Published online Sep 6, 2021. doi: 10.12998/wjcc.v9.i25.7605
Peer-review started: April 28, 2021
First decision: June 15, 2021
Revised: June 16, 2021
Accepted: July 15, 2021
Article in press: July 15, 2021
Published online: September 6, 2021
Processing time: 124 Days and 17.5 Hours
Both periprosthetic joint infections (PJIs) and severe femoral segmental defects are catastrophic complications of total hip arthroplasty (THA), and both present a significant challenge in revisional surgery. There are limited data available to guide clinical decision making when both occur concurrently.
A 61-year-old woman presented with a 6-mo history of a sinus tract at the site of her original THA incision. Radiological imaging revealed a total hip joint implant with an ipsilateral segmental femoral defect. Based on histological, radiological, laboratory, and clinical features, a diagnosis of concurrent chronic PJI and segmental femoral defect (Type IIIB, Paprosky classification) was made. After multidisciplinary team discussion, three-dimensional (3D)-printed, custom-made antibiotic spacers were created that could be used to mold antibiotic-loaded cement spacer. These were placed following PJI debridement in the first stage of revision surgery. After the PJI was eliminated, a 3D-printed, custom-made, femoral prosthesis was created to repair the considerable femoral defect. After 20-mo follow-up, the patient had excellent functional outcomes with a near-normal range of hip movement. So far, neither evidence of recurrent infection nor loosening of the prosthesis has been observed.
We describe a case of “two-stage, custom-made” total hip revision to treat PJI with a concurrent segmental femoral defect. Use of a personalized, 3D-printed spacer and proximal femoral prosthesis led to satisfactory hip function and no early postoperative complications. Use of a customized implant provides surgeons with an alternative option for patients where no suitable spacer or implant is available. However, the long-term function, longevity, and cost-effectiveness of the use of custom-made prostheses have yet to be fully explored.
Core Tip: This paper reports a pioneering technique where a 3D-printed, custom-made antibiotic spacer and femoral prosthesis were used in revisional surgery for a challenging case of periprosthetic joint infection with a concurrent femoral segmental defect after total hip arthroplasty. A review of other relevant cases from the literature is presented, and the potential challenges and solutions of novel, personalized reconstructive methods are discussed.
- Citation: Liu YB, Pan H, Chen L, Ye HN, Wu CC, Wu P, Chen L. Total hip revision with custom-made spacer and prosthesis: A case report. World J Clin Cases 2021; 9(25): 7605-7613
- URL: https://www.wjgnet.com/2307-8960/full/v9/i25/7605.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i25.7605
The safety and effectiveness of total hip arthroplasty (THA) have led to this being one of the most commonly performed operations worldwide, with more than 1 million hips replaced each year according to Organisation for Economic Co-operation and Development (OECD) data[1]. With the rise in the volume of primary THA performed, the total volume of revisional surgery (including complex re-revision) is projected to grow by 137% in the United States by 2030[2]. Infection and significant bone defects after THA are devastating and costly complications that are challenging to resolve. Here we present a rare case of two-stage revisional surgery for THA, in which both a 3D-printed, customized spacer and proximal femur prosthesis (PFP) were used to manage periprosthetic joint infection (PJI) with a concurrent segmental femoral defect.
A 61-year-old woman presented to our orthopaedic service with a 6-mo history of a non-healing ulcer and tract over the site of her original THA incision.
The patient reported low-grade fevers, particularly in the afternoons, and she had received several previous courses of antibiotics for deep infection at the wound site.
In September 2012, the patient had a severe car accident and was diagnosed with a left distal radius and ulna fracture (23r-E/4.2 and 23 μmol/L/3.1; ICD-10: S52.50 and S52.60), left acetabular fracture (62B3.1; ICD-10: S32.40), left femoral intertrochanteric and ipsilateral head fracture (31A2.3 & 31C1.3; ICD-10: S72.14 & S72.05), right-sided transverse process fracture at L1(ICD-10: S32.01), and multiple left-sided rib fractures (5-7th, 9th, 11th, ICD-10: S22.42). Internal fixation of the left proximal femoral fracture and ipsilateral femoral head fracture was performed, but later failed and she underwent total hip arthroplasty (THA) appropriately 6 mo after her initial injury. Four years after her primary THA, the patient had required a further open reduction of the replaced left hip due to another accident.
No other relevant family history was reported
On examination, the patient had swelling over the left hip region, with mild pain on pressing the swollen area. The healed THA wound site was moist with pale secretions, and a deep leading sinus tract was identified.
The patient’s haematological profile revealed a raised erythrocyte sedimentation rate (ESR, 74 mm/h; normal: 0-20 mm/h), and biochemistry demonstrated a raised level of C-reactive protein (CRP, 48.3 mg/L; normal: 0-8 mg/L). All other blood results were within normal limits. A swab test along the sinus tract grew an Enterococcus species on culture, which was consistent with the previous sinus tract examination
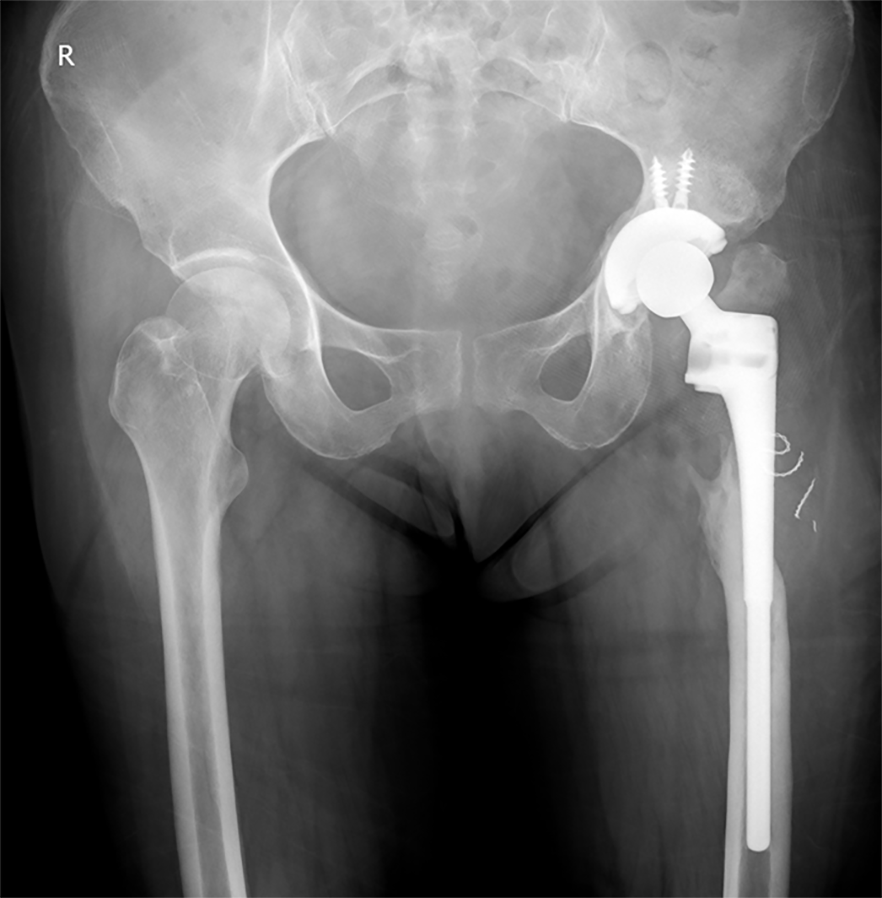
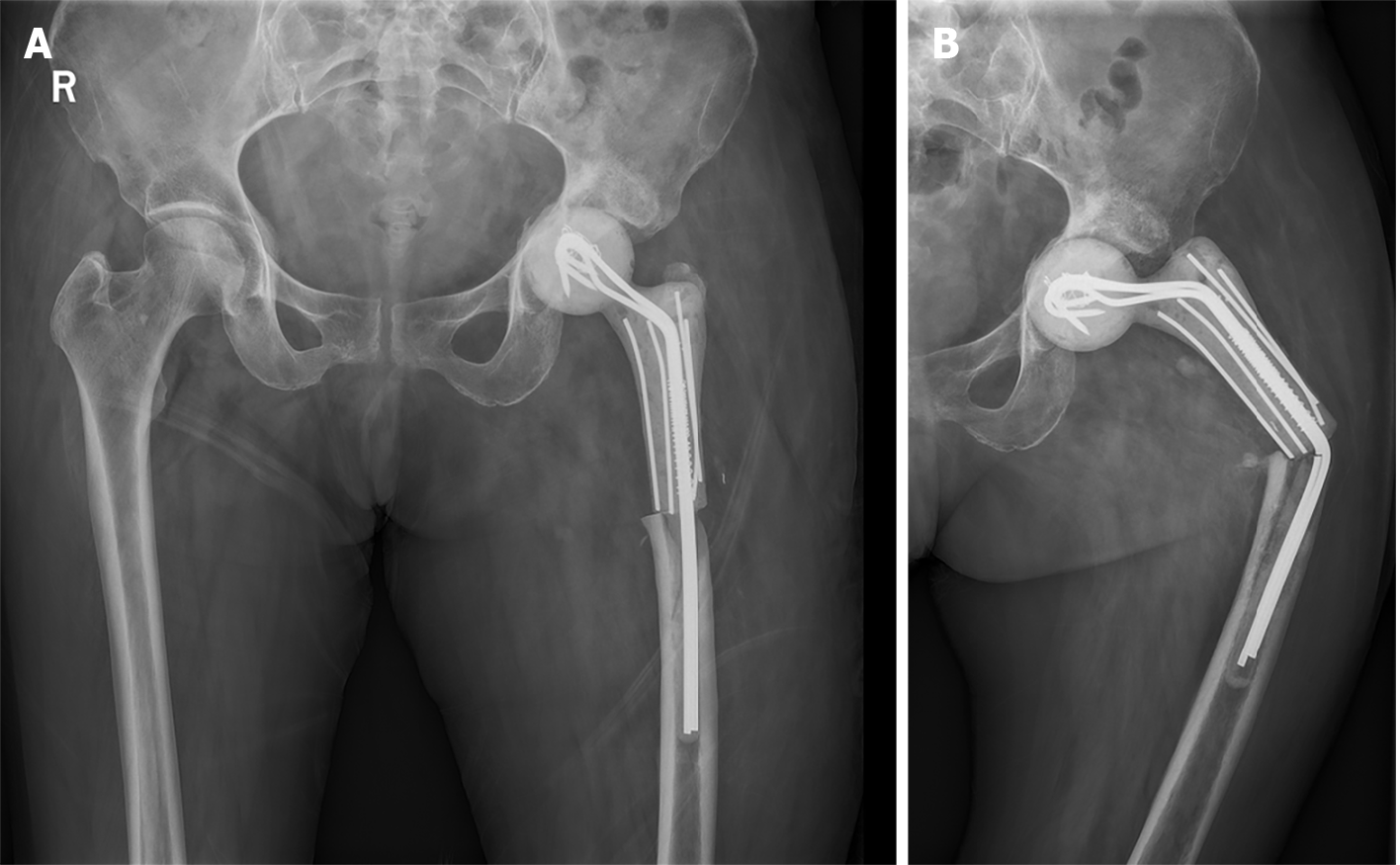
Plain radiography of the left hip in the anteroposterior plane demonstrated a post-THA hip with a severe proximal femoral defect (Figure 1).
The result of histological examination of a biopsy sample and bacterial cultures from the non-healing sinus tract over the incision site scar led to a diagnosis of PJI (ICD-10: T84.52), corroborated by the serum biochemistry results[3]. The femoral defect was classified using the Paprosky system as Type IIIB, and the acetabular defect as Type IIC.
Two-stage total hip revisional surgery was conducted using a 3D-printed, customized antibiotic-loaded cement spacer (ALCS) during the first stage and a personalized proximal femur prosthesis (PFP) for the second stage. Postoperatively, intravenous vancomycin was administered twice daily at a dose of 15 mm/kg for the first 7 postoperative days, followed by oral moxifloxacin (400 mg every 24 h) for a further 2 wk as recommended by the DISA (Infectious Diseases Society of America) guidelines[4].
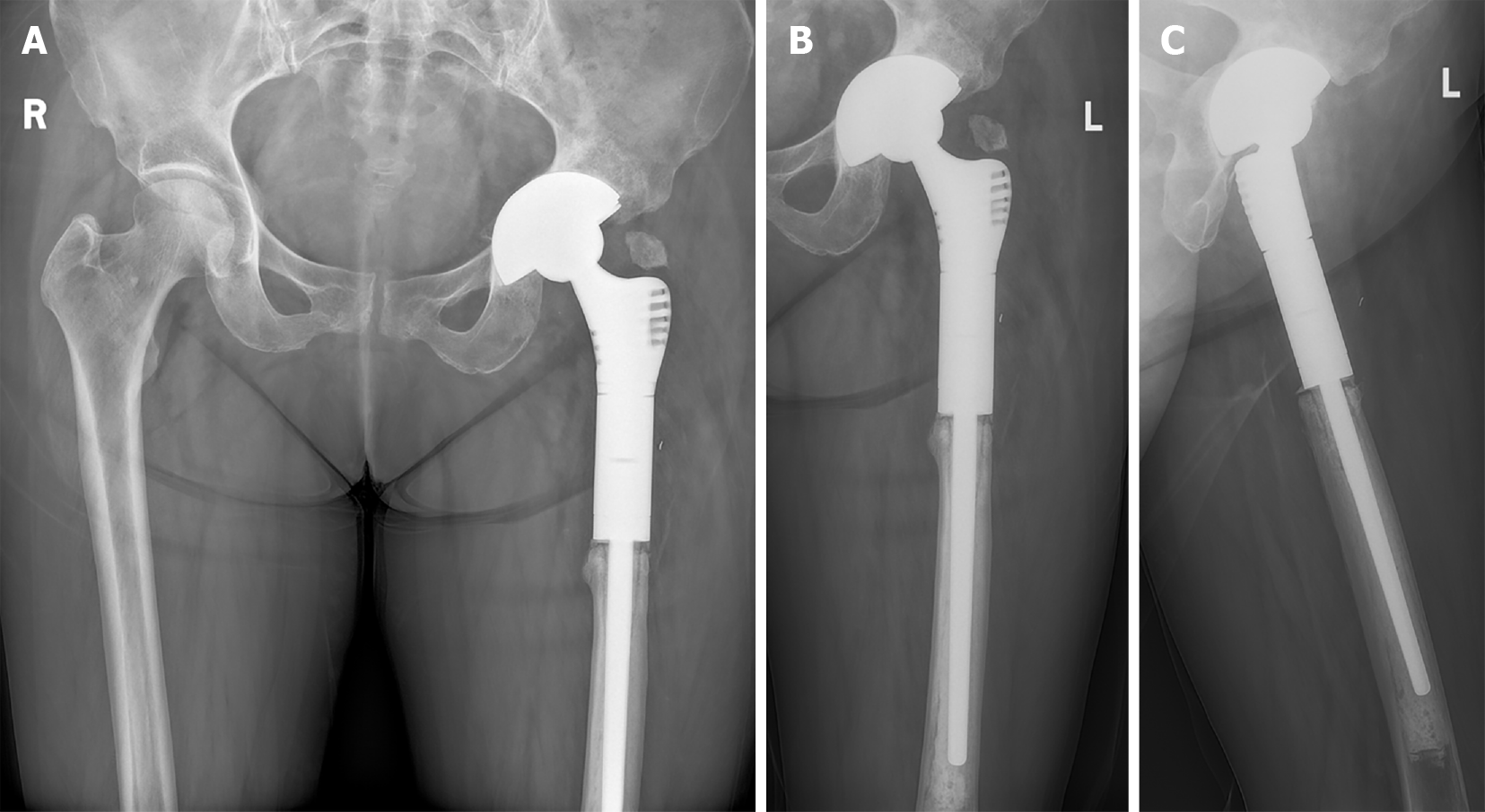
Postoperative inflammatory markers, including ESR and CRP, were monitored weekly for 8 wk, revealing the return to the normal range within 4 wk. The patient was kept non-weight bearing for 6 wk from the day of surgery, and then was allowed to partially weight bear for the following 6 wk before full weight bearing at 12 wk after surgery onwards. At her last follow-up (20 mo after surgery), she was asymptomatic and had significant functional improvement of her left hip with a Harris Hip Score of 91. Radiographs demonstrated no signs of implant loosening (Figure 2), and her serum markers were within normal limits.
This report describes a challenging case of chronic PJI with a concomitant segmental femoral defect, which were managed by a two-stage revisional procedure using custom-made, 3-D printed ALCS and PFP, respectively. There were several key learning points throughout the treatment pathway that will be beneficial for surgeons faced with this challenge in the future.
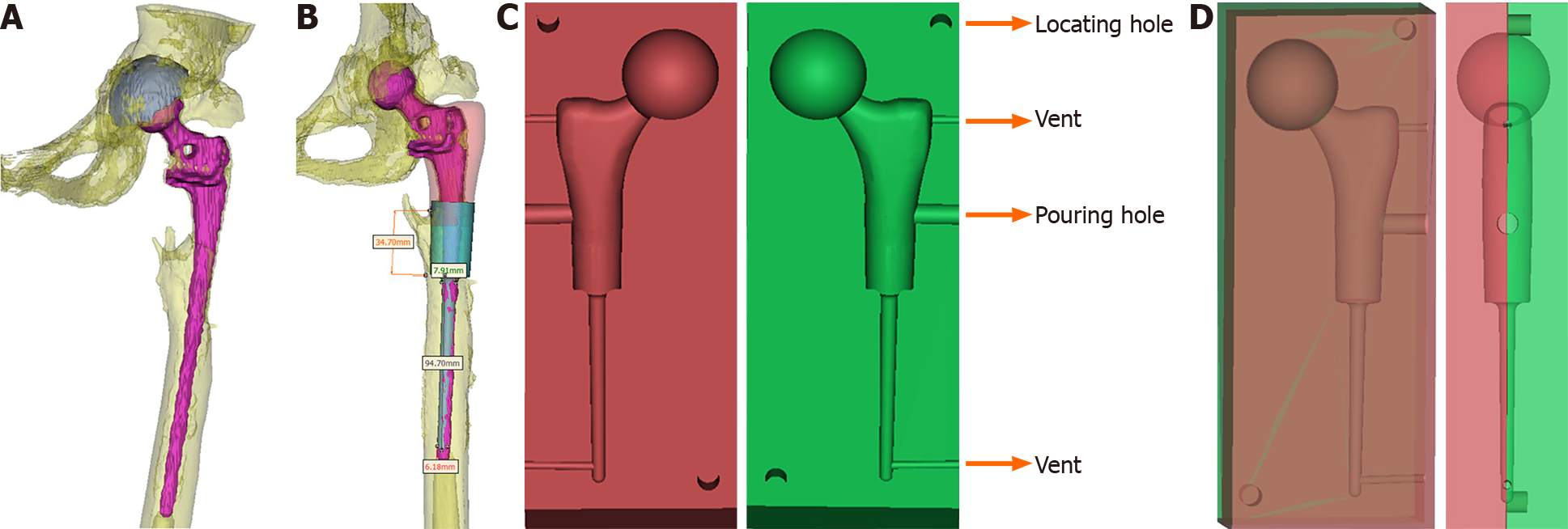
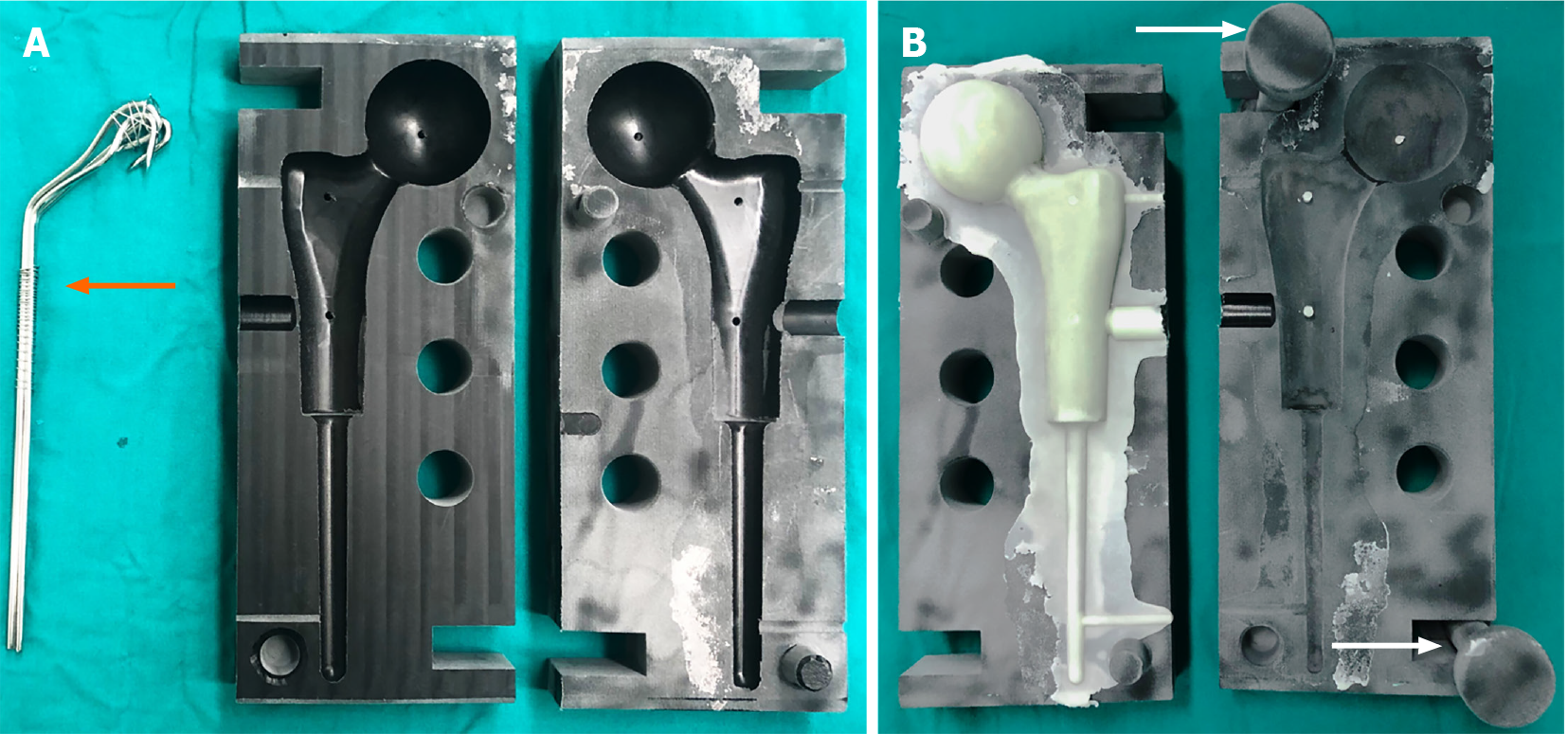
Prefabricated antibiotic-loaded interval spacers are available in various configurations. However, certain cases with complex anatomy and pathoaetiology warrant custom-made spacers. In the previous literature, both standard and customized spacers have similar infection clearance rates, and each has their own merits based on the clinical circumstances[5,6]. In this case, the treating surgeon attempted to manually transform an “off-the-shelf” spacer to fix the anatomy[7], but the reformed spacers were inadequate. Therefore, customized spacer molds were designed using computed tomography (CT) and three-dimension (3D) model data (Figure 3A and B). The molds were divided into two blocks, which could be accurately aligned using complementary locating bars and holes. Several discharge channels were included to allow space for excess cement to be removed (Figure 3C and D). The custom-made ALCS (Figure 4A and B) replaced the infected prosthesis to create a near anatomical left hip joint (Figure 5A). The patient was so satisfied with the first-stage revision that she consistently refused her scheduled 2nd-stage until a second fall occurred 6 mo after the first-stage surgery (Figure 5B).
A binding bundle of Kirschner wires surrounded by several single wires was settled to strengthen the positioning of the ALCS. This remained functional in the patient's body for nearly 6 mo (2 to 3 times longer than expected).
In our experience, the advantages of custom-made spacers included retention of limb length and lateral offset, both of which made it easier to perform further revisional surgery[8]. Moreover, custom-made spacers also allow the treating surgeon to control the type and dosage of antibiotics[9].
After reviewing sensitivities of the bacterial culture, 2 g of vancomycin were combined with each pouch of PALACOS MV+G cement, which delivered a safe and effective dosage of gentamicin[10]. Because ALCS can deliver high local concentrations of antibiotics, this can enter systemic circulation and result in toxicity or other adverse reactions such as acute renal failure, hepatic failure, and bone marrow depression[11,12]. Due to the high local concentration of vancomycin in the custom-made ALCS, the concentration of intravenous vancomycin administered postoperatively was down-titrated to ensure safe levels of delivery. The patient’s serum vancomycin concentration after surgery has been maintained above twice the minimal inhibitory concentration as recommended by Whiteside et al[13].
Reports to date of the operative management of severe proximal femoral osteopenia (classified as Paprosky types IIIB and IV) have included impaction grafting[14], allograft prosthesis composite (APC)[15,16], and prosthetic implants (i.e., modular mega-prostheses)[17]. Each of these methods has unique advantages and limitations[17-19]. Standard modular prostheses are an available option for proximal femoral reconstruction in many cases and have been developed to be broadly applicable across several patient groups and fracture morphologies. Where standard prosthetic implantation is feasible, the estimated 5-year survival rate is encouraging at approximately 90.7%[20]. However, for some cases, custom-made prosthesis is needed to facilitate reconstruction (Table 1)[21-26].
| Ref. | No. of patients | Patient age (yr) | Follow-up (yr) | PJI | Type of femoral defect | Clinical outcome | Complications | Custom method |
| Jones et al[21] | 1 in 9 | 60 | 3.3 | Chronic (for 50 yr) | Girdlestone resection | No recurrence of infection; walk unaided | - | - |
| Hsieh et al[22] | 9 in 24 | 59 (average) | 4.2 (average) | All chronic | Type-III1: 6 caseType-I1: 3 case | No recurrence of infection | 2 fractures & 1 dislocation | Spacer and femoral cement prosthesis with allografts |
| Westerman et al[23] | 1 | 14 | 0.8 | No infection | III-B2 | Symptom free | - | CT reconstruction |
| Wang et al[24] | 1 | 73 | 2 | No infection | III-B2 | Symptom free | - | 3D printed titanium sleeve-prosthetic with allografts |
| Kamath et al[25] | 1 | 68 | 1.5 | Chronic for both knee and hip | IV2 | Hip disarticulation | TKA incision breakdown for infection | Mating of a PROSTALAC spacer with an intramedullary nail |
| Angelini et al[26] | 1 in 41 | 66 | 1.5 | 1.3-mo after the first surgery | III-B2 | Healed | Deep infection | 3D-printed prosthetic implant |
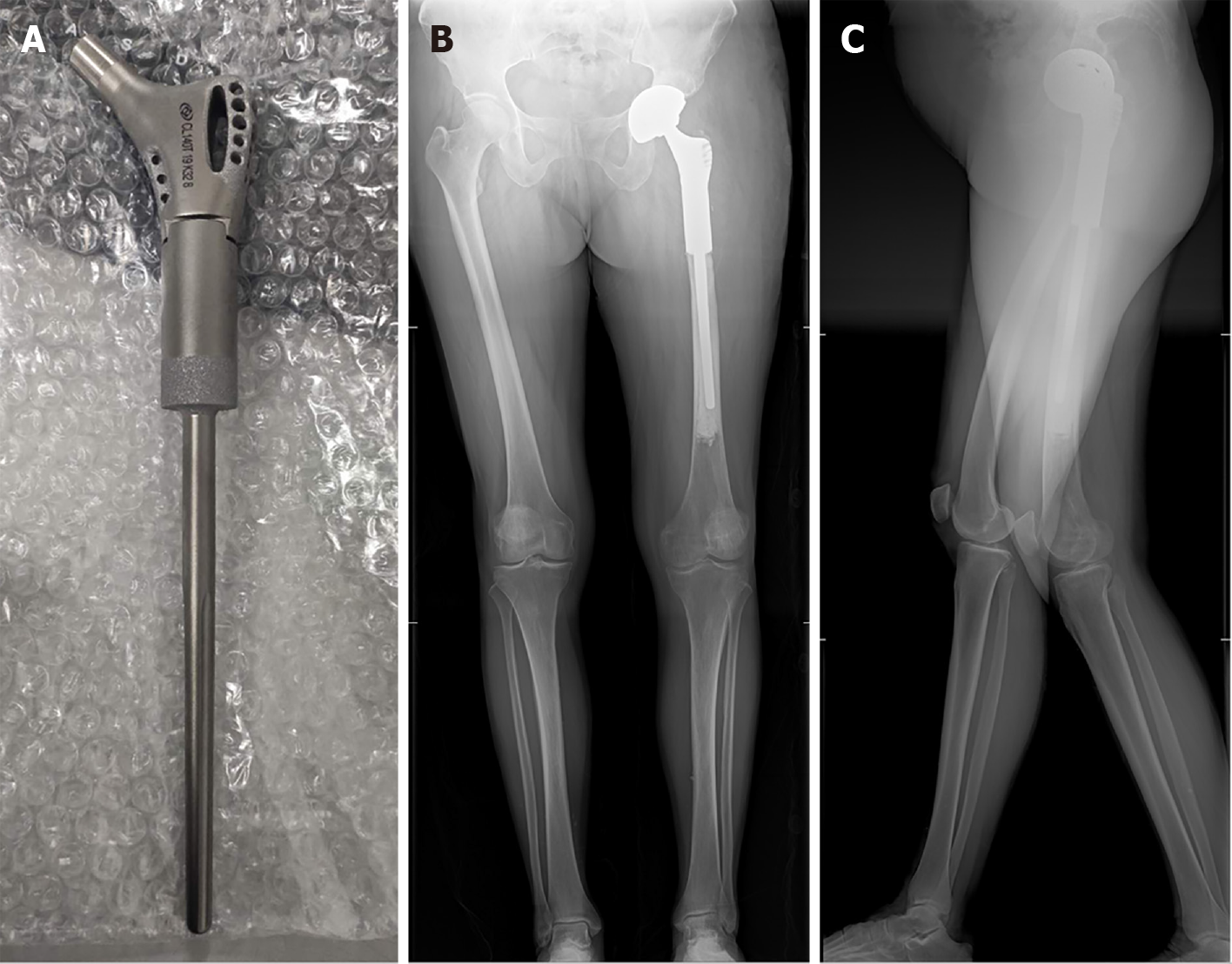
To reconstruct this large, atypical segmental femoral bone deficiency, a custom-made PFP was designed and manufactured by a qualified medical implant provider (Beijing Chunlizhengda Medical Instruments Corporation, Beijing, China) (Figure 6A). To adjust the lower limb length to fit the uneven proximal cortical bone, three accessory ring blocks of different height (5 mm, 10 mm, and 15 mm) were made available. The 10 mm block was chosen intraoperatively to neutralize any shortening of the femur. The postoperative radiographs showed excellent resolution of the proximal femoral defect with the custom-made prosthesis. The patient regained a near-anatomical hip joint with significant symptomatic improvement after years of discomfort and loss of function (Figure 6B and C).
In this case report, we have demonstrated the safety, feasibility, and effectiveness of two-stage revisional surgery for chronic PFI with a concurrent segmental femoral defect using a 3D-printed customized ALCS (first-stage) and a custom-made PFP (second-stage). We propose that the advantages of the custom-made ALCS are retention leg length and lateral offset, facilitating second stage revision, a robust fixation, and a low risk of dislocation or breakage. The apparent advantage of the custom-made PFP is near-perfect anatomical reconstruction of the affected hip with maximal preservation of bone tissue. Although manufacturing custom-made spacers and femoral prostheses is expensive and time-consuming, it presents a useful alternative when there is no suitable standard implant.
The authors are thankful to the Wenwen-Sun from the Department of Pathology, The First Affiliated Hospital of Wenzhou Medical University for her help in pathology. We are thankful to the patient enrolled in this study.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Baryshnikova NV S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Li X
| 1. | Ferguson RJ, Palmer AJ, Taylor A, Porter ML, Malchau H, Glyn-Jones S. Hip replacement. Lancet. 2018;392:1662-1671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 379] [Article Influence: 54.1] [Reference Citation Analysis (0)] |
| 2. | Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2079] [Cited by in RCA: 3257] [Article Influence: 180.9] [Reference Citation Analysis (0)] |
| 3. | Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, Shohat N. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J Arthroplasty. 2018;33:1309-1314.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 885] [Cited by in RCA: 1398] [Article Influence: 199.7] [Reference Citation Analysis (0)] |
| 4. | Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR; Infectious Diseases Society of America. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56:e1-e25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1079] [Cited by in RCA: 1402] [Article Influence: 107.8] [Reference Citation Analysis (0)] |
| 5. | Jacobs C, Christensen CP, Berend ME. Static and mobile antibiotic-impregnated cement spacers for the management of prosthetic joint infection. J Am Acad Orthop Surg. 2009;17:356-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 88] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Veltman ES, Moojen DJ, Glehr M, Poolman RW. Similar rate of infection eradication for functional articulating, prefabricated and custom-made spacers in 2-stage revision of the infected total hip: a literature review. Hip Int. 2016;26:319-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Ohtsuru T, Morita Y, Murata Y, Munakata Y, Itoh M, Kato Y, Okazaki K. Custom-made, antibiotic-loaded, acrylic cement spacers using a dental silicone template for treatment of infected hip prostheses. Eur J Orthop Surg Traumatol. 2018;28:615-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Veltman ES, Moojen DJF, Poolman RW. Improved patient reported outcomes with functional articulating spacers in two-stage revision of the infected hip. World J Orthop. 2020;11:595-605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Klinder A, Zaatreh S, Ellenrieder M, Redanz S, Podbielski A, Reichel T, Bösebeck H, Mittelmeier W, Bader R. Antibiotics release from cement spacers used for two-stage treatment of implant-associated infections after total joint arthroplasty. J Biomed Mater Res B Appl Biomater. 2019;107:1587-1597. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Wahlig H, Dingeldein E, Buchholz HW, Buchholz M, Bachmann F. Pharmacokinetic study of gentamicin-loaded cement in total hip replacements. Comparative effects of varying dosage. J Bone Joint Surg Br. 1984;66:175-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 81] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Luu A, Syed F, Raman G, Bhalla A, Muldoon E, Hadley S, Smith E, Rao M. Two-stage arthroplasty for prosthetic joint infection: a systematic review of acute kidney injury, systemic toxicity and infection control. J Arthroplasty. 2013;28:1490-8.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 12. | van Raaij TM, Visser LE, Vulto AG, Verhaar JA. Acute renal failure after local gentamicin treatment in an infected total knee arthroplasty. J Arthroplasty. 2002;17:948-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 92] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Whiteside LA, Peppers M, Nayfeh TA, Roy ME. Methicillin-resistant Staphylococcus aureus in TKA treated with revision and direct intra-articular antibiotic infusion. Clin Orthop Relat Res. 2011;469:26-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Oshima S, Yasunaga Y, Yamasaki T, Yoshida T, Hori J, Ochi M. Midterm results of femoral impaction bone grafting with an allograft combined with hydroxyapatite in revision total hip arthroplasty. J Arthroplasty. 2012;27:470-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Babis GC, Sakellariou VI, O'Connor MI, Hanssen AD, Sim FH. Proximal femoral allograft-prosthesis composites in revision hip replacement: a 12-year follow-up study. J Bone Joint Surg Br. 2010;92:349-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Mayle RE Jr, Paprosky WG. Massive bone loss: allograft-prosthetic composites and beyond. J Bone Joint Surg Br. 2012;94:61-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Meluzio MC, Oliva MS, Minutillo F, Ziranu A, Saccomanno MF, Maccauro G. The use of knee mega-prosthesis for the management of distal femoral fractures: A systematic review. Injury. 2020;51 Suppl 3:S17-S22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Gautam D, Malhotra R. Megaprosthesis vs Allograft Prosthesis Composite for massive skeletal defects. J Clin Orthop Trauma. 2018;9:63-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (1)] |
| 19. | Diaz-Dilernia F, Slullitel PA, Oñativia JI, Comba FM, Piccaluga F, Buttaro MA. Impaction Bone Grafting or Uncemented Modular Stems for the Treatment of Type B3 Periprosthetic Femoral Fractures? J Arthroplasty. 2019;34:2051-2057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Chandrasekar CR, Grimer RJ, Carter SR, Tillman RM, Abudu A, Buckley L. Modular endoprosthetic replacement for tumours of the proximal femur. J Bone Joint Surg Br. 2009;91:108-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 99] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 21. | Jones NF, Eadie P, Johnson PC, Mears DC. Treatment of chronic infected hip arthroplasty wounds by radical debridement and obliteration with pedicled and free muscle flaps. Plast Reconstr Surg. 1991;88:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Hsieh PH, Shih CH, Chang YH, Lee MS, Yang WE, Shih HN. Treatment of deep infection of the hip associated with massive bone loss: two-stage revision with an antibiotic-loaded interim cement prosthesis followed by reconstruction with allograft. J Bone Joint Surg Br. 2005;87:770-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Westerman RW, Timperley AJ. Use of an anatomic long-stemmed component in femoral impaction grafting. Hip Int. 2016;26:e1-e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 24. | Wang X, Xu H, Zhang J. Using personalized 3D printed Titanium sleeve-prosthetic composite for reconstruction of severe segmental bone loss of proximal femur in revision total hip arthroplasty: A case report. Medicine (Baltimore). 2020;99:e18784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 25. | Kamath AF, Austin D, Lee GC. Mating of a PROSTALAC spacer with an intramedullary nail for reconstruction of an infected interprosthetic femoral shaft fracture: a case report. J Orthop Surg (Hong Kong). 2012;20:263-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Angelini A, Kotrych D, Trovarelli G, Szafrański A, Bohatyrewicz A, Ruggieri P. Analysis of principles inspiring design of three-dimensional-printed custom-made prostheses in two referral centres. Int Orthop. 2020;44:829-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |