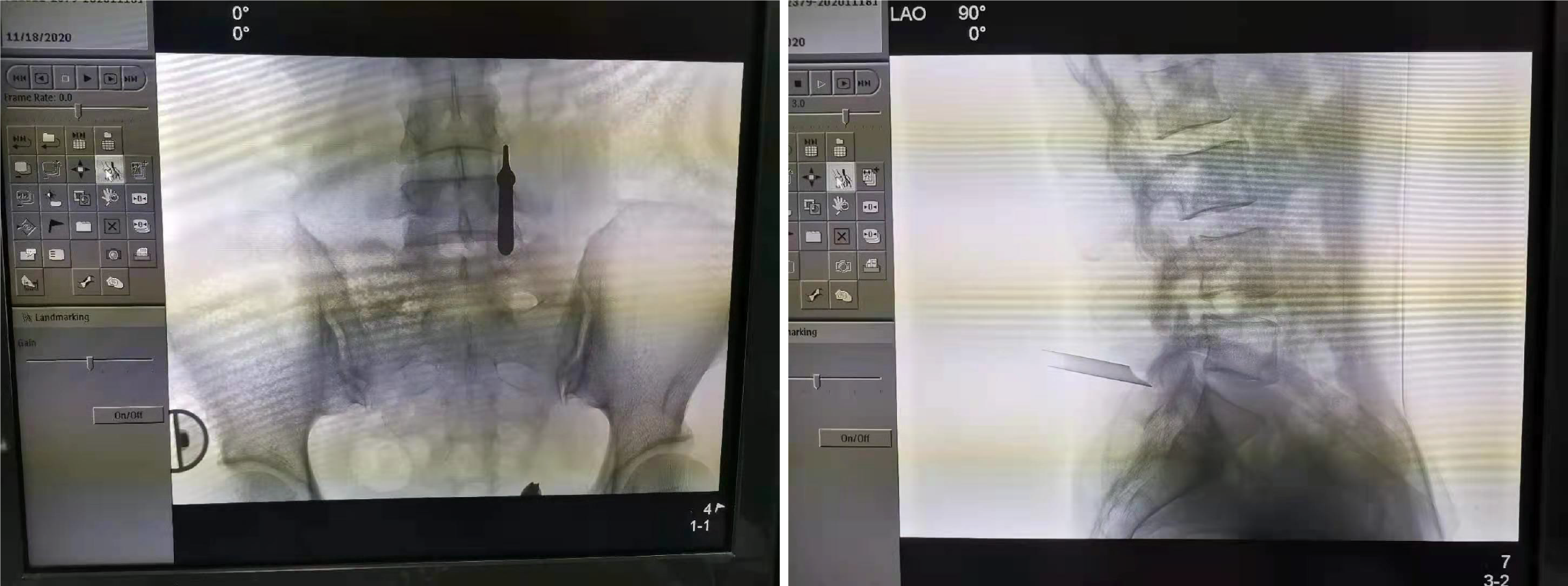
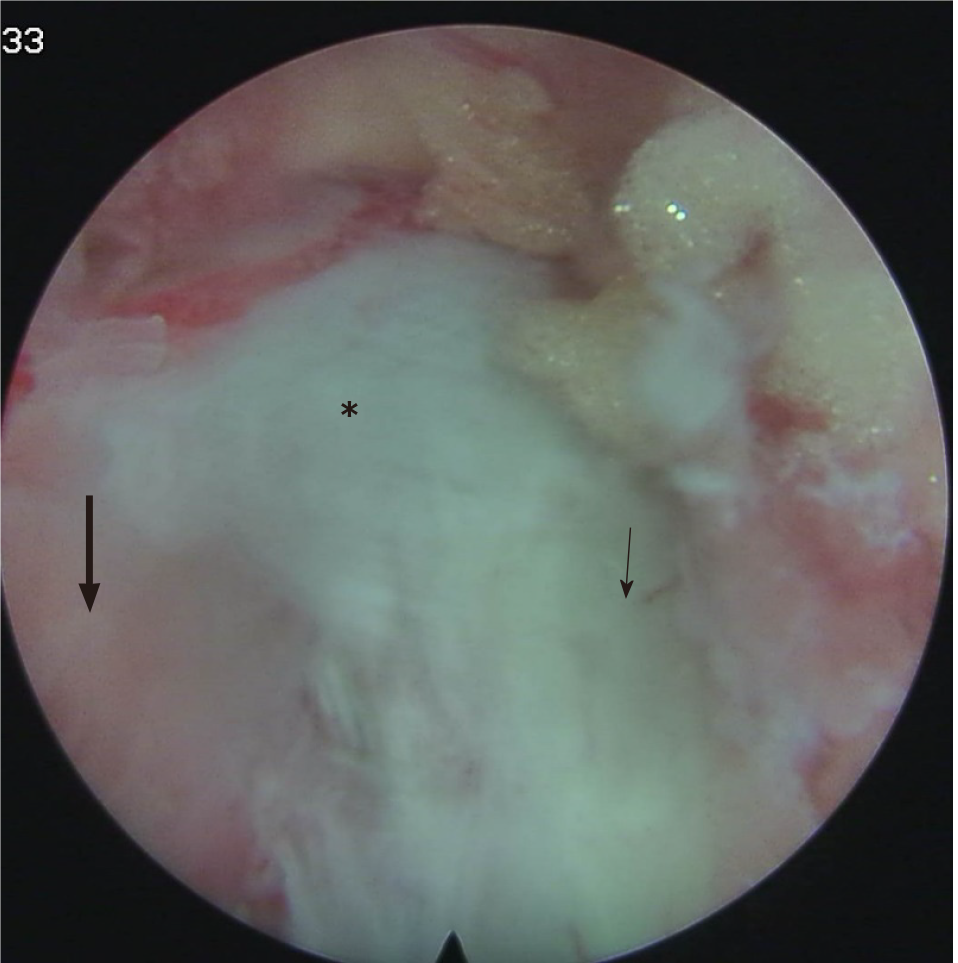
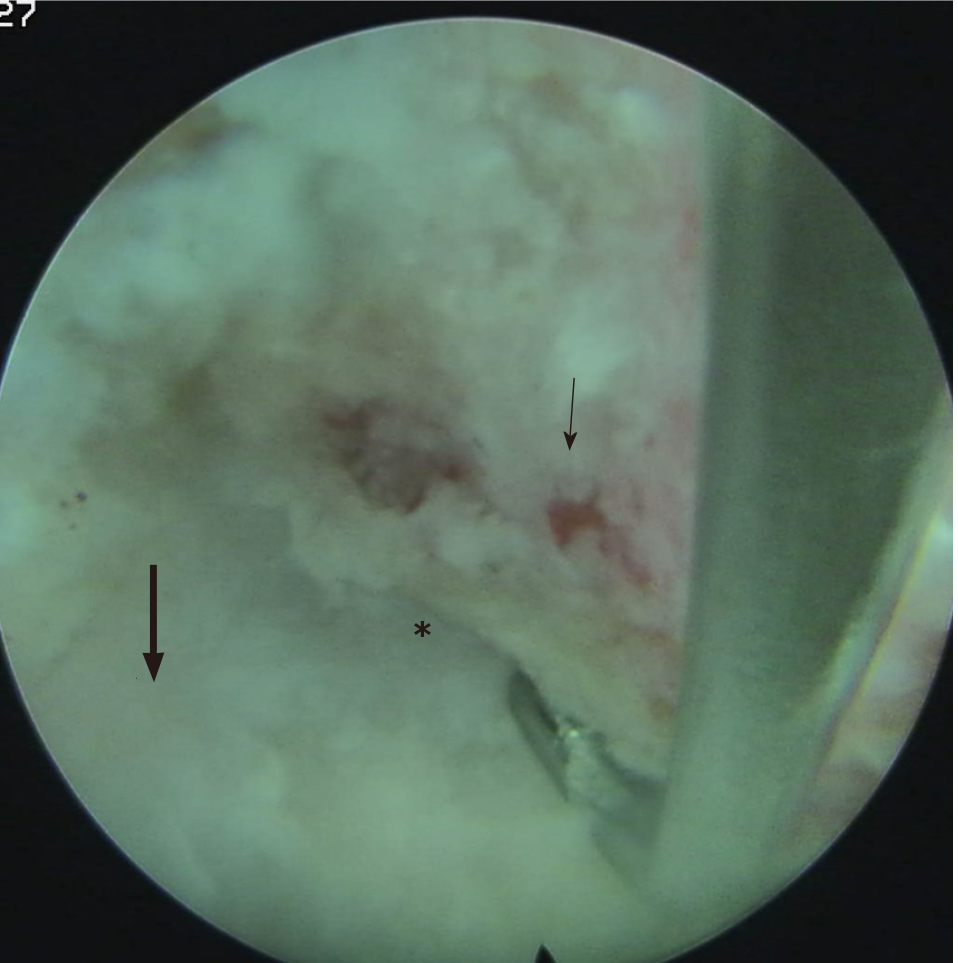
As the conservative treatments failed, endoscopic partial joint capsule and articular process excision were warranted. After the medical consent form was signed, the patient was placed in the prone position with a pillow under the abdomen to flex the lumbar spine. The right L5-S1 facet joint was positioned by a C arm X-ray and was marked. After disinfection, draping, and local anesthesia, a 25-cm 18-gauge needle was punctured into the dorsal surface of the right L5 articular process. Subsequent anteroposterior confirmed the location. A guidewire was inserted through the stylet, the dilating tubes, and the working canal was inserted successively through a 0.7-cm skin incision centered on the guidewire. Anteroposterior view and lateral view confirmed that the working cannula was located on the posterior surface of the L5-S1 facet joint (Figure 2). The spinal endoscope was positioned through the working cannula. The microvascular tissue, muscle tissue attached to the L5 inferior articular process and S1 superior articular process was removed endoscopically by a grasper. The bipolar radiofrequency probe was used for hemostasis. L5 inferior articular process, S1 superior articular process, the joint capsule was exposed (Figure 3). After the removal of the capsule, the joint space was revealed. A minor portion of the articular process was removed with a chisel. The tissue compressed in the joint space was also wiped out. After the joint space was clear and no bleeding points were existed (Figure 4), the endoscope and the working cannula were removed, and the incision was sutured.
After the treatment, the symptoms were utterly relieved. The patient was pain-free during the follow-up period of 6 mo. No complication was observed.
Low back pain was generally acknowledged as a highly complicated and hard-to-diagnose disease in clinical practice. Lumbar disc, facet joint, lumbar muscular fascia, and the sacroiliac joint were all possible pain generators[3]. LFJS is defined as a pain condition emanating from facet joint lesions. The pathologic changes of LFJS include facet joint arthritis, synovial impingement, meniscoid entrapment, pseudogout and intrafacetal cysts, etc.[6]. LFJS account for about 15%-40% of low back pain patients[1,2].
As the pathogenesis of LFJS varied, the diagnosis of LFJS is relatively complicated. The diagnosis should be supported by a combination of clinical history, physical examination, radiography, and diagnostic block, the latter of which is the most reliable method for diagnosis[3,7]. In this case, based on typical symptoms, physical examination as well as positive diagnostic block, the diagnosis of LFJS was verified.
Treatment for LFJS should be multimodal, consisting of conservative and interventional treatments. It was generally accepted that interventional therapy was necessitated after conservative treatments failed. Medial branch radiofrequency was the most commonly applied therapy, and reported to be an effective therapy for LFJS with high-level evidence[8-11]. As the mechanism of radiofrequency therapy is to ablate the nociceptive nerve conduction, the duration of treatment was reported to be 6 mo to 1 year, as the nerve fibers may regenerate[8,9,12,13]. Apart from medial brunch radiofrequency, Song reported endoscopic medial branch neurotomy to treat LFJS[14]. This innovative treatment was reported to generate a longer pain relief duration compared to conventional radiofrequency treatment. However, the mechanism of the two treatments was the same. Therefore, after nerve regeneration, symptoms relapse may also occur. Facet joint osteoarthritis is reportedly the primary pathological mechanism for facet joint syndrome[15]. However, in this case, the lumbar spinal MRI indicated no significant lesion of the facet joint. Instead, the patient’s pain could be aggravated during lumbar dorsal extension and left lateral flexion, especially during the cause of unbending the waist from sitting position and relieved during lumbar anterior bending. From her symptoms, we speculated that synovial impingement or meniscoid entrapment might exist and be located at the dorsal part of the facet joint in this case (the exact reason will be discussed below). Therefore, we implemented endoscopic partial facet joint capsule and articular process excision instead of medial brunch radiofrequency, which applied conventionally.
The superiority of endoscopic partial joint capsule and articular process excision over radiofrequency treatment was supposed to be longer and even permanent pain relief as the culprit hyperplastic joint capsule was removed. However, the theory mentioned above is based on presumption and necessitates further clinical research.
Haufe and Mork[5] reported a novel treatment named endoscopic facet debridement to treat facet arthritic pain. However, in this paper, the facet joint capsule was removed but not the articular process, and multiple facet joint capsules were removed. The reported therapeutic theory was to clear out the end-plate receptors located on the joint capsule, and aimed the procedure was to treat facet arthritic pain. In our case, apart from resecting the joint capsule, a minor part of the lower articular process was removed to expose the joint space and clear out the hyperplastic capsule compressed in the joint space. And our procedure was for the treatment of LFJS due to synovial impingement.
A point to note is which segment of facet joint should be treated. In our pain clinic, we chose the segment where the tenderness was located and the segment corresponding to the affected lumbar disc. As reported by Song et al[16], facet joint lesions tend to occur at the same level of narrowed lumbar disc. For example, if the patient’s MRI indicated L4-5 lumbar disc degeneration, especially the decreased height of the disc, the L4-5 facet joint was the most likely culprit joint.
Another point that merits consideration is which part of the facet and joint capsule should be removed. No report was available regarding the right point the articular capsule was entrapped. For this case, the pain was aggravated during lumbar dorsal extension and left lateral flexion, especially during the cause of unbending the waist from sitting position. The most likely point the capsule compressed is the dorsal part of the facet joint, as the dorsal joint gap widens during lumbar flexion and narrows during lumbar extension. As the widening of the joint gap, the compressed capsule is also relaxed, and the symptoms will be relieved accordingly. By contrast, as the joint gap narrowed, the capsule compression of the joint gap will be more severe. After that, the symptom will be aggravated.
The impact on the lumbar stability was the last but not the slightest concern for endoscopic partial joint capsule and articular process excision. However, the axial load is mainly supported by the lumbar disc. The facet joint only plays a minor role in load bearing[17]. Furthermore, only a tiny part of the joint was removed. Therefore, we argue that the procedure has little impact on lumbar stability.
This study had some limitations. First, the follow-up period of this case was relatively short. Second, the superiority of endoscopic partial joint capsule and articular process excision over medial brunch radiofrequency treatment was grounded by presumption. Therefore, further clinic trial with more participants and a more extended follow-up period was warranted.
Endoscopic partial joint capsule and articular process excision is an effective procedure for LFJS, especially for cases caused by synovial impingement. As the culprit hyperplastic joint capsule was removed, it is supposed to more prolonged and even permanent efficacy and a lower recurrence rate.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anandan H S-Editor: Yan JP L-Editor: Filipodia P-Editor: Wang LYT
| 1. | Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WD, Carey TS. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169:251-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 861] [Cited by in RCA: 968] [Article Influence: 60.5] [Reference Citation Analysis (0)] |
| 2. | Schwarzer AC, Wang SC, Bogduk N, McNaught PJ, Laurent R. Prevalence and clinical features of lumbar zygapophysial joint pain: a study in an Australian population with chronic low back pain. Ann Rheum Dis. 1995;54:100-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 235] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 3. | Perolat R, Kastler A, Nicot B, Pellat JM, Tahon F, Attye A, Heck O, Boubagra K, Grand S, Krainik A. Facet joint syndrome: from diagnosis to interventional management. Insights Imaging. 2018;9:773-789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 121] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 4. | Moussa WM, Khedr W. Percutaneous radiofrequency facet capsule denervation as an alternative target in lumbar facet syndrome. Clin Neurol Neurosurg. 2016;150:96-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Haufe SM, Mork AR. Endoscopic facet debridement for the treatment of facet arthritic pain--a novel new technique. Int J Med Sci. 2010;7:120-123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Saravanakumar K, Harvey A. Lumbar Zygapophyseal (Facet) Joint Pain. Rev Pain. 2008;2:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007;106:591-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 278] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 8. | Cohen SP, Bhaskar A, Bhatia A, Buvanendran A, Deer T, Garg S, Hooten WM, Hurley RW, Kennedy DJ, McLean BC, Moon JY, Narouze S, Pangarkar S, Provenzano DA, Rauck R, Sitzman BT, Smuck M, van Zundert J, Vorenkamp K, Wallace MS, Zhao Z. Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group. Reg Anesth Pain Med. 2020;45:424-467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 129] [Cited by in RCA: 177] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 9. | Leggett LE, Soril LJ, Lorenzetti DL, Noseworthy T, Steadman R, Tiwana S, Clement F. Radiofrequency ablation for chronic low back pain: a systematic review of randomized controlled trials. Pain Res Manag. 2014;19:e146-e153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. | Adams MA, Hutton WC. The effect of posture on the role of the apophysial joints in resisting intervertebral compressive forces. J Bone Joint Surg Br. 1980;62:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 257] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 11. | Manchikanti L, Kaye AD, Soin A, Albers SL, Beall D, Latchaw R, Sanapati MR, Shah S, Atluri S, Abd-Elsayed A, Abdi S, Aydin S, Bakshi S, Boswell MV, Buenaventura R, Cabaret J, Calodney AK, Candido KD, Christo PJ, Cintron L, Diwan S, Gharibo C, Grider J, Gupta M, Haney B, Harned ME, Helm Ii S, Jameson J, Jha S, Kaye AM, Knezevic NN, Kosanovic R, Manchikanti MV, Navani A, Racz G, Pampati V, Pasupuleti R, Philip C, Rajput K, Sehgal N, Sudarshan G, Vanaparthy R, Wargo BW, Hirsch JA. Comprehensive Evidence-Based Guidelines for Facet Joint Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines Facet Joint Interventions 2020 Guidelines. Pain Physician. 2020;23:S1-S127. [PubMed] |
| 12. | Shih CL, Shen PC, Lu CC, Liu ZM, Tien YC, Huang PJ, Chou SH. A comparison of efficacy among different radiofrequency ablation techniques for the treatment of lumbar facet joint and sacroiliac joint pain: A systematic review[ and meta-analysis. Clin Neurol Neurosurg. 2020;195:105854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | McCormick ZL, Choi H, Reddy R, Syed RH, Bhave M, Kendall MC, Khan D, Nagpal G, Teramoto M, Walega DR. Randomized prospective trial of cooled vs traditional radiofrequency ablation of the medial branch nerves for the treatment of lumbar facet joint pain. Reg Anesth Pain Med. 2019;44:389-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Song K, Li Z, Shuang F, Yin X, Cao Z, Zhao H, Qin J. Comparison of the Effectiveness of Radiofrequency Neurotomy and Endoscopic Neurotomy of Lumbar Medial Branch for Facetogenic Chronic Low Back Pain: A Randomized Controlled Trial. World Neurosurg. 2019;126:e109-e115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Kalichman L, Li L, Kim DH, Guermazi A, Berkin V, O'Donnell CJ, Hoffmann U, Cole R, Hunter DJ. Facet joint osteoarthritis and low back pain in the community-based population. Spine (Phila Pa 1976). 2008;33:2560-2565. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 267] [Cited by in RCA: 224] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 16. | Song Q, Liu X, Chen DJ, Lai Q, Tang B, Zhang B, Dai M, Wan Z. Evaluation of MRI and CT parameters to analyze the correlation between disc and facet joint degeneration in the lumbar three-joint complex. Medicine (Baltimore). 2019;98:e17336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Inoue N, Orías AAE, Segami K. Biomechanics of the Lumbar Facet Joint. Spine Surg Relat Res. 2020;4:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |